Abstract
Non-medulloblastoma CNS embryonal tumors (former PNET/Pineoblastomas) are aggressive malignancies with poor outcome that have been historically treated with medulloblastoma protocols. The purpose of this study is to present a tumor-specific, real-world data cohort of patients with CNS-PNET/PB to analyze quality indicators that can be implemented to improve the outcome of these patients. Patients 0–21 years with CNS-PNET treated in eight large institutions were included. Baseline characteristics, treatment and outcome [progression-free and overall survival (PFS and OS respectively)] were analyzed. From 2005 to 2014, 43 patients fulfilled entry criteria. Median age at diagnosis was 3.6 years (range 0.0–14.7). Histology was pineoblastoma (9%), ependymoblastoma (5%), ETANTR (7%) and PNET (77%). Median duration of the main symptom was 2 weeks (range 0–12). At diagnosis, 28% presented with metastatic disease. Seventeen different protocols were used on frontline treatment; 44% had gross total resection, 42% craniospinal radiotherapy, 86% chemotherapy, and 33% autologous hematopoietic stem cell transplantation (aHSCT). Median follow-up for survivors was 3.5 years (range 1.7–9.3). 3-year PFS was 31.9% (95% CI 17–47%) and OS 35.1% (95% CI 20–50%). Age, extent of resection and radiotherapy were prognostic of PFS and OS in univariate analysis (p < 0.05). Our series shows a dismal outcome for CNS-PNET, especially when compared to patients included in clinical trials. Establishing a common national strategy, implementing referral circuits and collaboration networks, and incorporating new molecular knowledge into routine clinical practice are accessible measures that can improve the outcome of these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Embryonal neuroectodermal tumors of the CNS that are not medulloblastoma, previously called central nervous system primitive neuroectodermal tumors (CNS-PNET) and pineoblastomas (PB) [1, 2], are rare and aggressive embryonal tumors with poor outcome. Together, they account for less than 5% of childhood CNS tumors [3, 4].
Due to their low incidence and to their insufficiently known biology, these tumors have been historically treated with protocols for high-risk medulloblastoma. However, there is growing evidence from molecular genetic studies that CNS-PNET, PB, new entities such as embryonal tumors with multilayered rosettes (ETMR), and medulloblastoma are different entities [5,6,7,8]. This knowledge has already been reflected in the most recent 2016 World Health Organization (WHO) classification, that differentiated pineoblastoma from ETMR, C19MC-altered, and has created a “wastebasket” category of CNS embryonal tumors, NOS [2]. There seems to be clinical differences as well, with CNS-PNET/PB showing a more aggressive behavior and lower survival rates than medulloblastoma [9].
Despite the achieved improvement over the last years, the historical series show a 5-year overall survival (OS) of 18–38% [10,11,12,13,14]. In addition, when practice-changing strategies obtained from clinical trials in particular institutions are brought to general clinical practice, the results, i.e. real-world data, are recurrently disappointing [15].
The two main aims of this study are: to present a tumor-specific, national real-world data cohort (as opposed to clinical trials data) of children and adolescents with CNS-PNET/PB and to identify weak points and quality indicators that can be implemented to improve the still dismal outcome of these patients.
Methods
Patient identification
Major Spanish pediatric cancer hospitals, all of them with one member participating in the CNS Tumors Group of the Spanish Society of Pediatric Hematology and Oncology (SEHOP), were contacted. At each site, the hospital’s clinical database was queried for all patients with the diagnosis of “PNET”, “pineoblastoma”, “ependymoblastoma” and “Embryonal Tumor with Abundant Neuropil and True Rosettes” (ETANTR) between 2005 and 2014.
(Note: At the beginning of data inclusion, the old terminology “PNET” was being used. Subsequently, the new 2016 WHO classification was published, removing the term ¨PNET” and reclassifying those tumors into the subtypes “ETMR, C19MC-altered”, “ETMR, NOS”, “Medulloepithelioma”, “CNS neuroblastoma”, “CNS ganglioneuroblastoma”, and “CNS embryonal tumor, NOS” [2]. The old terminology was used for this study.)
The Clinical Research Ethics Committee from Hospital Niño Jesus centrally approved the study. Local institutional approval for retrospective chart review was sought at all participating hospitals.
Eligibility
Inclusion criteria were histologically confirmed diagnosis of CNS-PNET/PB (according to the 2007 WHO classification [1]), ependymoblastoma and ETANTR, age 0–21 years at diagnosis, time of diagnosis between January 2005 and December 2014, and fully available clinical data. For this study, available pathology reports were reviewed by an experienced neuro-pathologist.
Record review
Data collected included demographic information, age and symptoms at diagnosis, extent of disease, extent of surgical resection, initial treatment strategy and its deviations and toxicities, as well as information regarding relapses and salvage treatments, if any, and outcome.
Size and location of primary tumor was assessed by the diagnostic MRI. Size of the primary tumor was measured in three dimensions. Standard Chang M-stage classification as established for medulloblastoma was used [16].
Extent of resection was determined from the operative report as well as post-operative MRI. Gross total resection (GTR) was defined as no evidence of enhancing tumor on post-operative imaging. Subtotal resection (STR) was defined as any surgical resection less than GTR. A third designation, “biopsy only”, was given to patients whose operative note included that text.
Chemotherapy (CT) modifications were defined as time-intensity deviations (delay > 1 week between cycles), dose-intensity deviations (> 10% dose reduction of CT agents) and/or CT agents withdrawal.
Toxicities were evaluated following the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE), v.4.03 [17].
Patients were stratified regarding whether they received radiotherapy as first-line non-surgical treatment (radiation-inclusive strategies), as opposed to those who followed radiation-sparing baby-brain strategies.
Statistical analysis
Time to progression was calculated from the date of first treatment to the date of radiologic progression. Endpoint of analysis for all patients was either the date of last follow-up or date of death.
Survival was estimated using the Kaplan–Meier method, and exact log-rank test was used for comparisons of survival in different groups. Progression free survival (PFS) was defined as the date of first treatment to date of first progression or relapse, or the date of last follow-up. Overall survival (OS) was defined as the date of first treatment to death of any cause or the date of last follow-up. Log-rank test was applied to identify significant prognostic factors for PFS and OS. 95% confidence intervals (CI) were provided. The significance level was fixed for all P values under 0.05. Analysis was performed using the SPSS software®, version 21.0, and the free software R, version 3.4.0. The ability to do multivariate analysis was limited due to the small sample size and was therefore not performed.
Results
Patient demographics and presentation
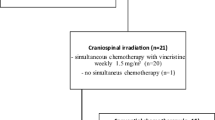
Eight major institutions (out of all nine contacted, belonging to the CNS tumors group of the SEHOP) contributed to this study and included all their potential patients: 52 patients aged 0–21 years with local histological diagnosis of CNS-PNET/PB were registered. Nine patients were excluded from this analysis: three patients who did not meet all inclusion criteria on central review and six patients whose medical records were incomplete (Fig. 1).
That yielded 43 eligible patients (22 male, 21 female). Demographic and diagnosis characteristics are shown in Table 1. The median age at diagnosis was 3.6 years (range 0.01–14.70). None of the patients had relevant medical history or identified genetic disorders.
At presentation, symptoms were heterogeneous, with headache, vomiting or irritability/somnolence occurring in > 81% of patients (Table 1). Median duration of the main symptom was 2 weeks (range 0–12).
Median longest diameter of primary tumor was 60.5 mm (range 21.0–95.0).
At diagnosis, 12 patients (28%) presented with metastatic disease. One patient was classified as M1 (2%), six as M2 (14%) and five as M3 (12%).
Histology was pineoblastoma (n = 4, 9%), ependymoblastoma (n = 2, 5%), ETANTR (n = 3, 7%), ganglioneuroblastoma (n = 1, 2%) and PNET (n = 33, 77%). Full pathology reports were reviewed in light of the 2007 WHO criteria for 36 patients (84%). 28 cases (78% of those with available pathology report) had all required information to confirm the diagnosis of CNS-PNET and 8 cases (22%) had insufficient descriptive information to confirm the diagnosis of CNS-PNET.
First line treatment
Global strategy
Frontline treatment strategy was very heterogeneous with 17 different approaches. The most frequently used protocols were Head Start II (n = 8, 19%), SIOP-PNET 4 (n = 5, 12%) and HART-MILAN (n = 3, 7%), all of them originally designed for patients with medulloblastoma [18,19,20,21,22]. In spite of this disparity of strategies, all of them included surgery with the widest possible resection and craniospinal irradiation (CSI) whenever the patient’s age and condition allowed it. Patients were treated upon two main categories, radiation-sparing and radiation-inclusive protocols, depending on their age, with a cut off between 3 and 4 years; the use of radiotherapy (RT) on first line applied for older patients, and sparing or delaying radiation for younger patients. Following this classification, 24 patients (56%) were treated with treatment strategies designed to avoid radio-induced brain damage, whereas 19 patients (44%) were treated with radiation-inclusive regimens.
The most important differences in treatment strategies were found among chemotherapy regimens, especially on their drug doses and time-design. Another extended first-line modality was aHSCT, with up to a third of patients (n = 14, 33%) undergoing transplant (eight within radiation-sparing strategies, six within radiation-inclusive strategies).
Surgery
All patients underwent surgery on the first-line approach. Median time to surgery (from MRI diagnosis) was three days (range 0–36). GTR was accomplished on first surgery in 19 patients (n = 43, 44%) and on second-look surgery in four patients (n = 43, 9.5%). In seven patients (16.5%) only STR was achieved, despite five of them undergoing a second-look surgery.
Twenty patients (47%) showed grade 3–4 severe surgical complications: cranial nerves paresis/paralysis (n = 7, 16.5%), other motor symptoms such as hemiparesis, limb weakness or hypotonia (n = 11, 26%), infection (n = 2, 5%). Five patients (12%) underwent second surgery due to complications derived from the first one. Two patients (5%) died due to brain hemorrhage during the second surgery, both performed as a second-look attempt; both patients were neonates.
Radiotherapy
RT was administered to 19 patients (n = 43, 44%) as frontline treatment. Four children older than 4 years did not receive RT on first line: in one patient, due to his palliative situation; in the other three, due to radiation-sparing treatment protocols (Head Start II [18] and COG-ACNS0334 -NCT00336024-). Median total dose was 55.8 Gy (range 54.0–62.0). Median CSI dose was 23.4 Gy (range 22.4–39.7) and median dose of the boost to the primary tumor was 26.5 Gy (range 18.0–32.4). One of the patients (8 year-old) received focal RT without CSI. Median duration of RT was 43 days (range 32–59). Most patients (n = 12, 63%) presented acute toxicity (first three months after RT start date), but this consisted mainly of grade 1–2 radiodermatitis (n = 8, 67% of patients with toxicity). Three patients had grade 3 toxicities (pancytopenia, vomiting). All patients completed the full planned radiation dose.
Chemotherapy
Most patients received CT as part of their first line treatment (n = 37, 86%). When combined with irradiation (n = 18), CT was administered as consolidation after RT in 12 (67%) patients, and prior to RT in six (33%) patients.
Intrathecal CT was used in 23% of the patients (n = 8/35). Median duration of CT treatment was 4.3 months (range 0.1–14.5). Up to 63% of patients (n = 22/35, 2 unknown) required significant modifications on the original CT plan due to chemotherapy-related toxicities. Forty-nine percent (n = 17/35) had time-intensity modifications, with at least one significant delay on a CT-cycle start. Twenty-six percent (n = 9) had dose-intensity modifications, with at least one CT agent dose reduction (min. 20% over initial dose). In 23% (n = 8) of the patients at least one CT agent had to be withdrawn or substituted with another agent (e.g. carboplatin for cisplatin due to tubulopathy).
Autologous HSCT
aHSCT was performed as part of the first-line strategy on 14 patients (33%), in five (35%) of them in combination with irradiation. It followed RT as consolidation treatment in three (21%) patients, and was administered prior to irradiation in two (14%). Most of them underwent a triple or quadruple tandem transplantation (n = 11/14, 79%) [23]. Patients were on situation of complete response (n = 7, 50%) or partial response (n = 7, 50%) prior to starting aHSCT. One of the patients went from partial response to complete response after aHSCT, one went from partial response to progressive disease, and the rest had the same disease status after aHSCT. Nine patients (64%) had grade 3–4 post-HSCT toxicities aside from hematologic toxicities.
Toxic mortality
Two patients (5%) died due to toxicity, both during surgery. No patients died due to CT or RT toxicity. During follow-up, no patients developed second malignancies or died of therapy-related causes after completion of treatment.
Relapse and patterns of failure
Twenty-eight (65%) patients experienced relapse. Median time to first relapse was 6.7 months (range 2.3–44.9). Nine (32%) patients had received RT as frontline treatment.
Eight patients (n = 43, 19%) had a second relapse and three (7%) a third relapse.
First relapse was local in 14/28 patients (50%), metastatic in eight patients (29%), and both local and metastatic in six patients (21%).
Salvage treatment on first relapse
Surgery was used on 13/28 patients (46%), but only in 4/13 patients (31%) GTR was achieved (one of them needing second-look surgery). RT was used on 10/28 patients (36%). Only one of them had received RT previously as first line approach and had re-irradiation. 15/28 patients (54%) were treated with chemotherapy, nine of them (60%) with diverse irinotecan-temozolomide regimens [24] and two with metronomic regimens [25]. Two patients also received intrathecal chemotherapy and another two underwent aHSCT. Only one patient (n = 28, 4%) received novel agents (bevacizumab and rapamycin), both used off-label. There are three survivors among the relapsed patients, with a follow-up of 1.8, 2.4 and 3.5 years. The first two patients had local relapse; both underwent surgery, achieving GTR. The third patient presented both with local and metastatic relapse (M2); he did not undergo surgical resection. All three received first RT at the time of salvage therapy, and all three received adjuvant chemotherapy as well.
Outcomes and prognostic factors
Median follow-up for survivors was 3.5 years (range 1.7–9.3). For the whole population, 3 year PFS was 31.9% (95% CI 17–47%) and 3 year OS was 35.1% (95% CI 20–50%), as shown in Fig. 2.
Age less than 3 years at diagnosis, not achieving GTR and not having been irradiated in first line were variables significantly associated with worse outcome in the univariate analysis (p < 0.05), with impact on both PFS and OS (see Table 2).
Neurocognitive outcome
The study did not include routine neurocognitive assessments due to its retrospective nature and hence, these toxicities are likely under-reported. Grade 3–4 long-term neurocoginitive toxicities/sequelae were present in 11/15 (73%) survivors, all of them needing intensive physical and neurocognitive rehabilitation treatment. These moderate-severe sequelae included hearing (27%) and visual impairment (20%), learning difficulties and/or IQ loss (27%), epilepsy (20%) and other neurological deficits, e.g. neuropathy (33%).
Discussion
Despite general improvement in the outcome of children with CNS tumors over the last decades, unacceptable mortality rates in patients with the formerly called PNET persist [10,11,12,13,14].
In addition to their low incidence and biological aggressiveness, these tumors have remained in the shadow of medulloblastoma. Instead of displaying specific approaches, PNET/PB have been historically included in medulloblastoma clinical trials [14, 18,19,20,21,22].
Moreover, lack of biological understanding of PNET adds to the critical deficiency in specific and novel treatment strategies. Recent molecular genetic studies [8] are extending our knowledge on these tumors, but we are still far from being able to translate this learning into the clinic. Furthermore, these studies suggest that a large proportion of PNET (up to 61% according to Sturm et al.) are being misdiagnosed under conventional histopathological criteria and are, in fact, high grade gliomas, ependymomas, or other tumors.
We conducted this study to establish how children with non-medulloblastoma embryonal CNS tumors (so called supratentorial PNET and pineoblastoma) have been managed over the last decade in Spain and identify areas of improvement.
Survival data in our study show a 3 year OS of 35.1% (95% CI 20–50%); in children < 3 years this drops to 10% (95% CI 0–27%), whereas in children > 3 years it is 45% (95% CI 25–65%). These results are close to a similar population-based study performed on UK (National Registry of Childhood Tumours –NRCT-) [15], where the authors described a 5 year OS of 32.5% for PNET. Our results are close as well to a similar study conducted by the Canadian Pediatric Brain Tumor Consortium [26], with a 4 year survival of 37.7%. However, they are far from US survival data (NCI’s Surveillance, Epidemiology, and End Results –SEER-) reflected on the same study, with a 5 year OS of 57.4%, which was conducted an earlier decade than ours (1996–2005). Of note, our study represents the practice of eight large institutions in our country, all having a pediatric oncologist participating into the CNS tumor group of the national Society. According to the national tumor registry (RETI), there are approximately five to six new cases of CNS-PNET per year in Spain. Our study, spanning 10 years, would have provided data for more than 75% of all cases over that period, but might not reflect the overall nation-wide situation where more than 40 pediatric oncology units treat children and adolescents with cancer [27]. The lack of a central pathology review is another limitation of the study; nevertheless, we put the accent on reporting the current situation with real-world data about clinical outcomes without further delays.
When compared to results obtained from clinical trials, the gap to our real-world data is widened. For instance, young children enrolled on the original Head Start I and II trials (the most frequently applied treatment strategy in our study) had 5 year EFS and OS of 39% (95% CI 24–53%) and 49% (95% CI 33–62%), respectively [9].
This recurrent gap between clinical trials and real-world survival reflects the need for collaboration through international multi-centric trials. Part of this difference can be explained by the strict patient selection of trials. However, it has been repeatedly pointed out in the literature that the recruitment into clinical trials improves the outcomes when compared to unselected populations treated at the discretion of the clinician [15, 28, 29]. Since none of the 43 patients included in this study were recruited into a clinical trial (neither on first line treatment nor at relapse), this is certainly a point that could be improved. Beyond that, with 17 different first-line strategies, the first step towards improvement should be, in our opinion, to establish a common national strategy for the treatment of these patients.
In the absence of internationally accepted quality standards for treatment of children with CNS tumors, the search for specific aspects to be improved is challenging. This report suggests the importance of several factors: Firstly, attention should be paid to time from initial symptoms to diagnosis. In our study, the median of this interval was two weeks (range 0–12), a good result when compared to data reported for CNS tumors in other countries (Germany 24 days, Switzerland 60 days, UK 100 days) [15, 30, 31]. While different studies have not demonstrated a prognostic impact of time to diagnosis, it remains important to ensure rapid initial diagnosis [32,33,34,35].
Also, our report shows that 74% of patients receive surgery within less than a week. However, of the 19 patients with irradiation planned upfront, only 42% received radiotherapy within 49 days of first surgery.
Secondly, extent of resection is a well-known prognostic factor, also reflected in our study, where the experience of the neurosurgical team is key. In our study only half of the patients (23/43) achieved GTR. In this sense, national initiatives such as the creation of reference centers for complex neurosurgery [36] are positive and its impact will be evaluated in the future.
Thirdly, radiotherapy is another crucial factor impacting patients’ outcome, but its association with long-term morbidity, particularly in young children, is the major limitation. Hence, postsurgical radiotherapy deferral is common practice in children younger than 3 years, but it remains controversial in older children, especially in the “grey zone” 3–4 years, leading to disparity of criteria among scientific groups and institutions [37]. There were four children older than 4 years in our study that did not undergo RT as first-line treatment. In one of them this was due to his palliative situation, and he passed away soon after diagnosis. The other three were treated using protocols designed for young children (Head Start II [18] and COG-ACNS0334 -NCT00336024-). All three underwent RT on first relapse, but only one of them was rescued.
Fourthly, there are no established standards to quantify major toxicities, toxic deaths and modifications in chemotherapy time and dose intensity. These treatment protocols have potential significant toxicities and this study will serve as a baseline to measure new indicators prospectively.
The main conclusion of this work is that although we benefit from a well-established health care system in Spain, there is a strong need for collaboration and networking in the treatment of complex CNS tumors such as PNET/PB. The efficacy of the primary care system is reflected in our study in the fast diagnosis of these patients. Survival rates of children with PNET/PB are far from the rates obtained in international clinical trials and a common therapeutic strategy is lacking. This study has served to identify specific aspects to improve in the care of patients with CNS-PNET, namely developing a common treatment strategy, ideally within international collaborative clinical trials, improving referral pathways and reference centers for treatment of complex and rare tumors, maximizing collaboration among pediatric oncology centers, and incorporating new biological markers and the new classification of embryonal CNS tumors. As a result of this study, a subsequent retrospective molecular analysis of archival tumor samples available for this patient cohort has been started in collaboration with European reference centers. Hopefully this will lead to improved outcomes for children with CNS-PNET in the near future.
Abbreviations
- aHSCT:
-
Autologous hematopoietic stem cell transplantation
- CNS:
-
Central nervous system
- CT:
-
Chemotherapy
- CTCAE:
-
Common terminology criteria for adverse events
- CI:
-
Confidence interval
- CSI:
-
Craniospinal irradiation
- ETANTR:
-
Embryonal tumor with abundant neuropil and true rosettes
- ETMR:
-
Embryonal tumor with multilayered rosettes
- GTR:
-
Gross total resection
- MRI:
-
Magnetic resonance imaging
- NCI:
-
National Cancer Institute
- OS:
-
Overall survival
- PB:
-
Pineoblastomas
- PNET:
-
Primitive neuroectodermal tumors
- PFS:
-
Progression free survival
- RT:
-
Radiotherapy
- SEHOP:
-
Spanish society of pediatric hematology and oncology
- STR:
-
Subtotal resection
- WHO:
-
World Health Organization
References
Louis DN, Ohgaki H, Wiestler OD et al (2007) The 2007 WHO classification of tumours of the central nervous system (vol 114, pg 97, 2007). Acta Neuropathol 114:547. https://doi.org/10.1007/s00401-007-0243-4
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World Health Organization Classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Ostrom QT, Gittleman H, Fulop J et al (2015) CBTRUS Statistical Report: primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2008–2012. Neuro Oncol 17:iv1–iv62. https://doi.org/10.1093/neuonc/nov189
Gatta G, Botta L, Rossi S et al (2014) Childhood cancer survival in Europe 1999–2007: results of EUROCARE-5-a population-based study. Lancet Oncol 15:35–47. https://doi.org/10.1016/S1470-2045(13)70548-5
Li MH, Bouffet E, Hawkins CE et al (2005) Molecular genetics of supratentorial primitive neuroectodermal tumors and pineoblastoma. Neurosurg Focus 19:E3. https://doi.org/10.3171/foc.2005.19.5.4
Pfister S, Remke M, Toedt G et al (2007) Supratentorial primitive neuroectodermal tumors of the central nervous system frequently harbor deletions of the CDKN2A locus and other genomic aberrations distinct from medulloblastomas. Genes Chromosom Cancer 46:839–851. https://doi.org/10.1002/gcc.20471
Spence T, Sin-Chan P, Picard D et al (2014) CNS-PNETs with C19MC amplification and/or LIN28 expression comprise a distinct histogenetic diagnostic and therapeutic entity. Acta Neuropathol 128:291–303. https://doi.org/10.1007/s00401-014-1291-1
Sturm D, Orr BA, Toprak UH et al (2016) New brain tumor entities emerge from molecular classification of CNS-PNETs. Cell 164:1060–1072. https://doi.org/10.1016/j.cell.2016.01.015
Fangusaro J, Finlay J, Sposto R et al (2008) Intensive chemotherapy followed by consolidative myeloablative chemotherapy with autologous hematopoietic cell rescue (AuHCR) in young children with newly diagnosed supratentorial primitive neuroectodermal tumors (sPNETs): report of the Head Start I and I. Pediatr Blood Cancer 50:312–318. https://doi.org/10.1002/pbc.21307
Reddy aT, Janss a J, Phillips PC et al (2000) Outcome for children with supratentorial primitive neuroectodermal tumors treated with surgery, radiation, and chemotherapy. Cancer 88:2189–2193
Dirks PB, Harris L, Hoffman HJ et al (1996) Supratentorial primitive neuroectodermal tumors in children. J Neurooncol 29:75–84
Cohen BH, Zeltzer PM, Boyett JM et al (1995) Prognostic factors and treatment results for supratentorial primitive neuroectodermal tumors in children using radiation and chemotherapy: a Childrens Cancer Group randomized trial. J Clin Oncol 13:1687–1696
McBride SM, Daganzo SM, Banerjee A et al (2008) Radiation is an important component of multimodality therapy for pediatric non-pineal supratentorial primitive neuroectodermal tumors. Int J Radiat Oncol 72:1319–1323. https://doi.org/10.1016/j.ijrobp.2008.03.033
Timmermann B, Kortmann RD, Kühl J et al (2006) Role of radiotherapy in supratentorial primitive neuroectodermal tumor in young children: results of the German HIT-SKK87 and HIT-SKK92 trials. J Clin Oncol 24:1554–1560. https://doi.org/10.1200/JCO.2005.04.8074
Mathew RK, O’kane R, Parslow R et al (2014) Comparison of survival between the UK and US after surgery for most common pediatric CNS tumors. Neuro Oncol 16:1137–1145. https://doi.org/10.1093/neuonc/nou056
Dufour C, Beaugrand A, Pizer B et al (2012) Metastatic medulloblastoma in childhood: chang’s classification revisited. Int J Surg Oncol. https://doi.org/10.1155/2012/245385
Institute NC (2010) Common Terminology Criteria for Adverse Events v4.3. NCI, NIH, DHHS. http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_8.5x11.pdf
Dhall G, Grodman H, Ji L et al (2008) Outcome of children less than three years old at diagnosis with non-metastatic medulloblastoma treated with chemotherapy on the “Head Start” I and II protocols. Pediatr Blood Cancer 50:1169–1175. https://doi.org/10.1002/pbc.21525
Lannering B, Rutkowski S, Doz F et al (2012) Hyperfractionated versus conventional radiotherapy followed by chemotherapy in standard-risk medulloblastoma: results from the randomized multicenter HIT-SIOP PNET 4 trial. J Clin Oncol 30:3187–3193. https://doi.org/10.1200/JCO.2011.39.8719
Gandola L, Massimino M, Cefalo G et al (2009) Hyperfractionated accelerated radiotherapy in the Milan strategy for metastatic medulloblastoma. J Clin Oncol 27:566–571. https://doi.org/10.1200/JCO.2008.18.4176
Massimino M, Gandola L, Spreafico F et al (2006) Supratentorial primitive neuroectodermal tumors (S-PNET) in children: a prospective experience with adjuvant intensive chemotherapy and hyperfractionated accelerated radiotherapy. Int J Radiat Oncol 64:1031–1037. https://doi.org/10.1016/j.ijrobp.2005.09.026
Massimino M, Gandola L, Biassoni V et al (2013) Evolving of therapeutic strategies for CNS-PNET. Pediatr Blood Cancer 60:2031–2035. https://doi.org/10.1002/pbc.24540
Chintagumpala M, Hassall T, Palmer S et al (2008) A pilot study of risk-adapted radiotherapy and chemotherapy in patients with supratentorial PNET. Neuro Oncol 11:33–40. https://doi.org/10.1215/15228517-2008-079
Grill J, Geoerger B, Gesner L et al (2013) Phase II study of irinotecan in combination with temozolomide (TEMIRI) in children with recurrent or refractory medulloblastoma: a joint ITCC and SIOPE brain tumor study. Neuro Oncol 15:1236–1243. https://doi.org/10.1093/neuonc/not097
Robison NJ, Campigotto F, Chi SN et al (2014) A phase II trial of a multi-agent oral antiangiogenic (metronomic) regimen in children with recurrent or progressive cancer. Pediatr Blood Cancer 61:636–642. https://doi.org/10.1002/pbc.24794
Johnston DL, Keene DL, Lafay-Cousin L et al (2008) Supratentorial primitive neuroectodermal tumors: a Canadian pediatric brain tumor consortium report. J Neurooncol 86:101–108. https://doi.org/10.1007/s11060-007-9440-1
Peris Bonet R, Felipe García S, Valero Poveda SPRE. (2015) Cáncer infantil en España. Estadísticas 1980–2014. Registro Español de Tumores Infantiles (RETI-SEHOP). http://www.uv.es/rnti/pdfs/INFORME 1980-2014.pdf
Vivekanandan S, Breene R, Ramanujachar R et al (2015) The UK Experience of a treatment strategy for pediatric metastatic medulloblastoma comprising intensive induction chemotherapy, hyperfractionated accelerated radiotherapy and response directed high dose myeloablative chemotherapy or maintenance chemothera. Pediatr Blood Cancer 62:2132–2139. https://doi.org/10.1002/pbc.25663
Desandes E, Guissou S, Chastagner P, Lacour B (2014) Incidence and survival of children with central nervous system primitive tumors in the French National Registry of Childhood Solid Tumors. Neuro Oncol 16:975–983. https://doi.org/10.1093/neuonc/not309
Dobrovoljac M, Hengartner H, Boltshauser E, Grotzer M (2002) Delay in the diagnosis of paediatric brain tumours. Eur J Pediatr 161:663–667. https://doi.org/10.1007/s00431-002-1088-4
Reulecke BC, Erker CG, Fiedler BJ et al (2008) Brain tumors in children: initial symptoms and their influence on the time span between symptom onset and diagnosis. J Child Neurol 23:178–183. https://doi.org/10.1177/0883073807308692
Brasme J-F, Morfouace M, Grill J et al (2012) Delays in diagnosis of paediatric cancers: a systematic review and comparison with expert testimony in lawsuits. Lancet Oncol 13:e445–e459. https://doi.org/10.1016/S1470-2045(12)70361-3
Ferrari A, Lo Vullo S, Giardiello D et al (2016) The sooner the better? How symptom interval correlates with outcome in children and adolescents with solid tumors: regression tree analysis of the findings of a prospective study. Pediatr Blood Cancer 63:479–485. https://doi.org/10.1002/pbc.25833
Wilne S, Collier J, Kennedy C et al (2012) Progression from first symptom to diagnosis in childhood brain tumours. Eur J Pediatr 171:87–93. https://doi.org/10.1007/s00431-011-1485-7
HeadSmart Be Brain Tumour Aware HBBT (2016) A new clinical guideline from the Royal College of Paediatrics and Child Health with a national awareness campaign accelerates brain tumor diagnosis in UK children–“HeadSmart: be Brain Tumour Aware”. Neuro Oncol 18:445–454. https://doi.org/10.1093/neuonc/nov187
Sanidad M (Ministerio de, Igualdad) SS e Centros, Servicios y Unidades de Referencia del Sistema Nacional de Salud (CSUR). https://www.msssi.gob.es/profesionales/CentrosDeReferencia/CentrosCSUR.htm. Accessed 14 Apr 2017
Kann BH, Park HS, Lester-Coll NH et al (2016) Postoperative radiotherapy patterns of care and survival implications for medulloblastoma in young children. JAMA Oncol 25:62–68. https://doi.org/10.1001/jamaoncol.2016.2547
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was approved by the Institutional Review Board of Hospital Niño Jesús, and approval for retrospective chart review was sought at all participating hospitals. All procedures performed in this study were in accordance with the declaration of Helsinki (1964) and its later amendments and comparable ethical standards.
Additional information
On behalf of the CNS Tumors Group of the Spanish Society of Pediatric Hematology and Oncology (SEHOP).
Rights and permissions
About this article
Cite this article
de Rojas, T., Bautista, F., Flores, M. et al. Management and outcome of children and adolescents with non-medulloblastoma CNS embryonal tumors in Spain: room for improvement in standards of care. J Neurooncol 137, 205–213 (2018). https://doi.org/10.1007/s11060-017-2713-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2713-4