Abstract
We retrospectively evaluated 203 patients newly diagnosed with medulloblastoma between 1975 and 2006. All patients underwent surgical resection and after surgery were treated with a combination of radiotherapy and chemotherapy. CCNU-based protocols were used in the early years, with CDDP+VP16 being used more recently. Radiotherapy was used in patients older than three years of age according to the protocols. One hundred fifteen patients had total surgical resection, 78 had subtotal resection, and 4 patients had only a biopsy. Every patient received chemotherapy: 124 with the CCNU-based protocol, 75 with CDDP+VP16, and 4 with other protocols. Overall (OS) and event free-survival (EFS) rates were 43.1 and 41.9% in the whole group, with a median follow-up time of 8 years. OS rates for patients with and without spinal seeding were 30 and 63.1% (P = 0.0002). OS rates for males and females were 36.2 and 54.7% (P = 0.03). OS rates for patients receiving the CCNU and CDDP+VP16 protocols were 41.1 and 45%.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Medulloblastoma, an embryonal brain tumor, is the most frequently occurring brain tumor in children [1, 2]. It can constitute up to 40% of the posterior fossa. The treatment strategy is surgery, followed by radiotherapy and chemotherapy. Multidrug chemotherapy, cisplatin-based, or CCNU, procarbazine, and vincristine protocols are the most commonly used chemotherapy protocols. Multidrug chemotherapy has not been found superior to three-drug regimens in multicenter prospective trials. In recent years, brain tumors have been stratified according to risk categories. The most important prognostic factor is seeding at the time of diagnosis [3]. Patients in the standard risk group have been treated successfully, whereas the prognosis for high-risk patients is still poor, with survival rates not reaching 40%.
In this study, we analyze the clinical features, treatment, and outcome of 203 patients with medulloblastoma treated in our institution in the last 32 years.
Patients and methods
We identified 224 patients with a diagnosis of medulloblastoma at our institution between January 1975 and December 2006. We excluded patients who were treated in another oncology center, those who discontinued the therapy, and those who died early after surgery with surgical complications. For the remaining 203 patients, we analyzed retrospectively their clinical and epidemiological characteristics, histopathology, treatment modalities, survival rates and prognostic criteria.
All patients were evaluated with a complete physical and neurological examination. To evaluate the primary tumor, cranial computed tomography (CT) or magnetic resonance imaging (MRI) was used. Spinal extension was investigated with cervical, thoracal, and lumbar MRI in most of the patients. Surgical resection was done in all patients. Before 1984, the amount of resection was determined by the surgeon’s opinion and postoperative CT scans, whereas after 1984 it was decided by postoperative MRI findings. Total resection or gross-total resection was defined as no visible disease after surgery on postoperative imaging studies. The other surgical procedures were defined as follows: subtotal resection, where surgical removal was greater than 50% of the total tumor mass but visible tumor remained, and biopsy, where surgical removal was less than 10% of the total tumor mass. The histopathological diagnosis was confirmed by examination of the surgical specimens obtained from the primary tumor. Histopathologic classification of the tumor was made according to WHO criteria.
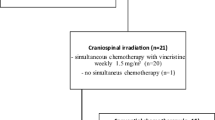
All patients were treated with a combination of radiotherapy and chemotherapy after surgery. Chemotherapy protocols were primarily chloroethylnitrosurea (CCNU) (100 mg/m2), procarbazine (100 mg/m2), vincristine (1 mg/m2), prednisolone (40 mg/m2) with 6-week intervals between 1975 and 1996, and cisplatinum 100 mg/m2 and etoposide 100 mg/m2 (CDDP+VP16) with a 4-week interval thereafter. Most of the patients were treated with fractionated conventional external beam radiotherapy to the craniospinal region. Radiotherapy doses for the cranium were 3,000 cGy and for the medulla spinalis were 2,500 cGy.
Mean and median values were used for demographic characteristics. Kaplan–Meier survival curves were used for survival analyses. The patient groups were compared in terms of survival duration using a log-rank test.
Results
Epidemiologic and clinical characteristics of the 203 patients are given in Table 1. There were 126 males and 77 females (M/F = 1.63) with a median age of 7 years (0.37–19 years) at diagnosis. The type of surgery was total in 115 (56.7%), subtotal in 78 (38.3%), biopsy in 4 (2.0%), and unknown in 6 (3.0%). Spinal seeding was determined in 31 (33.3%) of the 93 patients at diagnosis who were investigated for spinal involvement. Of the 128 patients whose tumor sizes were defined radiologically or perioperatively, tumor size was smaller than 3 cm in 10 (7.8%), 3–6 cm in 112 (87.5%), and larger than 6 cm in 6 (4.7%). Craniospinal radiotherapy was delivered to 198 patients (97.5%). Five patients who were under age of 3 years were not given radiotherapy because of their age. One hundred and twenty four patients (61.1%) were treated with a CCNU-based protocol, 75 (36.9%) with CDDP+VP16, and 4 with other protocols.
Overall survival (OS) and event-free survival (EFS) rates were 43.1 and 41.9% with a median follow-up time of 8 years (Fig. 1). The prognostic factors having a statistically significant influence on survival were gender (P = 0.03), age group (P = 0.04), and existence of spinal seeding (P = 0.0002) (Figs. 2 and 3). Among patients with medulloblastoma the survival rate for those with the desmoplastic type was 76.5%; for patients showing the classic type, 47.2%; and for those with large-cell type, 66.6% (P = 0.2).
The patients were divided into two groups according to the year of diagnosis; group 1, 1975–1995, and group 2, 1996–2006. There were 101 patients in group 1 and 102 in group 2. Overall survival for group 1 was 41.2 and 46.4% for group 2 (P = 0.4). The CDDP+VP16 chemotherapy protocol resulted in a survival rate of 44.9%, whereas the survival rate was 41.1% for those receiving the CCNU chemotherapy protocol and 33.3% for those treated with other chemotherapy regimes (P = 0.6). One patient treated with CDDP+VP16 died 9 years after diagnosis with recurrent disease. If we exclude this patient from the analysis, the overall survival rate in this group was 60%. Tumor size (P = 0,65) and type of surgery (P = 0.74) had no impact on survival (Table 2).
Discussion
According to the current WHO classification [4], embryonal brain tumors (EBTs) include medulloblastoma, medulloepithelioma, ependymoblastoma, supratentorial primitive neuroectodermal tumor (sPNET), and atypical teratoid/rhabdoid tumor (ATRT). The most frequently occurring embryonal brain tumor is medulloblastoma. The incidence of medulloblastoma—39% of all brain tumors—among our patients is slightly higher than found in other centers.
Although WHO designates medulloblastomas as grade IV, these tumors exhibit a wide spectrum of differentiation or anaplasia. Classic, desmoplastic, tumors with extensive nodularity, and large-cell type are the four medulloblastoma subtypes described in the 2000 WHO classification and used for prognostic potential [5]. Eberhart et al. [6] reported that desmoplasia was not associated with improved survival, but they found anaplasia to be a significant factor for poor prognosis. Other series have suggested a better prognosis for desmoplastic medulloblastoma compared to classic and large-cell/anaplastic subtypes [7, 8]. In our series, there was an increament in survival rate of patients with the desmoplastic type.
One of the unexpected findings in our study was the longer survival for girls compared to boys. Other studies have shown variable effects of gender on clinical outcome. Better survival for females was statistically significant in some series [6, 9]. However, other studies showed no survival disadvantage for boys nor any significant association of survival and gender [8, 10–12]. We could not explain the reason for the worse prognosis of male patients with medulloblastoma in our series.
Older patients have responded well to the therapy in our study (P = 0.04) in this group. In other studies, infants had the worst prognosis [13], primarily because they could not have radiotherapy or underwent delayed radiotherapy.
Metastatic stage is among the well-known clinical characteristics of prognostic significance. Many studies have reported the presence of dissemination at diagnosis as the dominant prognostic factor [3, 8, 12]. The survival rate of these high-risk patients in these studies was not higher than 30–40%. Similarly, in our series the patients with spinal metastasis at diagnosis had the worst prognosis (P = 0.0002).
To improve the survival of patients with medulloblastoma several chemotherapy protocols have been tried in combination with conventional surgery and radiotherapy. Among them the CCNU-based protocol and cisplatin plus etoposide protocol are the most commonly used. There are equivocal results in regard to chemotherapy reported in the literature. Packer et al. [14] reported a 5-year disease-free survival rate of 71% in medulloblastoma patients treated with radiotherapy and CCNU, cisplatin, and vincristine chemotherapy. A study conducted by CCG reported a 3-year disease-free survival rate of 80% in patients with medulloblastoma treated with a combination of radiotherapy and adjuvant chemotherapy [15]. In contrast, Padovani et al. [16] showed that chemotherapy had no impact on survival (P = 0.95) in adult patients with medulloblastoma. In our series, the cisplatin and etoposide chemotherapy protocol resulted in the highest rate of survival (44.9%). If we exclude the patient who died in 9 years from recurrent disease, the survival of the patients treated with the CDDP regimen was 60%. Most of our patients were given CCNU-based chemotherapy between 1975 and 1996; after 1996 they were given cisplatin plus etoposide with the intent of improving survival and decreasing toxicity.
The improvement in survival rates with medulloblastoma has been attributed to the use of more effective chemotherapy protocols, advances in surgical techniques, and better imaging and staging. However, postoperative radiotherapy plays the largest contributing factor to improved prognosis [17]. The posterior fossa dose given to medulloblastoma patients ranged between 34.3–72 Gy and to the rest of the craniospinal axis between 23.3–45.6 Gy [17, 18]. Most of the patients in the present series were given radiotherapy within 1–3 months after primary surgery with a dose of 3,000 cGy for the cranium and 2,500 cGy for the medulla spinalis. The timing of radiotherapy initiation after surgical intervention did not have a statistically significant effect on survival rates.
Overall survival and EFS in our series are comparable with other series reported in the literature [12]. Although 5-year survival rates of 50–60% have been achieved in medulloblastoma through the use of craniospinal radiotherapy and multiagent chemotherapy, damage to the developing nervous system of younger children is a major problem [5, 15, 19]. In this regard, risk classification is of major importance so that children in the standard-risk group can receive less aggressive therapy. For children older than 3 years standard-risk patients are defined as patients with localized disease at the time of diagnosis and total or nearly total resection. Patients younger than 3 years and those with disseminated disease or partially resected tumor are included in the high-risk group [13, 14, 20]. A non-metastatic, desmoplastic, female medulloblastoma patient can be categorized in the low-risk group in our study.
Medulloblastoma is the most common brain tumor in children. The prognostic factors in this study are gender, age group, and the presence of seeding. CDDP+VP16 was a more succesful treatment regimen. New treatment strategies should be sought for high-risk patients.
References
Blaney SM, Kun LE, Hunter J et al (2006) Tumors of the central nervous system. In: Pizzo PA, Poplack DG (eds) Principles and Practice of Pediatric Oncology, 5th edn. Lippincott Williams & Wilkins, Philadelphia, pp 786–864
Eberhart CG, Chaudhry A, Daniel RW (2005) Increased p53 immunopositivity in anaplastic medulloblastoma and supratentorial PNET is not caused by JC virus. BMC Cancer 5:19
Zeltzer PM, Boyett JM, Finlay JL et al (1999) Metastasis stage, adjuvant treatment, and residual tumor are prognostic factors for medulloblastoma in children: conclusions from the Children’s Cancer Group 921 randomized phase III study. J Clin Oncol 17:832–845
Kleihues P, Cavenee WK (eds) (2000) Pathology and genetics of tumors of the nervous system: World Health Organization classification of tumors. IARC Press, Lyon
Polkinghorn WR, Tarbell NJ (2007) Medulloblastoma: tumorigenesis, current clinical paradigm and efforts to improve risk stratification. Nat Clin Pract Oncol 4:295–304
Eberhart CG, Kepner JL, Goldthwaite PT et al (2002) Histopathologic grading of medulloblastomas. A pediatric oncology group study. Cancer 94:552–560
Bailey CC, Gnekow A, Wellek S et al (1995) Prospective randomised trial of chemotherapy given before radiotherapy in childhood medulloblastoma. International Society of Paediatric Oncology (SIOP) and the (German) Society of Paediatric Oncology (GPO): SIOP II. Med Pediatr Oncol 25:166–178
Jenkin D, Shabanah MA, Shail EA et al (2000) Prognostic factors for medulloblastoma. Int J Radiat Oncol Biol Phys 47:573–584
Weil MD, Lamborn K, Edwards MS et al (1998) Influence of a child’s sex on medulloblastoma outcome. JAMA 279:1474–1476
Danjoux CE, Jenkin RDT, McLaughlin J et al (1996) Childhood medulloblastoma in Ontario, 1977–1987: population based results. Med Pediatr Oncol 26:1–9
Gilbertson RJ, Jaros E, Perry RH et al (1997) Mitotic percentage index: a new prognostic factor for childhood medulloblastoma. Eur J Cancer 33:609–615
Urberuaga A, Navajas A, Burgos J, Pijoan JI (2006) A review of clinical and histological features of Spanish paediatric medulloblastomas during the last 21 years. Childs Nerv Syst 22:466–474
Varan A, Akalan N, Söylemezoğlu F et al (2006) Central nervous system tumors in patients under three years of age: treatment results of a single institute. Pediatr Neurosurg 42:89–94
Packer RJ, Sutton LN, Elterman R et al (1994) Outcome for children with medulloblastoma treated with radiation and cisplatin, CCNU and vincristine chemotherapy. J Neurosurg 81:690–698
Packer RJ, Goldwein J, Nicholson HS et al (1999) Treatment of children with medulloblastomas with reduced-dose craniospinal radiation therapy and adjuvant chemotherapy: a Children’s Cancer Group Study. J Clin Oncol 17:2127–2136
Padovani L, Sunyach MP, Perol D et al (2007) Common strategy for adult and pediatric medulloblastoma: a multicenter series of 253 adults. Int J Radiat Oncol Biol Phys 68:433–440
Delcharco JO, Bolek TW, McCollough WM et al (1998) Medulloblastoma: time-dose relationship based on a 30-year review. Int J Radiat Oncol Biol Phys 42:147–154
Prados MD, Edwards MSB, Chang SM et al (1999) Hyperfractionated craniospinal radiation therapy for primitive neuroectodermal tumors: results of a phase II study. Int J Radiat Oncol Biol Phys 43:279–285
Matsutani M (2004) Chemoradiotherapy for brain tumors: current status and perspectives. Int J Clin Oncol 9:471–474
Kortmann RD, Kühl J, Timmermann B et al (2000) Postoperative neoadjuvant chemotherapy before radiotherapy as compared to immediate radiotherapy followed by maintenance chemotherapy in the treatment of medulloblastoma in childhood: results of the German prospective randomized trial HIT ‘91. Int J Radiat Oncol Biol Phys 46:269–279
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akyüz, C., Varan, A., Küpeli, S. et al. Medulloblastoma in children: a 32-year experience from a single institution. J Neurooncol 90, 99–103 (2008). https://doi.org/10.1007/s11060-008-9638-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-008-9638-x