Abstract
Introduction
Neurodegenerative disorders are a diverse variety of diseases that can be distinguished from developing degeneration of neurons in the CNS. Several alkaloids have shown mounting effects in neurodegenerative disorders, and berberine is one of them. Demethyleneberberine is a metabolite of berberine that has better blood-brain barrier crossing capacity. Demethyleneberberine possesses anti-inflammatory, anti-oxidant, and mitochondrial targeting properties. However, neither the pharmacological action nor the molecular mechanism of action of demethyleneberberine on neurodegenerative disorders has been explored yet.
Materials and methods
A systematic literature review of PubMed, Medline, Bentham, Scopus, and EMBASE (Elseveier) databases was carried out with the help of keywords like “Demethyleneberberine; neuroinflammation; oxidative stress; Neuroprotective; Neurodegenerative disorders” till date.
Conclusion
This review focus on the neuroprotective potential of demethyleneberberine in neurodegenerative disorders by attenuating different pathways, i.e., NF-κB, MAPK, and AMPK signalling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neurodegenerative disorders (NDDs) affect the central nervous system (CNS) and are distinguished by the continuous degeneration of nerve cells. Neuronal changes impair their function and result in the demise of the cell. This is because neurons are unable to regenerate on their subsequent neural degeneration or damage [1]. The underlying cause of NDDs like Amyotrophic lateral sclerosis (ALS), Parkinson’s disease (PD), Epilepsy, Huntington’s disease (HD), Alzheimer's disease (AD), and stroke has been postulated to be oxidative damage [2]. Reactive oxygen species (ROS) can harm proteins, membrane polyunsaturated fatty acids, and nucleic acids resulting in the loss of membrane integrity, lipid peroxidation, a decrease in the potential of mitochondrial membrane, and an increase in plasma membrane's permeability to Ca2+ [3]. NDDs remain incurable and are notably increasing morbidity/mortality rates in developing countries, with a similar trend anticipated in developing countries as more statistics become available. The available treatments for NDDs are solely focused on disease management; actual treatment has yet to be examined [4]. Synthetic medications are used to treat NDDs and a variety of other chronic conditions, but they are not without negative effects such as extrapyramidal reactions caused by drugs like reserpine, metoclopramide and phenothiazines; riluzole can cause nausea, diarrhoea and rarely hepatotoxicity etc. Most drugs show their action by ameliorating the symptoms of disease, due to this the phytochemicals have gotten a lot of attention from researchers because of minimal side effects and good BBB crossing ability. Treatment with free radical scavengers or antioxidants targeted at reducing pro-oxidant synthesis or enhancing antioxidant defences [2, 5]. Since ancient times, phytomedicines or plant-derived components such as flavonoids and alkaloids have treated NDDs. They can be the most productive management and therapeutic agents for minimizing the critical characteristics of NDDs like amyotrophic lateral sclerosis, AD, PD, HD, epilepsy, and stroke [6]. Numerous phytochemicals exhibit neuroprotective activity, and among them, alkaloids are one of the most effective agents against NDDs. Plants, fungi and marine sponges all produce alkaloids which are a type of secondary metabolite. They are well-known as a trustworthy remedy for cancer, diabetes & therapeutic interventions for NDDs. Berberine (BBR) has been used in the Chinese and Ayurvedic systems of medicine for approximately 3100 years and can be obtained from various plants, namely Coptis Chinensis (golden thread or copies), Berberis vulgaris (barberry), Berberis aristata (tree turmeric) and Hydrastis canadensis (goldenseal)[6]. BBR alkaloids are a class of structurally disparate protoberberine compounds that comprise but are not limited to demethyleneberberine (DMB), jatrorrhizine, columbamine, palmatine and berberine. Berberine alkaloids are quaternary ammonium salts that spread a tetracyclic skeleton densely packed with hydroxyl oxidation states at locationsC2, C3, C9 and C10 [7]. BBR has been shown to improve pathology and symptoms related to AD, PD, HD, ALS, stroke and epilepsy [8,9,10,11,12,13,14].
Additionally, in various diabetes models of the animal, BBR has been proven to downregulate the pro-inflammatory cytokines and oxidative stress markers [15, 16]. DMB has been proposed to be the central intermediary in the biogenesis of berberine alkaloids. It was previously believed that the biosynthesis of berberine alkaloids began with the evolution of demethyleneberbeine from berberine. DMB was then methylated to form other types of berberine alkaloids [17, 18]. Due to less availability of literature on the neuroprotective potential of DMB, it was hypothesized that DMB possesses all the properties of berberine including neuroprotective potential, as DMB is a metabolite of berberine.
This review focuses on demethyleneberberine's neuroprotective potential in AD, PD, HD, ALS, epilepsy, and stroke via modulation of NF-κB, MAPK, and AMPK signalling.
Methodology
A systematic literature review of PubMed, Medline, Bentham, Scopus, and EMBASE (Elseveier) databases was carried out with the help of keywords like “Demethyleneberberine; neuroinflammation; oxidative stress; Neuroprotective; Neurodegenerative disorders” from 1985 to November 2021. The review was conducted using the above keywords to collect the latest articles and understand the nature of the extensive work done on Demethyleneberberine: Mechanistic and molecular approach in neurodegenerative disorders (Fig. 1).
Pathophysiology of neurodegenerative disorders in a nutshell
All neurodegenerative diseases are triggered by the unfolding of proteins, leading to the synthesis of “β-structures” and a pathological tendency for neuronal cell aggregation. This is a characteristic of tau protein in AD and various tauopathies linked with tau unfolding, huntingtin (htt) in Huntington's disease, and α-synuclein in PD. These unfolding events in proteins are molecular events that particularly initiate various NDDs. Notably, such episodes take place due to neuroinflammatory cascades [19]. Furthermore, based on the molecular pathogenesis, these diseases share a lot of similarities, and proteinopathy is one of them i.e. abnormal accumulation of misfolded proteins (accumulation of amyloid-beta (Aβ) in AD, α-synuclein PD, HTT in HD and p-TDP-43 aggregation in ALS) [20]. Normal ageing, dementia, high blood pressure, stroke, obesity, systemic and local infections, brain injury and environmental conditions all activate astrocytes, neurons and microglia in the brain, causing neuroinflammation. Immune & inflammatory cells in the brain, i.e. T-cells and mast cells, are also activated by these substances. Microglia & inflammatory cells that are activated trigger the discharge of cytokines and neurotoxic mediators, furthermore enhancing the expression of inflammatory receptor proteins in the brain. These inflammatory mediators and increased protein expressions exacerbate neuroinflammatory processes and neurodegeneration, leading to the progression of neurodegenerative disorders [21].
Alzheimer's brain is characterized by widespread cortical atrophy induced by dendritic tree shrinking and degeneration of the cholinergic axonal arborization. Microscopically, affected areas exhibit neurofibrillary tangles and amyloid-beta peptide deposits (senile plaques) [22, 23].
Additionally, AD is distinguished by neuroinflammation, triggered by the activation of astroglia and microglia [24].
In PD, the deposition and accumulation of α -synuclein, a presynaptic neuronal protein, drives its pathogenesis. The bioenergetic impairment, oxidative stress and anomalous protein regulation, are all linked to the aetiology of PD [24]. HD can be defined as the progressive loss of nerve cells in the stratum cerebral cortex and the selective neuronal dysfunction caused by various neuronal cell death mechanisms, including poor energy metabolism, apoptosis, oxidative stress, and excitotoxicity [25]. Microglia cells are activated macrophages in the brain which produce an array of pro-inflammatory cytokines in the presence of Htt [18].
ALS is catalyzed by a complex array of factors, including endoplasmic reticulum stress, inflammation, dysregulated endosomal trafficking, genetic susceptibility, oxidative stress, transcription and RNA processing, excitotoxicity, and mitochondrial dysfunction, and apoptosis [26]. A stroke causes an abrupt impairment of the function of the brain due to disruption in the cerebral blood supply. When the formation of plaques occurs along with the injured vessel, the intima is eroded, leading to the formation of thrombosis in intracranial arteries. According to studies, cerebral ischemia activates the NMDA receptor, resulting in the oxidation of vital cellular components and aggregation of ROS. Additionally, this alters signalling pathways, resulting in cellular damage and death [1]. Epilepsy's primary aetiology is currently an imbalance between inhibitory and excitatory neurotransmission, oxidative stress, and inflammation. Increased pro-inflammatory substances may result in the excessive loss of neuronal excitation, affecting GABA receptors. The neuronal excitability can be enhanced due to the alteration of calcium currents because of oxidative stress [27].
According to the literature available [21,22,23,24,25,26], it is clear that neuroinflammation, oxidative stress, and mitochondrial dysfunction has a major role in the pathophysiology of NDDs. Due to berberine’s antioxidant and neuroprotective properties [8,9,10,11,12,13,14], its metabolite, demethyleneberberine (DMB), could be utilized to decrease NDDs, as DMB is more effective than BBR at crossing the “blood–brain barrier” and employing its therapeutic effect.
Mechanistic approach of demethyleneberberine
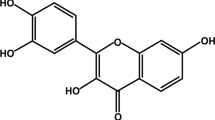
DMB (9,10-dimethoxy-5,6-dihydroisoquinolino [2,1-b] isoquinolin-7-ium-2,3-diol) is a novel cationic antioxidant having the molecular formula C 19H 18 NO 4+. DMB is one of berberine's primary metabolites and was found to be the crucial intermediate in the berberine alkaloids biogenesis [17]. DMB is known to have anti-oxidant [28], anti-inflammatory [29] and anti-fibrotic [30] properties which indicate that DMB may have therapeutic potential in neurogenerative disorders because the properties possessed by DMB have proven to be neuroprotective in NDDs.

The above flow chart indicates that the reduction of berberine leads to the formation of Columbamine, Dihydroberberine and Jatrorrhizine whereas demethylation of berberine results in the formation of Demethyleneberberine.
Demethyleneberberine as a potential anti-oxidant
Ageing and numerous brain disorders are thought to be regulated by oxidative stress. Oxidative stress occurs when the balance between the level of antioxidants and the formation of ROS is remarkably disrupted [31]. Through modulation of the function of biomolecules, ROS contributes to neurodegeneration development [32]. ROS can oxidize various substrates in cells, resulting in protein, DNA, RNA oxidation, and lipid peroxidation [33]. DMB contains two exposed phenolic hydroxyl groups, implying that it may possess antioxidative properties to combat the "second hit" (oxidative stress and inflammation), as previously demonstrated in studies that DMB reduced Alcoholic Liver Disease (ALD) via mitochondria-targeted antioxidative effects [28]. In chronic ethanol-fed mice, DMB inhibited iNOSs, CYP2E1, and HIF-1α, which resulted in oxidative stress and restored sirtuin 1/AMP activated protein kinase/PPARGC1A pathway-associated fatty acid oxidation ameliorated hepatic lipid peroxidation and macrosteatosis. According to the study, DMB treatment significantly reduced the oxidative damage caused by Non-Alcoholic Fatty Liver Disease (NAFLD), as measured by reducing the lipid oxidative product malonaldehyde (MDA) [34]. This demonstrated that DMB could alleviate oxidative stress and thus hepatitis caused by Con A. In another study, pre-treatment with DMB emerged to reduce MDA accumulation and increase serum Albumin and hepatic GSH levels [35]. As a result of these findings, it has been concluded that DMB possesses anti-oxidant properties.
Demethyleneberberine as an anti-fibrotic agent
The damaged neurons in the CNS can not regenerate and scar-forming cells like inflammatory immune cells, astrocytes, endothelial cells, and stromal fibroblasts can linger for a prolonged time in the brain. New evidence suggests that a fibrotic reaction is involved in persistent CNS injuries similar to those seen in neurodegenerative disorders, where fibrosis, as well as inflammation, promote deterioration. The essential pathogenic feature of fibrosis is the subsequent aggregation of proteins in the extracellular matrix (ECM) [36]. ECM and MMPs are essential moderators of neuroplasticity, cognition and may play a role in various neurological disorders [37]. In fibrotic tissue, Collagen type I is an extracellular matrix component, whereas serum hydroxyproline is an indicator of the metabolism and content of collagen (Fig. 2). During fibrogenesis, the interpretation of ECM proteases, for example, MMPs and TIMPs, rise. Additionally, the ECM contains growth factors, including TGF β-1, that modulate activation and proliferation. In thioacetamide (TAA)-induced hepatic fibrosis, qPCR and Immunohistochemical (IHC) analysis revealed that DMB inhibits collagen synthesis and increases collagen degradation by inhibiting TGF-1-Smad signalling, decreasing tissue inhibitors of MMP (TIMPs) and matrix metalloproteinases (MMPs) expression [30]. This suggests that DMB may be able to ameliorate hepatic fibrosis by inhibiting HSC activation. As a result, DMB can act as an anti-fibrotic agent.
Pictorial representation of Demethyleneberberine (DMB), a metabolite of Berberine showing three different properties, i.e., anti-oxidant, anti-inflammatory, and anti-fibrotic. HIF-1α hypoxia-inducible factor 1-alpha, CYP2E1 cytochrome P450 2E1, ROS reactive oxygen species, MDA malondialdehyde, GSH glutathione, TNF-α tumor necrosis factor alpha, IL-1 interleukin-1, IL-6 interleukin-6, INF-γ interferon gamma, iNOS inducible nitric oxide synthase, MMPs matrix metalloproteinases, TIMPs tissue inhibitors of metalloproteinases)
Demethyleneberberine as an anti-inflammatory agent
Inflammation is becoming more recognised as a key factor in neurodegenerative disorders. Microglia are known as the primary effectors in the central nervous system's inflammatory process and their activation leads to the increased expression of the cell surface antigens and discharge of pro-inflammatory cytokines, i.e., TNF-α, interleukin-6, interleukin-12, cyclooxygenase-2, and chemokines [38]. The formation of free radicals and excitotoxicity results in extensive brain damage leading to neuronal death occurs due to the release of pro-inflammatory cytokines [39]. In NDDs, where astrocytes and microglia are the primary inflammatory cells, therapeutic approaches aim to modulate the innate immune system's sensor/transducer/effector functions, i.e., TLRs, NF-κB, and TNF-α, respectively [40]. It was noted that, in the autoimmune hepatitis study, the expression and release of IFN-γ and TNF-α were significantly increased and were expectedly reversed in the DMB pre-treatment group. This study implicates that the expression of pro-inflammatory cytokines can be regulated by NF-κB signalling, leading to the pathogenesis of inflammatory liver diseases [35]. According to another study, DMB inhibited pro-inflammatory cytokine’s production, namely IL-6, TNF-α and decreased IFN-c levels in mice splenocytes in mice with inflammatory bowel disease [29]. These findings demonstrate that DMB can act as an anti-inflammatory agent (Table 1).
Molecular approach of demethyleneberberine in neurodegenerative disorders
Various studies have found that demethyleneberberine inhibits oxidative stress, neuroinflammation, mitochondrial dysfunctions, and ROS/RNS by showing its action on NF-κB, AMPK, and MAPK [28,29,30] and modulation of these pathways has shown neuroprotective function in neurodegenerative disorders. So, it has been hypothesized that DMB might have the potential to attenuate various neurodegenerative disorders via attenuating NFκB, AMPK, and MAPK signalling pathways in the brain. The role of berberine in the neuroprotection of various neurodegenerative disorders also indicates the possibility of DMB having the same potential as it is a metabolite of berberine (Table 2).
Demethyleneberberine in Alzheimer's disease
AD is correlated with ageing along with two neuropathological events, i.e., the deposition of amyloid plaques (Aβ) in extracellular space & intracellular neurofibrillary tangles (NFT) [46]. It is a multifactorial disease that develops due to the interaction of genetic and environmental factors. Neuroinflammation is linked to Alzheimer's disease over the last decade. Today, nearly all drug treatments for AD are ineffective. There is a critical need for therapies that can help prevent and slow down the progress of Alzheimer's disease [47]. The primary impediment to developing AD drugs is unclear regarding the mechanisms underlying AD pathogenesis and pathophysiology. Presently, there are no drugs available that modify AD. As a result, neuroinflammation has been put forward as an alternative therapeutic target for preventing and treating AD [48]. Since berberine has shown therapeutic potential in various mice and rabbit models of Alzheimer's disease [41], it becomes possible that the metabolite of berberine; DMB can also have therapeutic potential. Given that the transcription factor NF-κB is required to express many pro-inflammatory cytokines. According to the literature, brain-permeable inhibitors of NF-κB signalling may be used to slow the progression of AD. Microglia, the brain's resident macrophages, stimulate the NF-κB signalling [49]. NF-κB performs as a transcription factor for various chemokines and cytokines, including interleukins, tumour necrosis factors, interferons, and lymphokines [50]. According to a study, DMB inhibited the NF-κB and MAPK signalling activation in con-A-induced autoimmune hepatitis, indicating the use of DMB in the treatment of autoimmune hepatitis [35]. DMB also alleviated colitis and inhibited inflammatory responses in mice in an in vivo study via inhibiting the NF-κB pathway [29]. In another study, DMB inhibited the NF-κB signalling in mice with thioacetamide (TAA)-induced hepatic fibrosis [30]. So, it can be proposed that in AD, DMB could be used as a neuroprotective agent as DMB has been proven to inhibit the NF-κB signalling, which contributes to neuroinflammation in AD. Numerous proteins have been recognized as possible targets for treating Alzheimer's disease. The p38 MAPK signalling has been considerably reviewed in recent years; extensive research into the pathophysiology of AD has revealed novel roles for p38 MAPK in the process of memory loss and cognitive decline [51, 52]. Evidence states that DMB inhibited MAPK signalling [35], so it can be suggested that DMB may play a significant role in reversing memory loss and cognitive decline associated with AD (Fig. 3). There is mounting evidence that AMP-activated protein kinase (AMPK) may have a wide range of neuroprotective effects in neurodegenerative disorders. According to the available literature on AMPK for AD, activation of AMPK is beneficial in autophagy, insulin resistance, mitochondrial quality control, and oxidative stress relief. It had been demonstrated that AMPK might become a novel target for AD by treating the risk factors [53]. According to a study, by decreasing oxidative stress and inflammation, DMB can be used as an AMPK stimulator to treat non-alcoholic fatty liver disease and to prevent the pathologic progression of non-alcoholic fatty liver disease to non-alcoholic steatohepatitis [34]. Thus, this shows that DMB may exert neuroprotective effects in AD by acute activation of AMPK signalling, leading to downregulation of neuroinflammation and oxidative stress.
Demethyleneberbernine in Parkinson's disease
PD is a neurodegenerative condition distinguished by tenacious and selective loss of dopaminergic nerve cells in the substantia nigra, which add to the disease's cardinal motor symptoms: resting tremor, stiffness, and bradykinesia, along with dopaminergic neuropathology, cholinergic, serotonergic, glutamatergic, and nor-adrenergic pathways are malfunctioning [54]. Additionally, individuals with Parkinson's disease exhibit non-motor symptoms such as sleep problems, tiredness, and cognitive abnormalities. PD is a diverse disease that can proceed fast or slowly [55]. Pharmacologic treatments usually with levodopa formulations provided with or without other drugs and non-pharmacological methods, i.e., exercise, physical, occupational, and speech therapies, are utilized to treat the condition. Patients with drug-resistant tremors, dyskinesias, and worsening symptoms as the medicine wear off may benefit from treatment with levodopa-carbidopa enteral suspension and other approaches such as deep brain stimulation [56]. Since, berberine enhanced motor balance as well as coordination in PD by preventing dopaminergic neuronal loss in mice [9], indicating the possibility of the same effect by DMB. Among the numerous factors affecting the prognosis of PD, the importance of PI3K/AKT and p38 MAPK signalling in PD brains is captious because an imbalance between anti-apoptotic and pro-apoptotic pathways results in undesirable constellations such as microglial activation, oxidative stress, neuroinflammation, and apoptosis [57]. In the A53T model of α-synuclein, downregulation of p38 MAPK or overexpressing its kinase death variant lowers DRP1-mediated mitochondrial fission and restores mitochondrial dysfunction and cell death. Inhibiting the p38 MAPK-DRP1 signalling might be an essential therapeutic method for Parkinson's disease that maintains mitochondrial homeostasis [58]. As many studies revealed that DMB inhibits MAPK signalling [35], it can be further explored that DMB may serve a neuroprotective function in reducing PD symptoms via suppressing MAPK signalling. NF-κB, a well-characterized pro-death signalling pathway in response to oxidative stress, appears to be involved in the death of dopaminergic nerve cells in PD models [59]. The increased levels of NF-κB, interferon, and p53 in PD patients' nigrostriatal dopaminergic areas suggest an increase in immunological reactivity and programmed cell death of nerve cells [24]. NBD peptide enters the CNS in the MPTP model of Parkinson's disease, inhibits NF-κB signalling activation in the SNpc, and proinflammatory molecules' expression, glial cell activation in the midbrain, protects against dopaminergic neuron loss, and improves behavioural functions [60]. Since DMB is involved in the suppression of NF-κB [29], it can be supposed that DMB could be utilized to treat Parkinson's disease as a neuroprotective drug. AMPK regulates various physiological systems which can provide neuroprotection in PD, including energy balance, macro-autophagy, inflammation, antioxidant defences, and mitochondrial quality control. The degradation of particularly DA neurons and the subsequent motor-behavioural deficits associated with PD can be mimicked in experimental systems by administering dopaminergic poisons or expressing PD-related genetic abnormalities [61]. Since DMB promotes AMPK signalling [34], it may contribute to neuroprotection in PD via modulating AMPK signalling. Inhibitors of MAO-B are used to ameliorate symptoms of PD because they boost the level of synaptic dopamine by preventing the breakdown of the same. MAO-B inhibitors have a well-established role in Parkinson's disease patients as monotherapy or as adjuncts to levodopa. They are highly tolerated and uncomplicated to administer, making them ideal to commence therapy in eligible individuals [62]. DMB reversibly inhibited the MAO-B enzyme activity [63]; it has been hypothesized that DMB could be used to ameliorate PD symptoms.
Demethyleneberberine in Huntington's disease (HD)
HD is distinguished by motor, cognitive and behavioural manifestations. It occurs due to the expansion of a trinucleotide repeat on chromosome 4, specifically in the huntingtin gene (HTT) [64]. Although motor signs are currently used to define disease onset clinically, the presence of non-motor symptoms before motor diagnosis is becoming increasingly recognized. Complex multi-modal indications have a harmful effect on a patient’s quality of life and longevity. Interdisciplinary symptomatic care delivered thoughtfully can have a significant positive impact on patients and families [65]. There are currently a variety of symptomatic treatments available, and new symptomatic and potentially disease-modifying therapies are being developed aggressively. HD is an appealing model for developing therapies capable of delaying or even halting the progression of neurodegenerative diseases. Tetrabenazine and deutetrabenazine are the only treatment options for this patient population with a formal indication (chorea) [66]. Berberine has also shown therapeutic potential in the transgenic mice model of HD [10] which means DMB might also have the same effect in HD as it is a metabolite of BBR. In numerous HD models, stimulation of the p38 MAPK and JNK pathways results in neural toxicity. In a 3-NP-treated HD mouse model, Rg1 was found to exert neuroprotective effects by suppressing the activation of MAPK and NF-κΒ signalling pathways in the striatum [67]. Since multiple studies have established DMB to be a MAPK signalling inhibitor [35], it can be assumed that DMB may act as a neuroprotective agent in HD. In the striatum, the NF-κΒ cascade is activated in a variety of HD models. Studies in rodent models suggest a strong connection between neurodegeneration and NF-κΒ. 3NP induces nuclear translocation of NF-κΒ as well as nNOS and iNOS expression in Huntington's Disease, and that inhibition of NF-κΒ transcriptional activity blocks 3NP-induced NOS expression [67]. Since DMB inhibits NF-κΒ signalling [29], it may prove to be a neuroprotective agent by inhibiting NF-kB signalling. In cell and animal models of HD, the initiation of autophagy has been proven to be therapeutic. However, inducing autophagy through its primary regulator, i.e., mTOR, may have unintended consequences. According to a study, AMPK was recognized as a target for “mTOR-independent autophagy” enhancement in HD [68]. Since DMB activates AMPK signalling [34], which further initiates autophagy, it has given an idea of DMB’s neuroprotective effect in HD by inducing autophagy.
Demethyleneberberine in amyotrophic lateral sclerosis (ALS)
ALS typically manifests in adulthood and is distincted by the selective death of cortical motor, bulbar and spinal nerve cells, resulting in early death and progressive paralysis, typically occurring some years after diagnosis. It is almost always fatal within a few years of symptom onset [69]. Besides riluzole supportive care, a putative glutamate release inhibitor is associated with modestly prolonged survival [70]. In the cellular model of ALS, berberine deregulated the mTOR/p70S6K signal and activation in the autophagic degradation pathway [43], suggesting the therapeutic potential of BBR in NDDs.Numerous MAPK inhibitors have also been assessed in pre-clinical and clinical studies for NDDs treatment. Despite encouraging results in some preclinical models, the MAPK pathway is essential for proliferation and cell survival, proliferation is a major concern. Several tested inhibitors of the MAPK pathway have significant side effects but this does not preclude MAPK members from being therapeutic targets, as several of these members exhibit cell-specific expression [71]. Since DMB inhibits MAPK [35], it may be used to slow the progression of Amyotrophic lateral sclerosis. In mice models, the novel molecular mechanism underlying motor neuron death in ALS is the downregulation of NF-κΒ activation in microglia with IGF-1 [72]. As DMB inhibits NF-κB signalling [29] so it can be used as a neuroprotective agent in ALS. The continuous activation of AMPK can be harmful in ALS to extremely stressed neurons. Thence, pre-conditioning with AMPK activating molecules can serve as a novel strategy for developing ALS. The latrepirdine preconditioning can delay the progression of ALS in SOD1G93A mice via activating AMPK signalling [34]. Since DMB is involved in activating AMPK signalling, it can be said that DMB may provide neuroprotection in ALS via acute activation of AMPK [73].
Demethyleneberberine in stroke
Stroke is ranked third as the cause of disability & death across the globe; it is undergoing a paradigm shift due to the disclosure of new concepts related to neurodegeneration [74]. Stroke as a blood vessel problem has been enlarged to incorporate the adverse consequences of an interaction involving neurons, glia, matrix components, and vascular cells. Secondary neuroinflammation occurs after an acute stroke, and most strokes are ischemic, which elevates additional injury and supports recovery [31]. The penetration of inflammatory cells, i.e., macrophages, neutrophils, countless T cell subtypes, and others into the ischemic region, aggravating brain injury is influenced by rapid activation of the resident cells by the pro-inflammatory signals from immune mediators [74]. The treatment of berberine ameliorated apoptosis induced by ischemia, and inhibited reactive astrogliosis and microglial activation in the gerbils model [44], suggesting the possibility of DMB having the same effect. IVIg therapy downregulated the MAPK and NF-κΒ signalling, consequently suppressing the activation & NLRP1 of the NLRP3 inflammasome in the primary cortical nerve cells during an ischemic episode. As a result of these findings, treatments that precisely target inflammasome activation in nerve cells may pave the way for future stroke treatment [75]. The use of a non-invasive molecular imaging technique in regulating the p38 MAPK signalling pathway can modulate MMP activity following stroke, elucidating a new mechanism of post-ischemic brain injury and circumventing the limitations of conventional MMP inhibitor therapy [76]. In a mouse stroke model, UTI guarded the brain in an ischemic episode due to its ability to alleviate inflammation in the early stages of the disease by downregulating TLR4 & NF-κΒ signalling expression [77]. DMB has been demonstrated to suppress NF-κΒ and MAPK signalling, implying that it may also act as a neuroprotective agent in stroke. Apelin 13 protected ischemia reperfusion-induced ROS mediated inflammation and oxidative stress in vivo by activating the AMPK/GSK-3 and AR/G/PLC/IP3/CaMKK signalling, further upregulating Nrf2-regulated antioxidant enzyme production [78]. As DMB activates AMPK signalling, it can be stated that its activation by DMB in stroke may play a significant role in alleviating stroke. This needs to be confirmed by further preclinical studies.
Demethyleneberberine in epilepsy
Epilepsy is frequently accompanied by various pathological and neurodegenerative changes in the brain regions responsible for repetitive seizures. The changes include nerve cell loss and a rise in the size and number of astrocytes, additionally, they may also involve increased permeability of the blood–brain barrier, axonal sprouting, new capillaries, and central inflammation [79]. BBR has shown protection in various epilepsy models i.e., NMDA induced mice model, Kainic acid-induced mice model, Maximal electroshock mice model, and PTZ mice model [45], indicating the possibility of DMB having the same effect. Seizures trigger central nervous system inflammation, and NF-κB, chemokines, cytokines, cell adhesion molecules, and inflammatory molecules are expressed in the rodent brain [80]. Ghrelin decreases inflammation in cortical neurons during an epileptic seizure, which may help prevent necrosis and nerve cell death, preserving the cortex's normal function. Ghrelin may ease the cortex's inflammatory response by regulating TNF‑α and NF‑κB levels, reducing child epilepsy attacks frequently. These findings suggest that DMB can attenuate neuroinflammation in epilepsy via inhibiting NF‑κB. AMPK has a role in epileptic seizures; for instance, time-restricted feeding increased AMPK phosphorylation and had an anticonvulsant effect in the model of status epilepticus. It was also observed that in the brain of acute and chronic seizures animals, the AMPK expression was decreased [81]. DMB activates AMPK [34]; DMB can show an anticonvulsant effect in epilepsy via activation of AMPK. SB203580 treatment significantly lowered the Racine scores and length of the initial seizure in rats. This result is the same as another study, which demonstrated that SB203580 considerably lowered the intensity and duration of seizures in a rat model of refractory epilepsy [82,83,84]. As DMB inhibits MAPK [35], it can be said that DMB can reduce the intensity of seizures via modulating MAPK signalling.
Conclusion
Innumerable medications have been used in the past to treat NDDs, but they lack the efficacy necessary to slow disease progression and instead create a host of harmful effects. In this light, plant-based medications have also evolved as a form of innovation. The diverse range of natural alkaloids continues to treat a variety NDDs effectively. We have discussed the neuroprotective properties of DMB, in a variety of neurodegenerative diseases in this review. Since DMB has been demonstrated to influence NF-κΒ, MAPK, and AMPK signalling in various disorders, it is evident that modulating these signalling pathways is crucial in NDDs. Thus, in this review, various ideas for future directions have been provided via correlating DMB and its modulation by NF-κΒ, MAPK, and AMPK signalling. As a result, DMB could show neuroprotective effects in various NDDS. There is very little availability of studies demonstrating DMB’s role in NDDs. More scientific studies should be done in future to explore and evaluate the therapeutic potential of DMB in NDDs.
Abbreviations
- DMB:
-
Demethyleneberberine
- BBR:
-
Berberine
- NDDs:
-
Neurodegenerative disorders
- CNS:
-
Central nervous system
- ROS:
-
Reactive oxygen species
- Ca2+ :
-
Calcium
- Htt:
-
Huntingtin
- NAFLD:
-
Non-Alcoholic Fatty Liver Disease
- ALD:
-
Alcohol liver disease
- MDA:
-
Malonaldehyde
- GSH:
-
Glutathione
- ECM:
-
Extracellular matrix
- MMPs:
-
Matrix metalloproteinases
- TIMPS:
-
Tissue inhibitors of metalloproteinases
- TGF-1:
-
Transforming growth factor-1
- CYP2E1:
-
Cytochrome P450 2E1
- HIF-1α:
-
Hypoxia-inducible factor 1-alpha
- iNOS:
-
Inducible nitric oxide synthase
- qPCR:
-
Quantitative polymerase chain reaction
- IHC:
-
Immunohistochemical
- TNF-α:
-
Tumour necrosis factor-alpha
- CO:
-
Cyclooxygenase
- IL:
-
Interleukin
- iNOS:
-
Inducible nitric oxide synthase
- NFT:
-
Neurofibrillary tangles
- TAA:
-
Thioacetamide
- MAPK:
-
Mitogen-activated protein kinase
- AMPK:
-
AMP-activated protein kinase
- MAO-B:
-
Monoamine oxidase-B
- UTI:
-
Ulinastatin
- CYP2E1:
-
Cytochrome P450 2E1
- MDA:
-
Malondialdehyde
- INF-γ:
-
Interferon-gamma
References
Tiwari P, Khan H, Singh TG, Grewal AK (2022) Poly (ADP-ribose) polymerase: an overview of mechanistic approaches and therapeutic opportunities in the management of stroke. Neurochem Res 18:1–23. https://doi.org/10.1007/s11064-022-03595-z
Khan H, Garg N, Singh TG, Kaur A, Thapa K (2022) Calpain inhibitors as potential therapeutic modulators in neurodegenerative diseases. Neurochem Res 4:1–25. https://doi.org/10.1007/s11064-021-03521-9
Sun AY, Wang Q, Simonyi A, Sun GY (2008) Botanical phenolics and brain health. Neuromol Med 10:259–274. https://doi.org/10.1007/s12017-008-8052-z
Hussain G, Rasul A, Anwar H, Aziz N, Razzaq A, Wei W, Ali M, Li J, Li X (2018) Role of plant derived alkaloids and their mechanism in neurodegenerative disorders. Int J Biol Sci 14:341. https://doi.org/10.7150/ijbs.23247
Strain JJ, Karim A, Caliendo G, Brodsky M, Lowe RS III, Himelein C (2003) Neurologic drug–psychotropic drug update. Dis Mon 49:326–371. https://doi.org/10.1067/mda.2003.25
Egbuna C, Mishra AP, Goyal MR (2020) Preparation of phytopharmaceuticals for the management of disorders: the development of nutraceuticals and traditional medicine. Academic Press, Cambridge
Schmitt F, Hussain G, Dupuis L, Loeffler JP, Henriques A (2014) A plural role for lipids in motor neuron diseases: energy, signaling and structure. Front Cell Neurosci 20(8):25. https://doi.org/10.3389/fncel.2014.00025
Akbar M, Shabbir A, Rehman K, Akash MS, Shah MA (2021) Neuroprotective potential of berberine in modulating Alzheimer’s disease via multiple signaling pathways. J Food Biochem 10:e13936. https://doi.org/10.1111/jfbc.13936
Kim M, Cho KH, Shin MS, Lee JM, Cho HS, Kim CJ, Shin DH, Yang HJ (2014) Berberine prevents nigrostriatal dopaminergic neuronal loss and suppresses hippocampal apoptosis in mice with Parkinson’s disease. Int J Mol Med 33:870–878. https://doi.org/10.3892/ijmm.2014.1656
Jiang W, Wei W, Gaertig MA, Li S, Li XJ (2015) Therapeutic effect of berberine on Huntington’s disease transgenic mouse model. PLoS ONE 10:e0134142. https://doi.org/10.1371/journal.pone.0134142
Liu YJ, Ju TC, Chen HM, Jang YS, Lee LM, Lai HL, Tai HC, Fang JM, Lin YL, Tu PH, Chern Y (2015) Activation of AMP-activated protein kinase α1 mediates mislocalization of TDP-43 in amyotrophic lateral sclerosis. Hum Mol Genet 24:787–801. https://doi.org/10.1093/hmg/ddu497
Hong JS, Chu YK, Lee H, Ahn BH, Park JH, Kim MJ, Lee S, Ryoo HS, Jang JH, Lee SR, Park JW (2012) Effects of berberine on hippocampal neuronal damage and matrix metalloproteinase-9 activity following transient global cerebral ischemia. J Neurosci Res 90:489–497. https://doi.org/10.1002/jnr.22756
Gao F, Gao Y, Liu YF, Wang L, Li YJ (2014) Berberine exerts an anticonvulsant effect and ameliorates memory impairment and oxidative stress in a pilocarpine-induced epilepsy model in the rat. Neuropsychiatr Dis Treat 10:2139. 10.2147%2FNDT.S73210
Pirillo A, Catapano AL (2015) Berberine, a plant alkaloid with lipid-and glucose-lowering properties: from in vitro evidence to clinical studies. Atherosclerosis 243:449–461. https://doi.org/10.1016/j.atherosclerosis.2015.09.032
Jiang W, Wei W, Gaertig MA, Li S, Li XJ (2015) Therapeutic effect of berberine on Huntington’s disease transgenic mouse model. PLoS ONE 30(10):e0134142. https://doi.org/10.1371/journal.pone.0134142
Wang J, Jiang Y, Wang B, Zhang N (2019) A review on analytical methods for natural berberine alkaloids. J Sep Sci 42:1794–1815. https://doi.org/10.1002/jssc.201800952
Gupta S, Khan A, Vishwas S, Gulati M, Singh TG, Dua K, Singh SK, Najda A, Sayed AA, Almeer R, Abdel-Daim MM (2021) Demethyleneberberine: a possible treatment for Huntington’s disease. Med Hypotheses 1(153):110639. https://doi.org/10.1016/j.mehy.2021.110639
Chen WW, Zhang XI, Huang WJ (2016) Role of neuroinflammation in neurodegenerative diseases. Mol Med Rep 13:3391–3396. https://doi.org/10.3892/mmr.2016.4948
Guzman-Martinez L, Maccioni RB, Andrade V, Navarrete LP, Pastor MG, Ramos-Escobar N (2019) Neuroinflammation as a common feature of neurodegenerative disorders. Front Pharmacol 12(10):1008. https://doi.org/10.3389/fphar.2019.01008
Pievan M, Filippini N, Van Den Heuvel MP, Cappa SF, Frisoni GB (2014) Brain connectivity in neurodegenerative diseases—from phenotype to proteinopathy. Nat Rev Neurol 10(11):620–633. https://doi.org/10.1038/nrneurol.2014.178
Gil-Bea F, Akterin S, Persson T, Mateos L, Sandebring A, Avila-Cariño J, Gutierrez-Rodriguez A, Sundström E, Holmgren A, Winblad B, Cedazo-Minguez A (2012) Thioredoxin-80 is a product of alpha-secretase cleavage that inhibits amyloid-beta aggregation and is decreased in Alzheimer’s disease brain. EMBO Mol Med 4(10):1097–1111. https://doi.org/10.1002/emmm.201201462
Rosenblum WI (2014) Why Alzheimer trials fail: removing soluble oligomeric beta amyloid is essential, inconsistent, and difficult. Neurobiol Aging 1(35):969–974. https://doi.org/10.1016/j.neurobiolaging.2013.10.085
Mogi M, Kondo T, Mizuno Y, Nagatsu T (2007) p53 protein, interferon-γ, and NF-κB levels are elevated in the parkinsonian brain. Neurosci Lett 27(414):94–97. https://doi.org/10.1016/j.neulet.2006.12.003
Khan H, Singh TG, Dahiya RS, Abdel-Daim MM (2022) α-Lipoic acid, an organosulfur biomolecule a novel therapeutic agent for neurodegenerative disorders: an mechanistic perspective. Neurochem Res 21:1–2. https://doi.org/10.1007/s11064-022-03598-w
Khan H, Tiwari P, Kaur A, Singh TG (2021) Sirtuin acetylation and deacetylation: a complex paradigm in neurodegenerative disease. Mol Neurobiol 58(8):3903–3917. https://doi.org/10.1007/s12035-021-02387-w
Chen CC, Hung TH, Lee CY, Wang LF, Wu CH, Ke CH, Chen SF (2014) Berberine protects against neuronal damage via suppression of glia-mediated inflammation in traumatic brain injury. PLoS ONE 29(9):e115694. https://doi.org/10.1371/journal.pone.0115694
Zhang P, Qiang X, Zhang M, Ma D, Zhao Z, Zhou C, Liu X, Li R, Chen H, Zhang Y (2015) Demethyleneberberine, a natural mitochondria-targeted antioxidant, inhibits mitochondrial dysfunction, oxidative stress, and steatosis in alcoholic liver disease mouse model. J Pharmacol Exp 352(1):139–147. https://doi.org/10.1124/jpet.114.219832
Chen YY, Li RY, Shi MJ, Zhao YX, Yan Y, Xu XX, Zhang M, Zhao XT, Zhang YB (2017) Demethyleneberberine alleviates inflammatory bowel disease in mice through regulating NF-κB signaling and T-helper cell homeostasis. J Inflamm Res 66(2):187–196. https://doi.org/10.1007/s00011-016-1005-3
Wang Y, Zhao Z, Yan Y, Qiang X, Zhou C, Li R, Chen H, Zhang Y (2016) Demethyleneberberine protects against hepatic fibrosis in mice by modulating NF-κB signaling. Int J Mol Sci 17(7):1036. https://doi.org/10.3390/ijms17071036
Khan H, Kashyap A, Kaur A, Singh TG (2020) Pharmacological postconditioning: a molecular aspect in ischemic injury. J Pharm Pharmacol 72(11):1513–1527. https://doi.org/10.1111/jphp.13336
Gandhi S, Abramov AY (2012) Mechanism of oxidative stress in neurodegeneration. Oxid Med Cell Longev. https://doi.org/10.1155/2012/428010
Khan H, Singh A, Thapa K, Garg N, Grewal AK, Singh TG (2021) Therapeutic modulation of the phosphatidylinositol 3-kinases (PI3K) pathway in cerebral ischemic injury. Brain Res 15(1761):147399. https://doi.org/10.1016/j.brainres.2021.147399
Qiang X, Xu L, Zhang M, Zhang P, Wang Y, Wang Y, Zhao Z, Chen H, Liu X, Zhang Y (2016) Demethyleneberberine attenuates non-alcoholic fatty liver disease with activation of AMPK and inhibition of oxidative stress. Biochem Biophys Res Commun 472(4):603–609. https://doi.org/10.1016/j.bbrc.2016.03.019
Zhang M, Li Q, Zhou C, Zhao Y, Li R, Zhang Y (2020) Demethyleneberberine attenuates concanavalin A-induced autoimmune hepatitis in mice through inhibition of NF-κB and MAPK signaling. Int Immunopharmacol 1(80):106137. https://doi.org/10.1016/j.intimp.2019.106137
Raghu G, Striker LJ, Hudson LD, Striker GE (1985) Extracellular matrix in normal and fibrotic human lungs. Am Rev Respir Dis 131(2):281–289. https://doi.org/10.1164/arrd.1985.131.2.281
Hemmann S, Graf J, Roderfeld M, Roeb E (2007) Expression of MMPs and TIMPs in liver fibrosis–a systematic review with special emphasis on anti-fibrotic strategies. J Hepatol 46(5):955–975. https://doi.org/10.1016/j.jhep.2007.02.003
Morawski M, Filippov M, Tzinia A, Tsilibary E, Vargova L (2014) ECM in brain aging and dementia. Prog Brain Res 214:207–227. https://doi.org/10.1016/B978-0-444-63486-3.00010-4
Xu L, He D, Bai Y (2016) Microglia-mediated inflammation and neurodegenerative disease. Mol Neurobiol 53(10):6709–6715. https://doi.org/10.1007/s12035-015-9593-4
Glass CK, Saijo K, Winner B, Marchetto MC, Gage FH (2010) Mechanisms underlying inflammation in neurodegeneration. Cell 140(6):918–934. https://doi.org/10.1016/j.cell.2010.02.016
Durairajan SS, Liu LF, Lu JH, Chen LL, Yuan Q, Chung SK, Huang L, Li XS, Huang JD, Li M (2012) Berberine ameliorates β-amyloid pathology, gliosis, and cognitive impairment in an Alzheimer’s disease transgenic mouse model. Neurobiol Aging 33:2903–2919. https://doi.org/10.1016/j.neurobiolaging.2012.02.016
Panahi N, Mahmoudian M, Mortazavi P, Hashjin GS (2013) Effects of berberine on β-secretase activity in a rabbit model of Alzheimer's disease. Arch Med Sci 9:146. 10.5114%2Faoms.2013.33354
Palomo V, Tosat-Bitrian C, Nozal V, Nagaraj S, Martin-Requero A, Martinez A (2019) TDP-43: a key therapeutic target beyond amyotrophic lateral sclerosis. ACS Chem Neurosci 10:1183–1196. https://doi.org/10.1021/acschemneuro.9b00026
Kim M, Shin MS, Lee JM, Cho HS, Kim CJ, Kim YJ, Choi HR, Jeon JW (2014) Inhibitory effects of isoquinoline alkaloid berberine on ischemia-induced apoptosis via activation of phosphoinositide 3-kinase/protein kinase B signaling pathway. Int Neurourol J 18:115. 10.5213%2Finj.2014.18.3.115
Bhutada P, Mundhada Y, Bansod K, Dixit P, Umathe S, Mundhada D (2010) Anticonvulsant activity of berberine, an isoquinoline alkaloid in mice. Epilepsy Behav 18:207–210. https://doi.org/10.1016/j.yebeh.2010.03.007
Zhang Y, Liu D, Yao X, Zhang Y (2021) DMTHB ameliorates memory impairment in Alzheimer's disease mice through inhibition of IL-16 signaling. https://doi.org/10.21203/rs.3.rs-882646/v1
Sharma VK, Mehta V, Singh TG (2020) Alzheimer’s disorder: epigenetic connection and associated risk factors. Curr Neuropharmacol 18(8):740–753. https://doi.org/10.2174/1570159X18666200128125641
Sharma VK, Singh TG (2020) CREB: a multifaceted target for Alzheimer’s disease. Curr Alzheimer Res 17(14):1280–1293. https://doi.org/10.2174/1567205018666210218152253
Karunaweera N, Raju R, Gyengesi E, Münch G (2015) Plant polyphenols as inhibitors of NF-κB induced cytokine production—a potential anti-inflammatory treatment for Alzheimer’s disease? Front Mol Neurosci 16(8):24. https://doi.org/10.3389/fnmol.2015.00024
Escarcega RO, Fuentes-Alexandro S, Garcia-Carrasco M, Gatica A, Zamora A (2007) The transcription factor nuclear factor-kappa B and cancer. Clin Oncol 19(2):154–161. https://doi.org/10.1016/j.clon.2006.11.013
Figuera-Losada M, Rojas C, Slusher BS (2014) Inhibition of microglia activation as a phenotypic assay in early drug discovery. J Biomol Screen 19(1):17–31. https://doi.org/10.1177/1087057113499406
Munoz L, Ammit AJ (2010) Targeting p38 MAPK pathway for the treatment of Alzheimer’s disease. Neuropharmacology 58(3):561–568. https://doi.org/10.1016/j.neuropharm.2009.11.010
Yang L, Jiang Y, Shi L, Zhong D, Li Y, Li J, Jin R (2020) AMPK: Potential therapeutic target for Alzheimer’s disease. Curr Protein Pept Sci 21(1):66–77. https://doi.org/10.2174/1389203720666190819142746
Sharma T, Kaur D, Grewal AK, Singh TG (2021) Therapies modulating insulin resistance in Parkinson’s disease: a cross talk. Neurosci Lett 18:135754. https://doi.org/10.1016/j.neulet.2021.135754
Charvin D, Medori R, Hauser RA, Rascol O (2018) Therapeutic strategies for Parkinson disease: beyond dopaminergic drugs. Nat Rev Drug Discov 17(11):804–822. https://doi.org/10.1038/nrd.2018.136
Armstrong MJ, Okun MS (2020) Diagnosis and treatment of Parkinson disease: a review. JAMA 323(6):548–560. https://doi.org/10.1001/jama.2019.22360
Jha SK, Jha NK, Kar R, Ambasta RK, Kumar P (2015) p38 MAPK and PI3K/AKT signalling cascades in Parkinson’s disease. Int J Mol Cell Med 4(2):67
Gui C, Ren Y, Chen J, Wu X, Mao K, Li H, Yu H, Zou F, Li W (2020) p38 MAPK-DRP1 signaling is involved in mitochondrial dysfunction and cell death in mutant A53T α-synuclein model of Parkinson’s disease. Toxicol Appl Pharmacol 1(388):114874. https://doi.org/10.1016/j.taap.2019.114874
Tobón-Velasco JC, Limón-Pacheco JH, Orozco-Ibarra M, Macías-Silva M, Vázquez-Victorio G, Cuevas E, Ali SF, Cuadrado A, Pedraza-Chaverrí J, Santamaría A (2013) RETRACTED: 6-OHDA-induced apoptosis and mitochondrial dysfunction are mediated by early modulation of intracellular signals and interaction of Nrf2 and NF-κB factors. Toxicology. https://doi.org/10.1016/j.tox.2012.12.011
Ghosh A, Roy A, Liu X, Kordower JH, Mufson EJ, Hartley DM, Ghosh S, Mosley RL, Gendelman HE, Pahan K (2007) Selective inhibition of NF-κB activation prevents dopaminergic neuronal loss in a mouse model of Parkinson’s disease. Proc Natl Acad Sci 104(47):18754–18759. https://doi.org/10.1073/pnas.0704908104
Curry DW, Stutz B, Andrews ZB, Elsworth JD (2018) Targeting AMPK signaling as a neuroprotective strategy in Parkinson’s disease. J Parkinsons Dis 8(2):161–181. https://doi.org/10.3233/JPD-171296
Schapira AH (2011) Monoamine oxidase B inhibitors for the treatment of Parkinson’s disease. CNS Drugs 25(12):1061–1071. https://doi.org/10.2165/11596310-000000000-00000
Tao C, Hu SQ, Chen J, Chen YJ, Sun KH, Cui GZ, Ma M, Wu ZZ (2020) Highly efficient synthesis and monoamine oxidase B inhibitory profile of demethyleneberberine, columbamine and palmatine. Neurochem Int 139:104807. https://doi.org/10.1016/j.neuint.2020.104807
Testa CM, Jankovic J (2019) Huntington disease: a quarter century of progress since the gene discovery. J Neurol Sci 15(396):52–68. https://doi.org/10.1016/j.jns.2018.09.022
Mestre TA (2019) Recent advances in the therapeutic development for Huntington disease. Parkinsonism Relat Disord 59:125–130. https://doi.org/10.1016/j.parkreldis.2018.12.003
Yang X, Chu SF, Wang ZZ, Li FF, Yuan YH, Chen NH (2021) Ginsenoside Rg1 exerts neuroprotective effects in 3-nitropronpionic acid-induced mouse model of Huntington’s disease via suppressing MAPKs and NF-κB pathways in the striatum. Acta Pharmacol Sin 49:1409–1421. https://doi.org/10.1016/j.neulet.2007.09.056
Napolitano M, Zei D, Centonze D, Palermo R, Bernardi G, Vacca A, Calabresi P, Gulino A (2008) NF-kB/NOS cross-talk induced by mitochondrial complex II inhibition: implications for Huntington’s disease. Neurosci Lett 434:241–246. https://doi.org/10.1016/j.neulet.2007.09.056
Walter C, Clemens LE, Müller AJ, Fallier-Becker P, Proikas-Cezanne T, Riess O, Metzger S, Nguyen HP (2016) Activation of AMPK-induced autophagy ameliorates Huntington disease pathology in vitro. Neuropharmacology 108:24–38. https://doi.org/10.1016/j.neuropharm.2016.04.041
Arti AK, Singh M, Arora S, Dhiman S, Satija S, Singh TG (2019) Pharmacotherapy of amyotrophic lateral sclerosis: an insight. Plant Arch 19:1385–1397
Bucchia M, Ramirez A, Parente V, Simone C, Nizzardo M, Magri F, Dametti S, Corti S (2015) Therapeutic development in amyotrophic lateral sclerosis. Clin Ther 37:668–680. https://doi.org/10.1016/j.clinthera.2014.12.020
Sahana TG, Zhang K (2021) Mitogen-activated protein kinase pathway in amyotrophic lateral sclerosis. Biomedicines 9:969. https://doi.org/10.3390/biomedicines9080969
Hu H, Lin H, Duan W, Cui C, Li Z, Liu Y, Wang W, Wen D, Wang Y, Li C (2018) Intrathecal Injection of scAAV9–hIGF1 prolongs the survival of ALS model mice by inhibiting the NF-kB pathway. Neuroscience 381:1–10. https://doi.org/10.1016/j.neuroscience.2018.02.004
Coughlan KS, Mitchem MR, Hogg MC, Prehn JH (2015) “Preconditioning” with latrepirdine, an adenosine 5′-monophosphate-activated protein kinase activator, delays amyotrophic lateral sclerosis progression in SOD1G93A mice. Neurobiol Aging 36:1140–1150. https://doi.org/10.1016/j.neurobiolaging.2014.09.022
Jayaraj RL, Azimullah S, Beiram R, Jalal FY, Rosenberg GA (2019) Neuroinflammation: friend and foe for ischemic stroke. J Neuroinflammation 16:1–24. https://doi.org/10.1186/s12974-019-1516-2
Fann DY, Lim YA, Cheng YL, Lok KZ, Chunduri P, Baik SH, Drummond GR, Dheen ST, Sobey CG, Jo DG, Chen CL (2018) Evidence that NF-κB and MAPK signaling promotes NLRP inflammasome activation in neurons following ischemic stroke. Mol Neurobiol 55:1082–1096. https://doi.org/10.1007/s12035-017-0394-9
Chang D, Wang YC, Bai YY, Lu CQ, Xu TT, Zhu L, Ju S (2015) Role of P38 MAPK on MMP activity in photothrombotic stroke mice as measured using an ultrafast MMP activatable probe. Sci Rep 5:1–11. https://doi.org/10.1038/srep16951
Li X, Su L, Zhang X, Zhang C, Wang L, Li Y, Zhang Y, He T, Zhu X, Cui L (2017) Ulinastatin downregulates TLR4 and NF-kB expression and protects mouse brains against ischemia/reperfusion injury. Neurol Res 39:367–373. https://doi.org/10.1080/01616412.2017.1286541
Duan J, Cui J, Yang Z, Guo C, Cao J, Xi M, Weng Y, Yin Y, Wang Y, Wei G, Qiao B (2019) Neuroprotective effect of Apelin 13 on ischemic stroke by activating AMPK/GSK-3β/Nrf2 signaling. J Neuroinflammation 16:1–16. https://doi.org/10.1080/01616412.2017.1286541
Farrell JS, Wolff MD, Teskey GC (2017) Neurodegeneration and pathology in epilepsy: clinical and basic perspectives. J Neurodegener Dis. https://doi.org/10.1007/978-3-319-57193-5_12
De Simoni MG, Perego C, Ravizza T, Moneta D, Conti M, Marchesi F, De Luigi A, Garattini S, Vezzani A (2000) Inflammatory cytokines and related genes are induced in the rat hippocampus by limbic status epilepticus. Eur J Neurosci 12:2623–2633. https://doi.org/10.1046/j.1460-9568.2000.00140.x
Landgrave-Gómez J, Mercado-Gómez OF, Vázquez-García M, Rodríguez-Molina V, Córdova-Dávalos L, Arriaga-Ávila V, Miranda-Martínez A, Guevara-Guzmán R (2004) Anticonvulsant effect of time-restricted feeding in a pilocarpine-induced seizure model: metabolic and epigenetic implications. Front Cell Neurosci 10:7. https://doi.org/10.3389/fncel.2016.00007
Shao Y, Wang C, Hong Z, Chen Y (2016) Inhibition of p38 mitogen-activated protein kinase signaling reduces multidrug transporter activity and anti-epileptic drug resistance in refractory epileptic rats. J Neurochem 136:1096–1105. https://doi.org/10.1111/jnc.13498
Bulavin DV, Phillips C, Nannenga B, Timofeev O, Donehower LA, Anderson CW, Appella E, Fornace AJ (2004) Inactivation of the Wip1 phosphatase inhibits mammary tumorigenesis through p38 MAPK–mediated activation of the p16 Ink4a-p19 Arf pathway. Nat Genet 36:343–350. https://doi.org/10.1038/ng1317
Singh S, Singh TG, Rehni AK, Sharma V, Singh M, Kaur R (2021) Reviving mitochondrial bioenergetics: a relevant approach in epilepsy. Mitochondrion 58:213–226. https://doi.org/10.1016/j.mito.2021.03.009
Singh S, Singh TG, Rehni AK (2020) An insight into molecular mechanisms and novel therapeutic approaches in epileptogenesis. CNS Neurol Disord Drug Targets 19:750–779. https://doi.org/10.2174/1871527319666200910153827
Acknowledgements
The authors are grateful to the Chitkara College of Pharmacy, Chitkara University, Rajpura, Patiala, Punjab, India for providing the necessary facilities to carry out the research work.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
Conceptualization: Conceived and designed the experiments: HK, AKG, TGS. Analyzed the data: SG, AKG, TGS. Wrote the manuscript: PS, HK. Editing of the manuscript: TGS. Critically reviewed the article: TGS.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saklani, P., Khan, H., Singh, T.G. et al. Demethyleneberberine, a potential therapeutic agent in neurodegenerative disorders: a proposed mechanistic insight. Mol Biol Rep 49, 10101–10113 (2022). https://doi.org/10.1007/s11033-022-07594-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07594-9