Abstract
To investigate associations of trimester-specific GWG with fetal birth size and BMI at age 5 years. We examined 3,015 singleton births to women without pregnancy complications from the Child Health and Development Studies prospective cohort with measured weights during pregnancy. We used multivariable regression to examine the associations between total and trimester gestational weight gain (GWG) and birth weight for gestational age and child BMI outcomes, adjusting for maternal age, race/ethnicity, education, marital status, parity, pre-pregnancy body mass index (BMI), and smoking; paternal overweight, gestational age, and infant sex. We explored differences in associations by maternal BMI and infant sex. GWG in all trimesters was significantly and independently associated with birth weight with associations stronger, though not significantly, in the second trimester. First trimester GWG was associated with child BMI outcomes (OR for child overweight = 1.05; 95% CI = 1.02, 1.09). Each kg of first trimester GWG was significantly associated with increased child BMI z-score in women of low (β = 0.099; 95% CI = 0.034, 0.163) and normal (β = 0.028; 95% CI = 0.012, 0.044), but not high pre-pregnancy BMI. GWG in all trimesters was associated with birth weight; only first trimester GWG was associated with child BMI. If replicated, this information could help specify recommendations for maternal GWG and elucidate mechanisms connecting GWG to child BMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Increasing evidence links maternal gestational weight gain (GWG) with BMI and overweight status in child and adult offspring [1–8]. The effect of GWG on later-life body size may depend on the period or trimester of pregnancy. Data from the Dutch Famine studies reported that maternal exposure to famine in early pregnancy is associated with increased adult BMI in women [9, 10]. Animal models confirm that mechanisms affecting appetite and metabolism develop during early gestation and that this process may be affected by maternal nutrition [11–13].
Several epidemiologic studies have reported that GWG in the second trimester is more strongly associated with birth weight or small for gestational age (SGA) than GWG in the first or third trimester [14–20]. Further, the association between trimester-specific GWG and weight at birth may depend on maternal pre-pregnancy BMI [17]. Although birth weight is one predictor of later-life body size, additional research is needed to determine associations between trimester-specific GWG and child BMI.
Two recent European cohort studies report that high gestational weight gain in early and middle, but not late, pregnancy is associated with increased child BMI [21, 22]. Both studies examine populations that are racially/ethnically homogenous compared to US populations, and only one uses measured (vs. self-reported) weights during pregnancy. Research is therefore needed in more diverse US populations, using measured weights throughout pregnancy.
Identifying how trimester-specific GWG affects risk of adiposity in childhood could provide evidence for interventions during pregnancy and inform recommendations for GWG. In 2009, the Institute of Medicine (IOM) called for research to “determine whether the pattern of maternal weight gain affects short or long-term child outcomes [23].” Such research may also inform future study of biological mechanisms connecting childhood obesity to the intrauterine environment.
Our objectives were to investigate associations between trimester-specific GWG and both birth weight for gestational age and child BMI at age five and to explore whether these associations differed by maternal pre-pregnancy BMI. We used data from a racially diverse US population with clinical measurements of weight throughout pregnancy.
Materials and Methods
Study Participants
The Child Health and Development Studies (CHDS) is a longitudinal birth cohort study of prenatal and early life determinants of disease and has been described in detail elsewhere [24]. Pregnant women who were members of Kaiser Permanente Health Plan in Oakland, California and who received prenatal care between 1959 and 1967 were eligible for the study (n = 20,754 pregnancies). During interviews in the first trimester of pregnancy, women reported their age, race/ethnicity, level of education, marital status, parity, smoking status, pre-pregnancy weight, date of last menstrual period, and the weight and height of the father. Women’s height and weight were measured at enrollment and weight measurements at each prenatal visit were abstracted from participants’ medical records. Child’s measured height and weight at age five were obtained from either a CHDS 5-year follow-up exam or from the child’s medical record.
We selected the first live, singleton birth without congenital anomalies delivered during the study period for women 15–44 years of age at the time of birth with no known diagnosis of diabetes, hypertension, or pre-eclampsia (n = 12,178). Of these, height and weight data at age five were available for 9,475 children. Data on maternal height, pre-pregnancy weight, and weight within 28 days before delivery were available for 7,030 births, of which 3,070 had sufficient maternal weight measurements throughout pregnancy to calculate trimester rates of GWG (at least one weight measured in the first trimester and at least two weights measured seven or more days apart in both the second and third trimesters).
Maternal Gestational Weight Gain
We calculated total GWG in kg as the difference between self-reported pre-pregnancy weight and the last recorded weight (within 28 days before delivery; 95% of women had a weight in the last 10 days) in the medical record (mean (standard deviation [SD]) days before delivery = 4.3 (3.3). We calculated total net GWG by subtracting infant birth weight from total GWG to address the part-whole correlation between total GWG and birth weight [23, 25]. Using previously described methods [14], we estimated trimester-specific GWG in kg as follows: We calculated summary rates of weight gain (kg/week) for each woman in the second (13.3–26.6 weeks) and third trimester (>26.6 weeks) using linear regressions of clinically measured weights and multiplied this rate by 13.3 weeks to obtain second- and third- trimester GWG. We subtracted second and third trimester GWG from total GWG to estimate first trimester (<13.3 weeks) GWG. This method includes women who did not have multiple measured weights in the first trimester, decreasing the potential for selection bias [14].
Birth Weight for Gestational Age Percentiles
We assessed length of gestation using self-reported date of last menstrual period and calculated birth weight for gestational age percentile (heareafter called “birth weight percentile”) from US national reference data[26] and defined small for gestational age (SGA) as <10th and large for gestational age (LGA) as >90th birth weight for gestational age percentiles, respectively. (Ultrasounds were not in common use at the time of this study.)
Child BMI z-Score and Child Overweight
For children who participated in the CHDS 5-year follow-up exam (n = 718), trained CHDS staff measured child weight and height using a clinical stadiometer prior to 1966, and a Harpenden stadiometer subsequently. For the remaining children (n = 2297), we used weight and height from their medical record measured closest to their fifth birthday. The correlations of weight and height measurements between the two groups of children were high (r = 0.98 for weight and r = 0.94 for height). We used 2000 Centers for Disease Control (CDC) reference data to calculate child BMI z-scores standardized for age (in months) and sex [27]. Due to the low prevalence of child obesity (BMI ≥ 95th percentile [28]) in our study sample (3%), we combined overweight (BMI 85th–94th percentile) and obesity categories and subsequently refer to BMI ≥ 85th percentile as “child overweight”.
Covariates
We calculated maternal pre-pregnancy and paternal BMI (kg/m2) and categorized BMI as low (<18.5), normal (18.5–24.9), and high (≥25) [29]. Race/ethnicity was categorized as white, black, and other (Latina, Asian, mixed or other).
Analytic Sample
After examining the distribution of key variables, we excluded births with gestational ages <22 or >44 weeks (n = 43) and implausible values of child BMI as defined by the CDC [27] (n = 12), yielding a final study sample of 3015 births.
Women in our target population (n = 12,178) were, on average, younger (26.7 vs. 27.8) and more likely to have smoked during pregnancy (35.6% vs. 30.9%) or have less than a high school education (33.9% vs. 15.3%) compared to our analytic sample. The target population was also less likely to be of white race/ethnicity (68.1% vs. 73.3%) and more likely to be of black race/ethnicity (22.1% vs. 16.2%), although the proportion of other race/ethnicity was similar (9.8% vs. 10.5%).
Statistical Analyses
We calculated the mean total and trimester-specific GWG and the proportion of SGA, LGA, and child overweight for all women and by maternal characteristics. We examined the association between trimester-specific GWG and the continuous birth weight percentile and child BMI z-score outcomes using linear regression models. We used logistic regression models to examine the association between trimester-specific GWG and odds of SGA, LGA, and child overweight. We also examined all models using total GWG and net GWG as the independent variable. Covariates were chosen a priori based on the literature and included maternal age and length of gestation as continuous variables and indicator variables for maternal race/ethnicity, educational attainment, marital status, parity, pre-pregnancy BMI categories, and smoking during pregnancy, paternal overweight, and infant sex (see Table 1 for categories). Covariates with missing data were represented by an indicator variable for “missing”.
We chose to examine maternal pre-pregnancy BMI as a potential effect modifier based on prior evidence that associations between timing of GWG and birth weight differ by this variable [17]. We tested for statistical interactions between trimester-specific GWG and maternal pre-pregnancy BMI in linear regression models of birth weight percentile and child BMI z-score. We only examined interactions in continuous outcome models because we suspected that, given the relatively small number of observations with child overweight, SGA, or LGA, further stratification by potential modifiers would lead to unstable estimates. We assessed statistical interaction by examining Wald tests of statistical significance with a P-value cut-off of 0.10. All analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC).
To ensure that high and low values of trimester-specific GWGs did not disproportionately affect estimates of association, we also examined models excluding births in the top and bottom one percent of GWG values in each trimester from the data. We examined models restricted to births with three or more measured weights in the second and third trimesters and models restricted to births with a final measured weight within 14 days of delivery. Finally, we examined models of trimester-specific gain and child BMI outcomes additionally adjusted for birth weight for gestational age to assess whether observed associations were explained by effects of GWG on birth weight.
Results
Descriptive Results
Table 1 describes the characteristics of the births in the study population. The majority of births were to mothers of white race/ethnicity, with at least a high school education, and with normal BMI. Thirty percent of mothers smoked during pregnancy. Due to enrollment criterion, almost all women in this study were married. Mean (SD) maternal age was 27.8 (5.7).
Table 2 presents the mean total and trimester-specific GWG for the whole sample and by selected maternal characteristics. Mean (SD) total GWG was 11.5 kg (4.1), and mean (SD) gains in trimesters one, two, and three were 1.6 (3.9), 5.5 (2.7), and 4.5 (2.7), respectively. Women of black race/ethnicity had higher GWG throughout pregnancy. Women with low pre-pregnancy BMI had higher total, second, and third trimester GWG but lower first trimester GWG, while women with high pre-pregnancy BMI had lower GWG throughout pregnancy.
Table 3 presents the five study outcomes—mean birth weight percentile and child BMI z-score and proportions of SGA LGA, and child overweight—for the whole sample and by selected maternal characteristics. Women of black and other race/ethnicity were more likely to have an SGA birth and less likely to have an LGA birth compared to white women. Women of black race/ethnicity were more likely to have a child classified as overweight at age five. Women with low BMI had a higher probability of SGA and women with high BMI had a higher probability of LGA and child overweight at age five. Children of high BMI fathers and of mothers who smoked during pregnancy were also more likely to be overweight at age five.
Multivariable Model Results
Unadjusted associations were larger in magnitude but similar in direction to adjusted associations (data not shown). For both birth weight percentile and child BMI z-score, we found evidence of statistically significant interactions between maternal pre-pregnancy BMI and first, but not second or third, trimester GWG.
Total GWG and all Outcomes:
Each kg of total GWG was associated with a statistically significant increase in birth weight percentile of 1.60 (95% CI = 1.39, 1.82), a significant decrease in odds of SGA of 0.89 (95% CI = 0.86, 0.91) and a significant increase in odds of LGA of 1.13 (95% CI = 1.10, 1.17). Each kg of total GWG was associated with a significant increase in child BMI z-score of 0.023 units (95% CI = 0.011, 0.034) and a significant increase in odds of child overweight of 1.04 (95% CI = 1.02, 1.07).
Trimester-Specific GWG and Birth Weight for Gestational Age Outcomes:
GWG in all trimesters was significantly and independently associated with decreased odds of SGA and increased odds of LGA (Table 4). Figure 1 describes associations between trimester-specific GWG and birth weight percentile. Specifically, each kg of first trimester GWG was significantly associated with an increase in birth weight for gestational age of 1.94 (95% CI = 0.70, 3.19) percentile points for women of low BMI, 1.59 percentile points (95% CI = 1.28, 1.90) for women of normal BMI, and 0.92 percentile points for women of high BMI (95% CI = 0.43, 1.40). Each kg of second trimester GWG was associated with an increase in birth weight for gestational age of 1.99 percentile points (95% CI = 1.61, 2.37), and each kg of third trimester GWG was associated with an increase of 1.55 percentile points (95% CI = 1.18, 1.93). Second trimester GWG was associated with larger differences in odds of LGA and SGA than first or third trimester GWG; these differences were not statistically significant when compared using a Wald test.
Difference in birth weight for gestational age percentile associated with 1 kg increase in gestational weight gain (GWG) in first, second, and third trimester from multivariable adjusted model with interaction between maternal pre-pregnancy BMI and first trimester GWG. Models adjusted for: maternal age, race/ethnicity, educational attainment, marital status, parity, BMI categories, and smoking during pregnancy; paternal overweight, length of gestation, and infant sex
Trimester-Specific GWG and Child BMI Outcomes at Age Five:
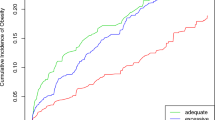
Each kg of first trimester GWG was associated with a five percent increase in odds of child overweight, while second and third trimester GWG were not significantly associated with child overweight (Table 4). Figure 2 shows associations between trimester-specific GWG and child BMI z-score. Specifically, each kg of first trimester GWG was associated with an increase in child BMI z-score of 0.099 (95% CI: 0.034, 0.163) z-score units among women of low pre-pregnancy BMI, 0.028 (95% CI: 0.012, 0.044) z-score units among women of normal pre-pregnancy BMI, and 0.020 (95% CI = −0.006, 0.045) z-score units among women of high pre-pregnancy BMI. Only the associations in low and normal pre-pregnancy BMI women achieved statistical significance. Second trimester GWG was marginally significantly associated with child BMI z-score (β = 0.020, 95% CI = −0.000, 0.039), while third trimester GWG was not significantly associated (β = 0.017, 95% CI = −0.003, 0.036).
Difference in child BMI z-score at age five associated with 1 kg increase in gestational weight gain (GWG) in first, second, and third trimester from multivariable adjusted models with interaction between maternal pre-pregnancy BMI and first trimester GWG. Models adjusted for: maternal age, race/ethnicity, educational attainment, marital status, parity, BMI categories, and smoking during pregnancy; paternal overweight, length of gestation, and infant sex
Sensitivity Analyses:
Estimates of association and standard errors (SE) for all outcomes (1) after excluding the top and bottom one percent of trimester GWG observations, (2) among births with at least three measured weights in the second and third trimesters, and (3) among births with a last measured weight within 14 days of delivery were similar in magnitude, direction, and statistical significance to those from the full dataset. Estimates of association from models of trimester-specific gain and child BMI outcomes adjusted for birth weight for gestational age were similar in direction and statistical significance but slightly attenuated in magnitude. Estimates of association from models using net GWG instead of total GWG were similar in direction, magnitude, and statistical significance to those for total GWG. (Results available from the corresponding author.)
Discussion
Gestational weight gain in all three trimesters contributed significantly and independently to birth weight for gestational age percentile, SGA, and LGA, with point estimates suggesting that second trimester GWG was most strongly associated with these outcomes. In contrast, GWG in the first, but not second or third trimesters was significantly associated with modest increases in child BMI z-score and overweight at age 5. To our knowledge, this is the first study of trimester-specific GWG to examine offspring body size at both birth and age 5 in a diverse sample of US women.
Our findings confirm previous research demonstrating stronger associations between second trimester GWG and birth weight outcomes and differences in this association by maternal BMI [14–20]. Although associations between GWG and birth weight percentile, SGA, and LGA were modest in magnitude, it should be noted that these associations are per kg of GWG and may therefore represent meaningful impacts on infant health. Our findings also support previous literature suggesting associations between total GWG and increased birth weight percentile and child BMI z-score, lower odds of SGA, and higher odds of child overweight and LGA [3, 4, 23].
For child BMI outcomes, we found that only first trimester GWG was associated with BMI z-score (among women of low and normal BMI) and increased odds of child overweight. Little existing research in humans examines associations between timing of GWG and later-life body size. Fraser and colleagues examined associations between early (0–14 weeks), middle (14–36 weeks), and late (>36 weeks) GWG and child adiposity at age 9 in more than 5000 pregnancies in the UK between 1991 and 1992 [22]. Significant increases in adiposity were associated with higher GWG in early pregnancy, and, among women gaining >500 g, in mid pregnancy. Unlike our study, there was no evidence of effect modification by maternal pre-pregnancy BMI. In a Danish cohort study of almost 10,000 births from 1996 to 2002, self-reported first and second trimester GWG was significantly associated with increased child BMI z-score at age 7 [21]. Estimates of association were slightly larger in magnitude than ours for the first and second trimester (β = 0.049 z-score units, β = 0.059 z-score units, respectively), similar in magnitude for the third trimester (β = 0.016 z-score units), and did not differ by maternal pre-pregnancy BMI. Results from our study in this more racially/ethnically diverse population generally agree with these previous studies in suggesting that early GWG is more strongly associated with child BMI than gain in later pregnancy.
Our finding that GWG in early pregnancy was more strongly associated with increased childhood BMI could have several explanations. First, women who gain more weight in early pregnancy may differ on unmeasured factors such as gestational diabetes mellitus (GDM) (which was not adequately assessed due to the absence of available tests), genetic characteristics, nausea, or diet and physical activity that are also associated with higher child BMI. Evidence also suggests that, in early pregnancy, maternal fat mass accumulation makes up a larger portion of GWG than does fetal growth, whereas the opposite is true in later pregnancy [23].
Second, the estimate of first trimester GWG depends on recalled pre-pregnancy weight, while second and third trimester GWG were estimated from clinically measured weights only, making the first trimester estimate more prone to potential bias. Underestimates of maternal pre-pregnancy weight have been shown to overestimate associations between maternal BMI and birth outcomes [30] but to our knowledge, no validity studies of self-reported versus measured first trimester weight gain have been published. Future studies should link pregnancy data with measured pre-conception weights from medical records or attempt to weigh women in very early pregnancy.
These associations may, however, reflect biological processes during gestation that impact offspring body size later in life. Endocrine and neuroendocrine regulators of metabolism become activated early in gestation, and GWG in the first trimester may affect this process [11, 13]. Later in pregnancy, maternal nutrition may increase deposition of adipose tissue [11, 13, 31], potentially explaining why second trimester GWG is more strongly associated with birth weight.
This study draws on the unique nature of the prospective CHDS cohort, which includes clinically-measured data on maternal and offspring weights and heights in a relatively large and diverse sample prior to the current obesity epidemic. Clinicians advising women in this cohort to gain no more than 20 lb during pregnancy [32] is demonstrated by the lower mean total and first, second, and third trimester GWGs compared to those from the recent study in Denmark [21]. While these temporal differences may limit generalizability to current populations with more overweight or obese mothers or larger GWG, these findings also may be less confounded by environmental factors and therefore suggest a more biological interpretation.
Only a subset of women from the initial CHDS study had adequate clinical measures of weight throughout pregnancy, limiting our sample size to 3,015 births. The differences between women in our analytic and target samples likely reflect differential utilization of prenatal care and follow-up of black women, those with less education, and smokers. Future studies should aim to include and measure weight gain throughout pregnancy in adequate numbers of women in these groups.
We also caution that estimates in the low and high pre-pregnancy BMI groups may be less stable than those from the normal BMI group or all women due to smaller sample sizes. Our findings suggest that associations between first trimester GWG and both child BMI z-score and birth weight for gestational age were strongest among women of low BMI and weakest among women of high BMI. This may represent an important difference in the effect of GWG on child body size at birth and age five by maternal pre-pregnancy BMI, but future studies with larger sample sizes are needed to confirm this pattern and should also investigate whether effects of trimester-specific GWG differ by maternal race/ethnicity, socioeconomic status, parity, or maternal age.
If replicated, our findings may have important clinical and scientific implications. The trade-off between decreased risk of SGA and increased risk of child overweight associated with higher GWG has led to much concern and debate about how to balance these outcomes in recommendations for GWG [2, 4]. Our findings suggest that moderation of early weight gain combined with not-overly restricted gain in the second and third trimesters is likely to promote the healthiest offspring size both at birth and in early childhood [23]. However, interventions to reduce excessive GWG have produced mixed results [33, 34]. In order to achieve the evidence base required to understand how to improve health outcomes through moderating gestational weight gain, there is a strong need to improve the size, scope, intervention methods and reporting of future trials to determine the most effective mechanisms for supporting healthy weight in pregnancy [33].
References
Li, C., et al. (2007). Developmental trajectories of overweight during childhood: Role of early life factors. Obesity (Silver Spring), 15(3), 760–771.
Mamun, A. A., et al. (2009). Associations of gestational weight gain with offspring body mass index, blood pressure at 21 years of age: evidence from a birth cohort study. Circulation, 119(13), 1720–1727.
Margerison Zilko, C. E., Rehkopf, D., & Abrams, B. (2010). Association of maternal gestational weight gain with short- and long-term maternal and child health outcomes. American Journal of Obstetrics and Gynecology, 202(6), 574. e1-e8.
Nohr, E. A., et al. (2008). Combined associations of prepregnancy body mass index and gestational weight gain with the outcome of pregnancy. American Journal of Clinical Nutrition, 87(6), 1750–1759.
Oken, E., et al. (2007). Gestational weight gain and child adiposity at age 3 years. American Journal of Obstetrics and Gynecology 196(4), 322 e1–e8.
Olson, C. M., Strawderman, M. S., & Dennison, B. A. (2009). Maternal weight gain during pregnancy and child weight at age 3 years. Maternal and Child Health Journal, 13(6), 839–846.
Stuebe, A. M., Forman, M. R., & Michels, K. B. (2009). Maternal-recalled gestational weight gain, pre-pregnancy body mass index, and obesity in the daughter. International Journal of Obesity (London), 33(7), 743–752.
Wrotniak, B. H., et al. (2008). Gestational weight gain and risk of overweight in the offspring at age 7 y in a multicenter, multiethnic cohort study. American Journal of Clinical Nutrition, 87(6), 1818–1824.
Ravelli, A. C., et al. (1999). Obesity at the age of 50 y in men and women exposed to famine prenatally. American Journal of Clinical Nutrition, 70(5), 811–816.
Roseboom, T., de Rooij, S., & Painter, R. (2006). The Dutch famine and its long-term consequences for adult health. Early Human Development, 82(8), 485–491.
Budge, H., et al. (2005). Maternal nutritional programming of fetal adipose tissue development: Long-term consequences for later obesity. Birth Defects Research C Embryo Today, 75(3), 193–199.
Gilbert, J. S., & Nijland, M. J. (2008). Sex differences in the developmental origins of hypertension and cardiorenal disease. American Journal of Physiology: Regulatory, Integrative and Comparative Physiology, 295(6), R1941–R1952.
Symonds, M. E., et al. (2004). Timing of nutrient restriction and programming of fetal adipose tissue development. Proceedings of the Nutrition Society, 63(3), 397–403.
Abrams, B., & Selvin, S. (1995). Maternal weight gain pattern and birth weight. Obstetrics and Gynecology, 86(2), 163–169.
Brown, J. E., et al. (2002). Variation in newborn size according to pregnancy weight change by trimester. American Journal of Clinical Nutrition, 76(1), 205–209.
Hickey, C. A., et al. (1996). Prenatal weight gain patterns and birth weight among nonobese black and white women. Obstetrics and Gynecology, 88(4 Pt 1), 490–496.
Lantz, M. E., et al. (1996). Maternal weight gain patterns and birth weight outcome in twin gestation. Obstetrics and Gynecology, 87(4), 551–556.
Neufeld, L. M., et al. (2004). Changes in maternal weight from the first to second trimester of pregnancy are associated with fetal growth and infant length at birth. American Journal of Clinical Nutrition, 79(4), 646–652.
Sekiya, N., et al. (2007). Maternal weight gain rate in the second trimester are associated with birth weight and length of gestation. Gynecologic and Obstetric Investigation, 63(1), 45–48.
Strauss, R. S., & Dietz, W. H. (1999). Low maternal weight gain in the second or third trimester increases the risk for intrauterine growth retardation. Journal of Nutrition, 129(5), 988–993.
Andersen, C. S., et al. (2010). Weight gain in different periods of pregnancy and offspring’s body mass index at 7 years of age. International Journal of Pediatric Obesity [Epub ahead of print].
Fraser, A., et al. (2010). Association of maternal weight gain in pregnancy with offspring obesity and metabolic and vascular traits in childhood. Circulation, 121(23), 2557–2564.
Institute of Medicine. (2009). Weight gain during pregnancy: reexamining the guidelines. Washington, DC: The National Academies Press.
Data Archive and User’s Manual of the Child Health and Development Studies, Version 2.0.2, September 10, 2008. Public Health Institute.
Selvin, S., & Abrams, B. (1996). Analysing the relationship between maternal weight gain and birthweight: Exploration of four statistical issues. Paediatric and Perinatal Epidemiology, 10(2), 220–234.
Oken, E., et al. (2003). A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatrics 3(6).
A SAS Program for the CDC Growth Charts. National Center for Health Statistics. Accessed October, 2007. http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm.
Defining Childhood Overweight and Obesity. Centers for Disease Control. Accessed September, 2009. http://www.cdc.gov/obesity/childhood/defining.html.
(2000). Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser, 894, i–xii, 1–253.
Bodnar, L. M., Siega-Riz, A. M., Simhan, H. N., et al. (2010). The impact of exposure misclassification on associations between prepregnancy BMI and adverse pregnancy outcomes. Obesity, 18(11), 2184–2190.
McMillen, I. C., et al. (2009). The early origins of later obesity: Pathways and mechanisms. Advances in Experimental Medicine and Biology, 646, 71–81.
Abrams, B., Altman, S. L., & Pickett, K. E. (2000). Pregnancy weight gain: Still controversial. American Journal of Clinical Nutrition, 71(5 Suppl), 1233S–1241S.
Gardner, B., Wardle, J., Poston, L., et al. (2011). Changing diet and physical activity to reduce gestational weight gain: A meta-analysis. Obesity Reviews, 12(7), e602–e620.
Phelan, S., Phipps, M. G., Abrams, B., et al. (2011). Randomized trial of a behavioral intervention to prevent excessive gestational weight gain: The Fit for Delivery Study. American Journal of Clinical Nutrition, 93(4), 772–779.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Margerison-Zilko, C.E., Shrimali, B.P., Eskenazi, B. et al. Trimester of Maternal Gestational Weight Gain and Offspring Body Weight at Birth and Age Five. Matern Child Health J 16, 1215–1223 (2012). https://doi.org/10.1007/s10995-011-0846-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-011-0846-1