Abstract
Purpose
Anticoagulation with heparin is required during catheter ablation of atrial fibrillation (AF) to reduce systemic thromboembolism. In this study, we aim to compare safety and efficacy outcomes between patients who receive protamine administration for reversal of heparin and those who do not, following cryoballoon-based pulmonary vein isolation (PVI) for AF.
Methods
Patients with symptomatic paroxysmal or persistent AF despite ≥1 antiarrhythmic drug(s) were scheduled for PVI per the recent consensus recommendations. Some patients were administered protamine at the end of the procedure depending on the operator’s choice.
Results
Among 380 patients [48.2 % male, 56 (20–86) years] that were enrolled, 188 patients received protamine at the end of the procedure. Baseline characteristics did not differ between groups (p > 0.05). Mean protamine dose was 39.1 ± 6.4 mg. Only 1 patient developed rash following protamine infusion. Hospital stay was significantly shorter in patients who were administered protamine (1 [1–5] vs. 2 [1–7] days, p < 0.001). Hematoma/pseudoaneurysm or femoral AV fistula requiring surgical or interventional repair in the femoral access site occurred in 2 (1.1 %) patients who received protamine and 12 (6.3 %) patients who did not (p = 0.011). Deep vein thrombosis was seen in 1 patient in whom protamine was not administered (p = 0.499).
Conclusion
To the best of our knowledge, this is one of the largest series showing that protamine administration for heparin reversal in patients undergoing cryoballoon-based PVI allows quicker sheath removal and minimizes the risk of potential vascular complications without causing an increase in thrombotic events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Atrial fibrillation (AF) is a common arrhythmia and is known to be associated with frequent hospitalization, hemodynamic abnormalities and thromboembolic events [1]. Catheter ablation has emerged as a beneficial strategy for rhythm control to improve symptoms and quality of life in AF patients [2]. However, periprocedural thromboembolism is a relatively common complication. The incidence of thromboembolic events varies from 1 to 5 %, depending on the ablation and the anticoagulation strategy used in the periprocedural period [3]. Current guidelines recommend administration of unfractionated heparin (UFH) prior to or immediately following transseptal puncture and dose adjustment to maintain an activated clotting time (ACT) above 300 s [4]. Nevertheless, reversal of heparin-mediated anticoagulation is required to avoid procedural complications, including vascular access complications or cardiac tamponade. Administration of protamine sulfate has been reported to be safe in patients undergoing radiofrequency catheter ablation [5]. Recently, reversal of UFH-mediated effects by protamine administration has been reported to be safe in patients undergoing cryoballoon-based pulmonary vein isolation (PVI) [6].
In the present study, we aim to assess safety and efficacy outcomes of protamine sulfate administration for reversal of UFH-mediated anticoagulation following cryoballoon-based PVI in a larger study population.
2 Methods
2.1 Study population
During the period between September 2010 and December 2014, 380 patients with symptomatic paroxysmal or persistent AF despite ≥1 antiarrhythmic drug(s) who were scheduled for cryoballoon-based AF ablation procedure per the recent consensus recommendations were included in this retrospective study [4].
Atrial fibrillation episodes that either last >7 days or require termination by cardioversion, either with drugs or by direct current cardioversion were defined as persistent; where AF episodes self-terminating within 7 days were defined as paroxysmal AF [7]. Patients who had moderate–severe valvular disease, thrombus in left atrium (LA), abnormal thyroid function, contraindication to anticoagulation, and left ventricular ejection fraction (LVEF) <50 % were excluded from the study.
Baseline demographic and clinical characteristics including age, gender, hypertension, diabetes mellitus, coronary artery disease, smoking history, and alcohol consumption were recorded for all patients. Data related to the diagnosis of AF including date of first diagnosis, oral anticoagulation, and antiarrhythmic medications were also recorded. Risk stratification for thromboembolism and bleeding complications were performed based on CHA2DS2-VASc and HAS-BLED scores, respectively [7]. The study was in compliance with the principles outlined in the Declaration of Helsinki and approved by the Institutional Ethics Committee.
2.2 Pre-procedural management
All patients underwent transthoracic echocardiography (TTE) within 1 week prior to ablation to assess intracavitary dimensions, LVEF and to exclude valvular heart disease. Transesophageal echocardiography was performed to rule out the presence of thrombus in the LA appendage, the day before procedure. Furthermore, patients underwent a pre-procedural multidetector computed tomography (MDCT) scan with three dimensional (3D) construction of the LA to assess detailed LA anatomy, including evaluation of the pulmonary vein (PV) configuration. Anticoagulation was discontinued at least 48–72 h before the procedure and the pre-procedural interval was bridged with enoxaparin 1 mg/kg. Treatment with antiarrhythmic drugs was discontinued for at least 3 days prior to the procedure.
2.3 Ablation procedure
Ablation was performed under conscious sedation using boluses of midazolam. Invasive arterial blood pressure, oxygen saturation, and electrocardiogram were monitored throughout the procedure.
Right femoral vein and left femoral vein and artery punctures were performed with Seldinger technique. A 6Fr steerable decapolar catheter (Dynamic Deca™, Bard Electrophysiology) was placed in the coronary sinus. Single transseptal puncture by modified Brockenbrough technique (BRK-1™, St Jude Medical) was performed under fluoroscopy and 8Fr transseptal sheath (Biosense Webster) was placed into the LA. Once LA access was obtained, heparin boluses were repeatedly administered to maintain the activated clotting time between 300 and 350 s. The sheath was then exchanged for a 12Fr steerable transseptal sheath (FlexCath™, Medtronic CryoCath) over a guidewire (0.032 in., 180 cm Super Stiff™, St Jude Medical). During PVI with Arc-CB, baseline electrical potentials of all PVs were recorded with a Lasso catheter™ (Biosense Webster, Inc.). In patients who underwent PVI with Arc-Adv-CB, the Achieve Mapping Catheter™ (Medtronic, Minneapolis, MN, USA) was positioned at the PV ostium where baseline PV potentials were documented [8].
A 28-mm first generation CB catheter (Arctic Front™, Medtronic CryoCath LP) was used in 197 patients who underwent PVI between September 2010 and December 2012. A 28-mm second generation CB catheter (Arctic Front Advance™, Medtronic CryoCath LP) was used in 183 patients who underwent PVI between December 2012 and December 2014. The cryoballoon was maneuvered to all PV ostia by means of the steerable 12Fr sheath and a guidewire was inserted through the lumen of the balloon catheter. The balloon was inflated in the LA and then directed toward the PV ostia. Assessment of balloon occlusion was performed by injecting 50 % diluted contrast through the cryoballoon catheter’s central lumen. Optimal vessel occlusion was considered to have been achieved when selective contrast injection showed total contrast retention with no flow back to the LA. Once occlusion was documented, cryothermal energy was started. A minimum of two consecutive freezing cycles were performed for each pulmonary vein. In cases of incomplete isolation of PV ostia, additional freezing cycles were applied until complete isolation was achieved. The duration of each freezing cycle was 240 and 300 s in patients undergoing PVI with Arc-Adv-CB and Arc-CB, respectively. The procedure systematically began with the left superior PV (LSPV), followed by the left inferior (LIPV), right superior (RSPV), and right inferior (RIPV) PVs, respectively. During ablation, if PV potentials (PVP) were visible during energy delivery, time to isolation was recorded when PVPs completely disappeared or were dissociated from LA activity. At the end of the procedure, PV conduction was reevaluated with the Lasso and Achieve catheters in PVI with first and second generation CB, respectively.
To avoid PNP, the decapolar catheter was inserted in the superior vena cava, and diaphragmatic stimulation was achieved by pacing the ipsilateral phrenic nerve with a 1000-ms cycle and a 20-mA output. PN capture was monitored by intermittent fluoroscopy and tactile feedback obtained following placement of the operator’s hand on the patient’s abdomen. Refrigerant delivery was immediately stopped if weakening or loss of diaphragmatic movement was noted. No further cryoenergy was delivered if PNP occurred.
2.4 Post-procedural management
A TTE was performed immediately after the procedure to exclude the presence of pericardial effusion.
Protamine was given at the end of the procedure for reversal of UFH-mediated anticoagulation effects in some patients depending on the operator’s choice. Protamine dose was determined on the basis of the amount of UFH received during the last hour of the procedure (total dose calculated as 1 mg of protamine per 100 units of heparin received, maximum protamine dose was 50 mg) and was administered slowly over a time period of 5 min [9]. Hemodynamic monitorization was continued during and after the infusion. In patients who received protamine, sheaths were removed following activated clotting time (ACT) assessment. On the other hand, in patients who did not receive protamine, sheaths were removed in the intensive care unit approximately 90 min after the last heparin dose, without assessing ACT. Venous and arterial bleeding was stopped by means of manual compression. Once the hemostasis was achieved, a period of 6 h of bed rest and 12 h of groin compression bandage was indicated.
All patients were followed up for at least 24 h in the telemetry unit. Any neurologic symptom or sign was evaluated cautiously for thromboembolism or bleeding events. Such cases were consulted with the neurology department and further evaluated with cranial computed tomography and/or magnetic resonance imaging in accordance with their suggestions. The groin was examined for complications related with puncture and/or thrombosis at discharge. When pseudoaneurysm or arteriovenous fistula was suspected at examination, the patient underwent further evaluation with Doppler sonography. Patients were then discharged provided that their clinical statuses were stable. Anticoagulation was initiated with low-molecular weight heparin and vitamin K antagonists at least 6–8 h after sheath removal, provided that there was no pericardial effusion on transthoracic echocardiogram. Oral anticoagulation with vitamin K antagonists was continued for at least 3 months after the procedure. Antiarrhythmic drug treatment was also continued for at least 3 months. Patients who experienced minor vascular complications were followed up by means of clinical visit at 1 and 4 weeks after discharge.
2.5 Statistical analysis
Normally distributed continuous parameters are presented as mean ± standard deviation and skewed continuous parameters are expressed as median (interquartile range defined as Q1-Q3, minimum-maximum). Categorical data are presented as frequencies and percentages and are compared using chi-square test. Comparisons between baseline characteristics are performed by independent student t, Mann-Whitney rank-sum, Fisher exact, or chi-square tests where appropriate. Statistical analyses are performed using SPSS statistical software (version 21.0; SPSS Inc., Chicago, Illinois, USA). A two-tailed p < 0.05 is considered statistically significant.
3 Results
Three hundred eighty patients [48.2 % male, 56 (20–86) years] were evaluated in this study. Of them, 188 patients received protamine post-procedurally. Baseline characteristics of the study population depending on protamine administration are shown in Table 1. None of the baseline demographic, clinical, laboratory, or echocardiographic parameters differed between patient groups.
Procedural and post-procedural follow-up characteristics of the study population are shown in Table 2. Mean dose of UFH administered during the procedure was 7817.8 ± 1274.3 U and did not differ between patients who received protamine and who did not (Table 2). Initial UFH bolus dose was 3294.0 ± 793.7 U. Total protamine dose was 39.1 ± 6.4 mg. Only one patient developed rash following protamine infusion, which responded well to intravenous antihistamine and corticosteroid administration.
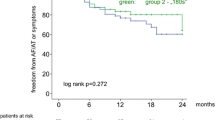
Time to sheath removal (6.3 ± 2.4 vs. 96.3 ± 2.4 min, p < 0.001) and mobilization (366.3 ± 13.3 vs. 456.3 ± 13.4 min, p < 0.001) was significantly shortened in patients who received protamine, whereas time to hemostasis did not significantly differ between two groups (p = 0.972). Hospital stay was shortened in patients who received protamine [1 (1–5) vs. 2 (1–7) days, p < 0.001]. Patients who received protamine developed less vascular access complications [2 (1.0) vs. 12 (6.3), p = 0.011]. Among those who received protamine, one patient developed hematoma/pseudoaneurysm and another 1 patient developed arteriovenous fistula. Of patients who did not receive protamine, 8 patients developed hematoma/pseudoaneurysm, and 4 patients developed arteriovenous fistula requiring surgical or interventional repair. Hematoma resolved spontaneously in all patients and none of the patients required blood transfusion. Femoral pseudoaneurysms were treated with manual compression. No symptomatic thromboembolic events (eg., transient ischemic attack, cerebrovascular accident) were observed in any groups. Thrombotic events did not differ between groups in a statistically significant way (p = 0.499). Deep vein thrombosis occurred in only 1 patient who had not received protamine. Other complications related with the procedure included mild pericardial effusion and pericardial tamponade, none of whose incidence differed between groups (Table 2). Pericardial tamponade case was treated with non- surgical drainage.
4 Discussion
To the best of our knowledge, this is the largest series reporting the safety and efficacy of protamine administration for reversal of UFH-mediated anticoagulation in patients undergoing cryoballoon-based PVI for AF. Our findings suggest that protamine sulfate administration in this patient group shortens sheath removal time, hospital stay, and minimizes vascular access complications without causing an increase in thromboembolic or thrombotic events.
Periprocedural thromboembolic and hemorrhagic events are of the most feared complications of catheter ablation for AF. Procedure-related strokes or transient ischemic attacks have been reported to occur in approximately 1 % of patients undergoing conventional RF ablation [10]. Furthermore, a higher rate of subclinical cerebral emboli has been detected in imaging studies, and incidence of subclinical microembolic events has been reported to vary between 8 and 14 % after cryoenergy or externally irrigated RF procedures [11, 12]. Embolic events related to PVI have been found to be linked with several issues including dislodgment of a pre-existing left atrial thrombus by catheter manipulation or formation of fresh thrombus on the sheath, the catheter, and over the newly created myocardial lesions [13]. Therefore, optimizing periprocedural anticoagulation is of vital importance.
There is limited evidence on bridging oral anticoagulants among atrial fibrillation patients undergoing invasive procedures. For patients at higher risk of thromboembolism (mechanical valves, prior stroke, CHA2DS2-VASc score ≥2), bridging with UFH or LMWH is a common practice, although data for LMWH are limited [14]. Several studies have suggested that bridging resulted in a high incidence of bleeding complications, especially at the site of vascular access [15–17]. Therefore, an increasingly common approach is to perform several procedures, including catheter ablation, without interrupting warfarin [18]. It is reported that radiofrequency catheter ablation of AF performed with a therapeutic INR does not increase bleeding risk and reduces the risk of emboli [18, 19]. Additional studies (e.g., BRIDGE [Bridging Anticoagulation in Patients who Require Temporary Interruption of Warfarin Therapy for an Elective Invasive Procedure or Surgery]) are ongoing. However, in our institution during the time the study took place, bridging oral anticoagulants was the preferred strategy.
Aggressive anticoagulation with UFH is required during catheter ablation of AF [4]. However, half-life time for elimination of UFH may cause prolonged immobilization period. Furthermore, the presence of a large sheath in the femoral vein for prolonged time may increase the risk of vascular complications [6]. At this point, protamine sulfate, which is used to neutralize UFH and thereby reverse anticoagulation in cardiac and vascular procedures [20], may help overcome this unfavorable outcome. Besides previous studies showing its desired effects following percutaneous coronary interventions both for providing early sheath removal [21, 22] and treating vascular complications including vessel rupture and major bleeding from the puncture site [23], protamine administration has also proved to be safe and effective in patients undergoing radiofrequency catheter ablation for AF [5] and cryoballoon-based PVI [6]. Our study, which has the largest study population to date, also confirms these results. Antagonizing UFH with protamine has shortened time to sheath removal and mobilization and also hospital stay, without causing an increase in thromboembolic or thrombotic events. Furthermore, vascular access complication burden was also reduced in patients who received protamine. A repeat measurement of ACT before sheath removal in patients who did not receive protamine may have been beneficial for lowering vascular access complication rate in this group.
Incidence of adverse reactions due to protamine administration, such as rash, urticaria, transient systemic hypotension, edema of the skin, mucosa and viscera, decreased systemic vascular resistance, bronchospasm, or pulmonary vasoconstriction, was reported to be 1.1 % [20]. Incidence of adverse effects due to protamine in our study was low (0.3 %) in a similar way. However, close monitorization for these rare but serious complications is essential following administration of the drug for early diagnosis and appropriate management.
5 Study limitations
This study has some limitations. First, this is a non-randomized and retrospective study. Second, only clinically apparent events suspected for thromboembolism were evaluated and cases were not investigated for silent thromboembolism. Furthermore, protamine administration was dependent on operator’s choice. This may have caused bias, however baseline characteristics of the patients did not differ between those who received and who did not receive protamine.
6 Conclusion
Post-procedural protamine sulfate administration for reversal of UFH-mediated anticoagulation in patients undergoing cryoballoon-based PVI for AF shortens sheath removal time, hospital stay, and minimizes vascular access complications without causing an increase in thromboembolic or thrombotic events. These findings should be proved in further randomized studies.
References
January, C. T., Wann, L. S., Alpert, J. S., Calkins, H., Cigarroa, J. E., Cleveland, J. C., Jr., et al. (2014). 2014 AHA/ACC/HRS Guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation, 130(23), 2071–2104.
Hagens, V. E., Ranchor, A. V., Van Sonderen, E., Bosker, H. A., Kamp, O., Tijssen, J. G., et al. (2004). Effect of rate or rhythm control on quality of life in persistent atrial fibrillation. Results from the Rate Control Versus Electrical Cardioversion (RACE) Study. Journal of the American College of Cardiology, 43(2), 241–247.
Viles-Gonzalez, J. F., & Mehta, D. (2011). Thromboembolic risk and anticoagulation strategies in patients undergoing catheter ablation for atrial fibrillation. Current Cardiology Reports, 13(1), 38–42.
Calkins, H., Kuck, K. H., Cappato, R., Brugada, J., Camm, A. J., Chen, S. A., et al. (2012). 2012 HRS/EHRA/ECAS Expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace, 14(4), 528–606.
Patel, A. A., Clyne, C. A., Henyan, N. N., White, C. M., Zembrowski, B. F., Migeed, M., et al. (2007). The use of protamine after radiofrequency catheter ablation: a pilot study. Journal of Interventional Cardiac Electrophysiology, 18(2), 155–158.
Conte, G., de Asmundis, C., Baltogiannis, G., Di Giovanni, G., Ciconte, G., Sieira, J., et al. (2014). Periprocedural outcomes of prophylactic protamine administration for reversal of heparin after cryoballoon ablation of atrial fibrillation. Journal of Interventional Cardiac Electrophysiology, 41(2), 129–134.
Camm, A. J., Lip, G. Y., De Caterina, R., Savelieva, I., Atar, D., Hohnloser, S. H., et al. (2012). 2012 focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation developed with the special contribution of the European Heart Rhythm Association. Europace, 14(10), 1385–1413.
Aytemir, K., Gurses, K. M., Yalcin, M. U., Kocyigit, D., Dural, M., Evranos, B., et al. (2014). Safety and efficacy outcomes in patients undergoing pulmonary vein isolation with second-generation cryoballoon†. Europace. 2014 Nov 5. pii: euu273. [Epub ahead of print].
Garcia, D. A., Baglin, T. P., Weitz, J. I., Samama, M. M., & American College of Chest, P. (2012). Parenteral anticoagulants: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest, 141(2 Suppl), e24S–e43S.
Cappato, R., Calkins, H., Chen, S. A., Davies, W., Iesaka, Y., Kalman, J., et al. (2010). Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation. Arrhythmia and Electrophysiology, 3(1), 32–38.
Gaita, F., Caponi, D., Pianelli, M., Scaglione, M., Toso, E., Cesarani, F., et al. (2010). Radiofrequency catheter ablation of atrial fibrillation: a cause of silent thromboembolism? Magnetic resonance imaging assessment of cerebral thromboembolism in patients undergoing ablation of atrial fibrillation. Circulation, 122(17), 1667–1673.
Neumann, T., Kuniss, M., Conradi, G., Janin, S., Berkowitsch, A., Wojcik, M., et al. (2011). MEDAFI-Trial (Micro-embolization during ablation of atrial fibrillation): comparison of pulmonary vein isolation using cryoballoon technique vs. radiofrequency energy. Europace, 13(1), 37–44.
Herrera Siklody, C., Deneke, T., Hocini, M., Lehrmann, H., Shin, D. I., Miyazaki, S., et al. (2011). Incidence of asymptomatic intracranial embolic events after pulmonary vein isolation: comparison of different atrial fibrillation ablation technologies in a multicenter study. Journal of the American College of Cardiology, 58(7), 681–688.
January, C. T., Wann, L. S., Alpert, J. S., Calkins, H., Cigarroa, J. E., Cleveland, J. C., Jr., et al. (2014). 2014 AHA/ACC/HRS Guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology, 64(21), 2246–2280.
Abhishek, F., Heist, E. K., Barrett, C., Danik, S., Blendea, D., Correnti, C., et al. (2011). Effectiveness of a strategy to reduce major vascular complications from catheter ablation of atrial fibrillation. Journal of Interventional Cardiac Electrophysiology, 30(3), 211–215.
Hoyt, H., Bhonsale, A., Chilukuri, K., Alhumaid, F., Needleman, M., Edwards, D., et al. (2011). Complications arising from catheter ablation of atrial fibrillation: temporal trends and predictors. Heart Rhythm, 8(12), 1869–1874.
Cappato, R., Calkins, H., Chen, S. A., Davies, W., Iesaka, Y., Kalman, J., et al. (2005). Worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation, 111(9), 1100–1105.
Di Biase, L., Burkhardt, J. D., Mohanty, P., Sanchez, J., Horton, R., Gallinghouse, G. J., et al. (2010). Periprocedural stroke and management of major bleeding complications in patients undergoing catheter ablation of atrial fibrillation: the impact of periprocedural therapeutic international normalized ratio. Circulation, 121(23), 2550–2556.
Lakkireddy, D., Reddy, Y. M., Di Biase, L., Vanga, S. R., Santangeli, P., Swarup, V., et al. (2012). Feasibility and safety of dabigatran versus warfarin for periprocedural anticoagulation in patients undergoing radiofrequency ablation for atrial fibrillation: results from a multicenter prospective registry. Journal of the American College of Cardiology, 59(13), 1168–1174.
Chilukuri, K., Henrikson, C. A., Dalal, D., Scherr, D., MacPherson, E. C., Cheng, A., et al. (2009). Incidence and outcomes of protamine reactions in patients undergoing catheter ablation of atrial fibrillation. Journal of Interventional Cardiac Electrophysiology, 25(3), 175–181.
Kuiper, K. K., & Nordrehaug, J. E. (2000). Early mobilization after protamine reversal of heparin following implantation of phosphorylcholine-coated stents in totally occluded coronary arteries. American Journal of Cardiology, 85(6), 698–702.
Pan, M., Suarez de Lezo, J., Medina, A., Romero, M., Hernandez, E., Segura, J., et al. (1997). In-laboratory removal of femoral sheath following protamine administration in patients having intracoronary stent implantation. American Journal of Cardiology, 80(10), 1336–1338.
Briguori, C., Di Mario, C., De Gregorio, J., Sheiban, I., Vaghetti, M., & Colombo, A. (1999). Administration of protamine after coronary stent deployment. American Heart Journal, 138(1 Pt 1), 64–68.
Acknowledgments
None.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gurses, K.M., Kocyigit, D., Yalcin, M.U. et al. Safety and efficacy outcomes of protamine administration for heparin reversal following cryoballoon-based pulmonary vein isolation. J Interv Card Electrophysiol 43, 161–167 (2015). https://doi.org/10.1007/s10840-015-9989-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-015-9989-0