Abstract
Background
The aims of this analysis were: to evaluate the impact of timing of ablation on the rate of atrial arrhythmias recurrence, verify if the timing of ablation impact differently in patients with paroxysmal and persistent AF.
Methods
Three thousand two hundred and five patients (60.5 ± 10 years, female 28.4%%, 78.8%% paroxysmal AF) were included in the analysis. All patients underwent only cryoballoon (CB) pulmonary vein (PV) isolation during the index procedure.
Results
The mean procedure time was 102.8 ± 50 min, with a mean fluoroscopy time of 26.3 ± 49 min. Acute PV isolation was achieved in 11760/11793 (99.7%) PVs. A total of 91 (2.8%) patients experienced a procedure-related complication. During the observation period 913/3205 (28.5%) patients had at least one atrial arrhythmias episode: 28% of patients with paroxysmal AF vs 33% of patients with persistent AF. In multivariate analysis, persistent AF together with time from symptomatic AF diagnosis to ablation, female sex, and ablation time showed to be significant predictors for AF recurrence. In particular, months from first symptomatic AF episode > 18 months was a significant predictor of AF recurrence (HR = 1.23, 95% CI = 1.03—1.46, p = 0.020).
In patients with paroxysmal AF, the multivariate analysis confirmed that months from first symptomatic AF episode > 18 month was an independent predictor of AF recurrence together with age > 62 years and female sex. In patients with persistent AF, the time from persistent AF showed to be significant predictor for AF recurrence.
Conclusions
In this multicenter analysis, time from first symptomatic AF episode > 18 months was a significant predictor of AF recurrence after CB PV isolation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Atrial fibrillation (AF) is the most common arrhythmia and is associated with increased morbidity and mortality [1]. Anti-arrhythmic drugs have long been the most often used treatment modality for symptomatic AF. The last decades, catheter ablation has.
emerged as an alternative treatment option, and several studies comparing catheter ablation and antiarrhythmic drugs have demonstrated superiority of catheter ablation.
in patients with previous failed antiarrhythmic drugs treatment, and recently, predominantly in patients with paroxysmal AF, also when used as first-line treatment [2]. Nevertheless, current guidelines [1] recommend AF catheter ablation for pulmonary vein (PV) isolation for rhythm control after one failed or intolerant class I or III antiarrhythmic drugs, to improve symptoms of AF recurrences in patients with both paroxysmal and persistent AF. Adherence to current guidelines risks to delay the ablation in patients with a short clinical history of AF [1]. Few data, collected mainly in patients undergoing radiofrequency PV isolation showed that an early rhythm control ablation strategy was associated with the lowest rate of recurrence [3,4,5]. The aim of our analysis was to investigate the impact of timing of ablation on arrhythmias recurrences in a large cohort of patients with paroxysmal and persistent AF who underwent cryoballoon (CB) PV isolation.
2 Methods
2.1 Patients selection
The patients included in the present analysis were included and followed in a network of 32 cardiology centres, which participate in the Italian ClinicalService® framework 1STOP project. This is a national medical care project aimed at evaluating and improving the use of medical therapies in the clinical practice. The project consists of a shared environment for the collection, management, analysis, and reporting of data from patients in whom Medtronic therapies have been applied [6]. Patients aged between 18 and 90 years with documented symptomatic paroxysmal or persistent AF, refractory to antiarrhythmic therapy, were eligible for the analysis. Exclusion criteria were: (1) permanent and long-standing persistent AF; (2) New York Heart Association functional class IV; (3) unstable angina or acute myocardial infarction within three months; (4) need for or prior cardiac surgery within six months; (5) contraindication to treatment with oral anticoagulants and (6) severe chronic renal or hepatic impairment.
The project was approved by each site’s Medical Ethics Committee or Medical Director and conforms to the principles outlined in the Declaration of Helsinki. Each patient provided informed consent for data collection and analysis.
2.2 Ablation procedure
In the 32 participating centres, 78 different operators performed the CB PV isolation only procedures. After transseptal catheterization, the CB catheter was introduced into the left atrium via a 12F steerable sheath (FlexCath Advance, Medtronic, Inc.). Mapping of the PVs was performed with an inner lumen mapping catheter (Achieve, Medtronic, Inc.). The mapping catheter was advanced in each PV ostia, positioned as proximal as possible to provide PV potentials recording. A 28-mm CB catheter (CB-1 Arctic Front or CB-2 Arctic Front Advance or CB-3 Arctic Front Advance ST or CB-4 Arctic Front Advance PRO, Medtronic) was advanced inflated and positioned at each PV antrum. Optimal vessel occlusion was considered to have been achieved when selective contrast injection showed the absence of contrast backflow to the atrium. When complete occlusion could not be achieved, the mapping catheter was replaced by a stiff guide wire (Amplatz Ultra Stiff, Cook Medical, Bloomington, IN, USA).The standard set of lesions includes the left superior PV treated as first, followed by the left inferior PV, right superior PV, and right inferior PV. As per nature of this project, we did not implement a standardized protocol on the number and duration of freeze nor the usage of a bonus freeze but a general strategy was shared among the centers. In case of the presence of a common ostium, the veins were treated as separate branches. Target application time was 180–240 s.
If the temperature did not attain -40 °C within 60 s or acceptable nadir temperature was not reached, a bonus freeze with a different occlusion was applied. The right phrenic nerve was paced from the superior cava or subclavian vein during freezing at the septal PVs. Phrenic capture was monitored by tactile feedback. In case of cessation or weakening of right hemi-diaphragm contractions, freezing was immediately terminated.
2.3 Post-ablation management and follow-up
Oral anticoagulation was left uninterrupted on the day of the procedure for all patients and continued for at least 3 months or long term in patients with a high thromboembolic risk assessed by CHA2DS2-VASc score. Antiarrhythmic drugs were usually discontinued ≥ 5 half-lives prior to ablation, except for amiodarone. Patients were scheduled for follow-up examinations 3, 6, and 12 months after the initial treatment and every six months thereafter. Rhythm monitoring during the follow-up visits was performed by the clinical assessment of AF recurrence, ECG and Holter monitoring according to the clinical practice of each center. Patients were asked to provide any other ECG or Holter monitoring performed since the previous visit.
Ablation was deemed successful in the absence of symptomatic or asymptomatic atrial tachyarrhythmias lasting longer than 30 s identified by surface ECG or Holter monitoring, after the blanking period (3 months) [7]. Long-term success was defined as single procedural success.
2.4 Aims of the research
The aims of this analysis were: to evaluate the impact of timing of ablation on the rate of atrial arrhythmias recurrence, verify if the timing of ablation impact differently in patients with paroxysmal and persistent AF.
2.5 Statistical analysis
Descriptive statistics were used to summarize patient characteristics. These include mean and standard deviation, minimum, maximum and median with the interquartile range (IQR) for continuous variables, and counts and percentages for categorical variables. Summary statistics were reported with maximum 2 decimals, as appropriate. Comparisons between groups have been performed using Wilcoxon’s Test for continuous variables, while comparisons of categorical variables have been performed using Chi-square test or Fisher’s exact test for extreme proportions, as appropriate.
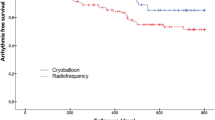
The analyses of time-to-first event were described using Kaplan–Meier curves and compared between the groups with the log-rank test. The follow-up duration (months) was computed from the date of implant to the date of last available follow-up or date of event: [(data end – data in)/30.4].
The annual rates of complications were reported, together with the 95% Confidence Intervals (CIs). The Poisson regression model was used to calculate the Incidence Rate ratio (IRR), using deviance scaling to correct for over/underdispersion. An IRR > 1 would show a lower incidence of event in the reference group, while an IRR < 1 would show a higher incidence of event in the reference group.
To find predictors of AF recurrences, a Cox Regression was used for both univariate and multivariate analyses, and the proportional hazard hypothesis was tested. Potential predictors defined a priori were assessed. Possible collinearity among the variables was tested using Spearman ‘s Rho, and a correlation coefficient > 0.80, together with clinical judgment, determined covariate exclusion. The final set of predictors was included in the multivariate model. The Hazard Ratios (HRs) and 95% CIs were estimated for all potential predictors. The multivariate Cox regression model used stepwise selection with entry = 0.30 and stay = 0.10 criteria, respectively, and AF as the dependent variable. The survival c-index was used as the main accuracy measure and reported together with the multivariate model’s results, if applicable.
Statistical tests were based on a two-sided significance level of 0.05.
The SAS software, version 9.4, (SAS Institute Inc., Cary, NC, USA) was used to perform statistical analyses.
3 Results
3.1 Study population
The analysis included 3205 patients, who underwent first CB ablation for paroxysmal (2524 patients) or persistent (681 patients) AF. Their main baseline clinical characteristics are showed in Table 1. Patients with paroxysmal AF were younger, had a lower mean body mass index, mean CHA2DS2-VASc score, left atrial diameter and volume, and, generally were a less sick population cohort.
3.2 PV isolation
All patients underwent only CB PV isolation during the index procedure. The mean procedure time was 102.8 ± 50 min, with a mean fluoroscopy time of 26.2 ± 23 min. Acute pulmonary vein isolation was achieved in 11,760/11793 (99.7%) pulmonary veins. A total of 91 (2.8%) patients experienced a procedure-related complication: 24 (0.7%) patients had a severe complication (that was permanent or required intervention), 76 (2.1%) patients had a minor complication, no death occurred. The most frequent adverse event was a transient diaphragmatic paralysis that occurred in 47 (1.5%) of patients. A permanent diaphragmatic paralysis occurred in two patients. One patient was free of diaphragmatic paralysis symptoms after 3 months and the other after 7 months. Table 2 shows procedural details and complications.
3.3 Follow-up data
During the observation period, after a blanking period of three months, 913/3205 (28.5%) patients had at least one episode of atrial arrhythmias: 27% of patients with paroxysmal AF vs 33% of patients with persistent AF (p < 0.001) (Fig. 1). In particular, out of 913 episodes, 19 were Atrial Flutter (11 in the paroxysmal group and 8 in the persistent group), and there was 1 episode of atrial tachycardia in the paroxysmal group. The remaining episodes were cases of AF. Out of the 893 AF recurrences, 69 occurred after 42 months from the first ablation. Out of 3205 patients, 10.2% (327/3205) patients had at least one Re-Do procedure (295 patients had only one redo, while 32 patients had more than one redo for a total of 36 procedures). At 36-month follow-up, the observed freedom from AF recurrence was 69.6% ( 95% CI = 67.4%—71.6%) and 62.3% (95% CI = 57.8%—66.5%) in paroxysmal and persistent AF groups, respectively (p < 0.001). In 98.2% of the patients during the first redo (321/327), the repeat procedure was to re-treat AF, while in 4 patients, the redo was to treat right atrial flutter, and in 2 patients, it was to ablate an atrial tachycardia. Among the 321 patients with a recurrence of AF, non-pulmonary vein ablations (including non-PV triggers, fragmented atrial potential ablation, and linear lesions) were performed in 111 procedures (34.6%). Data on redo were missing for 31 patients (9.7%), and in the remaining 179 patients (55.7%), a PV isolation procedure was performed: in 117 patients all the PVs were already disconnected, and no further ablation was performed; while in 21 patients, 1 PV was re-isolated; in 26 patients, 2 PVs were re-isolated; in 11 patients, 3 PVs were re-isolated, and in 4 patients, all 4 veins were isolated again.
3.4 Predictors of recurrence
All potential predictors have been included in multivariate analysis, and persistent AF together with time from AF diagnosis to AF PV isolation, time of ablation, and female sex showed to be significant predictors for AF recurrence (Table 3). In particular, months from first symptomatic AF episode > 18 months was a significant predictor of AF recurrence (Fig. 2). In patients with paroxysmal AF, female sex together with time of ablation, “Months from first symptomatic AF episode” showed to be significant predictors for AF recurrence. In particular, months from first symptomatic AF episode > 18 month (HR = 1.54 95% CI. 1.03–2.29, p = 0.034) was the best cut-off value to predict AF recurrence. In patients with persistent AF, months from persistent AF (HR: 1.01, 95% CI: 1.01—1.02, p < 0.001) and antiarrhythmic drug usage (HR: 0.57, 95% CI: 0.33–0.98, p < 0.044) and ablation time (HR: 4.11, 95% CI: 1.92–8.81, p < 0.001) showed to be significant independent predictors for AF recurrence.
4 Discussion
The main findings of this multicentre analysis were: 1) at 36-month follow-up, the freedom from AF recurrence was 69.6% ( 95% CI = 67.4%—71.6%) and 62.3% (95% CI = 57.8%—66.5%)in paroxysmal and persistent AF patients who underwent first CB PV isolation; 2) time from first symptomatic AF episode > 18 months was a significant predictor of AF recurrence; 3) in patients with paroxysmal AF, months from first symptomatic AF episode > 18 month was an independent predictor of AF recurrence, whereas in patients with persistent AF months of persistent AF (continuous) showed to be significant predictor for AF recurrence.
4.1 Timing of AF ablation
The superiority of AF prevention by catheter ablation over antiarrhythmic drugs is well established [1]. The question remains when catheter ablation should be performed in patients with symptomatic AF. AF often starts as brief and paroxysmal AF episodes and, in many patients, progresses over time to a persistent and long-standing AF. It is well known that AF itself promotes atrial remodeling that in turn promote AF perpetuation [8]. AF progression is associated with increased cardiovascular morbidity and mortality. Recently, the EAST-AFNET 4 Trial [9] demonstrated that a strategy of initiating rhythm-control therapy in all patients with early AF and concomitant cardiovascular conditions was associated with a lower risk of death from cardiovascular causes, stroke, or hospitalization for heart failure or acute coronary syndrome than usual care over a follow-up time of more than 5 years. Therefore, the concept that effective early rhythm control promotes sinus rhythm is of interest, as it thereby decelerates AF-related structural pathological atrial changes, and reduces progression to persistent AF [10], and reduces its associated cardiovascular morbidity and mortality.
4.2 Impact of timing of ablation on the rate of atrial arrhythmias recurrence
The predictive value of timing of AF ablation on AF recurrence remains controversial because often is hard to define the start of AF history and the duration of a patient’s AF history may not always be equivalent to the actual length of the AF episodes, and hence, may not reflect disease severity such as atrial remodeling. However, the two largest series [3, 4] seem support the hypothesis that the sooner the ablation is performed the better is its outcome. Pallisgard et al. [3], reported data from 5425 patients undergoing a first-time ablation in the Danish nationwide registers. Female gender, hypertension, AF history duration > 2 years, and cardioversion within 1 year prior to ablation were all associated with an increased risk of recurrent AF at one year after the ablation. Stabile et al. [4], reported data on 1948 patients enrolled in the ESC-EHRA atrial fibrillation ablation long-term registry. AF history duration ≥ 2 years, overall ablation procedure duration, hypertension and chronic kidney disease were all predictors of recurrences after the blanking period. The great amount of data has been collected in patients undergoing radiofrequency catheter ablation. In Stabile et al. [4] series, less than 20% of patients have been ablated by means of CB. Recently, Baysal et al. [11] investigated timing of PV isolation by CB after the first clinical diagnosis of AF on ablation-related outcomes in 132 patients with paroxysmal AF. They found that delays in treatment with CB ablation might negatively affect AF-free survival rates among patients with paroxysmal AF. Lunati et al. [12] showed that only the 21.5% of paroxysmal AF patients cryoablated in the first 15 months from the atrial fibrillation diagnosis reported an episode of atrial fibrillation recurrence versus the 31.6% of the late-treatment group. Chew [13] reported in a systematic review and meta-analysis on 6 studies for a total of 4950 patients that diagnosis-to-ablation times of 1 year or less were associated with a 27% less risk of AF recurrence compared with times > 1 year. Our study is the first to investigate the impact of timing of catheter ablation on a large, multicenter population, with both paroxysmal and persistent AF, on long-term outcome. We found that time from first symptomatic AF episode > 18 months was a significant predictor of AF recurrence. Looking at paroxysmal AF patients this cut-off value was prolonged to 28 months, whereas in patients with persistent AF time from first AF episode was no longer a predictor of AF recurrence. In this population, a significant predictor of AF recurrence was the length of persistent AF.
4.3 Clinical implications
Current ESC guidelines [1] for patients with AF suggest that patients should be first managed with a pharmaceutical drug therapy; when a patient becomes drug refractory (failure of or intolerance to at least one antiarrhythmic drug), or considering patient choice, catheter ablation by PV isolation is recommended. However, increased time between first AF diagnosis and catheter ablation may adversely affect long-term clinical efficacy. Early intervention by radiofrequency as well as CB ablation increase long-term success rates and reduce progression to persistent AF [14]. However, further randomized trials are needed to confirm our findings about the association between time-to-ablation and long-term outcomes of the procedure.
4.4 Limitations
The results of this study should be interpreted with caution due to a number of limitations. First, this study was a non-randomized retrospective analysis of data collected prospectively, so we cannot exclude bias in the patient selection and treatment. Second, this is a multicenter data collection, and the ablation strategy was not standardized, including: pre-procedural imaging, oral anticoagulant management, number and duration of freeze, and the usage of a bonus freeze. However, this observational retrospective research may provide a representative image of the real-life scenario on the usage of CB catheter for AF ablation. Third, sinus rhythm maintenance was based mainly on patients’ symptoms, ECG and scheduled 24-h Holter monitoring and not on continuous monitoring. Therefore, asymptomatic or short-lasting AF episodes may have occurred unnoticed, and our success rate may have been over-estimated. However, the success rate of CB PV isolation was in line with previous studies. Fourth, this study was not testing a prospective hypothesis, and consequently, no adjustments were formulated for the multiplicity of testing. Also, it is established that errors in confounding and bias are more common in non-prospective studies, which cannot utilize randomization or a true control arm. Consequently, this data should be viewed as a real-world snapshot of current usage practices amongst a large group of CB users in one European country. Moreover, the time to first symptomatic AF episode was collected on the basis of patients’ history during the baseline visit. Fifth, we excluded from this analysis long standing AF patients. Sixth, in our experience longer ablation time predicted AF recurrences. We do not have a conclusive explanation for it and we can only hypothesize that a shorter ablation time is related to a favourable PV anatomy that make CB ablation easier and more effective. Lastly, we have no data on the cumulative time (burden) our patients spent in AF that may influence the impact of time from diagnosis on ablation outcomes.
5 Conclusions
Time from first symptomatic AF episode > 18 months was a significant predictor of AF recurrence in patients undergoing CB PVI catheter ablation. In patients with paroxysmal AF months from first symptomatic AF episode > 18 month was an independent predictor of AF recurrence, whereas in patients with persistent AF months of persistent AF (continuous) showed to be significant predictor for AF recurrence. These results should be kept in mind when we plan a PVI procedure by the means of cryoballoon catheter in patients with AF.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, ESC Scientific Document Group, et al. ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42:373–498.
Imberti JF, Ding WY, Kotalczyk A, Zhang J, Boriani G, Lip G, et al. Catheter ablation as first-line treatment for paroxysmal atrial fibrillation: a systematic review and meta-analysis. Heart. 2021;107:1630–6.
Pallisgaard JL, Gislason GH, Hansen J, Johannessen A, Torp-Pedersen C, Rasmussen PV, et al. Temporal trends in atrial fibrillation recurrence rates after ablation between 2005 and 2014: a nationwide Danish cohort study. Eur Heart J. 2018;39:442–9.
Stabile G, Trines SA, Arbelo E, Dagres N, Brugada J, Kautzner J, et al. Atrial fibrillation history impact on catheter ablation outcome. Findings from the ESC-EHRA atrial fibrillation ablation long-term Registry. Pacing Clin Electrophysiol. 2019;42:313–20.
Solimene F, Giannotti Santoro M, Stabile G, Malacrida M, De Simone A, et al. Early rhythm-control ablation therapy to prevent atrial fibrillation recurrences: Insights from the CHARISMA Registry. Pacing Clin Electrophysiol. 2021;44:2031–40.
Padeletti L, Curnis A, Tondo C, Lunati M, Porcellini S, Verlato R, et al. Pulmonary vein isolation with the cryoballoon technique: feasibility, procedural outcomes, and adoption in the real world: data from one shot technologies to pulmonary vein isolation (1STOP) project. Pacing Clin Electrophysiol. 2017;40:46–56.
Stabile G, Iacopino S, Verlato R, Arena G, Pieragnoli P, Molon G, et al. Predictive role of early recurrence of atrial fibrillation after cryoballoon ablation. Europace. 2020;22:1798–804.
Wijffels MC, Kirchhof CJ, Dorland R, Allessie MA, Wijffels MC, Kirchhof CJ, Dorland R, Allessie MA. Atrial fibrillation begets atrial fibrillation. A study in awake chronically instrumented goats. Circulation. 1995;92:1954–68.
Kirchof P, Camm AJ, Goette A, Brandes A, Eckart L, Elvan A, EAST-AFNET 4 Trial Investigators, et al. Early Rhythm-Control Therapy in Patients with Atrial Fibrillation. N Engl J Med. 2020;383:1305–16.
Andrade J, Khairy P, Dobrev D, Nattel S. The Clinical profile and pathophysiology of atrial fibrillation: relationships among clinicalfeatures, epidemiology, and mechanism. Circ Res. 2014;114:1453–68.
Baysal E, Okşul M, Burak C, Yalin K, Soysal AU, Yalman H, et al. Decreasing time between first diagnosis of paroxysmal atrial fibrillation and cryoballoon ablation positively affects long-term consequences. J Interv Card Electrophysiol. 2022;65:365–72.
Lunati M, Arena G, Iacopino S, Verlato R, Tondo C, Curnis A, et al. Is the time between first diagnosis of paroxysmal atrial fibrillation and cryoballoon ablation a predictor of efficacy? J Cardiovasc Med (Hagerstown). 2018;19(8):446–52.
Chew DS, Black-Maier E, Loring Z, Noseworthy PA, Packer DL, Exner DV, et al. Diagnosis-to-ablation time and recurrence of atrial fibrillation following catheter ablation: a systematic review and meta-analysis of observational studies. Circ Arrhythm Electrophysiol. 2020;13:e008128. https://doi.org/10.1161/CIRCEP.119.008128.
Andrade JC, Deyell MW, Macle L, Wells GA, Bennett M, Essebag V, EARLY-AF Investigators, et al. Progression of atrial fibrillation after cryoablation or drug therapy. N Engl J Med. 2023;388:105–13.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Giuseppe Stabile and Roberto Verlato received modest consultancy and speaker’s fees from Medtronic. Giulio Molon received modest consultancy fees from Medtronic and Boston Scientific and speaker’s fees from Medtronic, Boston Scientific, St. Jude, and Boehringer Ingelheim. Claudio Tondo serves as a member of Medtronic European Advisory Board and Boston Scientific International Advisory Board. He received lecture and proctor fees from Medtronic, Abbott Medical, Biosense Webster, and Boston Scientific. All other authors have reported that they have no relationships relevant to the contents of this manuscript to disclose.
Ethical approval
The project was approved by each site’s Medical Ethics Committee or Medical Director and conforms to the principles outlined in the Declaration of Helsinki.
Informed consent
Each patient provided informed consent for data collection and analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stabile, G., Verlato, R., Arena, G. et al. Timing of cryoballoon pulmonary vein isolation to prevent atrial fibrillation recurrence. J Interv Card Electrophysiol 67, 609–616 (2024). https://doi.org/10.1007/s10840-023-01636-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-023-01636-3