Abstract
Common human reproductive inefficiencies have multiple etiologies. Going against chance, many effects, such as polycystic ovaries, endometriosis, and folate metabolic issues, have genetic components, while aneuploid losses arise from diverse mitotic and meiotic errors at different stages, some transitory. This can be advantageous, since greater overall survival with fewer offspring can increase reproductive success. Benefits primarily accrue to mothers, who bear most child related costs, and for whom early losses are less costly than late. Different adaptations to different situations reflect human evolutionary history. For early speciation, periodic climate extremes repeatedly reduced resources, favoring limitations while contracted populations helped fix relevant genes. Later, under better conditions, evolving social cooperation could increase fecundity faster than it added resources, further supporting reproductive suppression through mitotic aneuploidy, with very early losses minimizing maternal costs. The grandmother hypothesis suggests benefits in limiting reproduction as maternal age increased pregnancy risks in order to support grandchildren as they arrived, selecting for maternal age-related meiotic aneuploidy. Finally, with variable short-term agricultural shortages, acute reproductive responses arose through chromatin “nutrient sensor”-regulated epigenetic effects that also shifted some lethal effects earlier, reducing both maternal and mutation load costs. Overall, despite suggestions to the contrary, it is likely that human selective pressures have not decreased with civilization, but that many of the costs have been shifted to early reproduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human reproductive failures are common—even normally fertile women achieve biochemically determined embryo implantation less than half the time, with about half again failing to come to term [1]. Some issues are to be expected with a complex system in a varied environment but, as will be shown, several factors suggest that most of this is biologically programmed:
-
1.
A greater frequency of reproductive failures than in a variety of animal models.
-
2.
Multiple genetic components.
-
3.
Different types of intrinsic mechanisms, each with considerable heterogeneity.
-
4.
Early system defects that quickly resolve, and are exceptional later.
And here, despite what Day et al. [2] referred to for polycystic ovary syndrome as a “striking paradox of a highly heritable yet common condition that impairs fertility,” decreased fecundity can be advantageous [3]: Reproductive success depends upon the production of offspring and their survival, and decreases in one can be more than counterbalanced by increases in the other, with selection for fewer offspring if better overall survival results.
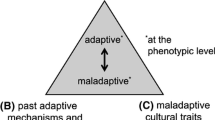
With this, human limitations can be placed into four basic categories:
-
1.
Genetic, including multiple polymorphisms
-
2.
Fixed intrinsic, primarily related to mitotic aneuploidy
-
3.
Advanced maternal age-dependent meiotic chromosomal abnormalities
-
4.
Variable epigenetic effects with intrinsic and extrinsic interactions
It is likely that each of these represents a different selective issue. Evidence of an adaptive response to intermittent food shortages exists for the epigenetic effects [4], and specific alternatives will be presented for each of the others.
These mechanisms interact with each other, with secondary advantages as early effects reduce costs to the mother, and mitigate what Muller [5] called “Our Load of Mutations” [6].
A basic problem
Albertini [7] noted how, over 65 years ago, “leading experts on animal reproduction who together first queried the apparent futility of human reproduction relative to the most thoroughly studied animal models of the day that included domesticated species, non-human primates and guinea pigs.” Baboons, generally a good model for human reproduction, can show close to 80% successes [8], compared to about 30% for humans [9, 10], or less.
Human studies typically involve selected and “presumably fertile couples” [9], creating a bias towards favorable outcomes, thereby underestimating reproductive failures. And here, chance, as with linkages to advantageous genes, or random genetic drift, is unlikely with multiple common hereditary mechanisms such as endometriosis [11], polycystic ovary disease [12], and polymorphisms affecting maternal mitotic stability [13] and folate metabolism [14]. Additionally, aneuploidy, the primary cause of conceptual losses, involves multiple system defects, including some that are transitory, and are exceptional later [15, 16], going against inevitable system flaws.
It should also be noted that infertility, a failure to conceive after a defined length of time that does not preclude future pregnancies, has a variety of different definitions [17] but, as used here, simply reflects cited references.
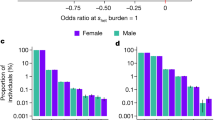
Genetic contributions
Genetic effects on fecundity are common. Endometriosis, with 30 to 50% infertility, affects 6–10% of women [18], and has a genetic component of close to 50% [11, 19]. A genome-wide association meta-analysis showed “remarkable consistency... with little evidence of population-based heterogeneity,” and stronger genetic associations with more severe difficulties [20]. Similarly, polycystic ovary syndrome includes infertility in 40% of affected women, plus increased spontaneous abortions. Prevalence varies according to criteria, and an estimate of 4–8% of women of reproductive age may actually be low [12].
After conception, a polymorphic allele significantly reduces preblastocyst survival, with 20 to 45% population frequencies indicating long-term balancing selection [13]. A meta-analysis found significant associations of 53 polymorphisms in 37 genes with recurrent miscarriages, so that “over-active immunological responses, thrombophilia, abnormal placental function, and disturbance of metabolic regulation may be implicated” [21]. Both of the metabolic genes involved folate, which can affect fertility as well as pregnancy outcomes. In one of these, methylenetetrahydrofolate reductase (MTHFR), common polymorphisms affect fertility [22], while a maternal allele may increase preterm birth and low birth weight [23].
There are also genetic components for common traits with pre- and/or perinatal morbidity and mortality. Preterm delivery before 37 weeks of gestation, mostly spontaneous, occurs in 9.6% of US pregnancies, and “is the leading cause of death in neonates and children under the age of 5 years... studies suggest that 30 to 40% of the variation in birth timing and in the risk of preterm birth arises from genetic factors that largely but not exclusively reside in the maternal genome.” Similarly, a genome-wide association study showed a role for several common gene variants here, apparently acting through the maternal rather than the fetal genome [24].
Maternal imprinting reduces fetal size [25], and several Mendelian variants have negative growth effects, mostly acting through the mother [26], a point we will return to later.
Intrinsic factors include repeated chaotic embryo divisions in some women but not others [27], and impaired endometrial stromal cell decidualization with recurrent pregnancy loss in about 1% of women [28].
Gene-specific hypotheses with varying degrees of support have been offered for polymorphisms [2, 13, 22], but some shared advantage related to fecundity may be responsible instead. Varying polymorphism frequencies suggest connections to recent acute population issues.
Aneuploid effects
Further evidence against chance comes from multiple mitotic and meiotic defects related to aneuploidy, the most common cause of prenatal losses.
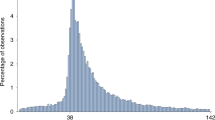
Mitotic errors in the cleavage stage result in aneuploid clones at least 30% of the time [29]. These involve cell cycle issues that reflect maternal controls prior to embryo system activation, with weakened G1, G2, and spindle assembly checkpoints, centrosome abnormalities, and chromatid cohesion failure. These problems quickly resolve and are exceptional later on, supporting a specific relationship to reproduction. The resulting clonal aneuploidy shows binary effects, with common adverse, generally lethal, outcomes, versus a rapid normalization with effective elimination of the abnormal clone [15].
Meiotic effects were originally attributed to nondisjunction, but premature sister chromatid separation is more common, while, “age-independent pathways also promote errors in meiosis, and insensitivity to meiotic checkpoint activation, instability of the meiotic spindle, in addition to defects in homologous recombination likely compound the risk of chromosome segregation errors in oocytes and aneuploidy in embryos” [16].
Maternal connections
Aneuploid and genetic fecundity issues are largely maternal, and evidence supports the ovum as the primary source of epigenetic effects [4]. This predilection is not surprising, since reproductive costs fall mainly on the mother with pregnancy, breast feeding, and child rearing [3]. Early effects, e.g., prior to the recognition of pregnancy, or conception failures, minimize maternal investments, while later events include situations where “mothers, whose very survival is threatened by pregnancy and childbirth, appear to play a crucial role in determining length of gestation and size of baby. Having smaller babies may thus have conferred an advantage to mothers, despite the increased risk to individual offspring” [30].
Therefore, although Turner syndrome and triploidy both contribute significantly to prenatal losses, strong paternal biases in their origins [31, 32] go against a direct relationship to maternal fecundity reductions.
At this point, parental contributions to fecundity reductions are worth noting. While there are often reproductive conflicts between fathers and mothers, as with fetal size [25], this may not be the case here, where quantitative differences are involved instead. That is, many selective advantages for reduced fecundity related to resource limitations are mediated through the offspring, and would affect both parents, even though they would weigh especially heavily on the mother, who would also have greater flexibility in terms of prenatal responses.
With this, similar but milder effects in men would actually be expected, especially when acute limitations on resources are involved, and male fecundity is related to levels of multiple nutrients. Although these are diverse, folate is certainly involved [33]. While a full discussion is beyond the scope of this paper, as one indication of this, a meta-analysis showed a significant paternal fertility effect from the folate related MTHFR C677T polymorphism [34], which also has adverse fetal effects through the mother [23].
Aneuploidy and evolutionary adaptations
Since fewer offspring can be advantageous in a variety of situations, different adaptations may reflect different issues. And here, mechanisms can be invariant, or they can respond to the maternal and/or fetal environment. Also, while chromosomal effects are biologically “hard-wired” and uniform, suggesting a long established fundamental role, genetic polymorphisms vary widely in populations, consistent with more recent circumstantial fine-tuning.
Aneuploidy-related losses decrease reproductive potentials that, as suggested by the baboon model [8], could more than double fecundity, creating potentially unsustainable demands on resources [35]. And again, typical chromosomal losses very early in pregnancy [36], reduce maternal costs.
This would have been particularly important in early human evolution in the East African Rift, where specific climate issues alternated periods of plenty with scarcities. Here, pulsed climate variability hypothesis reconstructions indicate that a “long-term drying trend in East Africa was punctuated by episodes of short alternating periods of extreme humidity and aridity which may have driven hominin speciation” [37].
Increased resources would support shortened interbirth intervals during this time [37] but, as periods of aridity interposed scarcities, reproductive costs would rise, with “substantial evidence that shorter interbirth intervals increase child mortality” [38], with two main contributions: (1) maternal physiologic and nutritional depletion from pregnancy, parturition, and breastfeeding and (2) sibling competition for resources [39]. As a result, decreased intervals from times of plenty would need to be adjusted, while contracted populations would facilitate adaptive gene fixation [40].
Along with this, structural changes show the emergence of a uniquely human cooperative phenomenon [41] perhaps best called “biocultural reproduction” [42]. Here, “Negotiation of the bipedal pelvis requires a series of rotations, the end of which has the infant emerging from the birth canal facing the opposite direction from the mother. This pattern, strikingly different from what is typically seen in monkeys and apes, places a premium on having assistance at delivery” [43].
With this, although advantages in other areas could follow, increased reproductive successes could outpace concomitant resource extensions, supporting continued selection for decreased fertility, and creating long-term selective pressures for modifying reproductive rates.
As opposed to mitotic aneuploidy, meiotic issues are directly related to maternal age [15]. And here, a rapid increase in abnormalities in women (but not in males [44]) beginning at around 35 years of age, roughly when infertility starts becoming more common [15], is consistent with a relatively early menopause compared to other primates, as risks and costs increase with age [45], and it is notable that human patterns of reproductive senescence before death appear to be unique among primates [46].
This may also involve the grandmother hypothesis, which postulates a shift from “independent mothering... when drying and more seasonal environments reduced the availability of foods that just-weaned juveniles could handle” [47], a reduction ameliorated by contributions from the mother’s mother. With this, advantages from continued pregnancies with accompanying risks were counterbalanced by benefits from decreased fertility with increased survival to support grandchildren. Assuming that early human reproduction began at age 15, with 3 years for weaning, a grandmother would begin to accrue benefits at about 33 years of age, with added later advantages as more grandchildren were born—a scenario roughly consistent with the timing of increasing meiotic losses, although other explanations are certainly possible.
Finally, mitotic and meiotic aneuploidy can interact [15, 48], increasing their overall impact.
Epigenetic effects on fecundity
The aneuploid effects discussed are, to my knowledge, consistently the same and stable in all studied populations. However, acute resource fluctuations, as with more than 10-fold variations in preindustrial agricultural yields [49] would create advantages for rapid and flexible reproductive compensations. Since shortages can arise at any time prior to, or during a pregnancy, and can last for varying periods of time, fecundity limitations would be advantageous in several situations: (1) prior to conception; (2) early in gestation, with improvements later in pregnancy; (3) early in gestation, and continuing throughout pregnancy; (4) finally, even though maternal costs increase as a pregnancy progresses, losses may become advantageous late in pregnancy.
Overall, an ideal mechanism would involve feedback on resource availability along with maternal responses adjusted to circumstances. These specifications are nicely met through epigenetic interactions, as gene expression is modified after conception. Further aspects are discussed elsewhere, with an emphasis, continued here, on DNA methylation, which is far from the only mechanism involved, but which is certainly the best studied [4].
For a start, chromatin acts as a “nutrient sensor,” so that “dietary availability of methyl donors has an impact on the patterns of gene expression by affecting DNA methylation at regulatory regions” [50]. This can affect fertility and fetal vulnerabilities throughout pregnancy through an association related to 1-carbon metabolism issues, and especially folic acid, that links early and late pregnancy losses, prematurity, growth delays, perinatal difficulties, parental fertility issues, and other adversities as well, with both intrinsic and extrinsic contributions. The primary defect arises in the ovum and reflects decreased folate availability [4].
This explains certain genetic influences, such as MTHFR “gene variants associated with lower ovarian reserves, diminished response to follicular stimulation, and reduced live birth after in vitro fertilization… imbalances in folate metabolism and related gene variants may impair female fecundity as well as compromise implantation and the chance of a live birth” [51].
Maternal periconception 1-carbon metabolism affected embryonic growth and development [52, 53], and folate, prior to conception, reduced growth delays, preterm births [54, 55], and adverse perinatal outcomes [56], and was linked to fecundability [57].
However, since epigenetic methylation continues during pregnancy, ongoing folate deficiencies can affect the fetus, especially if already compromised. In one study, improved perinatal outcomes occurred only with folate before conception and continuing beyond 12 weeks of pregnancy [56] supporting both early and late effects. These timing issues might explain mixed findings with folate intervention studies [58]. Higher maternal folate has also been associated with reductions in spontaneous abortions [59], preterm births, and low birth weights [60].
Likely population effects occurred with a 1944–1945 Dutch famine, with “markedly reduced... conceptions resulting in birth” after about 2 months, with immediate recovery with adequate food [61]. Less severe limitations also have effects, e.g., increases in small infants and prematurity with seasonal scarcities in The Gambia [62].
Interactions with aneuploidy are also possible, e.g., a reduced folate carrier (RFC-1) A80G gene polymorphism may increase maternal age related risks, with added adverse effects from maternal folate deficiencies [63].
While epigenetic effects related to resource availability are not limited to humans [64], there is a paucity of animal data for comparison with extensive information on humans, e.g., population effects of folic acid levels and availability, and of supplementation. Still, while epigenetic adaptations were undoubtedly selected for in early East African evolution in primates in general, this would have been relaxed in other primates once climates stabilized, but intensified in humans with the development of agriculture.
Our load of mutations
A final consideration in the persistence and extent of epigenetic issues involves what Muller called “Our Load of Mutations,” where accumulating deleterious mutations reduce population fitness. While the costs here are uncertain, they are, in theory at least, substantial [5]. However, epigenetic effects related to reproductive limitations may reduce costs, providing a significant secondary advantage.
In particular, by facilitating adverse outcomes [4], epigenetic disruptions would lower the age of prenatal loss, decreasing mutation costs [6]. This would occur by disturbing canalization, a developmental buffering of environmental and genetic perturbations that tends to break down with extremes, culling even cryptic mutations [65]. With indications “that many developmental and metabolic phenotypes are threshold traits” [66], even small genetic effects could be exaggerated. Pleiotrophic and epistatic effects would also make adverse issues more than just additive as mutation numbers increase, and copy number variants of methylated genes should also be particularly sensitive to epigenetic issues.
Lethality, preterm delivery, and malformations, which are all part of the epigenetic association cited above [4], could obscure even major selective effects: e.g., a combination of a 20% added unrecognized pregnancy lethality, 10% more miscarriages and stillbirths, 10% added prematurity losses, plus a 5% perinatal lethality with different malformations, would be difficult to distinguish from background.
While Muller argued for a relaxation of natural selection in humans, the findings discussed here suggest that it is still a potent force. However, they also indicate that much of the impact has shifted to issues of fecundity, and may, in fact, be even more intense than ever, justifying the highly ineffective human reproductive process noted at the start of the paper.
Conclusions
Human reproductive inefficiencies are remarkably common, and multiple mechanisms, some with genetic components, indicate more than just chance. Evolutionary history supports selective advantages with fewer offspring, but better overall survival, in diverse circumstances, resulting in a complex series of mechanisms arising from different situations.
Early on, periodic unfavorable climates caused repeated resource reductions, while later rapid biocultural advances in more favorable environments let reproduction outpace resources. Compensation here involved mitotic aneuploidy, which is unaffected by extrinsic factors and shows very early lethality.
At the same time, the evolution of grandmaternal involvement in resource provision added advantages for their increased survival through fertility limitations at older maternal ages. And here, selection favored meiotic aneuploidy, which shared the crucial features of the mitotic form, but depended upon maternal age, which the other did not. This is responsible for the apparently unique rapid human female loss of fertility after 35 years of age, with reproductive senescence significantly preceding death.
In these situations, early losses incidentally lowered mutation load burdens and minimized maternal costs. However, sporadic, often random, scarcities accompanying the development of agriculture supported compensatory reproductive limitations at all stages of pregnancy, and responses to exogenous factors. This was accomplished through epigenetic effects primarily involving DNA methylation, while genetic polymorphisms probably involve recent population-dependent issues.
Overall, these evolutionary considerations help make sense of an otherwise confusing array of human reproductive inefficiencies and support a shift in much of human selection to fecundity-related issues without the relaxation suggested by Mulleer [5].
References
Jarvis GE. 2016. Estimating limits for natural human embryo mortality [version 1. F1000Research 2016, 5:2083 Last updated: 30 AUG 2016.
Day FR, Hinds DA, Tung JY, Stolk L, Styrkarsdottir U, Saxena R, et al. Causal mechanisms and balancing selection inferred from genetic associations with polycystic ovary syndrome. Nat Commun. 2015;6:8464.
Low BS. Fertility. Life history and ecological aspects. In: Fisher M, Garcia JR, Chang RS, editors. Evolution’s empress: Darwinian perspectives on the nature of women. NY: Oxford University Press; 2013. p. 222–42.
Lubinsky M. An epigenetic association of malformations, adverse reproductive outcomes, and fetal origins hypothesis related effects. J Assist Reprod Genet. 2018;35:953–64. https://doi.org/10.1007/s10815-018-1197-2.
Muller HJ. Our load of mutations. Am J Hum Genet. 1950;2:111–76.
Knudson AG Jr. Presidential address. Our load of mutations and its burden of disease. Am J Hum Genet. 1979;31:401–13.
Albertini DF. Explaining the futility of the reproductive process in humans: past, present, and future. J Assist Reprod Genet. 2017;34:157–8.
Stevens VC. Some reproductive studies in the baboon. Hum Reprod Update. 1997;3:533–40.
Zinaman MJ, Clegg ED, Brown CC, O’Connor J, Selevan SG. Estimates of human fertility and pregnancy loss. Fertil Steril. 1996;65:503–9.
Wang X, Chen C, Wang L, Chen D, Guang W, French J. Conception, early pregnancy loss, and time to clinical pregnancy: a population-based prospective study. Fertil Steril. 2003;79:577–84.
Saha R, Pettersson HJ, Svedberg P, Olovsson M, Bergqvist A, Marions L, et al. Heritability of endometriosis. Fertil Steril. 2015;104:947–52.
Barthelmess EK, Naz RK. Polycystic ovary syndrome: current status and future perspective. Front Biosci (Elite Ed). 2014;6:104–19.
McCoy RC, Demko Z, Ryan A, Banjevic M, Hill M, Sigurjonsson S, et al. Common variants spanning PLK4 are associated with mitotic-origin aneuploidy in human embryos. Science. 2015;348:235–8.
Cao Y, Zhang Z, Zheng Y, Yuan W, Wang J, Liang H, et al. The association of idiopathic recurrent early pregnancy loss with polymorphisms in folic acid metabolism-related genes. Genes Nutr. 2014;9:1–8.
McCoy RC. Mosaicism in preimplantation human embryos: when chromosomal abnormalities are the norm. Trends Genet. 2017;33:448–63.
Webster A, Schuh M. Mechanisms of aneuploidy in human eggs. Trends Cell Biol. 2017;27:55–68.
Jacobson MH, Chin HB, Mertens AC, Spencer JB, Fothergill A, Howards PP. “Research on infertility: definition makes a difference” revisited. Am J Epidemiol. 2017;187:337–46.
Bulletti C, Coccia ME, Battistoni S, Borini A. Endometriosis and infertility. J Assist Reprod Genet. 2010;27:441–7.
Treloar SA, O’Connor DT, O'Connor VM, Martin NG. Genetic influences on endometriosis in an Australian twin sample. Fertil Steril. 1999;71:701–10.
Rahmioglu N, Nyholt DR, Morris AP, Missmer SA, Montgomery GW, Zondervan KT. Genetic variants underlying risk of endometriosis: insights from meta-analysis of eight genome-wide association and replication datasets. Hum Reprod Update. 2014;20:702–16.
Shi X, Xie X, Jia Y, Li S. Maternal genetic polymorphisms and unexplained recurrent miscarriage: a systematic review and meta-analysis. Clin Genet. 2017;91:265–84.
Enciso M, Sarasa J, Xanthopoulou L, Bristow S, Bowles M, Fragouli E, et al. Polymorphisms in the MTHFR gene influence embryo viability and the incidence of aneuploidy. Hum Genet. 2016;135:555–68.
Wu H, Zhu P, Geng X, Liu Z, Cui L, Gao Z, et al. Genetic polymorphism of MTHFR C677T with preterm birth and low birth weight susceptibility: a meta-analysis. Arch Gynecol Obstet. 2017;295:1105–8.
Zhang G, Feenstra B, Bacelis J, Liu X, Muglia LM, Juodakis J, et al. Genetic associations with gestational duration and spontaneous preterm birth. N Engl J Med. 2017;377:1156–67.
Moore GE, Ishida M, Demetriou C, Al-Olabi L, Leon LJ, Thomas AC, et al. The role and interaction of imprinted genes in human fetal growth. Philos Trans R Soc Lond B. 2015;370:20140074.
Beaumont RN, Warrington NM, Cavadino A, Tyrrell J, Nodzenski M, Horikoshi M, et al. Genome-wide association study of offspring birth weight in 86,577 women identifies five novel loci and highlights maternal genetic effects that are independent of fetal genetics. Hum Mol Genet. 2018;27(4):742–56.
Delhanty JD, Harper JC, Ao A, Handyside AH, Winston RM. Multicolour FISH detects frequent chromosomal mosaicism and chaotic division in normal preimplantation embryos from fertile patients. Hum Genet. 1997;99:755–60.
Coulam C. What about superfertility, decidualization, and natural selection? J Assist Reprod Genet. 2016;33:577–80.
Munné S, Wells D. Detection of mosaicism at blastocyst stage with the use of high-resolution next-generation sequencing. Fertil Steril. 2017;107:1085–91.
Basso O. Reproductive epidemiology in an evolutionary perspective: why bigger may not be better. Curr Epidemiol Rep. 2014;1:98–101.
Zaragoza MV, Surti U, Redline RW, Millie E, Chakravarti A, Hassold TJ. Parental origin and phenotype of triploidy in spontaneous abortions: predominance of diandry and association with the partial hydatidiform mole. Am J Hum Genet. 2000;66:1807–20.
Zhong Q, Layman LC. Genetic considerations in the patient with Turner syndrome—45, X with or without mosaicism. Fertil Steril. 2012;98:775–9.
Salas-Huetos A, Bulló M, Salas-Salvadó J. Dietary patterns, foods and nutrients in male fertility parameters and fecundability: a systematic review of observational studies. Hum Reprod Update. 2017;23:371–89.
Hong HH, Hu Y, Yu XQ, Zhou L, Lv MQ, Sun Y, et al. Associations of C677T polymorphism in methylenetetrahydrofolate reductase (MTHFR) gene with male infertility risk: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2017;212:101–9.
Malthus TR. An essay on the principle of population or a view of its past and present effects on human happiness; with an inquiry into our prospects respecting the future removal or mitigation of the evils which it occasions. 6th ed. London: John Murray; 1826.
van den Berg MM, van Maarle MC, van Wely M, Goddijn M. Genetics of early miscarriage. Biochim Biophys Acta. 1822;2012:1951–9.
Maslin MA, Shultz S, Trauth MH. A synthesis of the theories and concepts of early human evolution. Philos Trans Roy Soc Lond B: Biol Sci. 2015;370:20140064.
Stulp G, Barrett L. Fertility theory: theory of life history evolution. In: Wright J, editor. The International Encyclopedia of the Social and Behavioral Sciences. 2nd ed: Elsevier; 2015.
Koenig MA, Phillips JF, Campbell OM, D'Souza S. Birth intervals and childhood mortality in rural Bangladesh. Demography. 1990;27:251–65.
Waxman D. A unified treatment of the probability of fixation when population size and the strength of selection change over time. Genetics. 2011;188:907–13.
Burkart JM, Hrdy SB, Van Schaik CP. Cooperative breeding and human cognitive evolution. Evol Anthropol. 2009;18:175–86.
Bogin B, Bragg J, Kuzawa C. Humans are not cooperative breeders but practice biocultural reproduction. Ann Hum Biol. 2014;41:368–80.
Trevathan W. Primate pelvic anatomy and implications for birth. Philos Trans R Soc B. 2015;370:20140065.
Donate A, Estop AM, Giraldo J, Templado C. Paternal age and numerical chromosome abnormalities in human spermatozoa. Cytogenet Genome Res. 2016;148:241–8.
Shanley DP, Kirkwood TB. Evolution of the human menopause. BioEssays. 2001;23:282–7.
Alberts SC, Altmann J, Brockman DK, Cords M, Fedigan LM, Pusey A, et al. Reproductive aging patterns in primates reveal that humans are distinct. Proc Natl Acad Sci. 2013;110(33):13440–5.
Hawkes K. Genomic evidence for the evolution of human postmenopausal longevity. Proc Natl Acad Sci. 2016;113:17–8.
Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2:280–91.
Holopainen J, Helama S. Little ice age farming in Finland: preindustrial agriculture on the edge of the Grim Reaper’s scythe. Hum Ecol. 2009;37:213–25.
Navarro E, Funtikova AN, Fíto M, Schröder H. Prenatal nutrition and the risk of adult obesity: long-term effects of nutrition on epigenetic mechanisms regulating gene expression. J Nutr Biochem. 2017;39:1–4.
Laanpere M, Altmäe S, Stavreus-Evers A, Nilsson TK, Yngve A, Salumets A. Folate-mediated one-carbon metabolism and its effect on female fertility and pregnancy viability. Nutr Rev. 2010;68:99–113.
Parisi F, Rousian M, Koning AH, Willemsen SP, Cetin I, Steegers EA, et al. Periconceptional maternal biomarkers of one-carbon metabolism and embryonic growth trajectories: the Rotterdam Periconceptional Cohort (Predict Study). Fertil Steril. 2017;107:691–8. e1
Parisi F, Rousian M, Koning AH, Willemsen SP, Cetin I, Steegers-Theunissen RP. Periconceptional maternal one-carbon biomarkers are associated with embryonic development according to the Carnegie stages. Hum Reprod. 2017; https://doi.org/10.1093/humrep/dew349.
Hodgetts VA, Morris RK, Francis A, Gardosi J, Ismail KM. Effectiveness of folic acid supplementation in pregnancy on reducing the risk of small-for-gestational age neonates: a population study, systematic review, and meta-analysis. BJOG. 2015;122:478–90.
Zheng JS, Guan Y, Zhao Y, Zhao W, Tang X, Chen H, et al. Pre-conceptional intake of folic acid supplements is inversely associated with risk of preterm birth and small-for-gestational-age birth: a prospective cohort study. Br J Nutr. 2016;115:509–16.
De-Regil LM, Fernández-Gaxiola AC, Dowswell T, Peña-Rosas JP. Effects and safety of periconceptional folate supplementation for preventing birth defects. Cochrane Libr. 2010;
Cueto HT, Riis AH, Hatch EE, Wise LA, Rothman KJ, Sørensen HT, et al. Folic acid supplementation and fecundability: a Danish prospective cohort study. Eur J Clin Nutr. 2016;70:66–71.
Abu-Saad K, Fraser D. Maternal nutrition and birth outcomes. Epidemiol Rev. 2010;32:5–25.
Gaskins AJ, Rich-Edwards JW, Hauser R, Williams PL, Gillman MW, Ginsburg ES, et al. Maternal prepregnancy folate intake and risk of spontaneous abortion and stillbirth. Obstet Gynecol. 2014;124:23–31.
Rogne T, Tielemans MJ, Chong MF, Yajnik CS, Krishnaveni GV, Poston L, et al. Maternal vitamin B12 in pregnancy and risk of preterm birth and low birth weight: a systematic review and individual participant data meta-analysis. Am J Epidemiol. 2017;185:212–23.
Stein Z, Susser M. Fertility, fecundity, famine: food rations in the Dutch famine 1944/5 have a causal relation to fertility, and probably to fecundity. Hum Biol. 1975;47:131–54.
Moore SE. Early life nutritional programming of health and disease in The Gambia. J Dev Orig Health Dis. 2016;7:123–31.
Suresh RV, Udupa AS, Lingaiah K, Polapalli SK, Ramachandra NB. Association of RFC1 A80G gene polymorphism with advanced maternal age in risk of Down syndrome. Curr Med Res Practice. 2017;7:6–10.
Waterland RA. Epigenetic mechanisms affecting regulation of energy balance: many questions, few answers. Annu Rev Nutr. 2014;34:337–55.
Siegal ML, Bergman A. Waddington’s canalization revisited: developmental stability and evolution. Proc Natl Acad Sci. 2002;99:10528–32.
Yeyati PL, van Heyningen V. Incapacitating the evolutionary capacitor: Hsp90 modulation of disease. Curr Opin Genet Dev. 2008;18:264–72.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lubinsky, M. Evolutionary justifications for human reproductive limitations. J Assist Reprod Genet 35, 2133–2139 (2018). https://doi.org/10.1007/s10815-018-1285-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1285-3