Abstract
Objective
Attention-deficit hyperactivity disorder (ADHD) is a psychiatric disorder characterized by symptoms of inattention, hyperactivity, and impulsivity. Stimulant medication is the main pharmacological treatment for ADHD. However, the traditional pharmacological treatments may have significant side effects; therefore, non-pharmacological approaches are needed. Thus, there has been growing interest in alternative herbal treatments. The aim of this review was to comprehensively assess the current evidence for plant-based treatment of ADHD in human and animal models, as well as their ability to modulate the inflammatory process.
Methods
This study was an integrative review of the current evidence for the plant-based treatment of ADHD. The research involved using literature available on PubMed and Scopus databases.
Findings
Spontaneously hypersensitive rats treated with baicalin exhibited significant reductions in locomotion, increased spatial learning skills, and increased levels of dopamine in the striatum. Supplementation with Sansonite improved memory and attention capacity. In human studies, Ginkgo biloba significantly improved the symptoms of inattention and reduced memory impairment. In studies conducted using Korean Red ginseng, Klamath, and Crocus sativus L., the patients showed significant improvements in symptoms of inattention and hyperactivity/impulsivity. Furthermore, we demonstrated that the identified plants modulate the inflammatory process through pro-inflammatory and anti-inflammatory cytokines, nitric oxide, Th cells, Toll-like receptor 4, and mitogen-activated protein kinases.
Conclusion
All the studies included in this review focused on plants with demonstrated potential against inflammatory processes, positioning them as promising candidates for ADHD treatment, due to their potential to attenuate or even prevent neuroinflammatory mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention deficit hyperactivity disorder (ADHD) is a common neurodevelopmental disorder characterized by symptoms of inattention, hyperactivity, and impulsivity (APA 2013). Epidemiological data indicate that the global prevalence of ADHD is approximately 5.3% among children aged below 18 years (Polanczyk et al. 2007). Although it initiates in childhood, it is common for symptoms to persist into adulthood, leading to social, academic, and professional impairments (Mash and Barkley 2003).
ADHD is a multifactorial disorder, and several genetic and environmental factors have already been implicated in its pathophysiology (Faraone et al. 2015). Beyond traditional neurotransmitter theories, a substantial body of evidence suggests a potential role for neuroinflammation in the development of ADHD. In this context, epidemiological studies have consistently revealed a significant overlap between ADHD and inflammatory and autoimmune disorders; numerous studies have evaluated serum inflammatory markers in individuals with ADHD; and genetic studies have identified polymorphisms in genes related to inflammatory pathways that may contribute to the disorder (Dunn et al. 2019; Leffa et al. 2018; Verlaet et al. 2018; Chang et al. 2021; Chen et al. 2022).
Furthermore, various environmental factors associated with heghtened inflammation, such as maternal exposure to infections (Werenberg Dreier et al. 2016), smoking during pregnancy (Silva et al. 2014; Thapar et al. 2013), maternal obesity (Andersen et al. 2018; Chen et al. 2014; Rijlaarsdam et al. 2017; Sanchez et al. 2018), and maternal exposure to toxic agents (Thapar et al. 2013) have also been linked to an increased risk of ADHD. These environmental risk factors contribute to the creation of a uterine environment characterized by elevated inflammatory activity (Shankar et al. 2011; Terasaki and Schwarz 2016), thereby supporting the theory that exposure to inflammation during developmental phases may trigger neuroinflammatory processes (Shankar et al. 2011; Terasaki and Schwarz 2016).
The primary pharmacological treatment for ADHD involves the use of central nervous system (CNS) stimulant drugs, such as methylphenidate (MPH), which increases the intrasynaptic concentrations of dopamine (DA) and norepinephrine (NE) (Faraone et al. 2015). MPH stand as a first-line drug (Fredriksen et al. 2014; Surman et al. 2013) and numerous meta analyses have consistently demonstrated its efficacy and safety (Faraone et al. 2004; Koesters et al. 2009).
However, despite the well-stablished benefits of MPH in attenuating the core symptoms of ADHD, a significant portion of patients (approximately 30%) do not experience positive responses to this treatment (Spencer et al. 1996). Moreover, reports of adverse effects, including reduced appetite and sleep disturbances, are more prevalent among children and adolescents using MPH (White et al. 2014). Additionally, it is also necessary to monitor the psychiatric status, cardiovascular function, and growth of individuals undergoing MPH treatment for potential issues such as increased blood pressure, the emergence or exacerbation of psychotic or manic disorders, the development of motor or verbal tics, and mild growth suppression (Hennissen et al. 2017; Krinzinger et al. 2019).
So, considering the complexity associated with ADHD/MPH treatment, there is a growing need for the development of new or complementary treatment approaches, especially for children (Ghuman and Ghuman 2013). In this context, there has been a growing interest in herbal medicines since numerous studies have demonstrated the therapeutic potential of natural compounds in mitigating various brain disorders (Sharifi-Rad et al. 2020; Silva et al. 2019). The beneficial effects of phytochemicals can be attributed to a range of biological mechanisms, which include antioxidant and anti-inflammatory activities (Pan et al. 2011).
However, controlled trials investigating the efficacy of herbal medicines for treating ADHD remain relatively scarce. While some natural compounds show promise, the existing body of scientific research is limited in number and sometimes exhibit methodological inadequacies (Sarris et al. 2011). Therefore, the objectives of this study were: (1) to comprehensively review the current evidence concerning the use of herbal medicines in the treatment of ADHD, both in human subjects and animal models, and (2) to compile the anti-inflammatory properties of herbal medicines already explored in the context of ADHD. If neuroinflammation plays a role in the pathogenesis of ADHD, anti-inflammatory treatments may offer a promising avenue for therapeutic exploration.
Methodology
This study is an integrative bibliographical review of the current evidence for herbal treatments to treat ADHD. The guiding question of this research was, "Which natural products and/or plants have already been used to treat patients with ADHD and/or the animal models for ADHD?"
Data were collected between June and December 2022 from the National Library of Medicine (PubMed) and Scopus databases. The search strategy used the combination of these keywords: "ADHD and natural products"; "ADHD and Plants"; "ADHD and Animal model"; "ADHD and Herbal drug"; "Natural products and Animal model for ADHD"; "Plants and Animal model for ADHD "; and "Herbal drug and Animal model for ADHD.”
The inclusion criteria were as follows: (i) articles published between 2012 and 2022; (ii) research articles; and (iii) randomized clinical or experimental studies with animal models. The exclusion criteria were as follows: (i) revisions and (ii) studies that did not involve plants or products of plant origin. In addition, duplicate articles were excluded from analysis. In the data collection process, 985 articles were obtained, among which only 10 were used for this review.
The titles and abstracts of all articles obtained from the electronic search were reviewed and studies that met the inclusion criteria were obtained in an integral manner. The stages of the bibliographic research are shown in Fig. 1.
Besides, in addition to conducting a comprehensive review of the 10 selected articles, we conducted a focused search to identify studies that evaluated the anti-inflammatory effects of the identified plants.
Results
A total of 985 research papers from literature were obtained through bibliographical research. After excluding studies that were duplicates, reviews, those that did not involve plants or products of plant origin, and those focused only on pharmacological interventions, 28 articles were selected. After the first selection, the abstracts of the selected articles were read and 18 were excluded for being non-randomized clinical trials (eight articles), combination products (six articles), no benefit (three articles), studies in in vitro models (two articles). In total, ten studies were included in the review because they met our inclusion criteria. Following a comprehensive review of the 10 articles (Table 1), we subsequently focused on a total of 8 plant species for which we identified the more recent original articles that illustrate their impacts on inflammatory processes (Table 2).
Moving forward, we will present the studies and their respective plants investigated in the past decade for the treatment of ADHD, highlighting how these plants act to modulate the inflammatory process.
Interventions herbs
Bacopa monnieri
Bacopa monnieri (BM), belonging to the family Scrophulariaceae, is a creeping herb growing in wet and swampy areas in the Indian subcontinent. Bacopa has been used for approximately 3000 years in ayurvedic medicine to improve memory and intellect (Gohil and Patel 2010). In addition to modulating the monoaminergic system, BM improves oxidative status, thus protecting the nervous system from oxidative stress and neuronal cell death (Shinomol et al. 2012; Sheikh et al. 2007) and displaying adaptogenic properties (Sheikh et al. 2007). Bacopa is currently recognized for its potential effects in the treatment of mental illnesses and epilepsy (Dhawan and Singh 1996). Several phytochemical studies have shown that BM contains numerous active constituents, including alkaloids, betulin acid, stigmasterols, saponins, and sitosterols; however, the primary components are steroidal saponins and bacosides A and B (Chatterji et al. 1965).
Dave et al. (2014) investigated the effectiveness of the BM extract on ADHD symptoms in children. This open-label clinical trial included 31 children aged 6–12 years diagnosed with ADHD according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). The intervention included a 225 mg/day dose of BM extract administered for 6 months. The Parent Rating Scale was used to assess the baseline and end-of-study ADHD symptom scores. Treatment with BM for 6 weeks significantly reduced the subtest scores for ADHD symptoms, except for social problems. Symptom scores for restlessness and self-control reduced, along with improvement in attention deficit symptoms, learning problems, impulsivity, and psychiatric problems (Dave et al. 2014). The authors concluded that the standardized BM extract was effective in controlling ADHD symptoms and was well-tolerated by children. Randomized, double-blind, placebo-controlled clinical trials are currently underway (Kean et al. 2015). Kean et al. (2022) presented the first results of their study on BM for the treatment of children diagnosed with ADHD. Treatment with BM (CDRI 08 standardized to 55% bacosides) was administered for 14 weeks at the following doses: 1 × 160 mg CDRI 08, 2 × 160 mg CDRI 08, or placebo per day. After 14 weeks, no improvement in ADHD symptoms was observed; however, processing speed and cognitive flexibility improved, along with an improvement in mood and sleep quality (Kean et al. 2022). Thus, researchers claim that limitations with dropouts and external factors, such as physical exercise, may have altered the study outcomes and thus necessitated further studies.
Bacopa monnieri—inflammatory processes
Saini et al. (2019) aimed to assess whether BM prevented colchicine-induced inflammation and Aβ production. To demonstrate the effect, Wistar rats were induced into dementia through a single intracerebroventricular injection of colchicine (15 μg/5 μl), while BM extract was orally administered (50 mg/kg body weight, daily) for 15 days. A significant increase in pronounced nitric oxide (NO) production was observed, along with an elevation in the expression of cytokines IL-6, TNF-α, and chemokine MCP-1, as well as COX-2 and iNOS expression induced by colchicine. On the other hand, BM supplementation was able to attenuate all inflammatory markers in the animals' brain regions. Nemetchek et al. (2017) investigated BM's ability to inhibit the release of pro-inflammatory cytokines from the murine microglial cell lineage N9, originally derived from CBA mice. Multiple BM extracts were prepared and tested to determine whether they inhibited TNF-α and IL-6 release, as well as acted as inhibitors of caspase-1 and matrix metalloproteinase-3 (enzymes associated with inflammation), and caspase-3. Findings showed that different preparations, including tea infusions, alkaloid extracts of bacopa, as well as Bacoside A, significantly inhibited the release of TNF-α and IL-6, and effectively inhibited caspases 1 and 3, along with matrix metalloproteinase-3, in the cell-free assay. Lastly, Abhishek et al. (2022) assessed the neuroprotective effect of BM in an experimental model of autism spectrum disorder (ASD) in Wistar rats and explored its mechanism of action. For this, acid was administered at a dose of 600 mg/kg to mimic the ASD model. BM was tested at concentrations of 20, 40, and 80 mg/kg, and inflammatory cytokines IL-1β, IL-6, IL-10, TNF-α were evaluated. The results indicated that BM exhibits anti-inflammatory properties (at a concentration of 80 mg/kg), reducing IL-1β, IL-6, TNF-α levels.
Scutellariae baicalensis
For more than 2000 years, the root of Scutellariae baicalensis has been used in East Asia for therapeutic purposes, to treat diarrhea, vomiting, menstrual complications, hepatitis, diabetes, and hypertension. The main bioactive compound of the plant is baicalin, obtained from its dried root (Shang et al. 2010). Furthermore, it has been used as an anti-allergic, anti-inflammatory, and antibacterial agent to treat inflammatory and allergic diseases (Sun et al. 2013).
Several in vivo and in vitro studies have analyzed the potential protective effects of baicalin against oxidative injuries (Yin et al. 2011), improvements in memory impairment (Chen et al. 2015), and learning (Xiong et al. 2014). Another study using baicalin showed a significant increase in the gene and protein expression levels of antioxidant enzymes (Ding et al. 2015). Due to these potential effects, some studies have analyzed baicalin and substantiated its potential in treating the primary symptoms of ADHD.
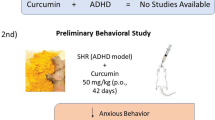
Zhou et al. (2017) evaluated the effect of baicalin treatment in vivo (spontaneously hypersensitive rats [SHR] and Wistar Kyoto models for ADHD) at three concentrations (3.33, 6.67, and 10 mg/mL) twice daily for 4 weeks. Hyperactivity and impulsivity were evaluated using the open-field test and Morris Water Maze. Eventually, they concluded that both baicalin and MPH, which are being used for the treatment of ADHD, can normalize the exercise capacity and learning and memory capacity of SHR, thus controlling the main symptoms of hyperactivity, impulsivity, and inattention from ADHD (Zhou et al. 2017). Moreover, the efficacy of baicalin was dose-dependent, with high doses having the greatest effect on the evaluated parameters. To elucidate the potential mechanism of action of baicalin after testing its therapeutic effects on ADHD in an animal model (SHR and Wistar Kyoto), Zhou et al. (2019) used the theory of dopamine deficit. In this study, SHR were divided into the following five groups: MPH, baicalin (50, 100, or 150 mg/kg), and saline-treated controls. Motor activity, spatial learning, and memory capacity were assessed using the open-field and Morris water maze tests. To elucidate the mechanism of action, the sinaptossomal mRNA and protein expressions of tyrosine hydroxylase (TH), vesicular monoamine transporter 2 (VMAT2), 25 kD molecular mass synaptosome-associated protein (SNAP25), and syntaxin 1a were evaluated. Finally, dopamine levels in the prefrontal cortex (PFC) and striatum were assessed. The results indicated that both MPH and baicalin at doses of 150 mg/kg and 100 mg/kg significantly decreased hyperactivity, improved spatial learning and memory deficits, and increased sinaptossomal mRNA and protein levels of TH, SNAP25, VMAT2, and syntaxin 1a, compared with saline treatment. MPH significantly increased the DA levels in the PFC and striatum, whereas baicalin significantly increased the DA levels in the striatum. Finally, the researchers suggested that baicalin may target the striatum and that the increased levels of DA may be partially attributed to the increased mRNA and protein expression of TH, SNAP25, VMAT2, and syntaxin 1a (Zhou et al. 2019).
Scutellariae baicalensis—inflammatory processes
Jin et al. (2019) aimed to investigate the effects of pre-treatment with baicalin on neuronal protection against microglia-induced neuroinflammation. They used the transgenic mouse model APP (amyloid beta precursor protein)/PS1 (presenilin-1). Baicalin was administered via intragastric route at a dose of 103 mg/kg. The results indicated that baicalin decreased the production of IL-18 and IL-1β proteins, as well as mRNA levels of IL-1β, IL-18, and iNOS. They also observed a reduction in caspase-1 and caspase-3, attenuating cell death, and appeared to inhibit the TLR4/NF-κB signaling pathway. Li et al. (2022) assessed the modulatory effect of baicalin on neuroinflammation in lipopolysaccharide (LPS)-activated BV-2 cells. Cells were treated with baicalin at concentrations of 2.5, 7.5, and 22.5 μM. Results showed that higher concentrations of baicalin led to a decrease in inflammatory mediators such as NO, iNOS, IL-1β, and COX-2. Baicalin also appeared to regulate proteins related to the Toll-like receptor 4 (TLR4)/myeloid differentiation factor 88 (MyD88)/nuclear factor κB (NF-κB) pathway and suppressed the phosphorylation of mitogen-activated protein kinase family proteins (JNK, ERK, and p38). Lastly, Wang et al. (2022) demonstrated the effect of Scutellaria baicalensis in treating psoriasis using an animal model. They utilized Balb/c mice and induced psoriasis with an imiquimod (IMQ) cream. To evaluate the effect of Scutellaria baicalensis, the skin was treated with a dose of 1 g/kg for 5 days, resulting in improvement in evaluated skin parameters. For inflammation assessment, macrophages (RAW264.7 cells) were used, and inflammation was induced by LPS. Cells were treated with baicalin at concentrations of 156 and 625 μg/mL. The results showed a decrease in COX-2, iNOS, NO expression, as well as NF-κB p65 and NF-κB p105.
Crocus sativus L.
Crocus sativus L., also known as saffron, is a perennial herb widely grown in India, Greece, and Iran. The oldest reference for its cultivation is in 2300 BC, and its consumption has increased significantly since then. Saffron is used in traditional Indian medicine as an analgesic and cardioprotective agent for various types of mental illnesses (Alonso et al. 2012). Moreover, turmeric and its constituents inhibit DA and NE reception (Pitsikas and Sakellaridis 2006; Pitsikas et al. 2008).
Two in vivo experiments using saffron extract indicated that its administration was useful in treating neurodegenerative disorders and memory impairment, with significant improvements in learning and memory skills (Abe and Saito 2000; Sugiura et al. 1995). Baziar et al. (2019) compared the safety and effectiveness of saffron and MPH in improving ADHD symptoms in children. This was a 6-week, double-blind randomized trial, including 54 children aged 6–17 years, diagnosed with ADHD, according to DSM-IV. These children randomly received treatment with MPH or saffron capsules, depending on their weight (20 mg/d for < 30 kg and 30 mg/d for > 30 kg). Symptoms were assessed using the Attention-Deficit/Hyperactivity Disorder Rating Scale IV for Teachers and Parents (ADHD-RS-IV) at baseline, 3 weeks, and 6 weeks. The authors found no significant difference in ADHD-RS-IV scores between the two groups at baseline and the end of the study (p = 0.731 and p = 0.883, respectively). The frequencies of adverse effects were similar between the saffron and MPH groups. Thus, the authors concluded that short-term therapy with saffron was as effective as that with MPH. However, larger controlled studies with longer treatment periods are warranted (Baziar et al. 2019).
Blasco-Fontecilla et al. (2022) compared the efficacy of saffron and MPH in children and young adults diagnosed with ADHD. The study was characterized as prospective, naturalistic, non-randomized, and non-blinded, where 56 patients aged 7–17 years were divided into the following two groups: the saffron group receiving psychoeducation and saffron (30 mg/day) and the MPH group receiving extended-release MPH (1 mg/kg per day) for 3 months. To assess the symptoms of hyperactivity and inattention, the following scales were used: SNAP-IV and the revised Conners Parental Rating Scale, to assess executive functions; the Behavioral Rating Inventory of Executive Function—Second Edition, to assess impulsivity; Conners' Continuous Performance Test, version 3, to assess sustained attention; and Sleep Disturbances Scale for Children, to assess sleep quality. The key finding here was that the efficacy of saffron is comparable to that of MPH. Saffron is the most effective in treating the symptoms of hyperactivity, while MPH is the most effective in treating the symptoms of inattention; both treatments are well-tolerated and no significant side effects have been reported. Finally, saffron markedly improves the time taken to fall asleep, according to the parents' reports. Thus, the study verified the effectiveness and safety of saffron extract compared to those of MPH. This, along with other studies, confirmed that saffron is a potential candidate for the treatment of ADHD (Blasco-Fontecilla et al. 2022).
Crocus sativus L.—inflammatory processes
Abbaszade-Cheragheali et al. (2022) assessed the effects of crocin, a constituent of saffron, on anxiety and depression induced by unpredictable chronic mild stress (UCMS) in rats. The rats underwent UCMS and were treated with crocin (10, 20, and 30 mg/kg) for 4 weeks. Inflammatory parameters and oxidative stress damage were evaluated afterward. The authors demonstrated that UCMS altered the assessed parameters, and crocin at concentrations of 20 and 30 mg/kg reduced serum corticosterone levels, malondialdehyde (MDA), TNF-α, and IL-6, while increasing IL-10 and brain-derived neurotrophic factor (BDNF) levels in cortical tissues. Akbari-Fakhrabadi et al. (2019) evaluated the effect of saffron treatment on resistance capacity, mitochondrial biogenesis, inflammation, antioxidants, and metabolic biomarkers in Wistar rats subjected to resistance training. The rats underwent resistance training and received saffron at a concentration of 40 mg/kg. IL-6 levels were assessed, and decreases in IL-6 levels were observed, alongside improvements in other parameters such as malondialdehyde, CPK, and AST. These findings indicated that saffron increased mitochondrial biogenesis, reduced oxidative stress and inflammation, and modulated metabolic biomarkers. Xu et al. (2022) evaluated the effect of crocin on breast cancer cells. They assessed the levels of nuclear factor kappa B (NF-κB) p-p65 and p65, as well as TNF-α and IL-1β levels. The results demonstrated that crocin inhibited NF-κB activation, suppressed cell viability and proliferation in breast cancer cells (BC). Crocin significantly reduced TNF-α and IL-1β levels, suggesting its role in suppressing inflammation in BC cells.
Ginkgo biloba
Ginkgo biloba (Ginkgoaceae), a plant native to China, has been used in traditional Chinese medicine for centuries. It is classified as one of the oldest seed plants, owing to which, it is usually called the "living fossil". Moreover, this tree can live for over a thousand years, reaching up to forty meters in height. The leaf and seed extracts have been used for several years to treat circulatory disorders, asthma, vertigo, and cognitive problems (Kleijnen and Knipschild 1992).
These therapeutic effects are attributed to their active ingredients, including terpenoids, flavonol glycosides, and proanthocyanidins, among which flavonol glycosides are the most prevalent (Kleijnen and Knipschild 1992; Pang et al. 1996). Several clinical studies have evaluated the efficacy of G. biloba. In addition, studies in an animal model have revealed that this plant increases central dopaminergic activity (Yeh et al. 2011).
Shakibaei et al. (2015) evaluated the effectiveness of G. biloba as a complementary therapy for children and adolescents with ADHD. This clinical trial was randomized, double-blind, placebo-controlled, and registered (registration number: IRCT2014111519958N1). This study included 60 patients receiving MPH (20–30 mg/day) and G. biloba (80–120 mg/day) or placebo for 6 weeks. The following two rating scales were used: the ADHD Rating Scale-IV (ADHD-RS-IV), parent and teacher ratings (days 1, 2, and 6), and the Children's Global Assessment Scale (days 1 and 6). Importantly, compared to the placebo, G. biloba reduced the ADHD-RS-IV parent inattentiveness score, total score, and the teacher inattentiveness score. The response rate was higher with G. biloba than that with the placebo, based on parental assessment. Therefore, the authors identified G. biloba as an effective complementary treatment for ADHD; however, additional studies with a longer duration of treatment are necessary (Shakibaei et al. 2015).
Another randomized clinical study was conducted by Chutko et al. (2019), whose objective was to evaluate the effectiveness of a memoplant formulation (EGb 761, a standardized G. biloba leaf extract) in the treatment of adult patients diagnosed with ADHD. Here, 40 patients aged 18–45 years diagnosed with ADHD and 30 healthy adults were evaluated as controls. Memoplant was administered at a dose of 240 mg once daily for 8 weeks. Clinical, psychological, and electroencephalographic (EEG) tests were also performed. The results showed that adult patients with ADHD had subjective and objective impairments in memory and attention; the EEG suggested dysfunction of the frontothalamic regulatory system and a deficit of nonspecific activation by the reticular system. Twenty-four (60%) patients administered memoplant showed general clinical improvements, followed by reduced attention deficit and improved measures of memory (Chutko et al. 2019). In summary, G. biloba can be perceived as a potential candidate for ADHD treatment.
Ginkgo biloba—inflammatory processes
Zhang et al. (2022) aimed to evaluate the effect of Ginkgo Biloba extract (GBE) on cardiac and cerebral inflammation in rats subjected to a high-fat diet (HFD) combined with unpredictable chronic mild stress (UCMS). The animals received 40 mg/kg/day of GBE for 8 weeks. They assessed helper T lymphocytes (CD3 + , CD4 +) and interleukins (IL-) 1β, IL-37, IL-38. They also evaluated nuclear factor kappa B (NF-κB) p65 and p-p65. The results showed that rats exposed to HFD + UCMS and treated with GBE exhibited elevated levels of helper T lymphocytes and serum anti-inflammatory cytokines including IL-37 and IL-38. Additionally, GBE inhibited the canonical NF-κB signaling pathway through negative regulation of p-p65 expressions. Mohammed et al. (2020) demonstrated the neuroprotective effect of GBE in a rotenone-induced Parkinson's Disease model in animals. The animals were treated with GBE (150 mg/kg/day) for 20 days, followed by a combination with rotenone (2.5 mg/kg/day) for 50 days. Inflammatory profile was assessed through IL-1β, IL-6, and TNF-α. The results showed that GBE treatment reduced the levels of IL-1β, IL-6, and TNF-α. Finally, Zhang et al. (2018) revealed the neuroprotective and anti-inflammatory effects of GBE extract in in vitro and in vivo models of cerebral ischemia. They used doses of 7.5 and 15 mg/kg of GBE extract. The results indicated that GBE significantly attenuated cerebral infarction and neuronal apoptosis. It also reduced the levels of inflammatory cytokines IL-1α, IL-6, and CXCL10 (IP-10), inhibited astrocyte activation, and decreased the phosphorylation of STAT3 and JAK2.
Panax ginseng
Red Ginseng (Panax ginseng) is considered as the most popular herbal medicine used globally. It has several positive effects on glucose metabolism, psychomotor function, and lung disease. Korean Red Ginseng (KRG) contains ginsenosides, polyacetylenes, acidic polysaccharides, aromatic compounds, antioxidants, and acidic peptides.Among these, ginsenoside has potent effects, as an anti-inflammatory, anticarcinogenic, and anti-stress agent, along with potent effects in the central nervous system (Christensen 2008).
Clinical studies have evaluated the potential positive effects of KRG on fatigue, insomnia, and depression (Tode et al. 1999). Some studies have also investigated the effects of KRG on ADHD symptoms. Ko et al. (2014) conducted a double-blind, placebo-controlled, randomized clinical trial to evaluate the effects of KRG on children with ADHD symptoms. Seventy patients aged 6–15 years were divided in the KRG (n = 33) and control (n = 37) groups. The KRG group received a pouch of KRG (1 g KRG extract/bag) twice daily, whereas the control group received a pouch of placebo twice daily for 8 weeks. The DSM-IV criteria were used to evaluate the inattention and hyperactivity scales. Secondary outcomes were quantitative EEG theta/beta ratio (QEEG TBR), and salivary cortisol and dehydroepiandrosterone (DHEA) levels. No differences were observed in the baseline characteristics between the KRG and control groups. After 8 weeks, the KRG group showed significantly lower inattention/hyperactivity scores than those of the control group. Moreover, the KRG group showed a significantly lower QEEG TBR than that in the control group. However, there were no significant differences in salivary cortisol or DHEA levels at week 8 compared with the baseline levels. No serious adverse events were reported in any of the groups. The authors concluded that KRG treatment may be an effective and safe alternative for children with symptoms of inattention and hyperactivity/impulsivity. However, further studies are required to corroborate these findings (Ko et al. 2014).
Panax ginseng—inflammatory processes
Cheah et al. (2022) evaluated the in vitro anti-neuroinflammatory properties of Panax ginseng root extract based on NO and cytokine production. BV2 microglial cell culture stimulated with lipopolysaccharides was treated with the extract, and its anti-neuroinflammatory properties were assessed by measuring NO production, as well as TNF-α, IL-6, and IL-10 levels. In this study, the authors did not observe differences in NO, TNF-α, and IL-6. However, Panax ginseng extract significantly increased interleukin IL-10 compared to untreated cells. Kumar et al. (2014) demonstrated in their animal model of cerebral trauma that Panax ginseng (100 and 200 mg/kg) for 2 weeks significantly attenuated neuroinflammatory changes measured by TNF-α and IL-6. Yang et al. (2022) showed in their study the effect of ginseng extract on inflammation and oxidative stress in RAW264.7 cells and in an animal model with dextran sulfate-induced colitis (DSS). Their results showed that ginseng extract reduced levels of nitric oxide, TNF-α, and IL-6 secreted by LPS-treated cells. The treatment inhibited NF-κB activity and the phosphorylation of JNK, ERK-1/2, and p38.
Klamin ®
Recently, microalgae from Lake Klamath have been studied for their potential effects on attention, mood, and anxiety. The extracts of these algae can reduce mood changes, such as anxiety and depression, and improve learning (Genazzani et al. 2010; Sedriep et al. 2011). These microalgal extracts contain different compounds, such as phenylethylamine (PEA), mycosporin-type amino acids (MAAs), AFA-phycocyanins, and AFA-phytochrome, which could be involved in related responses. Recently, Klamath microalgae extract was patented (Klamin®: β-phenylethylamine-12 mg/g AFA-phycocyanins-10%), MAAs-2%), and AFA-phytochrome (1%) were produced by the Center Research in Nutrition, Urbino, Italy) (Benedetti et al. 2004).
One study has been conducted in humans in the last decade. Cremonte et al. (2017) used Klamin® to treat the main ADHD symptoms. This study included 25 patients, aged 6–15 years diagnosed with ADHD according to the DSM-IV criteria. Supplementation was administered to all the participants for 6 months (in liquid or tablet form), according to their weight (125–1200 mg/kg). All patients were evaluated at baseline and at the end of the 6-month period. The following scales were used: inattention and hyperactivity-impulsivity, Child Global Rating Scale; SNAP IV (Conners-R Parent Rating Scale); oppositional defiant disorders (ODD subscale, SNAP IV); attention functions (Bell Test); executive functions (Tower of London test); freedom from distraction parameter (LD, Wechsler Intelligence Scale for Children III [WISC III scale]); short-term verbal memory (of numbers, WISC III scale); and arithmetic reasoning and mental math skills (arithmetic reasoning, WISC III scale). As main results, the authors showed that the use of Klamin® provided significant improvements based on assessments of its general functioning, behaviors related to inattention and hyperactivity-impulsivity, attention functions in the selective and sustained component, and executive functions. Finally, they proved the initial hypothesis that Klamin® extract improves ADHD symptoms; however, additional studies with a larger sample size are necessary (Cremonte et al. 2017).
Klamin ®—inflammatory processes
Nuzzo et al. (2018) aimed to demonstrate the antioxidant and neuroprotective effects of AFA extract Klamin® in a LAN5 neuronal cell model. Following cellular cytotoxicity experiments, a dose of 800 ng/μl was employed to assess the inflammatory profile through interleukins (IL-1β and IL-6) and p-NFκB. The results indicated that the AFA extract reduced the levels of IL-1β and IL-6, and inhibited p-NFκB, suggesting a positive role in alleviating neuroinflammation.
Pinus pinaster
Pinus pinaster belongs to the Pinaceae family; it is mainly found in the western Mediterranean region and can live for up to 300 years. The pine tree has been cultivated in vast monocultures in southern France, and since the middle ages, its preparations have been used for wound healing and treating scurvy (Chandler et al. 1979). The outer bark, which is relatively redder, is used for Pycnogenol® extraction. Pycnogenol® is a patented (Horphag Research), commercially available extract of French maritime pine bark. Some known properties of Pycnogenol® include anti-inflammatory activity, radical scavenging activity, and reduction of menstrual cramps and pain.
Pycnogenol is mainly composed of phenolic compounds, glycosides, glucose esters, procyanidins, and flavonoids (Packer et al. 1999). In addition to its extract being marketed for clinical purposes, it can also be used as a supplement, ingredient in cosmetics, and food additive (Rohdewald 2004). However, owing to its antioxidant and immunomodulatory properties, clinical studies have been conducted with Pycnogenol® in children and adolescents with ADHD, and favorable results have been obtained.
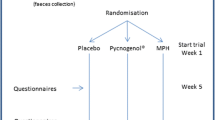
Trebatická et al. (2006) evaluated the effects of the Pycnogenol® extract in a randomized, placebo-controlled clinical study and showed that Pycnogenol® administration significantly reduces hyperactivity and improves attention, concentration, and visual-motor coordination (Trebatická et al. 2006). Based on these findings, Verlaet et al. (2017) presented a Phase III, randomized, double-blind, placebo-controlled, multicenter clinical trial (Clinicaltrials.gov number: NCT02700685; EudraCT 2016-000215-32) to evaluate the effect of Pycnogenol® treatment in ADHD. This study included 144 patients (aged 6–12 years), divided into the following three groups: MPH: patients with body weight < 30 kg administered at 20 mg/day, ≥ 30 kg at 30 mg/day. Treatment during the first week always contains 10 mg, increasing by 10 mg each week to limit side effects; Pycnogenol®: patients with body weight < 30 kg will receive 20 mg/day, those with body weight ≥ 30 kg, 40 mg/day, targeting a daily dose of 1 mg/kg. Treatment for the first 2 weeks was maintained at 20 mg; the placebo contained excipients only. Different analytical tools, such as (ADHD-RS ADHD-Rating Scale), Social-Emotional Questionnaire (SEQ), Physical Complaints Questionnaire, Food Frequency Questionnaire, erythrocyte glutathione analysis, and lipid-soluble antioxidant analysis. Antioxidant enzyme activity, plasma malondialdehyde, 8-OHdG 8-hydroxy-2-deoxyguanosine, cytokine, antibody, peripheral blood mononuclear cell count and reactivity, microbial composition, catecholamine, serum neuropeptide Y, zinc, and genetic analyses, were used for evaluation. All measurements were performed at baseline, and after 5 and 10 weeks of treatment (Verlaet et al. 2017). Weyns et al. (2022) reported that 88 patients completed the protocol. Teachers reported significant improvement in total and ADHD-RS hyperactivity/impulsivity scores using Pycnogenol® and MPH after 10 weeks, compared to those in the placebo. The SEQ scores corroborated the ADHD-RS results. Adverse effects were reported five times more frequently for MPH than those for Pycnogenol®. This is an ongoing study, however, the available results show promising perspectives regarding the use of Pycnogenol® for the treatment of ADHD (Weyns et al. 2022).
Pinus pinaster—inflammatory processes
Lee et al. (2023) investigated the neuroprotective effects of Pinus pinaster and its therapeutic mechanisms in an animal model of cerebral ischemia. Rats underwent common carotid artery occlusion and were then treated with Pycnogenol (25, 50, and 100 mg/kg, respectively) immediately, 24 h, and 48 h after occlusion. Immunohistochemistry for interleukin-1β (IL-1β) was performed to assess the inflammatory profile. Results showed that in addition to attenuating ischemic injury, only the dose of 100 mg/kg inhibited IL-1β expression, thereby reducing inflammation. Go et al. (2022) studied the effect of Pinus pinaster extract against cognitive decline and neuroinflammation caused by Alzheimer's Disease (AD) in an animal model induced by intracerebral Aβ 1–42 injection. The animals were treated with the extract orally at concentrations of 15 and 30 mg/kg. To assess the neuroinflammatory profile, levels of TNF-α, p-JNK, p-IκB-α, COX-2, and IL-1β expression were measured. The results showed a decrease in TNF-α, p-IκB-α, and IL-1β levels in animals treated with the extract at the concentration of 30 mg/kg. Jeong et al. (2022) investigated the antioxidant and anti-inflammatory effects of ethanolic extract of Pinus pinaster in vitro and in vivo under acute inflammation conditions. Here, we will report the in vitro experiments, where inflammatory mediators (NO, iNOS, COX-2, TNF-α, and IL-1β) were assessed in LPS-stimulated RAW264.7 cells treated with different concentrations of pinus extract (6.25, 12.5, 25, 50, and 100 μg/mL). The authors showed that pinus extract at concentrations of 25 and 100 μg/mL significantly reduced levels of NO, iNOS, COX-2, TNF-α, and IL-1β.
Ziziphus jujuba Mill. var. spinosa
Ziziphus jujuba Mill. var. spinosa is a thorny and branched deciduous plant of the Rhamnaceae family, which is widely distributed in northern and northeastern China. It has been used as an analgesic, tranquilizer, and anticonvulsant for over 2500 years in countries such as China and Korea. These effects are attributed to pharmacologically active compounds, such as flavones, alkaloids, and triterpenes (Cheng et al. 2000). Sansoninto (SST), a traditional herbal medicine used in Japan, China, and Taiwan, is extracted from its dried seeds and has positive effects on insomnia, depression, and neuropathy (Saito et al. 2000).
Because of the beneficial constituents of SST, some studies have assessed their effects on the main ADHD symptoms. Fujiwara et al. (2018) analyzed the potential of SST in the treatment of behavioral symptoms and neurochemical parameters in an animal model of ADHD. The study included 44 male mice (4-week-old), divided into the following four groups (n = 11 each): control (water), socially isolated (water), SST 800 mg/kg, or SST 2400 mg/kg. SST or water was orally administered once daily. Sociability, water seeking, and fear conditioning tests were performed at 9, 10, and 11 weeks of age. After completing the tests, the animals were decapitated for neurochemical studies, wherein EGR-1 protein expression in the hippocampus and prefrontal cortex was evaluated. The results showed that SST administration significantly improved deficits in sociability, attention-deficit-like behavior, and fear memory. Furthermore, reduced EGR-1 expression levels due to isolation stress were observed, which were restored by SST administration, suggesting that SST may be beneficial for the treatment of some ADHD symptoms (Fujiwara et al. 2018).
Ziziphus jujuba Mill. var. spinosa—inflammatory processes
Kandeda et al. (2021) investigated the anti-amnesic and molecular effects of aqueous extract of Ziziphus jujuba on D-galactose-induced working memory impairment in rats. The animals were treated with aqueous extract (41.5, 83, and 166 mg/kg, orally) daily for 14 days. At the end of the treatments, pro-inflammatory and neuronal damage markers were analyzed in the prefrontal cortex. The results showed that D-galactose caused working memory deficit along with alterations in tumor necrosis factor-alpha (TNF-α), interleukin-1 beta (IL-1β), interleukin-6 (IL-6), and interferon-gamma (IFN-γ). Treatment with the extract (166 mg/kg) reversed the working memory deficit and normalized levels of TNF-α, IL-6, and IFN-γ, thereby mitigating neuroinflammation. Tran et al. (2019) conducted a study to evaluate three new sesquilignan compounds from Z. jujuba for their bioactivity, including anti-inflammatory effects and cytotoxic activities. Here, we will report the anti-inflammatory findings. The authors used RAW264.7 cells and induced inflammation with LPS. First, they determined the IC50 of 18 compounds for NO inhibition and found NO inhibition in two compounds at concentrations ranging from 18.1 to 66.4 μM/mL. They then evaluated iNOS and COX-2 expressions and observed a decrease in the expression of iNOS and COX-2.
Conclusion
In summary, the all the studies included in this review focused on plants with demonstrated potential against inflammatory processes, positioning them as promising candidates for ADHD treatment, especially in patients who may not respond well to conventional medications.
The utilization of plants for medicinal purposes has a long history in human culture. In the context of ADHD treatment, natural products may play a role in attenuating or preventing the neuroinflammatory mechanisms. They have shown the capacity to positively modulate various inflammatory mediators, including cytokines, chemokines, and cytotoxic molecules, such as cyclooxygenase-2 (COX-2), reactive oxygen species (ROS), glutamate, and prostaglandins. Additionally, plant based medicines can impact specific signaling pathways like Toll-like receptor 4 (TLR4) and Mitogen-Activated Protein Kinases (MAPK), among others outlined in this review.
It's important to note, however, that while natural medicines are generally considered safe, they have not yet reached the status of a standard therapeutic resource for ADHD. This may be attributed to several factors, including the limited number of human clinical studies available, often with small sample sizes. Additionally, some of these studies lack proper control groups and exhibit inconsistent results. Furthermore, there is a dearth of initial studies elucidating the mechanisms of action of plant-derived compounds on the CNS, and there is no established standard animal or in vitro experimental model for studying ADHD.
Further studies are needed with the plants presented here. Future investigations should employ more rigorous and controlled methodologies to comprehensively evaluate the effectiveness of these alternative treatments and elucidate their mechanisms of action. This will facilitate equitable comparisons with existing studies and conventional ADHD medications, ultimately enhancing our knowledge of their therapeutic potential.
Data availability
Data sharing not applicable.
References
Abbaszade-Cheragheali A, Beheshti F, Kakhki S, Khatibi SR, Dehnokhalaji F, Akbari E, Fathi H, Farimani SS (2022) Crocin, the main active saffron (Crocus sativus L.) constituent, as a potential candidate to prevent anxiety and depressive-like behaviors induced by unpredictable chronic mild stress. Neurosci Lett 791(November):136912. https://doi.org/10.1016/j.neulet.2022.136912
Abe K, Saito H (2000) Effects of saffron extract and its constituent crocin on learning behaviour and long-term potentiation. Phytother Res 14(3):149–152. https://doi.org/10.1002/(SICI)1099-1573(200005)14:3%3c149::AID-PTR665%3e3.0.CO;2-5
Abhishek M, Rubal S, Rohit K, Rupa J, Phulen S, Gurjeet K, Raj SA, Manisha P, Alka B, Ramprasad P, Bikash M (2022) Neuroprotective effect of the standardised extract of Bacopa monnieri (BacoMind) in valproic acid model of autism spectrum disorder in rats. J Ethnopharmacol 293:115199. https://doi.org/10.1016/j.jep.2022.115199
Akbari-Fakhrabadi M, Najafi M, Mortazavian S, Rasouli M, Memari AH, Shidfar F (2019) Effect of saffron (Crocus sativus L.) and endurance training on mitochondrial biogenesis, endurance capacity, inflammation, antioxidant, and metabolic biomarkers in Wistar rats. J Food Biochem 43(8):e12946. https://doi.org/10.1111/jfbc.12946
Alonso GL, Zalacain A, Carmona M (2012) Saffron. In: Handbook of herbs and spices, pp 469–98. Elsevier. https://doi.org/10.1533/9780857095671.469
Andersen CH, Thomsen PH, Nohr EA, Lemcke S (2018) Maternal body mass index before pregnancy as a risk factor for ADHD and autism in children. Eur Child Adolesc Psychiatry 27(2):139–148. https://doi.org/10.1007/s00787-017-1027-6
APA (2013) Cautionary statement for forensic use of DSM-5. In: Diagnostic and statistical manual of mental disorders, 5th ed. American Psychiatric Publishing, Inc. https://doi.org/10.1176/appi.books.9780890425596.744053
Baziar S, Aqamolaei A, Khadem E, Mortazavi SH, Naderi S, Sahebolzamani E, Mortezaei A et al (2019) Crocus sativus L. versus methylphenidate in treatment of children with attention-deficit/hyperactivity disorder: a randomized, double-blind pilot study. J Child Adolesc Psychopharmacol 29(3):205–212. https://doi.org/10.1089/cap.2018.0146
Benedetti S, Benvenuti F, Pagliarani S, Francogli S, Scoglio S, Canestrari F (2004) Antioxidant properties of a novel phycocyanin extract from the blue-green alga aphanizomenon flos-aquae. Life Sci 75(19):2353–2362. https://doi.org/10.1016/j.lfs.2004.06.004
Blasco-Fontecilla H, Moyano-Ramírez E, Méndez-González O, Rodrigo-Yanguas M, Martin-Moratinos M, Bella-Fernández M (2022) Effectivity of saffron extract (Saffr’Activ) on treatment for children and adolescents with attention deficit/hyperactivity disorder (ADHD): a clinical effectivity study. Nutrients. https://doi.org/10.3390/nu14194046
Chandler RF, Freeman L, Hooper SN (1979) Herbal remedies of the maritime Indians. J Ethnopharmacol 1(1):49–68. https://doi.org/10.1016/0378-8741(79)90016-3
Chang JP-C, Su K-P, Mondelli V, Pariante CM (2021) Cortisol and inflammatory biomarker levels in youths with attention deficit hyperactivity disorder (ADHD): evidence from a systematic review with meta-analysis. Transl Psychiatry 11(1):430. https://doi.org/10.1038/s41398-021-01550-0
Chatterji N, Rastogi RP, Dhar ML (1965) Chemical examination of Bacopa monniera Wettst.—part II: the constitution of Bacoside A. Indian J Chem 3:24–29
Cheah CH, Kiong-Ling AP, Wong YP, Koh RY, Hussein S (2022) Anti-neuroinflammatory of chloroform extract of Panax ginseng root culture on lipopolysaccharide-stimulated BV2 microglia cells. Rep Biochem Mol Biol 11(1):125–137. https://doi.org/10.52547/rbmb.11.1.125
Chen Q, Sjolander A, Langstrom N, Rodriguez A, Serlachius E, D’Onofrio BM, Lichtenstein P, Larsson H (2014) Maternal pre-pregnancy body mass index and offspring attention deficit hyperactivity disorder: a population-based cohort study using a sibling-comparison design. Int J Epidemiol 43(1):83–90. https://doi.org/10.1093/ije/dyt152
Chen C, Li X, Gao P, Tu Y, Zhao M, Li J, Zhang S, Liang H (2015) Baicalin attenuates alzheimer-like pathological changes and memory deficits induced by amyloid Β1–42 protein. Metab Brain Dis 30(2):537–544. https://doi.org/10.1007/s11011-014-9601-9
Chen X, Yao T, Cai J, Fu X, Li H, Wu J (2022) Systemic inflammatory regulators and 7 major psychiatric disorders: a two-sample mendelian randomization study. Prog Neuro-Psychopharmacol Biol Psychiatry 116(June):110534. https://doi.org/10.1016/j.pnpbp.2022.110534
Cheng G, Bai Y, Zhao Y, Tao J, Liu Y, Tu G, Ma L, Liao N, Xu X (2000) Flavonoids from Ziziphus jujuba Mill Var. spinosa. Tetrahedron 56(45):8915–8920. https://doi.org/10.1016/S0040-4020(00)00842-5
Christensen LP (2008) Chapter 1 ginsenosides. In: Advances in food and nutrition research, pp 1–99. https://doi.org/10.1016/S1043-4526(08)00401-4
Chutko LS, Surushkina SYu, Yakovenko EA, Kropotov YuD, Sergeev AV (2019) Diagnosis and treatment of cognitive impairments in attention deficit syndrome in adults. Neurosci Behav Physiol 49(1):115–120. https://doi.org/10.1007/s11055-018-0703-4
Cremonte M, Sisti D, Maraucci I, Giribone S, Colombo E, Rocchi MBL, Scoglio S (2017) The effect of experimental supplementation with the klamath algae extract klamin on attention-deficit/hyperactivity disorder. J Med Food 20(12):1233–1239. https://doi.org/10.1089/jmf.2016.0181
Dave UP, Dingankar SR, Saxena VS, Joseph JA, Bethapudi B, Agarwal A, Kudiganti V (2014) An open-label study to elucidate the effects of standardized Bacopa monnieri extract in the management of symptoms of attention-deficit hyperactivity disorder in children. Adv Mind-Body Med 28(2):10–15
Dhawan BN, Singh HK (1996) Pharmacological studies on Bacopa monniera, an ayuredic nootropic agent. Europ Neuropsychopharmacol 653:144
Ding H, Wang H, Zhao Y, Sun D, Zhai X (2015) Protective effects of Baicalin on Aβ1–42-induced learning and memory deficit, oxidative stress, and apoptosis in rat. Cell Mol Neurobiol 35(5):623–632. https://doi.org/10.1007/s10571-015-0156-z
Dunn GA, Nigg JT, Sullivan EL (2019) Neuroinflammation as a risk factor for attention deficit hyperactivity disorder. Pharmacol Biochem Behav 182(July):22–34. https://doi.org/10.1016/j.pbb.2019.05.005
Faraone SV, Spencer T, Aleardi M, Pagano C, Biederman J (2004) Meta-analysis of the efficacy of methylphenidate for treating adult attention-deficit/hyperactivity disorder. J Clin Psychopharmacol. https://doi.org/10.1097/01.jcp.0000108984.11879.95
Faraone SV, Asherson P, Banaschewski T, Biederman J, Buitelaar JK, Ramos-Quiroga JA, Rohde LA, Sonuga-Barke EJS, Tannock R, Franke B (2015) Attention-deficit/hyperactivity disorder. Nat Rev Dis Primers 1(1):15020. https://doi.org/10.1038/nrdp.2015.20
Fredriksen M, Dahl AA, Martinsen EW, Klungsøyr O, Haavik J, Peleikis DE (2014) Effectiveness of one-year pharmacological treatment of adult attention-deficit/hyperactivity disorder (ADHD): an open-label prospective study of time in treatment, dose, side-effects and comorbidity. Eur Neuropsychopharmacol 24(12):1873–1884. https://doi.org/10.1016/J.EURONEURO.2014.09.013
Fujiwara H, Tsushima R, Okada R, Awale S, Araki R, Yabe T, Matsumoto K (2018) Sansoninto, a traditional herbal medicine, ameliorates behavioral abnormalities and down-regulation of early growth response-1 expression in mice exposed to social isolation stress. J Tradit Complement Med 8(1):81–88. https://doi.org/10.1016/j.jtcme.2017.03.004
Genazzani AD, Chierchia E, Lanzoni C, Santagni S, Veltri F, Ricchieri F, Rattighieri E, Nappi RE (2010) Effects of Klamath algae extract on psychological disorders and depression in menopausal women: a pilot study. Minerva Ginecol 62(5):381–388
Ghuman JK, Ghuman HS (2013) Pharmacologic intervention for attention-deficit hyperactivity disorder in preschoolers: is it justified? Pediatr Drugs. https://doi.org/10.1007/s40272-012-0001-5
Go MJ, Kim JM, Kang JY, Park SK, Lee CJ, Kim MJ, Lee HR et al (2022) Korean red pine (Pinus densiflora) bark extract attenuates Aβ-induced cognitive impairment by regulating cholinergic dysfunction and neuroinflammation. J Microbiol Biotechnol 32(9):1154–1167. https://doi.org/10.4014/jmb.2207.07015
Gohil KJ, Patel JA (2010) A review on Bacopa monniera: current research and future prospects. Int J Green Pharm 4(1):1. https://doi.org/10.4103/0973-8258.62156
Hennissen L, Bakker MJ, Banaschewski T, Carucci S, Coghill D, Danckaerts M, Dittmann RW et al (2017) Cardiovascular effects of stimulant and non-stimulant medication for children and adolescents with ADHD: a systematic review and meta-analysis of trials of methylphenidate, amphetamines and atomoxetine. CNS Drugs 31(3):199–215. https://doi.org/10.1007/s40263-017-0410-7
Jeong S-Y, Choi WS, Kwon OS, Lee JS, Son SY, Lee CH, Lee S, Song JY, Lee YJ, Lee J-Y (2022) Extract of Pinus densiflora needles suppresses acute inflammation by regulating inflammatory mediators in RAW264.7 macrophages and mice. Pharm Biol 60(1):1148–1159. https://doi.org/10.1080/13880209.2022.2079679
Jin X, Liu M-Y, Zhang D-F, Zhong X, Du K, Qian P, Yao W-F, Gao H, Wei M-J (2019) Baicalin mitigates cognitive impairment and protects neurons from microglia-mediated neuroinflammation via suppressing <scp>NLRP</Scp> 3 inflammasomes and <scp>TLR</Scp> 4/ <scp>NF</Scp> -κB signaling pathway. CNS Neurosci Ther 25(5):575–590. https://doi.org/10.1111/cns.13086
Kandeda AK, Nguedia D, Ayissi ER, Kouamouo J, Dimo T (2021) Ziziphus jujuba (Rhamnaceae) alleviates working memory impairment and restores neurochemical alterations in the prefrontal cortex of D-galactose-treated rats. Edited by Alin Ciobica. Evid-Based Complement Altern Med. https://doi.org/10.1155/2021/6610864
Kean J, Kaufman J, Lomas J, Goh A, White D, Simpson D, Scholey A et al (2015) A randomized controlled trial investigating the effects of a special extract of Bacopa monnieri (CDRI 08) on hyperactivity and inattention in male children and adolescents: BACHI study protocol (ANZCTRN12612000827831). Nutrients 7(12):9931–9945. https://doi.org/10.3390/nu7125507
Kean JD, Downey LA, Sarris J, Kaufman J, Zangara A, Stough C (2022) Effects of Bacopa monnieri (CDRI 08®) in a population of males exhibiting inattention and hyperactivity aged 6 to 14 years: a randomized, double-blind, placebo-controlled trial. Phytother Res 36(2):996–1012. https://doi.org/10.1002/ptr.7372
Kleijnen J, Knipschild P (1992) Ginkgo biloba for cerebral insufficiency. Br J Clin Pharmacol. https://doi.org/10.1111/j.1365-2125.1992.tb05642.x
Ko H-J, Kim I, Kim J-B, Moon Y, Whang M-C, Lee K-M, Jung S-P (2014) Effects of Korean red ginseng extract on behavior in children with symptoms of inattention and hyperactivity/impulsivity: a double-blind randomized placebo-controlled trial. J Child Adolesc Psychopharmacol 24(9):501–508. https://doi.org/10.1089/cap.2014.0013
Koesters M, Becker T, Kilian R, Fegert JM, Weinmann S (2009) Limits of meta-analysis: methylphenidate in the treatment of adult attention-deficit hyperactivity disorder. J Psychopharmacol 23(7):733–744. https://doi.org/10.1177/0269881108092338
Krinzinger H, Hall CL, Groom MJ, Ansari MT, Banaschewski T, Buitelaar JK, Carucci S et al (2019) Neurological and psychiatric adverse effects of long-term methylphenidate treatment in ADHD: a map of the current evidence. Neurosci Biobehav Rev 107(December):945–968. https://doi.org/10.1016/j.neubiorev.2019.09.023
Kumar A, Rinwa P, Dhar H (2014) Microglial inhibitory effect of ginseng ameliorates cognitive deficits and neuroinflammation following traumatic head injury in Rats. Inflammopharmacology 22(3):155–167. https://doi.org/10.1007/s10787-013-0187-3
Lee T-K, Park JH, Shin MC, Cho JH, Ahn JH, Kim DW, Lee J-C et al (2023) Therapeutic treatment with pycnogenol® attenuates ischemic brain injury in gerbils focusing on cognitive impairment, neuronal death, BBB leakage and neuroinflammation in the hippocampus. J Integr Neurosci 22(2):26. https://doi.org/10.31083/j.jin2202026
Leffa DT, Torres ILS, Rohde LA (2018) A review on the role of inflammation in attention-deficit/hyperactivity disorder. NeuroImmunoModulation 25(5–6):328–333. https://doi.org/10.1159/000489635
Li B, Wang M, Chen S, Li M, Zeng J, Wu S, Tu Y et al (2022) “Baicalin mitigates the neuroinflammation through the TLR4/MyD88/NF-ΚB and MAPK pathways in LPS-stimulated BV-2 microglia.” Edited by Anna Chiarini. BioMed Res Int. https://doi.org/10.1155/2022/3263446
Mash EJ, Barkley RA (2003) Child psychopathology, 2nd ed.
Mohammed NA, Abdou HM, Tass MA, Alfwuaires M, Abdel-Moneim AM, Essawy AE (2020) Oral supplements of Ginkgo biloba extract alleviate neuroinflammation, oxidative impairments and neurotoxicity in rotenone-induced Parkinsonian rats. Curr Pharm Biotechnol 21(12):1259–1268. https://doi.org/10.2174/1389201021666200320135849
Nemetchek MD, Stierle AA, Stierle DB, Lurie DI (2017) The ayurvedic plant Bacopa monnieri inhibits inflammatory pathways in the brain. J Ethnopharmacol 197(February):92–100. https://doi.org/10.1016/j.jep.2016.07.073
Nuzzo D, Presti G, Picone P, Galizzi G, Gulotta E, Giuliano S, Mannino C, Gambino V, Scoglio S, Di Carlo M (2018) Effects of the aphanizomenon flos-aquae extract (Klamin®) on a neurodegeneration cellular model. Oxid Med Cell Longev 2018(September):1–14. https://doi.org/10.1155/2018/9089016
Packer L, Rimbach G, Virgili F (1999) Antioxidant activity and biologic properties of a procyanidin-rich extract from pine (Pinus maritima) Bark, pycnogenol. Free Radic Biol Med 27(5–6):704–724. https://doi.org/10.1016/S0891-5849(99)00090-8
Pan M-H, Chiou Y-S, Tsai M-L, Ho C-T (2011) Anti-Inflammatory activity of traditional chinese medicinal herbs. J Tradit Complement Med 1(1):8–24. https://doi.org/10.1016/S2225-4110(16)30052-9
Pang Z, Pan F, He S (1996) Ginkgo biloba L.: history, current status, and future prospects. J Altern Complement Med 2(3):359–363. https://doi.org/10.1089/acm.1996.2.359
Pitsikas N, Boultadakis A, Georgiadou G, Tarantilis PA, Sakellaridis N (2008) Effects of the active constituents of Crocus sativus L., Crocins, in an animal model of anxiety. Phytomedicine 15(12):1135–1139. https://doi.org/10.1016/j.phymed.2008.06.005
PitsikasN SN (2006) Crocus sativus L. extracts antagonize memory impairments in different behavioural tasks in the rat. Behav Brain Res 173(1):112–115. https://doi.org/10.1016/j.bbr.2006.06.005
Polanczyk G, De Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164(6):942–948. https://doi.org/10.1176/ajp.2007.164.6.942
Rijlaarsdam J, Cecil CAM, Walton E, Mesirow MSC, Relton CL, Gaunt TR, McArdle W, Barker ED (2017) Prenatal unhealthy diet, insulin-like growth factor 2 gene ( IGF2) methylation, and attention deficit hyperactivity disorder symptoms in youth with early-onset conduct problems. J Child Psychol Psychiatry 58(1):19–27. https://doi.org/10.1111/jcpp.12589
Rohdewald P (2004) Pycnogenol® French maritime pine bark extract. Encycl Diet Suppl. https://doi.org/10.1081/E-EDS-120022123
Saini N, Singh D, Sandhir R (2019) Bacopa monnieri prevents colchicine-induced dementia by anti-inflammatory action. Metab Brain Dis 34(2):505–518. https://doi.org/10.1007/s11011-018-0332-1
Saito K, Umeda S, Kawashima K, Kano Y (2000) Pharmacological properties of traditional medicines. XXVI. Effects of sansohnin-to on pentobarbital sleep in stressed mice. Biol Pharm Bull 23(1):76–79. https://doi.org/10.1248/bpb.23.76
Sanchez CE, Barry C, Sabhlok A, Russell K, Majors A, Kollins SH, Fuemmeler BF (2018) Maternal pre-pregnancy obesity and child neurodevelopmental outcomes: a meta-analysis. Obes Rev 19(4):464–484. https://doi.org/10.1111/obr.12643
Sarris J, Kean J, Schweitzer I, Lake J (2011) Complementary medicines (herbal and nutritional products) in the treatment of attention deficit hyperactivity disorder (ADHD): a systematic review of the evidence. Complement Ther Med 19(4):216–227. https://doi.org/10.1016/j.ctim.2011.06.007
Sedriep S, Xia X, Marotta F, Zhou L, Yadav H, Yang H, Soresi V et al (2011) Beneficial nutraceutical modulation of cerebral erythropoietin expression and oxidative stress: an experimental study. J Biol Regul Homeost Agents 25(2):187–194
Shakibaei F, Radmanesh M, Salari E, Mahaki B (2015) Ginkgo biloba in the treatment of attention-deficit/hyperactivity disorder in children and adolescents. a randomized, placebo-controlled, trial. Complement Ther Clin Pract 21(2):61–67. https://doi.org/10.1016/j.ctcp.2015.04.001
Shang X, He X, He X, Li M, Zhang R, Fan P, Zhang Q, Jia Z (2010) The genus Scutellaria an ethnopharmacological and phytochemical review. J Ethnopharmacol 128(2):279–313. https://doi.org/10.1016/j.jep.2010.01.006
Shankar K, Zhong Y, Kang P, Lau F, Blackburn ML, Chen J-R, Borengasser SJ, Ronis MJJ, Badger TM (2011) Maternal obesity promotes a proinflammatory signature in rat uterus and blastocyst. Endocrinology 152(11):4158–4170. https://doi.org/10.1210/en.2010-1078
Sharifi-Rad M, Lankatillake C, Dias DA, Docea AO, Mahomoodally MF, Lobine D, Chazot PL et al (2020) Impact of natural compounds on neurodegenerative disorders: from preclinical to pharmacotherapeutics. J Clin Med 9(4):1061. https://doi.org/10.3390/jcm9041061
Sheikh N, Ahmad A, Siripurapu KB, Kuchibhotla VK, Singh S, Palit G (2007) Effect of Bacopa monniera on stress induced changes in plasma corticosterone and brain monoamines in rats. J Ethnopharmacol 111(3):671–676. https://doi.org/10.1016/J.JEP.2007.01.025
Shinomol GK, Mythri RB, Srinivas Bharath MM, Muralidhara (2012) Bacopa monnieri extract offsets rotenone-induced cytotoxicity in dopaminergic cells and oxidative impairments in mice brain. Cell Mol Neurobiol 32(3):455–465. https://doi.org/10.1007/s10571-011-9776-0
Silva D, Colvin L, Hagemann E, Bower C (2014) Environmental risk factors by gender associated with attention-deficit/hyperactivity disorder. Pediatrics 133(1):e14-22. https://doi.org/10.1542/peds.2013-1434
Silva AR, Grosso C, Delerue-Matos C, Rocha JM (2019) Comprehensive review on the interaction between natural compounds and brain receptors: benefits and toxicity. Eur J Med Chem 174(July):87–115. https://doi.org/10.1016/j.ejmech.2019.04.028
Spencer T, Biederman J, Wilens T, Harding M, O’Donnell D, Griffin S (1996) Pharmacotherapy of attention-deficit hyperactivity disorder across the life cycle. J Am Acad Child Adolesc Psychiatry 35(4):409–432. https://doi.org/10.1097/00004583-199604000-00008
Sugiura M, Saito H, Abe K, Shoyama Y (1995) Ethanol Extract of Crocus sativus L. antagonizes the inhibitory action of ethanol on hippocampal long-term potentiationin vivo. Phytother Res 9(2):100–104. https://doi.org/10.1002/ptr.2650090204
Sun J, Li L, Wu J, Liu B, Gong W, Lv Y, Luo Q, Duan X, Dong J (2013) Effects of Baicalin on airway remodeling in asthmatic mice. Planta Med 79(03/04):199–206. https://doi.org/10.1055/s-0032-1328197
Surman CBH, Hammerness PG, Pion K, Faraone SV (2013) Do stimulants improve functioning in adults with ADHD? A review of the literature. Eur Neuropsychopharmacol. https://doi.org/10.1016/j.euroneuro.2012.02.010
Terasaki LS, Schwarz JM (2016) Effects of moderate prenatal alcohol exposure during early gestation in rats on inflammation across the maternal-fetal-immune interface and later-life immune function in the offspring. J Neuroimmune Pharmacol 11(4):680–692. https://doi.org/10.1007/s11481-016-9691-8
Thapar A, Cooper M, Eyre O, Langley K (2013) Practitioner review: what have we learnt about the causes of ADHD? J Child Psychol Psychiatry 54(1):3–16. https://doi.org/10.1111/j.1469-7610.2012.02611.x
Tode T, Kikuchi Y, Hirata J, Kita T, Nakata H, Nagata I (1999) Effect of Korean red ginseng on psychological functions in patients with severe climacteric syndromes. Int J Gynecol Obstet 67(3):169–174. https://doi.org/10.1016/S0020-7292(99)00168-X
Tran HNK, Cao TQ, Kim JA, Woo MH, Min BS (2019) Anti-inflammatory and cytotoxic activities of constituents isolated from the fruits of Ziziphus jujuba Var. Inermis rehder. Fitoterapia 137(September):104261. https://doi.org/10.1016/j.fitote.2019.104261
Trebatická J, Kopasová S, Hradečná Z, Činovský K, Škodáček I, Šuba J, Muchová J et al (2006) Treatment of ADHD with french maritime pine bark extract, Pycnogenol®. Eur Child Adolesc Psychiatry 15(6):329–335. https://doi.org/10.1007/s00787-006-0538-3
Verlaet AAJ, Ceulemans B, Verhelst H, Van West D, De Bruyne T, Pieters L, Savelkoul HFJ, Hermans N (2017) Effect of Pycnogenol® on attention-deficit hyperactivity disorder (ADHD): study protocol for a randomised controlled trial. Trials 18(1):145. https://doi.org/10.1186/s13063-017-1879-6
Verlaet A, Maasakkers C, Hermans N, Savelkoul H (2018) Rationale for dietary antioxidant treatment of ADHD. Nutrients 10(4):405. https://doi.org/10.3390/nu10040405
Wang P-W, Lin T-Y, Yang P-M, Fang J-Y, Li W-T, Pan T-L (2022) Therapeutic efficacy of Scutellaria baicalensis georgi against psoriasis-like lesions via regulating the responses of keratinocyte and macrophage. Biomed Pharmacother 155(November1):113798. https://doi.org/10.1016/j.biopha.2022.113798
Werenberg Dreier J, Andersen A-MN, Hvolby A, Garne E, Andersen PK, Berg-Beckhoff G (2016) Fever and infections in pregnancy and risk of attention deficit/hyperactivity disorder in the offspring. J Child Psychol Psychiatry 57(4):540–548. https://doi.org/10.1111/jcpp.12480
Weyns AS, Verlaet AAJ, Breynaert A, Naessens T, Fransen E, Verhelst H, Van West D et al (2022) Clinical investigation of french maritime pine bark extract on attention-deficit hyperactivity disorder as compared to methylphenidate and placebo: part 1: efficacy in a randomised trial. J Funct Foods 97(October):105246. https://doi.org/10.1016/J.JFF.2022.105246
White RD, Harris GD, Gibson ME (2014) Attention deficit hyperactivity disorder and athletes. Sports Health. https://doi.org/10.1177/1941738113484679
Xiong J, Wang C, Chen H, Hu Y, Tian L, Pan J, Geng M (2014) Aβ-induced microglial cell activation is inhibited by baicalin through the JAK2/STAT3 signaling pathway. Int J Neurosci 124(8):609–620. https://doi.org/10.3109/00207454.2013.865027
Xu Q, Yu J, Jia G, Li Z, Xiong H (2022) Crocin attenuates NF-ΚB-mediated inflammation and proliferation in breast cancer cells by down-regulating PRKCQ. Cytokine 154(June):155888. https://doi.org/10.1016/j.cyto.2022.155888
Yang S, Li F, Lu S, Ren L, Bian S, Liu M, Zhao D, Wang S, Wang J (2022) Ginseng root extract attenuates inflammation by inhibiting the MAPK/NF-ΚB signaling pathway and activating autophagy and P62-Nrf2-Keap1 signaling in vitro and in vivo. J Ethnopharmacol 283(January):114739. https://doi.org/10.1016/j.jep.2021.114739
Yeh K-Y, Wu C-H, Tai M-Y, Tsai Y-F (2011) Ginkgo biloba extract enhances noncontact erection in rats: the role of dopamine in the paraventricular nucleus and the mesolimbic system. Neuroscience 189(August):199–206. https://doi.org/10.1016/j.neuroscience.2011.05.025
Yin F, Liu J, Ji X, Wang Y, Zidichouski J, Zhang J (2011) Baicalin prevents the production of hydrogen peroxide and oxidative stress induced by Aβ aggregation in SH-SY5Y cells. Neurosci Lett 492(2):76–79. https://doi.org/10.1016/j.neulet.2011.01.055
Zhang Y, Liu J, Yang B, Zheng Y, Yao M, Sun M, Xu L, Lin C, Chang D, Tian F (2018) Ginkgo biloba extract inhibits astrocytic lipocalin-2 expression and alleviates neuroinflammatory injury via the JAK2/STAT3 pathway after ischemic brain stroke. Front Pharmacol. https://doi.org/10.3389/fphar.2018.00518
Zhang L, Li G, Tao S, Xia P, Chaudhry N, Kaura S, Stone SS, Liu M (2022) Ginkgo biloba extract reduces cardiac and brain inflammation in rats fed a HFD and exposed to chronic mental stress through NF-ΚB inhibition. Edited by Feng Zhang. Mediat Inflamm. https://doi.org/10.1155/2022/2408598
Zhou R-Y, Han X-M, Wang J-J, Yuan H-X, Sun J-C, You Y, Song Y-C (2017) Effect of baicalin on behavioral characteristics of rats with attention deficit hyperactivity disorder. Zhongguo Dang Dai Er Ke Za Zhi Chin J Contemp Pediatr 19(8):930–937. https://doi.org/10.7499/j.issn.1008-8830.2017.08.016
Zhou R, Wang J, Han X, Ma B, Yuan H, Song Y (2019) Baicalin regulates the dopamine system to control the core symptoms of ADHD. Mol Brain. https://doi.org/10.1186/s13041-019-0428-5
Funding
This study was funded in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001 and Conselho Nacional de Pesquisa (CNPq) Grant number 420381/2018-0.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest was reported by the author(s).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martins, A., Conte, M., Goettert, M.I. et al. Attention-deficit/hyperactivity disorder and inflammation: natural product-derived treatments—a review of the last ten years. Inflammopharmacol 31, 2939–2954 (2023). https://doi.org/10.1007/s10787-023-01339-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-023-01339-1