Summary
The potential of natural substances with immunotherapeutic properties has long been studied. β-glucans, a cell wall component of certain bacteria and fungi, potentiate the immune system against microbes and toxic substances. Moreover, β-glucans are known to exhibit direct anticancer effects and can suppress cancer proliferation through immunomodulatory pathways. Mortality of lung cancer has been alarmingly increasingly worldwide; therefore, treatment of lung cancer is an urgent necessity. Numerous researchers are now dedicated to using β-glucans as a therapy for lung cancer. In the present attempt, we have reviewed the studies addressing therapeutic effects of β-glucans in primary and metastatic lung cancer published in the time period of 1991–2016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer ranks as the leading cause of cancer-related mortality worldwide [1]. There are estimated 1.82 million new cases of lung cancer globally which constitutes nearly 13% of all newly diagnosed cancer cases annually [2]. Lung cancer is a heterogeneous disease categorized into two main types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) [3]. The most common type, NSCLC, accounts approximately for 80 to 85% of all lung cancer cases and comprises squamous cell carcinoma (SCC), adenocarcinoma (ADC), and large cell carcinoma (LCC) [3]. SCLC is characterized by a high propensity for invasion and metastasis and its five-year survival is only 6.9% [4]. Surgical resection combined with or without adjuvant chemotherapy is the standard line of treatment in early stage NSCLC [5]. Radiotherapy combined with chemotherapy is recommended for advanced stage NSCLC patients, including some of the stage IIIA and all stage IIIB NSCLC patients [6]. Despite the availability of these treatment modalities, the tremendous mortality and morbidity caused by lung cancer can be due to two reasons: first, a high proportion of lung cancer patients are only diagnosed at an advanced stages; and second, a large population of patients manifests drug resistant, and local or distant metastasis [7–9]. The cancer stem cell theory assumes that the bulk of tumors is composed of a hierarchy of heterogeneous subpopulations [10, 11]. Hypermalignant subpopulations of cancer cells termed cancer stem cells (CSCs), also referred to tumor-initiating cells (TICs) or stem-like cancer cells have been isolated from patients with different tumor types [12–18]. These cells are found to be highly malignant, tumorigenic, and possess high stemness properties, as well as, resistant to conventional chemotherapy and radiation therapy regimens. Moreover, chemotherapy and radiation induce stemness genes in cancer cells that lead to CSCs enrichment in tumor tissues [19, 20].
Use of dietary supplements in parallel with chemotherapeutic regimens has received much attention for their benefits in lung cancer treatment [21, 22]. One of the most interesting dietary components is β-glucans (beta-glucans) which are naturally found in the cell walls of fungi, yeast, bacteria, and cereals [23]. Since the development of novel therapeutic approaches to overcome the current obstacles in the treatment of lung cancer including chemotherapy and radiotherapy resistance, metastasis and relapse is an urgent necessity, we reviewed the research studies concerning the role of β-glucans in lung cancer treatment.
The source and structure of β-glucans
β-glucans are glucose polymers within the cell wall of a wide range of fungi, including Candida albicans and Saccharomyces cerevisiae as well as barley and some seaweed plants [24, 25]. β-glucans have been purified from different sources including brewer’s and backer’s yeast as well as from oats and barley bran [26]. For example, Saccharomyces cerevisiae cell wall consists of three layers: an inner layer of insoluble β-glucan (30–35%), a middle layer of soluble β-glucan (20–22%), and an external layer of glycoprotein (30%) [24]. Moreover, β-glucans have been isolated from some mushrooms as shiitake (Lentinusedodes), maitake (Grifolafrondosa), schizophyllan (Schizophyllum commune), and SSG (Sclerotinia sclerotiorum) [27, 28]. Fruit pieces and cultured mycelium of these mushrooms contain these biologically active polysaccharides with treatment advantage. Yeast and mushroom’s β-glucans are often considered for experimental studies due to their easy purification and high amount of polysaccharide in their cell wall [29, 30].
Structurally β-glucans consist of a backbone of β-(1 → 3)-linked-D-glucopyranosyl units with β-(1 → 6)-linked side chains of varying distribution and length. The differences in the structure, length of the polysaccharide chain, branches, and molecular weight influence the activity of the β-glucans. Oat and barley β-glucans are primarily linear with large regions of β-(1 → 4) linkages separating shorter stretches of β-(1 → 3) structures, whereas mushroom’s β-glucans have short branches with the β-(1 → 3) backbone [31]. Yeast β-glucans have β-(1 → 6) branches that are linked with the more β-(1 → 3) unit. Overall, in vitro studies have indicated that large molecular weight or particular β-glucans (such as zymosan) can activate leukocytes, inducing the production of reactive oxygen and nitrogen intermediates. Intermediate or low molecular weight glucans (such as glucan phosphate) have biological activity in vivo, while very short β-glucans such as laminarin (molecular weight; < 5000–10,000) are mostly inactive [32–34]. High levels of β-glucans were extracted from oat grain to use in food products, which is used as an agglomerated food additive which boosts the immune system. Production of prebiotic sausage has also been facilitated by using a combination of β-glucan and resistant starch [35].
The health benefits of oral administration of β-glucans have been shown in several clinical trials. The cyclic glucans and β-glucan-chitosan complex are shown to have therapeutic effects in wound healing both in human and mice [36]. Furthermore, β-glucan- chitosan complex sheet or a film-forming moisturizer are a promising new wound dressing products [37]. Additionally, use of β-glucan in the healing of partial-thickness burns has shown promising results [38]. Some other benefits of β-glucans are in vaccinology, where they effectively promote protective T cell activities and antibody responses and act as strong immunomodulators for T cell and antibody responses [39, 40]. β-glucans stimulate the immune system and are cell response modifiers through specific receptors by modulating activities of several mediators including cytokines, chemokines, and transcriptional and growth factors. It is established that β-glucans have different receptors on the surface of immune cells such as monocytes, macrophages, dendritic cells (DCs), neutrophils and natural killer (NK) cells [41] (Fig. 1 a and b). Some of these receptors include complement receptor 3 (CR3), Lactosylceramide (LacCer; CDw17) and Lactosylceramide (LacCer; CDw17) and dectin-1 receptors [42–44]. On the other hand, β-glucans in the cell wall of microorganisms such as fungi are known as Pathogen-Associated Molecular Patterns (PAMPs) recognized by host innate immune system which have an important role in the elimination of fungal infections. One of the significant receptors for recognizing β-glucan on monocyte/macrophage lineages and neutrophils and with lower frequency on T cells is dectin-1 (β-glucan receptor, β GR) containing a unique structure comprised mainly of immunoreceptor tyrosine-based activation motif. This receptor recognizes carbohydrates containing β-(1 → 3) and/or β-(1 → 6)- glucan linkages [45]. A key role for dectin-1 together with Toll-like receptor 2 (TLR2) has been proven for activation of macrophages in inducing inflammatory responses against bacterial infection [46, 47]. Also, in human neutrophils, β-(1 → 6)-glucan elicit the phagocytosis, production of reactive oxygen species, and expression of heat shock proteins (HSPs) [48].
Function of β-glucan on innate and adaptive immune system. β-glucans can function on a variety of membrane receptors expressed on the immune cells. a Initially β-glucans are bound through dectin-1, Toll-like receptors (TLRs) and complement receptor 3 (CR3) receptors expressed on macrophages, neutrophils, and dendritic cells. Various signaling pathways are activated (not shown) and subsequence leading to proinflammatory cytokine production including IL-12, IL-1, IL-6, and tumor necrosis factor α (TNFα) as well as costimulatory molecule expressions such as B7.1 and B7.2 on macrophages and dendritic cells. These cytokines and costimulatory molecules lead to stimulation and activation of T lymphocyte (TH and TC). Finally, TC lymphocytes via releasing cytotoxic substrates such as perforin and granzyme can provide an environment for killing tumor cells. b β-glucan binds to CR3 on natural killer (NK) cells and activates them. NK cells after activation by β-glucans via releasing perforin and granzyme can directly kill the tumor cells (TH: T helper and TC: T cytotoxic)
Several signaling molecules are shown to be involved in this process including NF-κB (through Syk-mediated pathway), signaling adaptor protein CARD9 and nuclear factor of activated T cells (NFAT). This process will ultimately lead to the release of cytokines such as interleukin (IL)-12, IL-6, tumor necrosis factor (TNF)-α, and IL-10 [49–51]. Several in vitro and in vivo studies have demonstrated the role of β-glucans in host immunity against infections and its enhancing effect on immune responses. Roudbary et al. showed that standard pure powder of β-glucan in Saccharomyces cerevisiae can stimulate the Balb/c macrophages to the produce nitric oxide (NO). Moreover, the supernatant of macrophages stimulated with β-glucan had a significant cytotoxic effect on WEHI-164 cells (fibrosarcoma cell line) in the TNF-α bioassay [52]. Kournikakis et al. assessed the effect of β-glucan on protection against anthrax in a mouse model of anthrax infection. Results demonstrated the potential immunomodulatory effect of β-(1 → 3)-glucan to provide a significant protection against anthrax [53]. Moreover, in a clinical trial performed by medeiros et al., the effects of the β-glucan on wound healing were evaluated on human venous ulcers monitored by histopathological analysis after 30 days of topical treatment. Results showed that β-(1 → 3)-glucan improved ulcer healing by potentiating epithelial hyperplasia, inflammatory responses, angiogenesis and fibroblast proliferation [54].
β-glucans as anticancer agents
It is well-documented that β-glucans have anticancer activity through a biological response modifier (BRM) effect when administered in the form of drug or food supplement which was first displayed by animal experiments [55, 56]. The antitumor mechanism of β-glucans might involve inhibition of tumor growth through the enhancement of immune system (i.e. activation of T-cells, B-cells, macrophages and NK cells and production of cytokines) [57]. Schizophyllan, one of the β-glucans has antitumor activity and clinically acts as an immunomodulator against several cancer types where its antitumor effect is related to the triple helical structure of β-glucan’s backbone chain. For example, the triple helical structure of β-glucans inhibited the growth of ascites in mice [58]. Administration of β-glucans from Lentinan along with chemotherapy resulted in prolonged survival in colorectal cancer patients [59]. Orally delivered β-glucan is found to increase proliferation rate and activation of monocytes in peripheral blood of patients with advanced breast cancer [60]. A targeted delivery system for doxorubicin (Dox) using β-(1 → 3)-glucan (Glu) was used as a carrier covered by trastuzumab antibody to treat Her 2+ breast tumor implant in mice. Glu-Dox targeted nanoparticles proved to have significant advantages for delivering anticancer drugs to target tissues [61]. Additionally, β-glucans can serve as potent adjuvants for tumor vaccines which elicit both potent cytotoxic T lymphocyte (CTL) responses as well as humoral responses. Moreover, combined therapy with β-glucans can add another protective layer of innate immunity toward the adaptive antitumor immunity. Therefore, β-glucan mediated therapy can target both granulocytes and CTLs to give a more effective means of eliminating tumors and developing a long-term tumor-specific T cell immunity that prevents tumor recurrence [62].
β-glucan and lung cancer
In this section, we summarize the chemopreventive effect of β-glucans obtained from different sources studied from 1991 to 2016, in primary lung cancer and other tumor cells metastasized to the lung in experimental studies, as well as in clinical trials.
Laboratory and animal studies
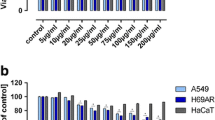
Suzuki et al. showed that SSG, a β-(1 → 3)-D-glucan obtained from Sclerotina Sclerotiorum IFO 9395, administered by either through oral or intraperitoneal route, inhibited the experimental pulmonary metastasis of Lewis lung carcinoma (3LL) cells in mice. They concluded that the effector cells of immune systems, such as macrophages and NK cells, activated by the administration of SSG, may inhibit the processes of the implantation of 3LL cells in the lungs and also inhibit the growth of the metastasizing cells in new tumor colonies [63]. Yoon et al. examined the prophylactic administration of β-glucan purified from mutated S. cerevisiae (IS-2) in experimental lung metastasis model of colon 26-M3.1 carcinoma or B16-BL6 melanoma cells, showing that it significantly inhibits lung metastasis in a dose-dependent manner. Also, pretreatment with IS-2 two days before tumor inoculation significantly prolonged the survival time of the tumor-bearing mice [64]. Furthermore, therapeutic administration of IS-2 also significantly inhibited the growth of colon cancer cell line 26-M3.1 in mice. On the other hand, Maitake D-Fraction extracted from Grifola frondosa (Maitake mushroom) containing β-(1 → 6)-glucan with β-(1 → 3) branched chains have been found to possess strong anticancer activity by increasing immune-competent cellular activity [65]. Kobayashi et al. at showed that oral supplementation with β-(1 → 6)-D-glucan extracted from Agaricus blazei Murill used as a food supplement for the prevention of cancer, reduced pulmonary metastasis of 3LL cells in mice, and inhibited the growth of these metastatic tumors in lung, in part by suppressing urokinase-type plasminogen activator (uPA) expression [66]. Moreover, Yamamoto et al. reported that the growth rate of subcutaneously injected B16-BL6 tumor cells (mouse melanoma cell lines) in C57BL/6 J mice was suppressed by the oral administration of β-D-glucan extracted from Sparassis Crispa (SBG), an edible mushroom with medicinal properties. Furthermore, the number, as well as the size of lung metastatic tumor colonies, was significantly reduced by SBG administration through the inhibition of tumor-induced angiogenesis. The results indicated that oral administration of SBG can suppress tumor angiogenesis and metastasis [67]. Another study by Li et al. investigated the effect of β-glucan therapy on antitumor adaptive T cell responses against Lewis lung carcinoma model. Orally administered particulate β-glucan trafficked into spleen and lymph nodes; activated dendritic cells captured apoptotic LLC/ovalbumin cells in-vivo and up-regulated accessory surface molecules on dendritic cells, leading to the expansion and activation of antigen-specific CD4 and CD8 T cells. In their study, they clearly showed the ability of yeast-derived β-glucan as an adjuvant for tumor immunotherapy [68]. In another study, Thetsrimuang et al. reported that crude polysaccharides obtained from Lentinus polychrous Lév possess variable antioxidant activities and might serve as a possible immunomodulatory agent for cancer prevention. Although their antioxidant activities were weak, these polysaccharides had certain cytotoxic effects on cancer cell lines A549 (non-small cell lung adenocarcinoma), MCF-7 (breast adenocarcinoma), SK-Hep1 (hepatocarcinoma) [69]. This natural compound is shown to enhance anticancer effects when combined with chemotherapy. Kogan, et al. showed that antitumor and antimetastatic activity of cyclophosphamide can be enhanced through the addition of carboxymethylated β-(1 → 3)-D-glucan, a well-known macrophage stimulator, in the Lewis lung carcinoma model [70]. Moreover, combined use of several natural immunomodulators is getting much of attention. Vetvicka et al. showed that combination of glucan/resveratrol and glucan/vitamin C suppresses the growth of lung tumors via the stimulation of apoptosis in a mouse model of lung cancer [71]. On the other hand, diet and exercise can have beneficial preventive effects on the initiation and growth of some types of cancer [72, 73]. Murphy et al. investigated the effects of moderate exercise and oat glucan on lung tumor metastasis. The results of this study showed that short-term moderate exercise training and consumption of the soluble fiber oat-glucan can decrease the metastatic spread of injected B16 melanoma cells to the lungs in an experimental tumor metastasis model. The effects may be mediated in part by an increase in macrophage cytotoxicity and antitumor function against the B16 melanoma [74]. Photodynamic therapy (PDT) combines pretreatment with a drug or photosensitizer with a specific type of laser to kill the cancer cells. The cellular damage induced by PDT leads to activation of the DNA damage repair mechanisms, which is an important factor for modulating tumor sensitivity to this treatment type [75]. Akramiene et al. demonstrated that PDT in combination with barley, baker’s yeast, or marinebrown algae containing glucan significantly reduced tumor growth and the expression of proliferating cell nuclear antigen, and increased necrosis in tumor tissues in C57BL/6 Lewis lung carcinoma xenograft model. The study showed that β-glucans enhance tumor response to PDT, resulting in increased necrosis of PDT-treated tumors and suppression of the DNA damage repair system [76].
As mentioned above, β-glucan significantly augments antibody-mediated antitumor activity via stimulation of the CR3. Monoclonal antibodies (mAb) against tumor cells bind to tumors coated with iC3b and activate complement. Soluble yeast β-(1 → 3);(1 → 6)-glucan and soluble barley β-(1 → 3);(1 → 4)-glucan bind to CR3 (iC3b receptors) in leukocytes and primes to this receptor to enhance leukocyte mediated cytotoxicity against tumor cells coated with iC3b [77]. Hong et al. treated mice bearing Lewis lung carcinoma cells transduced with human MUC1 (LL/2-MUC1) with anti-MUC1 mAb. Treatment with oral barley or yeast β-(1 → 3)- glucan and mAb elicited significantly enhanced tumor regression compared with that mediated by mAb alone. By contrast, neither β-(1 → 3)-glucan given orally alone or in combination with anti-MUC1 mAb could promote tumor regression in C3-deficient mice. The results indicated that β-(1 → 3)-glucan promoted this activity through mouse NK cells that express CR3 [77]. Li et al. designed the combination of yeast-derived β-glucan with antitumor mAb. They demonstrated that the combined immunotherapy was therapeutically effective against human NSCLC cells NCI-H23, but this influence did not find in human ovarian carcinoma cells SKOV-3 [78]. Zhong et al. investigated combined bevacizumab and β-glucan therapy for human lung cancer using murine xenograft model. They showed that in xenograft mouse model of human lung adenocarcinoma expressing tumor surface vascular endothelial growth factor (VEGF), intravenous administration of yeast-derived β-glucan significantly enhanced the effect of bevacizumab in inhibiting tumor growth and improving overall survival. Therefore, yeast-derived β-glucan augments bevacizumab-mediated therapeutic efficacy against human NSCLC tumors which express membrane-bound VEGF [79]. Also, yeast-derived β-glucan supplementation significantly reduced the number and weight of primary tumors and the number of metastatic lung colonies in mice inoculated with B16 melanoma cells [80]. Moreover, polysaccharides can activate monocytes, macrophages, neutrophils, and NK cells in the absence of antibodies via glucan receptors (dectin-1 and CR3). Lo et al. showed that co-culture of irradiated human lung adenocarcinoma A549 cells with the branched α-(1 → 4)-glucan-activated THP-1 cells (a human monocyte cell line) resulted in significant decrease in the percentage of viable A549 cells from 66 to 37% and also increased levels of IL-8, RANTES and superoxide, and decreased levels of VEGF and angiogenin in THP-1 cells [81]. The results also indicated that combining radiotherapy with branched α-(1 → 4)-glucan stimulated monocytes decreased the viability of A549 lung cancer cells by stimulating inflammatory and cytotoxic responses [81]. Also, the effect of γ-irradiated β-glucan in in vivo and in vitro models was shown by Byun et al. showing that low-molecular-weight β-glucan (LMBG) produced by γ-irradiation (50 kGy) more effectively inhibited tumor growth and lung metastasis in comparison with high-molecular-weight β-glucan (HMBG) in mice injected with B16BL6 melanoma cells [82]. A recent study showed that β-glucan affects the number of different Myeloid-Derived Suppressor Cells (MDSC) subsets in the tumor [83]. MDSCs are a heterogeneous population of immature myeloid cells that promote tumor progression. It has been well documented that MDSC accumulates in different human cancers such as the brain [84], head and neck [85], breast [86], lung cancers [87] and others. Albeituni et al. demonstrated that in-vivo treatment of mice bearing lewis lung carcinoma and mammary cell carcinoma with particulate β-glucan decreased tumor weight and splenomegaly, and decreased the accumulation of polymorphonuclear-MDSC but not monocytic-MDSC in the spleen and within the tumor [83].
Clinical trials of β-glucan in lung cancer
A few clinical trials have studied the effect of β-glucans derived from various sources in lung cancer patients (Table 1). Maitake D-Fraction containing β-(1 → 6)-glucan was shown to decrease the size of a lung tumor in >60% of patients when it was combined with chemotherapy in a clinical cohort comparing with chemotherapy alone [88]. Ganoderma polysaccharides are β-glucans derived from Ganoderma lucidum (Lingzhi, Reishi) with an antitumor activity which enhance host immune responses in patients with advanced solid tumors. In an open-label study performed by Gao et al. on patients with advanced lung cancer, thirty-six patients were treated with 5.4 g/day Ganopoly for 12 weeks and some cancer patients showed markedly modulated immune functions including changes in IL-1, IL-12 and NK activity [89]. These findings showed that subgroups of patients might be responsive to Ganopoly in combination with chemotherapy and/or radiotherapy. Also, another trial was performed by Weinberg et al. on twenty patients with advanced malignancies (three of patients had NSCLC) receiving chemotherapy were given a β-(1 → 3)/(1 → 6)- D-glucan preparation. This trial demonstrates that β-(1 → 3)/(1 → 6) - D-glucan is very well-tolerated in patients with advanced cancers receiving chemotherapy [90]. Moreover, in a study by Albeituni et al. a particulate β-glucan extracted from Saccharomyces cerevisiae was undertaken in patients with NSCLC that were newly diagnosed and had not received any treatment. Particulate β-glucan was administered orally 500 mg per dose for two weeks and blood was withdrawn before and after treatment. Particulate β-glucan treatment significantly reduced the percentage of HLA-DR-CD14-CD33 + CD11b + MDSC in the peripheral blood of NSCLC patients when compared to the peripheral blood samples obtained before the treatment [83]. These results showed that particulate β-glucan may be a potent immunomodulator of MDSCs suppressive function against cancer.
Conclusion and future directions
These results indicate that use of β-glucans derived from various sources can possess chemopreventive effects in experimental models as well as in clinical subjects. However, it is essential to investigate effect(s) of purified products of β-glucans on immune cells with antitumor activities which might cause tumor regression such as M2 macrophage and regulatory T cells in animal model of lung cancer and in cancer patients. So far, only a few clinical trials have been performed on assessing the effectiveness of purified β-glucans in combination with anticancer drugs. These studies had relatively small sample sizes and also generally did not show promising results on cancer patients. Therefore, additional well-designed clinical trials are needed to verify the actual clinical efficacy of β-glucans. Emerging evidence shows the critical role of cancer stem cells (CSCs) in lung tumor initiation, maintenance, drug resistance, metastasis, and relapse, but to the best of our knowledge, the effect of β-glucans on lung CSCs have not been studied yet, which is likely a good subject for future studies.
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66:7–30. doi:10.3322/caac.21332
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108. doi:10.3322/caac.21262
Herbst RS, Heymach JV, Lippman SM (2008) Lung cancer. N Engl J Med 359:1367–1380. doi:10.1056/NEJMra0802714
Youlden DR, Cramb SM, Baade PD (2008) The international epidemiology of lung cancer: geographical distribution and secular trends. J Thorac Oncol 3:819–831. doi:10.1097/JTO.0b013e31818020eb
Scott WJ, Howington J, Feigenberg S, Movsas B, Pisters K (2007) Treatment of non-small cell lung cancer stage I and stage II: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 132:234s–42s. doi: 10.1378/chest.07-1378
Robinson LA, Ruckdeschel JC, Wagner H, Stevens CW (2007) Treatment of non-small cell lung cancer-stage IIIA: ACCP evidence-based clinical practice guidelines. Chest 132:243S–265S. doi:10.1378/chest.07-1379
Lardinois D, Suter H, Hakki H, Rousson V, Betticher D, Ris H-B (2005) Morbidity, survival, and site of recurrence after mediastinal lymph-node dissection versus systematic sampling after complete resection for non-small cell lung cancer. Ann Thorac Surg 80:268–275. doi:10.1016/j.athoracsur.2005.02.005
Reck M, Heigener DF, Mok T, Soria J-C, Rabe KF (2013) Management of non-small-cell lung cancer: recent developments. Lancet 382:709–719. doi:10.1016/S0140-6736(13)61502-0
Afanasjeva J, Hui RL, Spence MM, Chang J, Schottinger JE, Millares M, Rashid N (2016) Identifying subsequent therapies in patients with advanced non–small cell lung cancer and factors associated with overall survival. Pharmacotherapy 36:1065–1074. doi:10.1002/phar.1826
Nassar D, Blanpain C (2016) Cancer stem cells: basic concepts and therapeutic implications. Annu Rev Pathol 11:47–76. doi:10.1146/annurev-pathol-012615-044438
Soltanian S, Matin MM (2011) Cancer stem cells and cancer therapy. Tumour Biol 32:425–440. doi:10.1007/s13277-011-0155-8
Roudi R, Madjd Z, Ebrahimi M, Najafi A, Korourian A, Shariftabrizi A, Samadikuchaksaraei A (2016) Evidence for embryonic stem-like signature and epithelial-mesenchymal transition features in the spheroid cells derived from lung adenocarcinoma. Tumour Biol 37:11843–11859. doi:10.1007/s13277-016-5041-y
Roudi R, Korourian A, Shariftabrizi A, Madjd Z (2015) Differential expression of cancer stem cell markers ALDH1 and CD133 in various lung cancer subtypes. Cancer Investig 33:294–302. doi:10.3109/07357907.2015.1034869
Roudi R, Madjd Z, Korourian A, Mehrazma M, Molanae S, Sabet MN, Shariftabrizi A (2014a) Clinical significance of putative cancer stem cell marker CD44 in different histological subtypes of lung cancer. Cancer Biomark 14:457–467. doi:10.3233/CBM-140424
Roudi R, Madjd Z, Ebrahimi M, Samani FS, Samadikuchaksaraei A (2014b) CD44 and CD24 cannot act as cancer stem cell markers in human lung adenocarcinoma cell line A549. Cell Mol Biol Lett 19:23–36. doi:10.2478/s11658-013-0112-1
O’Brien CA, Pollett A, Gallinger S, Dick JE (2007) A human colon cancer cell capable of initiating tumour growth in immunodeficient mice. Nature 445:106–110. doi:10.1038/nature05372
Collins AT, Berry PA, Hyde C, Stower MJ, Maitland NJ (2005) Prospective identification of tumorigenic prostate cancer stem cells. Cancer Res 65:10946–10951. doi:10.1158/0008-5472.CAN-05-2018
Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF (2003) Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci U S A 100:3983–3988. doi:10.1073/pnas.0530291100
Li F, Zhou K, Gao L, Zhang B, Li W, Yan W (2016) Radiation induces the generation of cancer stem cells: a novel mechanism for cancer radioresistance. Oncol Lett 12:3059–3065. doi:10.3892/ol.2016.5124
Tirino V, Desiderio V, Paino F, De Rosa A, Papaccio F, La Noce M, Laino L, De Francesco F, Papaccio G (2013) Cancer stem cells in solid tumors: an overview and new approaches for their isolation and characterization. FASEB J 27:13–24. doi:10.1096/fj.12-218222
Luo J, Shen L, Zheng D (2014) Association between vitamin C intake and lung cancer: a dose-response meta-analysis. Sci Rep 4:6161. doi:10.1038/srep06161
Zhang L, Wang S, Che X, Li X (2015) Vitamin D and lung cancer risk: a comprehensive review and meta-analysis. Cell Physiol Biochem 36:299–305. doi:10.1159/000374072
Aleem E (2013) β-glucans andtheir applications in cancer therapy: focus on human studies. Anti Cancer Agents Med Chem 13:709–719
Tokunaka K, Ohno N, Adachi Y, Miura NN, Yadomae T (2002) Application of Candida solubilized cell wall β-glucan in antitumor immunotherapy against P815 mastocytoma in mice. Int Immunopharmacol 2:59–67
Tokunaka K, Ohno N, Adachi Y, Tanaka S, Tamura H, Yadomae T (2000) Immunopharmacological and immunotoxicological activities of a water-soluble (1→ 3)-β-d-glucan, CSBG from Candida spp. Int J Immunopharmacol 22:383–394
Baur S, Geisler G (1996) Variability of the beta-glucan content in oat caryopsis of 132 cultivated-oat genotypes and 39 wild-oat genotypes. J Agron Crop Sci 176:151–157
Borchers AT, Keen CL, Gershwin ME (2004) Mushrooms, tumors, and immunity: an update. Exp Biol Med (Maywood) 229:393–406
Wasser S (2002) Medicinal mushrooms as a source of antitumor and immunomodulating polysaccharides. Appl Microbiol Biotechnol 60:258–274. doi:10.1007/s00253-002-1076-7
Chan WK, Lam DTW, Law HKW, Wong WT, Leung Koo MW, Lau ASY, Chan GC (2005) Ganoderma lucidum mycelium and spore extracts as natural adjuvants for immunotherapy. J Altern Complement Med 11:1047–1057. doi:10.1089/acm.2005.11.1047
Vetvicka V, Dvorak B, Vetvickova J, Richter J, Krizan J, Sima P, Yvin JC (2007) Orally administered marine (1→ 3)-β-D-glucan Phycarine stimulates both humoral and cellular immunity. Int J Biol Macromol 40:291–298
Driscoll M, Hansen R, Ding C, Cramer DE, Yan J (2009) Therapeutic potential of various β-glucan sources in conjunction with anti-tumor monoclonal antibody in cancer therapy. Cancer Biol Ther 8:218–225
Brown GD, Gordon S (2003) Fungal β-glucans and mammalian immunity. Immunity 19:311–315
Ishibashi K-I, Miura NN, Adachi Y, Ohno N, Yadomae T (2001) Relationship between solubility of grifolan, a fungal 1, 3-β-D-glucan, and production of tumor necrosis factor by macrophages in vitro. Biosci Biotechnol Biochem 65:1993–2000
Lee D-Y, Ji I-H, Chang H-I, C-W KIM (2002) High-level TNF-α secretion and macrophage activity with soluble β-glucans from Saccharomyces cerevisiae. Biosci Biotechnol Biochem 66:233–238. doi:10.1271/bbb.66.233
Ahmad A, Munir B, Abrar M, Bashir S, Adnan M, Tabassum T (2012) Perspective of β-glucan as functional ingredient for food industry. J Nutr Food Sci 2:2
Gulcelik MA, Dincer H, Sahin D, Faruk DO, Yenidogan E, Alagol H (2010) Glucan improves impaired wound healing in diabetic rats. Wounds 22:12–16
Kim J-Y, Jun J-H, Kim S-J, Hwang K-M, Choi SR, Han SD, Son MW, Park ES (2015) Wound healing efficacy of a chitosan-based film-forming gel containing tyrothricin in various rat wound models. Arch Pharm Res 38:229–238. doi:10.1007/s12272-014-0368-7
Delatte SJ, Evans J, Hebra A, Adamson W, Othersen HB, Tagge EP (2001) Effectiveness of beta-glucan collagen for treatment of partial-thickness burns in children. J Pediatr Surg 36:113–118. doi:10.1053/jpsu.2001.20024
Cheung N-KV, Modak S, Vickers A, Knuckles B (2002) Orally administered β-glucans enhance anti-tumor effects of monoclonal antibodies. Cancer Immunol Immunother 51:557–564. doi:10.1007/s00262-002-0321-3
Huang H, Ostroff GR, Lee CK, Specht CA, Levitz SM (2013) Characterization and optimization of the glucan particle-based vaccine platform. Clin Vaccine Immunol 20(10):1585–1591. doi:10.1128/CVI.00463-13
Rice PJ, Kelley JL, Kogan G, Ensley HE, Kalbfleisch JH, Browder IW, Williams DL (2002) Human monocyte scavenger receptors are pattern recognition receptors for (1→ 3)-β-D-glucans. J Leukoc Biol 72(1):140–146
Herre J, Gordon S, Brown GD (2004)Dectin-1 and its role in the recognition of β-glucans by macrophages. Mol Immunol 40:869–876
Schorey J, Lawrence C (2008) Thepattern recognition receptor Dectin-1: from fungi to mycobacteria. Curr Drug Targets 9:123–129
Zimmerman JW, Lindermuth J, Fish PA, Palace GP, Stevenson TT, DeMong DE (1998) A novel carbohydrate-glycosphingolipid interaction between a β-(1–3)-glucan immunomodulator, PGG-glucan, and lactosylceramide of human leukocytes. J Biol Chem 273:22014–22020
Taylor PR, Brown GD, Reid DM, Willment JA, Martinez-Pomares L, Gordon S, Wong SY (2002) The β-glucan receptor, dectin-1, is predominantly expressed on the surface of cells of the monocyte/macrophage and neutrophil lineages. J Immunol 169:3876–3882
Gantner BN, Simmons RM, Canavera SJ, Akira S, Underhill DM (2003) Collaborative induction of inflammatory responses by dectin-1 and toll-like receptor 2. J Exp Med 197:1107–1117
Yadav M, Schorey JS (2006) The β-glucan receptor dectin-1 functions together with TLR2 to mediate macrophage activation by mycobacteria. Blood 108:3168–3175. doi:10.1182/blood-2006-05-024406
Rubin-Bejerano I, Abeijon C, Magnelli P, Grisafi P, Fink GR (2007) Phagocytosis by humanneutrophils is stimulated by a unique fungal cell wall component. Cell Host Microbe 2:55–67. doi:10.1016/j.chom.2007.06.002
Goodridge HS, Simmons RM, Underhill DM (2007) Dectin-1 stimulation by Candida albicans yeast or zymosan triggers NFAT activation in macrophages and dendritic cells. J Immunol 178:3107–3115
Gross O, Gewies A, Finger K, Schäfer M, Sparwasser T, Peschel C, Förster I, Ruland J (2006) Card9 controls a non-TLR signalling pathway for innate anti-fungal immunity. Nature 442:651–656. doi:10.1038/nature04926
Rogers NC, Slack EC, Edwards AD, Nolte MA, Schulz O, Schweighoffer E, Williams DL, Gordon S, Tybulewicz VL, Brown GD, Reisesousa C (2005) Syk-dependent cytokine induction by Dectin-1 reveals a novel pattern recognition pathway for C type lectins. Immunity 22:507–517. doi:10.1016/j.immuni.2005.03.004
Roudbary M, Daneshmandi S, Hajimoradi M, Roudbarmohammadi S, Hassan ZM (2015) Immunomodulatory effect of β-glucan on peritoneal macrophages of Bab1/c mice. Pol J Microbiol 64:175–179
Kournikakis B, Mandeville R, Brousseau P, Ostroff G (2003) Anthrax-protective effects of yeast beta 1, 3 glucans. MedGenMed 5:1
Medeiros SD, Cordeiro SL, Cavalcanti JE, Melchuna KM, Lima AM, Filho IA, Medeiros AC, Rocha KB, Oliveira EM, Faria ED, Sassaki GL, Rocha HA, Sales VS (2012) Effects of purified Saccharomyces cerevisiae (1→ 3)-β-glucan on venous ulcer healing. Int J Mol Sci 13:8142–8158. doi:10.3390/ijms13078142
McIntosh M, Stone B, Stanisich V (2005) Curdlan and other bacterial (1→ 3)-β-D-glucans. Appl Microbiol Biotechnol 68:163–173. doi:10.1007/s00253-005-1959-5
Kidd PM (2000) The use of mushroom glucans and proteoglycans in cancer treatment. Altern Med Rev 5:4–27
Han S-SR, Cho C-K, Lee Y-W, Yoo H-S (2009) Antimetastatic and immunomodulating effect of water extracts from various mushrooms. J Acupunct Meridian Stud 2:218–227. doi:10.1016/S2005-2901(09)60058-3
Kulicke W-M, Lettau AI, Thielking H (1997) Correlation between immunological activity, molar mass, and molecular structure of different (1→ 3)-β-D-glucans. Carbohydr Res 297:135–143
Hazama S, Watanabe S, Ohashi M, Yagi M, Suzuki M, Matsuda K, Yamamoto T, Suga Y, Suga T, Nakazawa S, Oka M (2009) Efficacy of orally administered superfine dispersed lentinan (β-1, 3-glucan) for the treatment of advanced colorectal cancer. Anticancer Res 29:2611–2617
Demir G, Klein H, Mandel-Molinas N, Tuzuner N (2007) Beta glucan induces proliferation and activation of monocytes in peripheral blood of patients with advanced breast cancer. Int Immunopharmacol 7:113–116. doi:10.1016/j.intimp.2006.08.011
Nasrollahi Z, Mohammadi SR, Mollarazi E, Yadegari MH, Hassan ZM, Talaei F, Dinarvand R, Akbari H, Atyabi F (2015) Functionalized nanoscale β-1, 3-glucan to improve Her2+ breast cancer therapy: in vitro and in vivo study. J Control Release 202:49–56. doi:10.1016/j.jconrel.2015.01.014
Boscardin SB, Hafalla JC, Masilamani RF, Kamphorst AO, Zebroski HA, Rai U, Morrot A, Zavala F, Steinman RM, Nussenzweig RS, Nussenzweig MC (2006) Antigen targeting to dendritic cells elicits long-lived T cell help for antibody responses. J Exp Med 203:599–606. doi:10.1084/jem.20051639
Suzuki I, Sakurai T, Hashimoto K, Oikawa S, Masuda A, Ohsawa M, Yadomae T (1991) Inhibition of experimental pulmonary metastasis of Lewis lung carcinoma by orally administered beta-glucan in mice. Chem Pharm Bull (Tokyo) 39:1606–1608
Yoon TJ, Kim TJ, Lee H, Shin KS, Yun YP, Moon WK, Kim DW, Lee KH (2008) Anti-tumor metastatic activity of β-glucan purified from mutated Saccharomyces cerevisiae. Int Immunopharmacol 8:36–42. doi:10.1016/j.intimp.2007.10.005
Lin H, Cheung SW, Nesin M, Cassileth BR, Cunningham-Rundles S (2007) Enhancement of umbilical cord blood cell hematopoiesis by maitake beta-glucan is mediated by granulocyte colony-stimulating factor production. Clin Vaccine Immunol 14:21–27. doi:10.1128/CVI.00284-06
Kobayashi H, Yoshida R, Kanada Y, Fukuda Y, Yagyu T, Inagaki K, Kondo T, Kurita N, Suzuki M, Kanayama N, Terao T (2005) Suppressing effects of daily oral supplementation of beta-glucan extracted from Agaricus blazei Murill on spontaneous and peritoneal disseminated metastasis in mouse model. J Cancer Res Clin Oncol 131:527–538. doi:10.1007/s00432-005-0672-1
Yamamoto K, Kimura T, Sugitachi A, Matsuura N (2009) Anti-angiogenic and anti-metastatic effects of β-1, 3-D-glucan purified from Hanabiratake, Sparassis crispa. Biol Pharm Bull 32:259–263
Li B, Cai Y, Qi C, Hansen R, Ding C, Mitchell TC, Yan J (2010) Orally administered particulate β-glucan modulates tumor-capturing dendritic cells and improves antitumor T-cell responses in cancer. Clin Cancer Res 16:5153–5164. doi:10.1158/1078-0432.CCR-10-0820
Queiroz EA, Fortes ZB, da Cunha MA, Barbosa AM, Khaper N, Dekker RF (2015) Antiproliferative and pro-apoptotic effects of three fungal exocellular β-glucans in MCF-7 breast cancer cells is mediated by oxidative stress, AMP-activated protein kinase (AMPK) and the Forkhead transcription factor, FOXO3a. Int J Biochem Cell Biol 67:14–24. doi:10.1016/j.biocel.2015.08.003
Kogan G, Šandula J, Korolenko TA, Falameeva OV, Poteryaeva ON, Zhanaeva SY, Levina OA, Filatova TG, Kaledin VI (2002) Increased efficiency of Lewis lung carcinoma chemotherapy with a macrophage stimulator—yeast carboxymethyl glucan. Int Immunopharmacol 2:775–781
Vetvicka V, Vetvickova J (2012) Combination of glucan, resveratrol and vitamin C demonstrates strong anti-tumor potential. Anticancer Res 32:81–87
Friedenreich CM, Orenstein MR (2002) Physical activity and cancer prevention: etiologic evidence and biological mechanisms. J Nutr 132:3456S–3464S
Greenwald P, Clifford C, Milner J (2001) Diet and cancer prevention. Eur J Cancer 37:948–965
Murphy E, Davis J, Brown AS, Carmichael MD, Mayer EP, Ghaffar A (2004) Effects of moderate exercise and oat β-glucan on lung tumor metastases and macrophage antitumor cytotoxicity. J Appl Physiol 97:955–959. doi:10.1152/japplphysiol.00252.2004
Vrouenraets MB, Visser G, Snow G, Van Dongen G (2003) Basic principles, applications in oncology and improved selectivity of photodynamic therapy. Anticancer Res 23:505–522
Akramiene D, Aleksandraviciene C, Grazeliene G, Zalinkevicius R, Suziedelis K, Didziapetriene J, Simonsen U, Stankevicius E, Kevelaitis E (2010) Potentiating effect of β-glucans on photodynamic therapy of implanted cancer cells in mice. Tohoku J Exp Med 220:299–306
Hong F, Yan J, Baran JT, Allendorf DJ, Hansen RD, Ostroff GR, Xing PX, Cheung NK, Ross GD (2004) Mechanism by which orally administered β-1, 3-glucans enhance the tumoricidal activity of antitumor monoclonal antibodies in murine tumor models. J Immunol 173:797–806
Li B, Allendorf DJ, Hansen R, Marroquin J, Cramer DE, Harris CL, Yan J (2007) Combined yeast β-glucan and antitumor monoclonal antibody therapy requires C5a-mediated neutrophil chemotaxis via regulation of decay-accelerating factor CD55. Cancer Res 67:7421–7430. doi:10.1158/0008-5472.CAN-07-1465
Zhong W, Hansen R, Li B, Cai Y, Salvador C, Moore GD, Yan J (2009) Effect of yeast-derived β-glucan in conjunction with bevacizumab for the treatment of human lung adenocarcinoma in subcutaneous and orthotopic xenograft models. J Immunother 32:703–712. doi:10.1097/CJI.0b013e3181ad3fcf
Vetvicka V, Vetvickova J (2015) Glucan supplementation has strong anti-melanoma effects: role of NK cells. Anticancer Res 35:5287–5292
Lo TC-T, Hsu F-M, Chang CA, Cheng JC-H (2011) Branched α-(1, 4) glucans from Lentinula edodes (L10) in combination with radiation enhance cytotoxic effect on human lung adenocarcinoma through the toll-like receptor 4 mediated induction of THP-1 differentiation/activation. J Agric Food Chem 59:11997–12005
Byun EB, Park SH, Jang BS, Sung NY, Byun EH (2016) Gamma-irradiated β-glucan induces immunomodulation and anticancer activity through MAPK and NF-κB pathways. J Sci Food Agric 96:695–702. doi:10.1002/jsfa.7215
Albeituni SH, Ding C, Liu M, Hu X, Luo F, Kloecker G, Bousamra M 2nd, Zhang HG, Yan J (2016) Yeast-derived particulate β-glucan treatment subverts the suppression of myeloid-derived suppressor cells (MDSC) by inducing polymorphonuclear MDSC apoptosis and monocytic MDSC differentiation to apc in cancer. J Immunol 196:2167–2180. doi:10.4049/jimmunol.1600346
Raychaudhuri B, Rayman P, Ireland J, Ko J, Rini B, Borden EC, Garcia J, Vogelbaum MA, Finke J (2011) Myeloid-derived suppressor cell accumulation and function in patients with newly diagnosed glioblastoma. Neuro-Oncology 13:591–599. doi:10.1093/neuonc/nor042
Brandau S, Trellakis S, Bruderek K, Schmaltz D, Steller G, Elian M, Suttmann H, Schenck M, Welling J, Zabel P, Lang S (2011) Myeloid-derived suppressor cells in the peripheral blood of cancer patients contain a subset of immature neutrophils with impaired migratory properties. J Leukoc Biol 89:311–317. doi:10.1189/jlb.0310162
Diaz-Montero CM, Salem ML, Nishimura MI, Garrett-Mayer E, Cole DJ, Montero AJ (2009) Increased circulating myeloid-derived suppressor cells correlate with clinical cancer stage, metastatic tumor burden, and doxorubicin–cyclophosphamide chemotherapy. Cancer Immunol Immunother 58:49–59. doi:10.1007/s00262-008-0523-4
Iclozan C, Antonia S, Chiappori A, Chen D-T, Gabrilovich D (2013) Therapeutic regulation of myeloid-derived suppressor cells and immune response to cancer vaccine in patients with extensive stage small cell lung cancer. Cancer Immunol Immunother 62:909–918. doi:10.1007/s00262-013-1396-8
Kodama N, Komuta K, Nanba H (2002) Can maitake MD-fraction aid cancer patients? Altern Med Rev 7:236–239
Gao Y, Tang W, Dai X, Gao H, Chen G, Ye J, Chan E, Koh HL, Li X, Zhou S (2005) Effects of water-soluble Ganoderma lucidum polysaccharides on the immune functions of patients with advanced lung cancer. J Med Food 8:159–168
Weitberg AB (2008) A phase I/II trial of beta-(1, 3)/(1, 6) D-glucan in the treatment of patients with advanced malignancies receiving chemotherapy. J Exp Clin Cancer Res 27:40. doi:10.1186/1756-9966-27-40
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Raheleh Roudi declares that she has no conflict of interest.
Shahla Roudbar Mohammadi declares that she has no conflict of interest.
Maryam Roudbary declares that she has no conflict of interest.
Monireh Mohsenzadegan declares that she has no conflict of interest.
Funding
No.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Roudi, R., Mohammadi, S.R., Roudbary, M. et al. Lung cancer and β-glucans: review of potential therapeutic applications. Invest New Drugs 35, 509–517 (2017). https://doi.org/10.1007/s10637-017-0449-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-017-0449-9