Abstract
Purpose: The Basidiomycete fungus Agaricus blazei Murill has traditionally been used as a health food for the prevention of cancer. Methods: We examined whether beta-(1–6)-D-glucan extracted from A. blazei is a potential anticancer agent in an in vitro and in vivo animal model. Results: Here we show that (1) beta-glucan had cytotoxic effect against human ovarian cancer HRA cells, but not against murine Lewis lung cancer 3LL cells, in vitro; (2) beta-glucan promotes p38 MAPK activity for suppressing HRA cell proliferation and amplifying the apoptosis cascade; (3) beta-glucan stimulates translocation of the proapoptotic protein, Bax, from the cytosol to mitochondria, cytochrome c release, and subsequent caspase-9 activation; (4) treatment with SB203580, a p38 MAPK-specific inhibitor, suppresses beta-glucan-induced effects, indicating that activation of p38 MAPK is involved in the suppression of cell proliferation and mitochondrial activation-mediated cell death pathway; (5) in mice, oral supplementation with beta-glucan reduces pulmonary metastasis of 3LL cells and peritoneal disseminated metastasis of HRA cells and inhibits the growth of these metastatic tumors in lung or peritoneal cavity, in part, by suppressing uPA expression; and (6) in an in vivo experimental metastasis assay, however, the oral supplementation with beta-glucan after i.v. tumor cell inoculation did not reduce the number of lung tumor colonies. Conclusion: Treatment with beta-glucan may be beneficial for cancer patients with or at risk for metastasis. The beta-glucan-dependent signaling pathways are critical for our understanding of anticancer events and development of cancer therapeutic agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Currently, mushroom and fungi brought to attention by complementary and alternative medicine, are undergoing scientific analysis and development to prevent and treat cancer. The edible mushroom Agaricus blazei Murill is considered a health food in many countries after it was reported to be a source of antitumor and immunoactive compounds (Beier 1990; Mizuno et al. 1990). The common mushroom Agaricus bisporus contains benzyl alcohol as its most abundant volatile, and A. bisporus and Gyromitra esculenta both contain hydrazine analogues (Beier 1990). The water extract of A. blazei has potent antitumor activity in tumor-bearing mice (Beier 1990; Kawagishi et al. 1990; Mizuno et al. 1990; Itoh et al. 1994; Fujimiya et al. 1998; Lee et al. 2003), and the antitumor substance was postulated to be the beta-glucan fraction. Beta-glucans are polymers of glucose that are extractable from cereals, mushrooms, seaweed and yeasts (Beier 1990; Kawagishi et al. 1990; Mizuno et al. 1990; Itoh et al. 1994; Fujimiya et al. 1998; Lee et al. 2003). Orally administered beta-(1–6)-D-polyglucose extracted from A. blazei results in tumor regression in tumor-bearing mice (Oshima et al. 2002). The (1–3)-beta-backbone and the (1–6)-linked branches were thought to be important for their immune effects. Furthermore, a highly branched (1–3)-beta-glucan segment forms the active center of the antitumor activity (Ohno et al. 2001). Thus, beta-(1–6)-glucan with beta-(1–3)-branched chains has exhibited strong anticancer activity by increasing immune-competent cell activity (Kodama et al. 2002). Oral administration of botanical and yeast extracts containing (1–3), (1–6)-beta-glucans has shown anti-tumor effects in animal studies, and in patients with colorectal cancer (Torisu et al. 1990) and gastric cancer (Nakazato et al. 1994). Beta-(1–3)-D-glucan, such as schizophyllan has been used clinically in cancer therapy in Japan. A new approach is using the extracts of A. blazei or beta-glucan, preferably as an oral therapy, suitable for chronic administration and continual restraint of metastasis.
In the present study, daily oral administration of beta-glucan extracted from A. brazei was examined to determine whether it would inhibit production of experimental and spontaneous pulmonary metastasis by mouse Lewis lung carcinoma 3LL cells. Furthermore, we investigated the effect of treatment with this compound on peritoneal disseminated metastasis in an experimental nude mice model using intraperitoneal injections of human ovarian cancer HRA cells. The histology of this model closely resembles the characteristics of peritoneally disseminated metastasis from human ovarian cancer. To clarify the mechanism of antitumor activity by beta-glucan, we examined the effects of this compound on cell proliferation, apoptosis, signal transduction (phosphorylation of MAP kinase), and uPA expression were examined. In this study, we showed for the first time that beta-glucan has a direct effect on tumor invasion and metastasis possibly through a direct modulation of signaling cascades.
Materials and methods
Natural materials, chemicals and reagents
Agaricus blazei was supplied by DreamWorld Co., Ltd., Iwata, Japan. The acid-treatment preparation of the active fraction (fraction 3) was as described previously (Fujimiya et al. 1998; Oshima et al. 2002). This fraction had a molecular weight of approximately 10 kDa and consisted mainly of beta-1,6-D-glucan (Oshima et al. 2002). Endotoxin contamination of this preparation was less than 6 pg/ml as determined by a chromogenic endotoxin-specific assay, Endospecy (Seikagaku Kogyo, Tokyo). High molecular weight (HMW)-uPA, synthetic chromogenic substrate of uPA (Spectrozyme UK), Glu-type plasminogen, purified plasmin, and chromogenic plasmin substrate (Spectrozyme PL) were obtained from American Diagnostica (Greenwich, CT). RPMI 1640 medium, DMEM and FCS were obtained from Invitrogen Japan K.K. (Tokyo). TGF-β1 and mouse G-CSF were purchased from CosmoBio, Tokyo. Matrigel was purchased from Collaborative Research (Bedford, MA). Mouse anti-phospho-Thr202/Tyr204 ERK1/2, mouse anti-ERK antibodies were purchased from New England Biolabs Inc. (Beverly, MA). Rabbit anti-p38 kinase, rabbit anti-phospho-Tyr182 p38 kinase, rabbit anti-JNK2, rabbit anti-phospho-Thr183/Tyr185 JNK, anti-caspase-9, and anti-Bax antibodies were obtained from Santa Cruz Biotechnology (Santa Cruz, CA). Polyclonal antibody to cytochrome c was obtained from Pharmingen (San Diego, CA). PD98059, SB203580, and SP600125 were supplied by Calbiochem (La Jolla, CA). PD98059, SB203580, and SP600125 are MEK1/2-specific, p38 kinase-specific, and JNK-specific inhibitors, respectively. The inhibitors were dissolved in dimethyl sulfoxide and used in the following concentrations: PD98059 (10 μM, 30 min), SB203580 (15 μM, 30 min), and SP600125 (50 μM, 30 min). Unless otherwise specified, reagents for cell culture and all other chemicals including protease inhibitors were of the highest purity and obtained from Sigma.
Cells and culture
A murine Lewis lung carcinoma cell line, 3LL (Kobayashi et al. 1994), selected for its high lung colonization potential was kindly provided by Chugai Pharmaceuticals Co., Tokyo. The tumor was maintained by serial subcutaneous (s.c.) transplantation in C57BL/6 mice. In some experiments, 3LL cells were maintained as adherent monolayers cultured on tissue culture plastic in Eagle’s minimal essential medium supplemented with 10% fetal bovine serum, sodium pyruvate, nonessential amino acids, L-glutamine, and vitamins at 37°C in a humidified incubator with 5% CO2 in air. The human ovarian cancer HRA cells were maintained in RPMI 1640 medium supplemented with 10% fetal bovine serum in a cell culture incubator (constantly set at 37°C with 5% CO2) (Suzuki et al. 2003). Cells were stained with 0.2% trypan blue and viable cells were counted.
MTT assay
Cellular proliferation was measured by reduction of MTT, which corresponds to living cell number and metabolic activity (Mosmann 1983). Cells were thoroughly washed, plated at 5×104 cells/well in 24-well plates and incubated with or without test drugs for various periods of time. Fifty microliters of 1 mg/mls MTT solution (WST-8, Nacalai Tesque, Kyoto, Japan) was added to each well. After 1 h of incubation, the absorbance of each well was measured at 492 and 630 nm using a microplate reader (Bio-Rad Laboratories) according to the manufacturer’s protocol.
Thymidine incorporation assay
Cells (2×105 viable cells) were cultured in 1.5-ml polypropylene tubes containing 200 μl (final volume) of serum-free culture medium. After a 24-h preculture period, treated cells were incubated with 0.5 μCi/tube of [methyl−3H]thymidine. After another 24 h of culture, the cells were washed, centrifuged, and incubated with 10% ice-cold trichloroacetic acid. The cell pellet was solubilized in 0.2 M NaOH, and its radioactivity was measured (Otsuka et al. 2000).
Detection of cell surface-associated uPA activity by colorimetric assay
Cells were seeded at 10,000 cells/well in 96-well plates in the maintenance medium and allowed to reach ~90% confluence. The cells were washed once with phosphate-buffered saline and analyzed in a reaction buffer (100 μl/well) containing 0.8 mM MgCl2 and 0.2 μg/ml leupeptin. The reactions were initiated by the addition of the chromogenic amidolytic substrate specific for uPA (Spectrozyme UK) to a final concentration of 0.2 mM in the absence or presence of 1 mM amiloride or neutralizing antibodies to 10 μg/ml uPA (Nakazato et al. 1994). No amidolytic substrate was added in the blank reactions. The photometric absorbance of the reaction mixtures at 405 nm was monitored at 37°C over the next 30 min.
Hoechst 33258 staining
Hoechst 33258 staining was performed as described previously (Kim et al. 2001). Morphological changes in the nuclear chromatin of cells undergoing apoptosis were detected by staining with 2.5 μg/ml bisbenzimide Hoechst 33258 fluorochrome (Calbiochem), followed by examination on a fluorescence microscope. Apoptotic cells were identified by the condensation and fragmentation of their nuclei. The percentage of apoptotic cells was calculated from the ratio of apoptotic cells to total cells counted. At minimum, 500 cells were counted for each treatment.
Preparation of cytosolic and mitochondrial protein fractions
Cytosolic and mitochondrial protein fractions were prepared as described previously (Park et al. 2003). Cells were collected and washed twice in ice-cold PBS, resuspended in extraction buffer (20 mM HEPES, pH 7.5, 10 mM KCl, 1.9 mM MgCl2, 1 mM EGTA, 1 mM EDTA, mixture of protease inhibitors), and incubated on ice for 20 min. Then, the cells were homogenized with a glass homogenizer and a loose pestle. Cell homogenates were spun at 1,000 g to remove unbroken cells, nuclei, and heavy membranes. The supernatant was spun again at 14,000 g for 30 min to collect the mitochondria-rich (pellet) and cytosolic (supernatant) fractions. The mitochondria-rich fraction was washed once with the extraction buffer, followed by a final resuspension in lysis buffer (150 mM NaCl, 50 mM Tris–HCl, pH 7.4, 1% Nonidet P-40, 0.25% sodium deoxycholate, 1 mM EGTA) containing protease inhibitors for Western blot analysis. In parallel, cells treated in the same condition in different dishes were harvested and counted using a hemocytometer. Protein was measured by the Bradford assay (Bio-Rad) using bovine serum albumin as the standard.
Western blotting
Samples were electrophoresed under nonreducing conditions and transferred to polyvinylidene difluoride membrane using a semi-dry transfer system. Nonspecific binding sites were blocked for 1 h in Tris-buffered saline, pH 7.6, containing 2% bovine serum albumin. Blots were incubated with 0.1 μg/ml primary antibody for 1 h and with secondary antibody (goat anti-rabbit/mouse horseradish peroxidase-conjugated IgG diluted 1:5,000 in blocking solution) for 1 h. After several washes, reactive bands were visualized by a chemiluminescence detection kit (Amersham Biosciences, Tokyo).
Invasion assay
The ability of cells to migrate across a Matrigel barrier (invasion) was determined by the modified Boyden chamber method (Suzuki et al. 2003). Briefly, cells (105/chamber) were added to polyvinylpyrrolidone-free, 8-μm polycarbonate filters coated with 50 μl of 50 μg/ml Matrigel and incubated with complete medium containing 0.1% bovine serum albumin for 24 h at 37°C. NIH3T3 fibroblast-conditioned medium was used as a chemoattractant, and serum-free medium containing 0.1% bovine serum albumin was used as a negative control. Filters were removed from the chambers and stained with hematoxylin. Cells were counted at a 100× magnification, and the mean numbers of cells/field in five random fields were recorded. Duplicate filters were used, and the experiments were repeated three times. In a parallel experiment, standard chemotaxis assays were performed in the absence of Matrigel.
Animals
All protocols for animal studies were reviewed and approved by the Animal Research and Ethics Board of Hamamatsu University. The care and use of the animals were in accordance with the Institution’s guidelines. Specific-pathogen-free female C57BL/6 mice and female inbred nude (BALB/cnu/nu) mice, 5 weeks old (16–19 g), were purchased from SLC (Hamamatsu, Japan). The animals were maintained under the following standard conditions: 22±2°C, 45±10% relative humidity, and 12-h light/12-h dark cycles each day. Control mice were also fed water alone on the same schedule. Powdered CE-2 (CLEA Japan, Inc., Tokyo) was used as a basal diet. Both the diets and water were offered ad libitum. They were randomized into groups, so that mean body weights in the group were approximately equal and were initially housed up to nine mice in a group.
Experimental and spontaneous lung metastasis in C57BL/6 mice
C57BL/6, 5-week-old female mice, were housed in the Hamamatsu University Animal Care Facility for 1 week prior to use. Per experiment, control animals not injected with tumor cells were included.
Experimental metastasis [which may determine only the later steps of the metastatic migration process (extravasation from the blood stream and then growth into pulmonary tumor)]: 3LL cells (2.5×105 cells/50 μl/mouse) were slowly injected via the lateral tail vein of unanesthetized C57BL/6 mice (Kobayashi et al. 1994, 1995). The mice were killed 21 days after tumor inoculation. The lungs were fixed in Bouin’s solution and the lung tumor colonies were counted under a dissecting microscope.
Spontaneous metastasis (which measures metastasis from a primary tumor): 3LL cells (1×106 cells/50 μl/mouse) were injected s.c. in the mouse abdominal wall. The mice were sacrificed 28 days after tumor inoculation (Kobayashi et al. 1994, 1995). The number of lung tumor colonies was determined as already described.
During the experimental period, animals of each group (n=10 for each group) were treated with aqueous solutions of the beta-glucan, with a dry weight of 20, 100, and 500 μg/ml, respectively. The solutions were offered to animals ad libitum, in aluminum foil-wrapped bottles to avoid light decomposition. They were the sole source of drinking fluid.
Peritoneally disseminated metastasis model in nude mice
HRA cells were injected intraperitoneally according to Suzuki et al. (2003). The cells (0.1 ml of cell suspension containing 5×106 cells) were injected intraperitoneally using a 26-gauge needle. Nine days after injection of the cells, the animals were sacrificed, and intraperitoneal tumor nodules were also dissected, weighted, fixed in formalin, and embedded in paraffin.
During the experimental period, animals of each group (n=10) were treated with solutions of the beta-glucan (0, 20, 100, or 500 μg/ml). The solutions were offered to animals ad libitum as described above. In a separate experiment, the indicated doses of beta-glucan were administered i.p. (20, 100, or 500 μg/0.1 ml PBS, bolus injection) on days 0, 1, 2, 3, 5, and 7. Control mice were given PBS instead of the test solution.
Tumor volume
The tumor volume was determined through direct measurement with calipers and calculated by the formula [length (mm) × width (mm2)]/2 every 2–3 days. On day 21, blood was obtained via venipuncture in mice with diethyl ether anesthesia, and then the tumor, epididymal adipose tissue, spleen and thymus were removed and weighed for evaluation of antitumor activity and side effects. The blood samples were chilled in test-tubes containing heparin, and the number of leukocytes was measured using a Coulter Counter (Japan Scientific Instruments Ltd., Tokyo, Japan).
Statistical analysis
All experiments were performed using at least three different cell preparations. Data are presented as mean ± standard deviation (SD). All statistical analyses were performed using StatView for Macintosh. Data were analyzed by one-way ANOVA, and then differences in means among groups were analyzed using Dunnett’s test (significantly different at P<0.05).
Results
Beta-glucan extracted from A. Blazei directly suppresses HRA cell proliferation in vitro
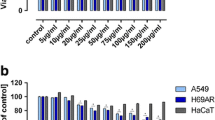
We initially examined whether beta-glucan extracted from A. blazei reduces cell proliferation in cancer cells using a thymidine incorporation assay. It has been reported that beta-glucan is one of the major components extracted from fungi and mushroom such as A. blazei. Therefore, HRA cells were treated with beta-glucan. The beta-glucan inhibited thymidine incorporation in a dose-dependent fashion at concentrations up to 10 μg/ml of beta-glucan in HRA cells (Fig. 1a, left panel). This suggests strongly that beta-glucan suppresses cell proliferation in ovarian cancer cells.
Cancer cell proliferation in response to beta-glucan extracted from A. blazei. HRA and 3LL cells were deprived of serum for 24 h and incubated with the control, serum-free medium or beta-glucan (0.4, 2, or 10 μg/ml) for 20 h. a [3H]thymidine incorporation was measured during the last 5 h. b Cell viability was measured by the enzymatic reduction of MTT (OD 550–670 nm) during the last 3 h. Values represent the mean ± SD of quadruplicate samples of a representative experiment. *P<0.05 vs. control
In a parallel experiment, we performed the MTT assay, a colorimetric cell growth assay that measures the reduction of MTT by mitochondrial succinate dehydrogenase and, thus, detects living cells. Consistent with thymidine incorporation, 10 μg/ml beta-glucan decreased living cells (Fig. 1b, left panel). This confirms that beta-glucan-inhibited thymidine incorporation correlates with beta-glucan-suppressed cell proliferation in ovarian cancer cells.
Beta-glucan does not suppress 3LL cell proliferation in vitro
We examined whether beta-glucan reduces cell proliferation in another cell type (Lewis lung cancer 3LL cells) using a thymidine incorporation assay and MTT assay. In contrast to HRA cells, both assays revealed that beta-glucan failed to inhibit 3LL cell proliferation even at concentrations of up to 10 μg/ml of beta-glucan (Fig. 1a, b, right panel).
Effects of beta-glucan on the peritoneally by disseminated metastasis in human ovarian cancer cells
We hypothesize that beta-glucan may inhibit ovarian cancer progression in vivo. By using an experimental model of peritoneally by disseminated metastasis caused by HRA ovarian cancer cells that quite closely mimics the conditions likely to occur in naturally arising metastatic human ovarian cancers, we first examined the suppressing effects of i.p. injection of beta-glucan on peritoneally by disseminated metastasis of HRA cells. In an initial experiment, the mice without tumor inoculation in each group did not show any significant difference in body weight (data not shown). Bolus i.p. injection of beta-glucan (100 and 500 μg/mouse) did significantly reduce tumor burden (Fig. 2a). In the control group, the total tumor weight/animal amounted to 3.38±0.92 g, whereas the total tumor burden in the beta-glucan (500 μg/mouse) group was only 2.50±0.31 g, a reduction of 25% (P<0.05). The i.p. tumor growth was also significantly decreased in mice given beta-glucan (100 μg/mouse) (P<0.05). Thus, beta-glucan was effective at inhibiting in vitro ovarian cancer cell proliferation and in vivo disseminated metastasis.
Effects of beta-glucan on peritoneal disseminated metastasis. HRA cells (5×106) were injected intraperitoneally. a Beta-glucan (0, 20, 100, or 500 μg/mouse) was injected intraperitoneally on days 0, 1, 2, 3, 5, and 7. b Mice received oral beta-glucan by drinking fluid (0, 20, 100, or 500 μg/ml) every day during the experimental period. Nine days after injection of the cells, the animals were sacrificed, intraperitoneal tumor masses were dissected and weighted. Results are the mean ± SD of three different determinations. *P<0.05 vs. control
We secondarily examined the suppressing effects of daily oral supplementation of beta-glucan on peritoneal by disseminated metastasis of HRA cells. In the control group, the total tumor weight/animal amounted to 3.90±0.52 g, whereas the total tumor burden in the beta-glucan (500 μg/ml) group was 3.01±0.21 g, a reduction of 22%. Thus, the extent of intraperitoneal tumor burden in HRA-bearing animals was significantly decreased in animals treated with daily oral administration of beta-glucan (500 μg/ml) (Fig. 2b). The beta-glucan treatment had no influence on the mean body weight gain or on food consumption at the end of the experimental period (data not shown).
Beta-glucan does not inhibit the growth of subcutaneous 3LL tumor
To determine whether beta-glucan has a direct growth-inhibitory effect on 3LL lung cancer cells in vivo, 3LL cells were implanted subcutaneously into C57BL/6 mice. Unfortunately, daily oral administration of beta-glucan did not suppress primary tumor growth (Fig. 3). This lack of effect of beta-glucan on primary tumor growth in vivo could not be due to a shortfall of daily supplementation of drinking fluid, because beta-glucan-treated animals had significantly repressed lung metastasis when compared with that observed in untreated animals (see below).
Beta-glucan did not inhibit the growth of subcutaneous 3LL tumor. 3LL cells were inoculated subcutaneously into the flank of mice. The tumor volume from animals treated (black squares) or not treated (white squares) with oral beta-glucan was assessed by bilateral Vernier caliper measurement. Values are the mean ± SD of six animals per group and are expressed in mm3
Beta-glucan inhibits the formation of lung metastases caused by lung cancer cells in vivo
We have shown previously that mouse lung cancer 3LL cells have the unique property of metastasizing to the lung after intravenous or subcutaneous tumor cell inoculation in C57BL/6 mice. To determine whether beta-glucan has anti-metastatic effect on 3LL lung cancer cells in vivo, 3LL cells were implanted subcutaneously into C57BL/6 mice. As shown in Fig. 4a, the incidence of 3LL lung metastasis (the mean numbers of metastatic lung tumors) in mice that received oral beta-glucan (100 or 500 μg/ml) was significantly less than that in control mice. The extent of this inhibition depends on the concentrations of beta-glucan in the drinking fluid. These results suggest that the production of spontaneous lung metastasis was inhibited predominantly by beta-glucan.
Effect of beta-glucan on the formation of lung metastases caused by 3LL cells. a The number of lung tumor colonies from mice bearing 3LL cells 28 days after s.c. tumor cell inoculation. b The number of lung tumor colonies from mice bearing 3LL cells 21 days after i.v. tumor cell inoculation. Mice were treated with daily oral administration of beta-glucan (0, 20, 100, or 500 μg/ml) during these experiments. Values are mean ± SD of five to seven animals. *P<0.05 vs. control
Effects of beta-glucan on the experimental metastasis in mouse Lewis lung cancer cells
In a parallel experiment, we examined the suppressing effects of oral supplementation of beta-glucan on experimental lung metastasis after systemic i.v. injection of 3LL cells. The results of a representative experiment are shown in Fig. 4b. The daily oral supplementation of beta-glucan even at a dose of 500 μg/ml for 21 days did not significantly reduce the number of lung tumor colonies in the experimental metastasis model, although the average number of the formation of pulmonary nodules was lower in mice treated with beta-glucan (P>0.05).
Beta-glucan promotes p38 MAPK activation in HRA ovarian cancer cells
These data allow us to speculate that beta-glucan is potent to modulate the cell proliferation- or metastasis-related intracellular signaling pathways in certain types of cancer cells. We analyzed the activation of different MAPKs in HRA cells using phospho-specific antibodies in cancer cells after being treated with beta-glucan for various periods up to 60 min (Fig. 5). Added beta-glucan (10 μg/ml) significantly induced p38 activation in HRA cells, peaking 15 min and returning to the basal level 60 min after (Fig. 5c). Beta-glucan promoted p38 activity in HRA cells in a dose-dependent manner (Fig. 5d, lanes 2–4). In contrast, ERK1/2 (Fig. 5a) and JNK (Fig. 5b) pathways were unaffected by beta-glucan. Therefore, promoting p38 activation may correlate to inhibition of ovarian cancer cell proliferation in response to beta-glucan. In contrast, beta-glucan does not promote MAPK signalings including p38, JNK, and ERK phosphorylation in 3LL cells (data not shown). We further showed that SB203580, a p38 inhibitor, suppressed the beta-glucan-induced p38 phosphorylation (Fig. 5d, lane 5).
Beta-glucan specifically promotes p38 MAPK activation in HRA cells. Cells were deprived of serum for 24 h and incubated in the serum-free medium containing 10 μg/ml beta-glucan for indicated periods. Phosphorylation of the specific proteins was detected by Western blot analysis using antibodies to total- or phosphorylated-ERK1/2 (a), JNK (b), or p38 MAPK (c). d HRA ovarian cancer cells were deprived of serum for 24 h and pretreated with or without SB203580, a p38 inhibitor, for 30 min. Then cells were treated with 0, 0.4, 2, and 10 μg/ml beta-glucan for 15 min. Phosphorylation of p38 was assessed by Western blot analysis with anti-phospho-p38 antibodies. To normalize p38 phosphorylation levels to total amounts of p38 protein, membranes were then stripped and re-probed with the antibody that recognizes both phosphorylated and non-phosphorylated form of p38. The data represent a typical experiment conducted three times with similar results
To determine whether promotion of p38 activation mediates beta-glucan-induced suppression of cell proliferation, we analyzed the effects of pharmacological p38 inhibition on thymidine incorporation in HRA cells. As shown in Fig. 6, SB 203580 abrogates beta-glucan-mediated inhibition of cell proliferation at the same range of concentrations in this cell line. These indicate that beta-glucan suppresses cell proliferation in HRA cells through activation of p38 pathway.
Promotion of p38 activation is required for beta-glucan-mediated suppression of ovarian cancer cell proliferation. After a 24-h serum deprivation, cells were pretreated with beta-glucan or beta-glucan plus SB203580 at indicated concentrations for 20 h. Cell proliferation was measured by [3H]thymidine incorporation during the last 5 h. Values represent the mean ± SD of quadruplicate samples of a representative experiment. Unlike letters (a, b, and c) stand for statistical differences (P<0.05)
Beta-glucan induces apoptosis
We hypothesize that beta-glucan-induced suppression of cell proliferation through activation of p38 MAPK is related to beta-glucan-mediated apoptosis. We examined whether beta-glucan induces apoptosis in HRA cells. For confirmation, we treated these cells with different doses of beta-glucan, and analyzed the induction of apoptotic cell death. Figure 7 shows that there is a dose- and time-dependent increase of apoptotic cells after the beta-glucan treatment, as measured by Hoechst 33258 staining for nuclei fragmentation and condensation.
Beta-glucan induces apoptosis through p38 MAPK cascade. HRA cells pretreated with or without pharmacological inhibitors, PD98059 (10 μM), SP600125 (50 μM), and SB203580 (15 μM), were treated with beta-glucan (10 μg/ml) for the time periods indicated (3 and 12 h). Cells were stained with Hoechst 33258, and apoptotic cells were analyzed by fluorescence microscopy. Apoptotic cells containing condensed chromatin fragments were scored and expressed as a percentage of the total cell number measured. Results from three independent experiments are shown as means (bars, ±SD). Unlike letters (a, b, and c; a′, b′, c′, and d′) stand for statistical differences (P<0.05)
We next examined whether beta-glucan-induced apoptosis is specifically inhibited by SB203580. HRA cells pretreated with each pharmacological inhibitor were stimulated with beta-glucan (10 μg/ml). At a concentration of 15 μM, SB203580 abrogated beta-glucan-induced apoptosis by 90%. On the other hand, neither the JNK inhibitor SP 600125 nor the inhibitor of MEK1 PD98059 abrogated the apoptotic effect of beta-glucan, even at high concentrations.
Beta-glucan induces Bax translocation, cytochrome c release, and caspase-9 activation in HRA cells
As shown in Fig. 8, beta-glucan treatment redistributes Bax from the cytosol to mitochondrial fraction. Cytochrome c was detected in the cytosolic fraction. Caspase-9 proform was also degraded in response to beta-glucan. These results suggest that Bax translocation, cytochrome c release, and caspase-9 activation occur during the apoptotic process triggered by beta-glucan. SB203580 significantly abrogated beta-glucan-induced redistribution of Bax, cytochrome c release and degradation of caspase-9 proform protein. We thus confirmed that SB203580 abrogated beta-glucan-induced apoptotic process in HRA cells.
Beta-glucan induces Bax translocation, cytochrome c release, and caspase-9 activation in HRA cells. HRA cells were treated with 10 μg/ml beta-glucan for 3 h. Cell lysates were prepared, and Western blot analysis was performed for caspase-9 and β-actin. Cytosolic fraction was prepared, and cytochrome c was detected by Western blot analysis using anti-cytochrome c antibody. Mitochondrial fraction was analyzed for Bax protein expression using anti-Bax antibody. The data represent a typical experiment conducted three times with similar results
Effects of beta-glucan on uPA expression and cell invasion in vitro
In our previous experiments, we confirmed the role of uPA in cancer cell invasion (Suzuki et al. 2003), demonstrating that the regulation of invasion seen in the HRA and 3LL cells is mainly mediated by the uPA-plasmin system. It has been reported previously that granulocyte colony-stimulating factor (G-CSF) can stimulate uPA expression and promote the invasion of 3LL lung cancer cell lines in vitro (Pei et al. 1998). Furthermore, TGF-β1 stimulates uPA expression and invasion in HRA cells. In this study, we showed that TGF-β1 (10 ng/ml) significantly stimulates uPA upregulation in HRA cells and that treatment of cells with beta-glucan specifically induced a suppression of TGF-β1-stimulated up-regulation of uPA in a dose-dependent manner (Fig. 9a, lanes 3–5).
Effects of beta-glucan on uPA expression and cell invasion in vitro. a HRA cells pretreated with or without beta-glucan were stimulated with 10 ng/ml TGF-β1. Total proteins were obtained and subjected to electrophoresis. Gels were transferred to PVDF membrane and probed with antibodies to uPA and β-actin, respectively. b The monolayer of HRA cells seeded in 96-well plate was pretreated with beta-glucan (2 or 10 μg/ml) in the presence of 10 ng/ml TGF-β1 for 12 h. The monolayers were washed twice with PBS and analyzed by colorimetric assay in the presence of the Spectrozyme UK. Results represent mean ± SD of three experiments and triplicate determination. *P<0.05 compared with lane 3. c A cell suspension, 200 μl (500,000 cells/ml) in medium, was placed at the upper compartment. After a 24-h incubation, cells that invaded through the Matrigel-coated membrane were stained and counted under the microscope. All experiments were performed three times, and typical data are shown. Results represent mean ± SD of three experiments and triplicate determination. *P<0.05 compared with lane 3
To determine whether the cell-associated receptor-bound uPA is affected by beta-glucan, the monolayer of HRA cells was pretreated with these compounds for 24 h and analyzed by colorimetric assay in the presence of the Spectrozyme UK. The beta-glucan specifically suppresses cell-associated uPA activity in cells treated with TGF-β1 (Fig. 9b, lane 5). Therefore, tumor cell invasion and metastasis would be suppressed after the receptor-bound uPA expression was inhibited by this compound. The colorimetric assay confirmed that beta-glucan at the concentrations used in this study do not directly inhibit uPA catalytic activity (data not shown). In a parallel experiment, we confirmed that in 3LL cells beta-glucan also suppressed G-CSF-stimulated uPA expression in vitro (data not shown).
The beta-glucan showed a dose-dependent and statistically significant inhibition of invasion in vitro (Fig. 9c, lane 5). In addition, we examined the effects of these compounds on cell attachment. Under optimal conditions, 80% of these cells remain attached to the Matrigel after washing. No inhibition of attachment to Matrigel was seen with beta-glucan (data not shown). These data speculate that beta-glucan extracted from A. blazei may inhibit tumor invasion and metastasis at least through suppression of uPA expression.
Discussion
Intense efforts have been made in several laboratories to understand the role of A. blazei of the anticancer process. Beta-glucan potentiates the cytolytic activity of macrophages against tumor cells in vitro. The mechanism of action of beta-glucan involves macrophage stimulation and subsequent release of inflammatory mediators such as IL-1 and TNF-α (Sveinbjornsson and Rushfeld 1998). It has been established that the antitumor activities were observed not only in water extract (beta-glucan) but also in lipid fraction (ergosterol). In contrast to beta-glucan, ergosterol had no cytotoxic effect against sarcoma 180 cells in vitro. Ergosterol may be involved in the inhibition of tumor-induced neovascularization (Takaku et al. 2001). However, little is known about the effects of A. blazei on cancer cell invasion and metastasis. In this study, we showed for the first time that beta-glucan has a direct effect on tumor invasion and metastasis.
The results of the current in vivo study provide the first evidence that oral supplementation suppressed spontaneous metastasis of 3LL lung cancer cells in mice, as revealed by the low incidence of metastases in the lungs, the small number and low tumor weights of metastatic lesions in mice which received oral beta-glucan, an isolated product from A. blazei compared with those in control mice. In contrast, oral supplementation did not reduce primary tumor growth when 3LL cells were inoculated subcutaneously in mice. This lack of effect of beta-glucan on tumor growth in vivo could not be due to a defect of daily supplementation of beta-glucan, because beta-glucan-treated animals had significantly repressed lung metastasis when compared with that observed in untreated animals. Furthermore, oral administration of beta-glucan reduced peritoneally disseminated metastasis in a mouse model using human ovarian cancer HRA cells. Interestingly, treatment of mice with beta-glucan does not reduce the number of experimental lung metastasis, after tumor cells entered into the intravascular space. The in vivo experimental metastasis model may test merely the later stages of the metastatic process because the tumor cells are injected directly in the circulation. One possibility is that beta-glucan may inhibit the process involved in entry of tumor cells into circulation (intravasation) and peritoneal tumor spread. These experiments, however, do not eliminate roles for uPA in the initial steps of the metastatic process (Ossowski and Reich 1983; Ostrowski et al. 1986). It may be that other factors are rate determining in the extravasation followed by lung colonization process rather than the uPA expression and activity. It is of interest to further investigate the effects of beta-glucan on an early step of metastasis. It must be kept in mind that beta-glucan inhibited lung metastasis formation as well as peritoneal disseminated metastasis in vivo. Beta-glucan modified the metastatic capabilities rather than in vivo tumor growth, indicating that beta-glucan in vivo was acting on metastatic cells.
Our in vitro results allow us to conclude that beta-glucan-mediated inhibition of tumor cell proliferation, invasion and metastasis appear to consist of at least two pathways, a direct pathway through the activation of p38 MAPK, which results in suppression of cell proliferation and induction of apoptosis and an alternate pathway through the suppression of uPA expression, both of which play a cooperative and pivotal role in the inhibition of tumor cell invasion and metastasis.
Some papers report the relationship between activation of p38 MAPK and inhibition of cell growth and the promotion of apoptosis: for example, genistein-induced activation of p38 MAPK resulted in growth arrest of tumor cells in the G2 phase of the cell cycle, a large induction of phosphorylation of Cdc2 (along with decreased activity of Cdc2), increased expression of p21(waf/cip1) and decreased expression of the cell cycle phosphatase Cdc25C (Frey and Singletary 2003). Activation of p38 precedes the activation of caspase 3. SB203580, a specific kinase inhibitor for p38 which can block the activation of caspase 3 and inhibit the resultant apoptosis (Liu et al. 2004). Therefore, beta-glucan-induced activation of p38 MAPK may also be related to cell proliferation and apoptosis.
In addition, the beta-glucan-dependent promotion of phosphorylation of p38 MAPK and repression of uPA expression could be one of the mechanisms of antimetastatic action. It has been reported that suppression of p38 MAPK activation reversed the growth factor-dependent inhibition of uPA activity (Bein et al. 2004). The proliferative balance of high ERK/p38 ratio was induced by high uPA receptor (uPAR) expression. Thus, high ERK/p38 ratio favors tumor growth, whereas high p38/ERK ratio induces tumor growth arrest (dormancy) in vivo and this ERK is negatively regulated by p38. (Aguirre-Ghiso et al. 2003). These data support the present results. In contrast, some evidence has accumulated that p38 MAPK signaling pathway is important for uPA expression in certain types of cancer cells by enhancing the promoter activity of uPA and uPA mRNA stability (Chen et al. 2001; Han et al. 2002; Shin et al. 2003). Therefore, the relationship between p38 MAPK activation and uPA regulation is controversial, possibly due to differences in cell types and species specificity.
This report extends previous studies demonstrating that Ganoderma lucidum (Reishi), another member of mushroom, suppresses tumor invasion and metastatic potential (Jiang et al. 2004). Similar to A. blazei, Reishi is an oriental medical mushroom. It has been previously demonstrated that Reishi down-regulates the expression of uPA and its receptor (uPAR), which results in suppression of cell migration of highly invasive human breast and prostate cancer cells (Sliva et al. 2002). Reishi inhibits cell proliferation by the down-regulation of expression of cell cycle-specific proteins. The inhibition of cell growth was also demonstrated by cell cycle arrest at G2/M phase. Furthermore, Reishi induced apoptosis of PC-3 cells (Jiang et al. 2004). Humans consume some active components from fungus and mushroom in their daily lives. Thus, A. brazei and Ganoderma lucidum exert their effects on cancer cells by multiple mechanisms and may have potential therapeutic use for the prevention and treatment of cancer (Jiang et al. 2004).
Oral administration of beta-glucan had no effect on food intakes and body weight gain in 3LL- or HRA-bearing mice (data not shown). Our findings suggest that the antimetastatic effect of beta-glucan was demonstrated in the absence of side effects such as weight loss, which might indirectly affect metastasis. Thus, we would expect that the property of water extract from A. blazei contributes to the antimetastatic activity found in the present study. A. blazei exerts its effect on cancer cells by multiple mechanisms. Therefore, concentrated beta-glucan would be the more likely candidate for use in future clinical trials.
Previously, we showed the antitumor effect of paclitaxel in this model. The weight of peritoneal tumors was significantly reduced from a mean weight of 3.18±0.33 g in PBS-treated mice to 0.53±0.05 g in mice treated with 5 μg of paclitaxel (Kobayashi et al. 2004), indicating that the inhibition ratio by paclitaxel treatment is around 80%. Inhibition ratio by i.p. treatment with A. blazei is around 25% and this is not so intensive. This effect seems to be moderate. In order to raise the intensity of the antitumor effects of beta-glucan, animals were i.p. injected with 5 mg of beta-glucan. The maximum effect was obtained using 500 μg of β-glucan and this amount was used in subsequent experiments (data not shown).
In conclusion, our current in vivo experimental and spontaneous metastasis assays for the first time suggest the role for A. blazei-derived beta-glucan in the initial steps of the metastatic process or intravasation step in lung cancer. In addition, beta-glucan reduced tumor burden associated with peritoneally disseminated metastasis from ovarian cancer. Beta-glucan suppresses cell proliferation, induces apoptosis and inhibits uPA expression, possibly through promotion of p38 MAPK activation. Treatment might still be very beneficial for ovarian cancer or lung cancer patients with or at risk for metastasis.
Abbreviations
- 3LL:
-
Murine Lewis lung carcinoma
- MAPK:
-
Mitogen-activated protein kinase
- uPA:
-
Urokinase-type plasminogen activator
- FCS:
-
Fetal calf serum
- ERK:
-
Extracellular signal-regulated kinase
- JNK:
-
c-Jun N-terminal kinase
- TGF-β:
-
Transforming growth factor-beta
References
Aguirre-Ghiso JA, Estrada Y, Liu D, Ossowski L (2003) ERK(MAPK) activity as a determinant of tumor growth and dormancy; regulation by p38(SAPK). Cancer Res 63:1684–1695
Beier RC (1990) Natural pesticides and bioactive components in foods. Rev Environ Contam Toxicol 113:47–137
Bein K, Odell-Fiddler ET, Drinane M (2004) Role of TGF-beta1 and JNK signaling in capillary tube patterning. Am J Physiol Cell Physiol 287:C1012–C1022
Chen J, Baskerville C, Han Q, Pan ZK, Huang S (2001) Alpha(v) integrin, p38 mitogen-activated protein kinase, and urokinase plasminogen activator are functionally linked in invasive breast cancer cells. J Biol Chem 276:47901–47905
Frey RS, Singletary KW (2003) Genistein activates p38 mitogen-activated protein kinase, inactivates ERK1/ERK2 and decreases Cdc25C expression in immortalized human mammary epithelial cells. J Nutr 133:226–231
Fujimiya Y, Suzuki T, Oshiman K, Kobori H, Moriguchi K, Nakashima H, Matumoto Y, Takahara S, Ebina T, Katakura R (1998) Selective tumoricidal effect of soluble proteoglucan extracted from the Basidiomycete, Agaricus blazei Murill, mediated via natural killer cell activation and apotosis. Cancer Immunol Immunother 46:147–159
Han Q, Leng J, Bian D, Mahanivong C, Carpenter KA, Pan ZK, Han J, Huang S (2002) Rac1-MKK3-p38-MAPKAPK2 pathway promotes urokinase plasminogen activator mRNA stability in invasive breast cancer cells. J Biol Chem 277:48379–48385
Itoh H, Ito H, Amano H, Noda H (1994) Inhibitory action of (1–6)-ß-glucan-protein complex (FIII 020b) isolated from Agaricus blazei Murill (“Himematsutake”) on Meth A fibrosarcoma-bearing mice and its antitumor mechanism. Jpn J Pharmacol 66:265–271
Jiang J, Slivova V, Valachovicova T, Harvey K, Sliva D (2004) Ganoderma lucidum inhibits proliferation and induces apoptosis in human prostate cancer cells PC-3. Int J Oncol 24:1093–1099
Kawagishi H, Kanao T, Inagaki R, Mituno T, Shimura K, Itoh H, Hagiwara T, Nakamura T (1990) Formolysis of a potent antitumor (1–6)-ß-glucan-protein complex from Agaricus blazei fruiting bodies and antitumor activity of the resulting products. Carbohydr Polym 12:393–403
Kim MR, Lee JY, Park MT, Chun YJ, Jang YJ, Kang CM, Kim HS, Cho CK, Lee YS, Jeong HY, Lee SJ (2001) Ionizing radiation can overcome resistance to TRAIL in TRAIL-resistant cancer cells. FEBS Lett 505(1):179–184
Kobayashi H, Gotoh J, Shinohara H, Moniwa N, Terao T (1994) Inhibition of the metastasis of Lewis lung carcinoma by antibody against urokinase-type plasminogen activator in the experimental and spontaneous metastasis model. Thromb Haemost 71:474–480
Kobayashi H, Shinohara H, Fujie M, Gotoh J, Itoh M, Takeuchi K, Terao T (1995) Inhibition of metastasis of Lewis lung carcinoma by urinary trypsin inhibitor in experimental and spontaneous metastasis models. Int J Cancer 63:4554–4562
Kobayashi H, Yagyu T, Inagaki K, Kondo T, Suzuki M, Kanayama N, Terao T (2004) Bikunin plus paclitaxel markedly reduces tumor burden and ascites in mouse model of ovarian cancer. Int J Cancer 110:134–139
Kodama N, Komuta K, Nanba H (2002) Can maitake MD-fraction aid cancer patients? Altern Med Rev 7:236–239
Lee YL, Kim HJ, Lee MS, Kim JM, Han JS, Hong EK, Kwon MS, Lee MJ (2003) Oral administration of Agaricus blazei (H1 strain) inhibited tumor growth in a sarcoma 180 inoculation model. Exp Anim 52:371–375
Liu Q, Chen T, Chen H, Zhang M, Li N, Lu Z, Ma P, Cao X (2004) Triptolide (PG-490) induces apoptosis of dendritic cells through sequential p38 MAP kinase phosphorylation and caspase 3 activation. Biochem Biophys Res Commun 319:980–986
Mizuno T, Inagaki R, Kanno T, Hagiwara T, Nakamura T, Itoh T, Shimura K, Sumiya T, Asakura A (1990) Antitumor activity and some properties of water-soluble polysaccharides from “Himematsutake”, the fruiting body of Agaricus blazei Murill. Agric Biol Chem 54:2889–2896
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65(1–2):55–63
Nakazato H, Koike A, Saji S, Ogawa N, Sakamoto J (1994) Efficacy of immunochemotherapy as adjuvant treatment after curative resection of gastric cancer. Study group of immunochemotherapy with PSK for gastric cancer. Lancet 343(8906):1122–1126
Ohno N, Furukawa M, Miura NN, Adachi Y, Motoi M, Yadomae T (2001) Antitumor beta glucan from the cultured fruit body of Agaricus blazei. Biol Pharm Bull 24:820–828
Oshiman K, Fujimiya Y, Ebina T, Suzuki I, Noji M (2002) Orally administered beta-1,6-D-polyglucose extracted from Agaricus blazei results in tumor regression in tumor-bearing mice. Planta Med 68:610–614
Ossowski L, Reich E (1983) Antibodies to plasminogen activator inhibit human tumor metastasis. Cell 35:611–619
Ostrowski LE, Ahsan A, Suthar BP, Pagast P, Bain DL, Wong C, Patel A, Schultz RM (1986) Selective inhibition of proteolytic enzymes in an in vivo mouse model for experimental metastasis. Cancer Res 46:4121–4128
Otsuka F, Yao Z, Lee TH, Yamamoto S, Erickson GF, Shimasaki S (2000) Bone morphogenetic protein-15. Identification of target cells and biological functions. J Biol Chem 275:39523–39528
Park MT, Choi JA, Kim MJ, Um HD, Bae S, Kang CM, Cho CK, Kang S, Chung HY, Lee YS, Lee SJ (2003) Suppression of extracellular signal-related kinase and activation of p38 MAPK are two critical events leading to caspase-8- and mitochondria-mediated cell death in phytosphingosine-treated human cancer cells. J Biol Chem 278:50624–50634
Pei XH, Nakanishi Y, Takayama K, Bai F, Kawasaki M, Hara N (1998) G-CSF increases secretion of urokinase-type plasminogen activator by human lung cancer cells. Clin Exp Metastasis 16:551–558
Shin BA, Yoo HG, Kim HS, Kim MH, Hwang YS, Chay KO, Lee KY, Ahn BW, Jung YD (2003) P38 MAPK pathway is involved in the urokinase plasminogen activator expression in human gastric SNU-638 cells. Oncol Rep 10:1467–1471
Sliva D, Labarrere C, Slivova V, Sedlak M, Lloyd FP Jr, Ho NW (2002) Ganoderma lucidum suppresses motility of highly invasive breast and prostate cancer cells. Biochem Biophys Res Commun 298:603–612
Suzuki M, Kobayashi H, Tanaka Y, Hirashima Y, Kanayama N, Takei Y, Saga Y, Suzuki M, Itoh H, Terao T (2003) Suppression of invasion and peritoneal carcinomatosis of ovarian cancer cell line by overexpression of bikunin. Int J Cancer 104:289–302
Sveinbjornsson B, Rushfeldt C (1998) Inhibition of establishment and growth of mouse liver metastasis after treatment with interferon gamma and beta-1,3-D-glucan. Hepatol 27:1241–1248
Takaku T, Kimura Y, Okuda H (2001) Isolation of an antitumor compound from Agaricus blazei Murill and its mechanism of action. J Nutr 131:1409–1413
Torisu M, Hayashi Y, Ishimitsu T, Fujimura T, Iwasaki K, Katano M, Yamamoto H, Kimura Y, Takesue M, Kondo M (1990) Significant prolongation of disease-free period gained by oral polysaccharide K (PSK) administration after curative surgical operation of colorectal cancer. Cancer Immunol Immunother 31:261–268
Acknowledgements
Agaricus blazei was obtained from K. Naito (DreamWorld Co., Ltd.). This work was supported by a grant-in-aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (to H.K.), by grants from the Fuji Foundation for Protein Research (H.K.), the Kanzawa Medical Foundation (H.K.), Sagawa Cancer Research foundation (H.K.), and Aichi Cancer Research foundation (H.K).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kobayashi, H., Yoshida, R., Kanada, Y. et al. Suppressing effects of daily oral supplementation of beta-glucan extracted from Agaricus blazei Murill on spontaneous and peritoneal disseminated metastasis in mouse model. J Cancer Res Clin Oncol 131, 527–538 (2005). https://doi.org/10.1007/s00432-005-0672-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-005-0672-1