Abstract
The therapeutic value of doxorubicin as an effective antineoplastic agent is limited by its cardiotoxic side-effects. The administration of doxorubicin (10 mg/kg) to male Wistar rats induced necrosis and apoptosis in heart tissues. It also caused oxidative stress damage as evidenced by the elevation of malondialdehyde and protein carbonyl levels and catalase activity, accompanied by the concurrent depletion of total antioxidant capacity and of superoxide dismutase level in cardiac tissues. The doxorubicin-induced cardiotoxicity and oxidative stress damage were also accompanied by increases of myeloperoxidase activity, total calcium content, and the expression of Bcl-2 protein in heart tissues. Most of these doxorubicin-induced biochemical and histological alterations were effectively attenuated by prior administration of purified standardized extract (1.5% withanolides; manufactured by Idea Sphere Inc., American Fork, UT, USA) of Withania somnifera (300 mg/kg). Thus, Withania may play a role in the protection against cardiotoxicity and thus might be a useful adjuvant therapy where doxorubicin is the cancer-treating drug.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Doxorubicin (DXR), an anthracycline antibiotic, is a commonly used antineoplastic agent for many types of cancers including lymphoma, leukemia, and solid tumors. However, DXR is known to be associated with various toxic effects such as cardiotoxicity (Yagmurca et al. 2003; Fujimura et al. 2004; Oliveira et al. 2004; Yilmaz et al. 2006). DXR-induced cardiotoxicity is mediated by the formation of free radicals that oxidatively damage many cellular components (Mukherjee et al. 2003; Yagmurca et al. 2003; Oliveira et al. 2004). DXR is enzymatically reduced to its semiquinone radical (Minotti et al. 2001). This DXR semiquinone radical directly transfers its electron to molecular oxygen, generating a superoxide radical and hydrogen peroxide (Gille and Nohl 1997). As reactive oxygen species (ROS) play important roles in DXR-induced toxicity, many compounds with antioxidant properties have been examined as potential therapeutic and/or protective agents. Among these compounds were p-coumaric acid (Abdel-Wahab et al. 2003), garlic acid (Mukherjee et al. 2003), erdosteine (Yagmurca et al. 2003), carvedilol (Oliveira et al. 2004), and lycopene (Yilmaz et al. 2006).
Withania somnifera Dunal (WIT), family Solanaceae, is an annual herb that is most commonly known as ashwagandha. WIT has been used extensively as a valuable drug in Ayurveda, the Indian traditional system of medicine (Mishra et al. 2000; Scartezzini and Speroni 2000). Withanolides are the major active constituents of WIT that are isolated from its root and leaves (Mishra et al. 2000; Scartezzini and Speroni 2000). Previous studies have shown that WIT possesses anti-inflammatory, antitumor, antistress, antioxidant, immunomodulatory, and hepatoprotective properties (Mishra et al. 2000; Scartezzini and Speroni 2000). Cardioprotective effects of WIT have also been documented against myocardial damage induced by strophanthin-K (Dhuley 2000) and by isoproterenol (Mohanty et al. 2004) in different animal models. Moreover, administration of WIT extract was found to reduce the myelosuppression (Davis and Kuttan 1998) and urotoxicity (Davis and Kuttan 2000) induced by antineoplastic agents such as cyclophosphamide in mice. WIT roots have also shown a specific chemopreventive efficacy against forestomach and skin carcinogenesis in mice (Padmavathi et al. 2005).
The purpose of this investigation was to evaluate the protective effects of WIT against DXR-induced cardiotoxicity in male rats and to study the mechanism underlying these effects.
Materials and methods
Chemicals
The herbal formulation of WIT tablets (Ashwaganda; 205154311) was manufactured by Idea Sphere Inc., American Fork, UT, 84003 USA. The herbal formulation of root and leaf tablets contains 300 mg extract, which is standardized by the manufacture company to 1.5% withanolides (4.5 mg of withanolides in each tablet). Apoptag plus Peroxidase in situ Apoptosis Detection Kit was purchased from Chemicon International Inc., Temecula, CA, U.S.A. A kit for serum aspartate aminotransferase activity was purchased from BioMerieux, RCS Lyon, France. o-Dianisidine, 2,4-dinitophenylhydrazine, thiobarbituric acid, Folin reagent, epinephrine, SOD enzyme, H2O2 and bovine albumin were obtained from Sigma Chemical Co., St. Louis, MO, USA. All other chemicals were obtained from local commercial suppliers.
Animals
Adult male albino rats, Wistar strain (150–200 g), were obtained from the Animal House, UAE University, U.A.E. Rats were maintained on standard pellet diet and tap water ad libitum and were kept in polycarbonate cages with wood chip bedding under a 12 h light/dark cycle and at room temperature 22–24°C. Rats were acclimatized to the environment for one week prior to experimental use. The study was approved by the Animal Research Ethics Committee, UAE University.
Treatment regime
DXR (Adriamycin) solution was freshly prepared in a saline solution. WIT tablets were suspended in distilled water. This extract was then used at a dose of 300 mg/kg body weight (bw) (4.5 mg of withanolides), which is equivalent to a volume of 5 ml/kg bw. Rats were randomly divided into four groups (n = 6) and were subjected to the following treatments. In the DXR-treated group, animals were orally administered a dose of distilled water (5 ml/kg bw) for 14 days. After the first 7 days, animals of this group received a single intraperitoneal dose of DXR (10 mg/kg bw) DXR was freshly prepared in a saline solution. This DXR dose was selected as it has been used previously to induce cardiotoxicity in male albino rats (Jang et al. 2004; Yilmaz et al. 2006). Animals of the protective group were fed WIT extract for 14 days and, similarly, cardiotoxicity was induced by injecting the same single dose of DXR after 7 days of WIT administration. The third group was treated with WIT daily for 14 days and injected with single dose of saline (5 ml/kg bw) after 7 days of WIT treatment. The control group was treated with distilled water (5 ml/kg bw) for 14 days and injected with single dose of saline after 7 days of water administration. At the end of treatments and after the last WIT or vehicle solution administration, blood and heart tissues were collected from all groups and stored at −20°C for further processing.
Sample preparation
Following diethyl ether anesthesia, blood was collected from the retro-orbital plexus. Diethyl ether-anesthetized rats were then sacrificed and heart tissues were removed. For histopathological examination, the left half of the heart was immediately fixed in 10% buffered formalin. For biochemical determination, the right half of the heart was homogenized in ice-cold KCl (150 mmol/L). The ratio of tissue weight to homogenization buffer was 1:10. From the latter, suitable dilutions were prepared to determine the levels of calcium, protein carbonyl (P.carbonyl), malondialdehyde (MDA), total antioxidants, and total proteins. To assess the activity of superoxide dismutase (SOD), catalase (CAT), and myeloperoxidase (MPO), suitable dilutions were made in different buffers. To obtain serum, blood was collected in centrifuge tubes and centrifuged in a refrigerated centrifuge (4°C) at 1300 g for 20 min.
Biochemistry and histopathology
MDA is the most abundant individual aldehyde resulting from lipid peroxidation (LP) breakdown in biological systems and is commonly used as an indirect index of LP (Sorg 2004). Determination of MDA, as described by Uchiyama and Mihara (1978), is based on its reaction with thiobarbituric acid (TBA) to form a pink complex with absorption maximum at 535 nm.
CAT activity was determined by measuring the exponential disappearance of H2O2 at 240 nm and expressed in units/mg of protein as described by Aebi (1984).
MPO activity in cardiac homogenate was determined as described in Hillegas et al. (1990). The substrate for MPO assay was potassium phosphate buffer (pH 6.0) containing 0.53 mmol/L o-dianisidine and 20 mmol/L H2O2. Absorbance of the sample was monitored at 460 nm over a period of 3 min. One unit of MPO was defined as the amount of MPO that degrades 1 μmole peroxide per minute.
In heart tissues, the SOD enzyme activity was determined according to the method described by Sun and Zigman (1978). This method is based on the ability of SOD to inhibit the auto-oxidation of epinephrine at alkaline pH to adrenochrome and other derivatives, which are easily monitored in the near-UV region of the absorption spectrum.
P.carbonyl contents were determined according to the method of Reznick and Packer (1994). This method is based on spectrophotometric detection of the end product of the reaction of 2,4-dinitophenylhydrazine with P.carbonyl to form protein hydrazones at 370 nm. The results were expressed as nmoles of carbonyl group per milligram of protein with molar extinction coefficient of 22 000 L M−1cm−1.
The total antioxidant capacity (TAC) in heart tissues was evaluated with the ferric reducing antioxidant power (FRAP) assay. The FRAP assay was determined according to the method described by Benzie and Strain. (1996). The FRAP assay measures the change in absorbance at 593 nm caused by the formation of a blue-colored ferrous-tripyridyltriazine complex from an initially colorless oxidized ferric form. Tissue-embedded electron-donating antioxidants drive the reduction of Fe(III) to Fe(II).
Serum aspartate aminotransferase (AST) activity was measured spectrophotometrically using a Shimadzu recording spectrophotometer (UV-160). The assay was performed using a BioMerieux reagent kit, according to the protocol supplied with the kit.
Calcium content was measured in heart tissues using inductively coupled plasma optical emission spectrometry (ICP-OES) (Varian vista-MPXCCD Simultaneous ICP-OES). Heart samples were digested with concentrated nitric acid and perchloric acid and heated up gently to 200°C until digestion was complete.
The total protein contents of heart tissues were determined according to the Lowry method as modified by Peterson (1977). Absorbance was recorded using a Shimadzu recording spectrophotometer (UV-160) for all measurements.
For the histological examinations, small pieces of heart tissue were fixed in 10% neutral phosphate-buffered formalin. Hydrated tissue sections, 5 μm in thickness, were then stained with hematoxylin and eosin. The sections were examined under a Leica DMRB/E light microscope.
In-situ localization of apoptotic cells
Apoptosis was assessed in deparaffinized sections using the TUNEL technique. In this technique, the manufacturer’s protocol for the Apoptag plus Peroxidase in Situ Apoptosis Detection Kit (Chemicon International, CA, USA) was followed. This method detects the DNA fragmentation associated with apoptosis by labeling 3-OH DNA termini with digoxigenin-nucleotides, a process facilitated by terminal deoxynucleotidyl transferase. The labeled fragments are then allowed to bind to anti-digoxigenin antibody conjugated with peroxidase. Color was developed by adding sufficient peroxidase substrate to specimens. The number of apoptotic cells in each section was calculated by counting the number of TUNEL-positive apoptotic cells in 10 fields per slide at 400× magnification.
Immunohistochemical analysis of Bcl-2
The expression of Bcl-2 protein was studied on sections by immunohistochemistry. Briefly, after deparaffinization and rehydration, tissue sections were treated with 3% hydrogen peroxide for 20 min to diminish nonspecific staining. The sections were immersed in 10 mmol/L citrate buffer solution (pH 6.0) in a microwave oven twice for 5 min and then incubated with normal goat serum for 20 min. Sections were incubated for overnight at 4°C with the rabbit Bcl-2 primary antibody and were then washed with phosphate-buffered saline. Sections were exposed to the avidin-biotin-peroxidase complex (1/400, Dako) for 1 h at room temperature. The chromogenic substrate of peroxidase was developed using a 0.05% solution of 3,3-diaminobenzidine tetrahydrochloride, 0.03% hydrogen peroxide, and imidazol in Tris-HCl buffer (pH 7.6). Sections were counterstained with hematoxylin. The number of immunostained cells was counted in each section per 10 microscopic fields at 400× magnification.
Statistical analysis
SPSS (version 10) (SPSS Inc., Chicago, IL, USA) was used to carry out a one-way analysis of variance (ANOVA) on our data. When significant differences were detected by ANOVA, analyses of differences between the means of the treated and control groups were performed using Dunnett’s t-test.
Results
Biochemical and histological effects on heart tissues
The levels of serum AST as a marker of heart damage significantly increased (p < 0.001) compared to the control after treatment with DXR. The treatment with WIT alone did not show any significant changes in the AST activity (Fig. 1), while concomitant treatment with WIT and DXR treatment attenuated this increase in AST level.
Figure 2a shows the normal architecture of control cardiac muscles. Severe degenerations of the myofibrils, with focal necrosis, and vacuolated cytoplasm were clearly seen in the DXR-treated group. DXR intoxication also induced eosinophilic cytoplasm and focal hemorrhage and with inflammatory cell infiltrations (Fig. 2c,d). Animals pretreated with WIT showed better-preserved appearance of cardiac muscle fibers with slight degeneration and some leukocyte infiltration (Fig. 2e,f). Heart tissues of WIT-treated rats shows normal myofibrillar structure (Fig. 2b).
Photomicrograph of the heart tissues of control (a) and WIT-treated rats (b) showing the normal myofibrillar structure with striations and branched appearance. Heart tissues of DXR-treated rats (c, d) showing focal necrosis of muscle fibers with eosinophilia in the cytoplasm (arrows). Heart tissues of DXR-treated rats also show deformations of muscle fibers with focal hemorrhage (arrowheads) and inflammatory cell infiltrations (stars). Rats treated with WIT+DXR (e, f) before DXR, exhibiting relatively normal myocardial cells with vascular dilatation and moderate degeneration of some fibril cells. (hematoxylin and eosin, ×200.)
Cell death
TUNEL assay was used to identify apoptotic cells in the heart tissues. Brown staining, indicating TUNEL-positive nuclei, was visible in heart tissues of control and WIT-treated animals (Fig. 3a,b). TUNEL-positive cells were significantly increased (p < 0.001), however, in the DXR-treated group compared to the control group (Fig. 3c,e). Concomitant treatment with WIT and DXR significantly prevented the increase in the number of TUNEL-positive cells in DXR treated group (Fig. 3d,e).
TUNEL-positive cells in the heart tissues of rats treated with vehicle (a, control), WIT (b), DXR (c), and WIT+DXR (d). Photomicrographs (a–d) and the semi-quantitative analysis (e) show variable levels of apoptosis in different experimental groups. The number of apoptotic cells in each section was calculated by counting the number of TUNEL-positive cells in 10 fields at 400× magnification. Brown staining indicates TUNEL-positive cells. TUNEL-positive cells are indicated by arrows (hematoxylin counterstained, 400×). ***p < 0.001 vs. control
Effects on MDA and P.carbonyl levels
Levels of both MDA and P.carbonyl were significantly elevated (p < 0.001) in heart tissues of DXR-treated rats compared to control values (Fig. 4a,b). Concurrent treatment with WIT and DXR prevented the elevations of these oxidative stress markers. WIT alone, however, exhibited no significant effects on the MDA and P.carbonyl levels when compared to control groups.
Changes of antioxidants
Heart tissues of rats treated with DXR showed significant depletion in SOD activity (p < 0.001) and in TAC (FRAP) content (p < 0.001). In contrast, the activity of CAT enzyme was elevated significantly (p < 0.001) in heart tissues from this group of rats (Table 1). Interestingly, the treatment with WIT prevented the depletions in SOD activity and TAC content as well as attenuating the elevation in CAT activity. Treatment with WIT alone exhibited no significant effect on the enzyme activity of SOD and CAT or on the content of TAC, compared with control group.
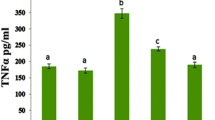
Change in MPO enzyme activity
WIT treatment alone did not induce any change in the activity of MPO enzyme compared to the control group. In contrast, the DXR-treated group exhibited significant (p < 0.001) elevation in the MPO activity in the heart tissues, compared to the control group (Fig. 5). No significant effect on the MPO enzyme activity was detected between the WIT+DXR and control groups.
Effects on cardiac calcium concentrations
DXR-treated rats showed a significant increase (p < 0.001) in heart-specific calcium content (Table 1) in heart tissues. The calcium concentration did not differ significantly from control levels when WIT was administered before DXR treatment. At the same time, WIT alone exhibited no significant effect on calcium levels in heart tissues compared to the control group.
Effects on Bcl-2 protein expression
Using immunohistochemistry, Bcl-2 protein expression was detected in hearts of control and WIT-treated animals (Fig. 6a,b). Brown staining, indicative of positively immunostained cells, was significantly (p < 0.001) increased in the DXR-treated group compared to the control group (Fig. 6c,e). Concomitant treatment with WIT and DXR significantly prevented the increase in the number of Bcl-2-positive cells in the DXR-treated group (Fig. 6d,e).
The protein expression of Bcl-2 in the heart tissues of rats treated with vehicle (a, control), WIT (b), DXR (c), and WIT+DXR (d). Photomicrographs (a–d) and the semi-quantitative analysis (e) show the degree of immunostained cells in different experimental groups. The number of Bcl-2-positive cells in each section was calculated by counting the number of immunostained cells in 10 fields at 400× magnification. Brown staining indicates positive-stained cells. Bcl-2-positive cells are indicated by arrows (hematoxylin counterstain, 400×). ***p < 0.001 vs. control
Discussion
This paper reports an investigation of the protective effects of a standardized extract of WIT against cardiotoxicity and DXR-induced oxidative stress in an animal model. DXR has been reported to cause cardiomyopathy in various animal species (Yagmurca et al. 2003; Fujimura et al. 2004; Oliveira et al. 2004, Yilmaz et al. 2006). The present results showed a significant elevation in serum levels of AST (Fig. 1) (a reliable biomarker of cardiac injury), after treatment with DXR at dose level 10 mg/kg bw. Similarly to many other studies, the DXR-induced myocardial damage reported here was associated with clear myocardial histopathological lesions (myocyte necrosis, degeneration, and inflammatory cell infiltrations, Figs. 2 and 3) (Mukherjee et al. 2003; Yagmurca et al. 2003; Fujimura et al. 2004; Yilmaz et al. 2006).
Oxidative stress is an important biological process that is believed to cause severe damage to cell membranes (Sorg 2004). Oxidative stress has also been implicated as the major contributing factor to the DXR-induced deformation of heart tissues (Dalloz et al. 1999, Yagmurca et al. 2003; Oliveira et al. 2004). In the present work, DXR-induced oxidative stress is confirmed by the elevation of oxidized lipids (MDA) and proteins (P. carbonyl). Interestingly, the DXR-induced oxidation of lipids and proteins were prevented by WIT (Fig. 4), suggesting an antioxidant effect of this herb. In addition, DXR reduced the TAC content and the antioxidant activity of SOD enzyme in the heart (Table 1). Free radicals have been shown to exhaust the antioxidant defense system and hence elevate the oxidation process of both lipids and proteins in heart tissues of DXR-treated rats (Dalloz et al. 1999; Yagmurca et al. 2003; Oliveira et al. 2004). In that context, the anthracycline ring structure of DXR has been shown to induce both enzymatic and nonenzymatic single-electron redox cycle liberation of ROS from molecular oxygen (Gille and Nohl 1997). In the present study, the depletion in antioxidant defense mechanism was associated with the elevation of CAT activity, an enzyme that is normally responsible for H2O2 elimination (Sun and Zigman 1978), in heart and other tissues. Similar results have been reported in male Wistar rats treated with the same dose of DXR as used in this work (Dalloz et al. 1999; Yilmaz et al. 2006). This explains, at least in part, the massive production of H2O2 and its significant role in DXR-induced cardiotoxicity. The redox-cycle of DXR in the presence of cytochrome P450 reductase and NADPH was also shown as a major source of H2O2 in tissues (Gille and Nohl 1997).
WIT alone had no effect on the normal levels of oxidative stress markers (MDA and P.carbonyl). The same was true for the antioxidant profile (TAC, CAT, and SOD) as treatment with WIT alone did not show any effect. However, the concomitant treatment with WIT and DXR restored normal levels of cardiac oxidative stress markers and of antioxidants. WIT extract has been reported to attenuate or inhibit both the lipid and protein oxidative damage induced by copper (Gupta et al. 2003) and by isoproterenol (Mohanty et al. 2004) in the spinal cord and the heart of animal models. It was also shown that WIT was able to scavenge the free radicals produced as a result of lead toxicity in liver and kidney of mice as evidenced by decreased lipid peroxidation and increased activity of antioxidant enzymes in tissues (CAT and SOD) (Chaurasia et al. 2000). It was argued that the antioxidant effect of WIT can be attributed to the presence of steroidal lactones, withanolides, which represent the main active component of WIT (Mishra et al. 2000).
ROS can also be produced and accumulated in the inflammatory cells within cardiac tissues. In the present study, cardiac MPO activity was increased in DXR-treated rats (Fig. 5). This is consistent with results from a previous study (Yagmurca et al. 2003) and indicates an acute inflammation and leukocyte accumulation in heart tissues of the DXR-treated animals (Nicholls and Hazen 2005). During inflammation, activated neutrophils and some polymorphonuclear leukocytes generate a variety of highly reactive oxidants such as hypochlorous acid that are capable of oxidation, halogenation, and nitration of cellular macromolecules (Klebanoff 1999; Nicholls and Hazen 2005). WIT treatment prevented the elevation in renal MPO activity, which indicates inhibition of neutrophil infiltration and inflammation. WIT was reported to possess anti-inflammatory and immunosuppressive properties both in vivo and in vitro (Mishra et al. 2000; Rasool and Varalakshmi 2006).
In addition to their ability to directly inflict damage upon cellular macromolecules, ROS play a pivotal role in apoptosis by initiating mitochondrial damage and activating sensitive signaling pathways (Kannan and Jain 2000). It has been documented that apoptosis plays a crucial role in the pathogenesis of DXR-induced cardiac damage (Fujimura et al. 2004, Jang et al. 2004). In this study, the apoptosis was confirmed by increase in TUNEL-positive cells in heart tissues of DXR-treated rats (Fig. 6). In fact, the anticancer property of DXR has been shown to be mediated by oxidative DNA damage and apoptosis that are a direct result of the DXR-induced production of H2O2 (Mizutani et al. 2005). In agreement with previous investigations, the DXR-induced apoptotic effect (Fig. 6c) shown in this study was associated with an increased expression of anti-apoptotic protein Bcl-2 (Childs et al. 2002, Jang et al. 2004). Bcl-2 protein has been shown to prevent ROS-induced apoptosis through an antioxidant mechanism (Kannan and Jain 2000). Thus, the upregulation of Bcl-2 in the present study may represent an adaptive mechanism during the generation of ROS. Administration of WIT alone did not alter the basal level of apoptotic cells and apoptosis-related protein Bcl-2 (Fig. 6b). However, concomitant treatment of WIT with DXR partially attenuated the elevation of apoptosis and restored normal levels of Bcl-2, suggesting antioxidant and antiapoptotic roles of WIT (Fig. 6d).
Accumulation of intracellular calcium level may lead to both necrotic and apoptotic cell death. ROS is known to cause damage to calcium channels and therefore to cause calcium influx into the cytoplasm from internal cellular stores and from the extracellular spaces (Ermak and Davies 2001; Waring 2005). Necrotic cell death induced by calcium overload is generally thought to be due to the activation of cellular enzymes such as proteases, nucleases, and lipases (Waring 2005). In addition, increased intracellular calcium is associated with mitochondrial calcium accumulation and activation of caspases, which initiate apoptotic cell death (Kannan and Jain 2000; Waring 2005). In the present study, DXR induced an elevation in intracellular calcium concentration while concomitant treatment with WIT and DXR caused a marked reduction in calcium levels in heart tissues (Table 1). This protective effect could be attributed to the WIT antioxidant property proposed in this study and/or its calcium antagonistic property observed in a previous study (Choudhary et al. 2005).
In conclusion, DXR induced elevation of the oxidation end products of lipids and proteins. It also increased the MPO activity and intracellular calcium. However, DXR decreased TAC, and SOD levels of the heart tissue. Cardiotoxicity was confirmed both histologicaly and biochemically. WIT treatment ameliorated oxidative damage and protected against cardiotoxicity induced by DXR in rats. The protective effect of WIT may be mediated through its antioxidant, anti-inflammatory, and calcium-antagonistic properties.
Abbreviations
- AST:
-
aspartate aminotransferase
- CAT:
-
Catalase
- DXR:
-
Doxorubicin
- FRAP:
-
ferric reducing antioxidant power
- LP:
-
lipid peroxidation
- MDA:
-
Malondialdehyde
- MPO:
-
Myeloperoxidase
- ROS:
-
reactive oxygen species
- SOD:
-
superoxide dismutase
- TAC:
-
total antioxidant capacity
- TBA:
-
thiobarbituric acid
- TUNEL:
-
terminal deoxynucleotidyl transferase mediated dUTP nick end labelling
- WIT:
-
Withania somnifera Dunal
References
Abdel-Wahab MH, El-Mahdy MA, Abd-Ellah MF, Helat GK, Khalifa F, Hamada FMA. Influence of p-coumaric acid on doxorubicin-induced oxidative stress in rat heart. Pharmacol Res 2003;48:461–5.
Aebi H. Catalase. Methods Enzymol 1984;105:121–6.
Benzie IF, Strain JJ. The ferric reducing ability of plasma (FRAP) as a measure of (antioxidant power): The FRAP assay. Anal Biochem 1996;293:70–6.
Chaurasia SS, Panda S, Kar A. Withania somnifera root extracts in the regulation of lead-induced oxidative damage in male mouse. Pharmacol Res 2000;41:663–6.
Childs AC, Phaneuf SL, Dirks AJ, Phillips T, Leeuwenburgh C. Doxorubicin treatment in vivo causes cytochrome c release and cardiomyocyte apoptosis, as well as increased mitochondrial efficiency, superoxide dismutase activity, and Bcl-2:Bax ratio. Cancer Res 2002;62:4592–8.
Choudhary MI, Nawaz SA, ul-Haq Z, et al. Withanolides, a new class of natural cholinesterase inhibitors with calcium antagonistic properties. Biochem Biophys Res Commun 2005;334:276–87.
Dalloz F, Maingon P, Cottin Y, Briot F, Horiot JC, Rochette L. Effect of combined irradiation and doxorubicin treatment on cardiac function and antioxidant defenses in the rat. Free Radic Biol Med 1999;26:785–800.
Davis L, Kuttan G. Suppressive effect of cyclophosphamide-induced toxicity by Withania somnifera extract in mice. J Ethnopharmacol 1998;62:209–14.
Davis L, Kuttan G. Effect of Withania somnifera on cyclophosphamide-induced urotoxicity. Cancer Lett 2000;148:9–17.
Dhuley JN. Adaptogenic and cardioprotective action of ashwagandha in rats and frogs. J Ethnopharmacol 2000;70:57–63.
Ermak G, Davies KJA. Calcium and oxidative stress: from cell signaling to cell death. Mol Immunol 2001;38:713–21.
Fujimura L, Matsudo Y, Kang M, Takamori Y, Tokuhisa T, Hatano M. Protective role of Nd1 in doxorubicin-induced cardiotoxicity. Cardiovasc Res 2004;64:315–21.
Gille L, Nohl H. Analyses of the molecular mechanism of adriamycin-induced cardiotoxicity. Free Radic Biol Med 1997;23:775–82.
Gupta SK, Dua A, Vohra BP. Withania somnifera (Ashwagandha) attenuates antioxidant defense in aged spinal cord and inhibits copper induced lipid peroxidation and protein oxidative modifications. Drug Metab Drug Interact 2003;19:211–22.
Hillegas LM, Griswold DE, Brickson B, Albrightson-Winslow C. Assessment of myloperoxidase activity in whole rat kidney. J Pharmacol Methods 1990;24:285–95.
Jang YM, Kendaiah S, Drew B, et al. Doxorubicin treatment in vivo activates caspase-12 mediated cardiac apoptosis in both male and female rats. FEBS Lett 2004;577:483–90.
Kannan K, Jain SK. Oxidative stress and apoptosis. Pathophysiology 2000;7:153–63.
Klebanoff SJ. Myloperoxidase. Proc Assoc Am Physicians 1999;111:383–9.
Minotti G, Parlani M, Salvatorelli E, et al. Impairment of myocardial contractility by anticancer anthracyclines: role of secondary alcohol metabolites and evidence of reduced toxicity by a novel disaccharide analogue. Br J Pharmacol 2001;134(6):1271–8.
Mishra LC, Singh BB, Dagenais S. Scientific basis for the therapeutic use of Withania somnifera (ashwagandha): a review. Altern Med Rev 2000;5:334–46.
Mizutani H, Tada-Oikawa S, Hiraku Y, Kojima M, Kawanishi S. Mehanism of apoptosis induced by doxorubicin through the generation of hydrogen peroxide. Life Sci 2005;76:1439–53.
Mohanty I, Arya DS, Dinda A, Talwar KK, Joshi S, Gupta SK. Mechanisms of cardioprotective effect of Withania somnifera in experimentally induced myocardial infraction. Basic Clin Pharmacol Toxicol 2004;94:184–90.
Mukherjee S, Banerjee SK, Maulik M, Dinda AK, Maulik KS. Protection against acute adriamycin-induced cardiotoxicity by garlic endogenous antioxidants and inhibition of TNF-alpha expression. BMC Pharmacol 2003;3:1–9.
Nicholls S, Hazen SL. Myloperoxidase and cardiovascular disease. Arterioscler Thromb Vasc Biol 2005;25:274–8.
Oliveira PJ, Bjork JA, Santos MS, et al. Carvedilol-mediated antioxidant protection against doxorubicin-induced cardiac mitochondrial toxicity. Toxicol Appl Pharmacol 2004;200:159–68.
Padmavathi B, Rath PC, Rao AR, Singh RP. Roots of Withania somnifera inhibit forestomach and skin carcinogenesis in mice. eCAM 2005;2:99–105.
Peterson GL. A simplification of the protein assay method of Lowry et al which is more generally applicable. Anal Biochem 1977;83:346–56.
Rasool M, Varalakshmi P. Immunomodulatory role of Withania somnifera root powder on experimental induced inflammation: An in vivo and in vitro study. Vascul Pharmacol 2006;44:406–10.
Reznick AZ, Packer L. Oxidative damage to proteins: spectrophotometric method for carbonyl assay. Methods Enzymol 1994;233:357–63.
Scartezzini P, Speroni E. Review on some plants of Indian traditional medicine with antioxidant activity. J Ethnopharmacol 2000;71, 23–43.
Sorg O. Oxidative stress: a theoretical model for a biological reality. Comptes Rendus Biol 2004;327:649–62.
Sun M, Zigman S. An improved spectrophotometric assay for superoxide dismutase based on epinephrine autoxidation. Anal Biochem 1978;247:81–9.
Uchiyama M, Mihara M. Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal Biochem 1978;86:271–8.
Waring P. Redox active calcium ion channels and cell death. Arch Biochem Biophys 2005;434:33–42.
Yagmurca M, Fadillioglu E, Erdogan H, Ucar M, Sogut S, Irmak MK. Erdosterine prevents doxorubicin-induced cardiotoxicity. Pharmacol Res 2003;48:377–82.
Yilmaz S, Atessahin A, Sahna E, Karahan I, Ozer S. Protective effect of lycopene on adriamycin-induced cardiotoxicity and nephrotoxicity. Toxicology 2006;218:164–71.
Acknowledgments
We are grateful to Ms. Duaa Al-Harbawi for her valuable assistance. We also thank Professor Waleed Hamza (Biology Department Head) for his continuous help and support throughout this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hamza, A., Amin, A. & Daoud, S. The protective effect of a purified extract of Withania somnifera against doxorubicin-induced cardiac toxicity in rats. Cell Biol Toxicol 24, 63–73 (2008). https://doi.org/10.1007/s10565-007-9016-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10565-007-9016-z