Abstract
Objective: Despite aggressive reduction of low-density lipoprotein cholesterol (LDL-C), there is a residual risk of cardiovascular disease (CVD). Hypertriglyceridemia is known to be associated with increased CVD risk, independently of LDL-C. Triglycerides are one component of the heterogenous class of triglyceride-rich lipoproteins (TGRLs). Methods/Results: Growing evidence from biology, epidemiology, and genetics supports the contribution of TGRLs to the development of CVD via a number of mechanisms, including through proinflammatory, proapoptotic, and procoagulant pathways. Conclusion: New genetics-guided pharmacotherapies to reduce levels of triglycerides and TGRLs and thus reduce risk of CVD have been developed and will be discussed here.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) remains the leading cause of death in the world, causing nearly 860,000 deaths in the USA alone and 17.8 million globally in 2017 [1]. As a result of significant clinical evidence, low-density lipoprotein cholesterol (LDL-C) reduction via statin therapy has long been a mainstay of primary and secondary prevention of atherosclerotic CVD [2]. However, there appears to be a residual cardiovascular risk even with the use of therapies that aggressively reduce LDL-C levels [3, 4]. This residual risk remains even after multivariate adjustment for other risk factors, including lifestyle factors and comorbidities. Systematic reviews of lipid-lowering therapies that reduce triglyceride (TG) levels more than LDL-C levels demonstrate that lower TG levels are associated with a lower risk of major vascular events, even after adjusting for LDL-C reductions [5].
A growing body of evidence derived from Mendelian randomization (MR) indicates that triglyceride-rich lipoproteins (TGRLs) contribute to the development of atherosclerotic coronary artery disease. TGRLs constitute a heterogeneous class of particles, synthesized from exogenous (chylomicrons) and endogenous (very low-density lipoprotein [VLDL] and intermediate density lipoprotein [IDL]) pathways [6]. Insights from biology, epidemiology, and genetics suggest a causal association between elevated TGRLs, CVD, and mortality [7,8,9].
This review aims to discuss the association between TGRLs and risk of atherosclerotic CVD, as well as the latest genetics-guided pharmacotherapies for TG reduction.
Metabolism of TGRLs
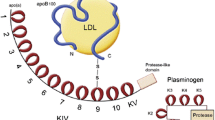
TGRLs are composed of a neutral core of TG and cholesterol esters and a surface monolayer of phospholipids, free cholesterol, and apolipoproteins [10, 11]. TGRLs are synthesized through an exogenous, enterocyte-based pathway and an endogenous hepatocyte-based pathway (Figure 1). Chylomicrons are predominantly formed in the jejunum through the exogenous pathway, and VLDL is synthesized by the liver [12].
After consumption of a meal, gastric lipase in the stomach and then pancreatic lipase in the proximal small intestine hydrolyze dietary TG to form fatty acids and 2-monoacylglycerol (MG) [13]. These lipid products are emulsified by bile salts to produce micelles, which facilitate their absorption by enterocytes through either passive diffusion or with assistance from transporter proteins. Once in the enterocyte, monoacylglycerol:acyl CoA transferase (MGAT) at the smooth endoplasmic reticulum (ER) membrane combines fatty acids and MG into diacylglycerol acids. The enzyme diacylglycerol:acyl CoA transferase (DGAT) subsequently converts these into TG [14]. The TG, along with some cholesteryl esters, are released into the cytosol in transient lipid droplets.
Chylomicron assembly continues through the two-step secretory pathway: the major chylomicron protein, apoB-48, is synthesized in the rough ER and then fuses with lipid droplets to create the primordial chylomicron—both steps require assistance from the microsomal transfer protein (MTP). Pre-chylomicron transport vesicles carry these particles from the ER to the Golgi apparatus where the chylomicrons mature further. As the chylomicron travels between ER and Golgi compartments, various apolipoproteins, such as apoC-III, apoA-I, and apoA-IV, are added to the phospholipid monolayer, creating a diverse array of chylomicron particles [15].
Of note, the size and composition of chylomicrons is dependent on the amount and type of dietary fat ingested and absorbed. They are predominantly composed of TG molecules. Since each chylomicron only has one apoB-48, the variation in size is due to intestinal lipid flux [16, 17].
Mature chylomicrons are ultimately secreted from the basal pole of the enterocyte to the peri-mesenteric lymphatics, which drain into the circulation via the thoracic duct, where they contribute to the postprandial TG concentrations [18]. In the circulation, chylomicrons further acquire apoC-II, apoC-III, and apoE lipoproteins from HDL molecules often via intravascular exchange for apoA-I and apoA-IV. ApoC-III is secreted by both the small intestine and the liver and is exchanged between circulating TGRLs [19]. In addition, the plasma cholesteryl ester transfer protein (CETP) facilitates the intravascular exchange of cholesteryl ester in HDL molecules for TG in the apoB-containing lipoproteins. Thus, chylomicrons that are present longer in the circulation become more enriched in cholesteryl ester. (Unfortunately, several CETP-inhibiting drugs have failed to show meaningful clinical improvement despite increasing HDL levels.) [20]
Lipoprotein lipase (LPL) is an endothelium-localized enzyme that is activated by apoC-II. Hydrolysis of core triglyceride from chylomicrons elaborates free fatty acids and results in the formation of chylomicron remnants. Free fatty acids are oxidized into adenosine triphosphate (ATP) as an energy source by skeletal muscle cells and cardiomyocytes. Excess fatty acids are acquired by adipocytes through diffusion and protein-mediated uptake to be stored [21]. Meanwhile, chylomicron remnants, which are now enriched in cholesteryl esters and contain apoE, bind to LDL receptors (LDLR) on hepatocytes via the apoE ligand or the LDL receptor-related protein 1 (LRP1) through the heparan sulfate proteoglycan pathway and are ultimately removed from the circulation [22]. A third mechanism of clearance via the syndecan-1 receptor and an independent heparan sulfate proteoglycan pathway in hepatocytes also exists [23].
LPL is synthesized by myocytes and adipocytes, which utilize fatty acids for energy and TG storage, respectively [24]. The endothelial glycosylphosphatidylinositol-anchored high-density lipoprotein-binding protein-1 (GPIHBP1) binds LPL at its hydrolase domain, preventing its denaturation and translocates it to the luminal side of capillaries where it can hydrolyze chylomicrons [25,26,27]. LPL is activated by apoC-II and is further tightly regulated at the transcriptional, posttranscriptional, translational, and posttranslational levels [28].
One such regulatory protein is angiopoietin-like protein 4 (ANGPTL4), secreted by adipocytes during fasting states, which inhibits LPL activity, thus increasing plasma TG levels [29, 30]. ANGPTL4 catalyzes the unfolding of the hydrolase domain in LPL, leading to the dissociation of the catalytically active dimer into inactive, unstable monomers [31]. Similarly, angiopoietin-like protein 3 (ANGPTL3) also raises plasma TG levels by inhibiting LPL and HDL-C levels by inhibiting endothelial lipase activity [32]. ANGPTL3 loss-of-function variants result in lower levels of plasma lipoproteins, as seen in conditions like familial hypolipidemia [33].
Meanwhile, increased expression of the APOC3 gene results in hypertriglyceridemia in mice and a null mutation in the gene decreases TG levels, but the mechanism by which apoC-III reduces TG catabolism is less certain [34, 35]. While it was initially believed that apoC-III inhibits LPL via direct competition with apoC-II, this has only been found to be the case when the ratio of apoC-III to apoC-II molecules is higher than what is typically physiologically seen [36]. Further challenging the physiological impact of apoC-III on LPL inhibition, a study in familial chylomicronemia syndrome (FCS) patients, in whom significantly reduced LPL activity results in extremely high plasma TG levels, found that antisense oligonucleotides targeting hepatic APOC3 expression led to reductions in plasma TG levels, suggesting that apoC-III acts independently of LPL as well [37]. Subsequent research demonstrated that apoC-III in fact prevents LDLR and LRP1-mediated remnant TGRL clearance, though the exact mechanism is still under investigation [38]. Another potential mechanism is that the coexistence of apoC-III on VLDL particles reduces apoE binding to LDLR, LRP1, and the syndecan-1 receptor, opposing the role of apoE in metabolism [39]. Conversely, a higher apoE content of VLDL was associated with a lower risk of CVD [40].
The endogenous pathway of TGRL metabolism results in VLDL synthesis in hepatocytes. First, the apoB-100 lipoprotein is made by the rough ER in hepatocytes. Then, similar to the production of chylomicrons, once triglycerides are synthesized from free fatty acids and glycerol, they are subsequently incorporated into the core of the apoB-100 VLDL particles, with help from MTP. VLDL transport vesicles then facilitate movement to the Golgi for further maturation and acquisition of apoE [41, 42]. Upon being secreted into the circulation, VLDL particles gain additional apolipoproteins. LPL again mediates the hydrolysis of VLDLs, resulting in progressively smaller and denser VLDLs and then IDLs, with progressively diminishing amounts of TG (Table 1 and Fig. 1).
Key pathways regulating intestinal and hepatic synthesis and metabolism of triglyceride-rich lipoproteins (TGRLs) are illustrated (see the text for details of these pathways and their genetic regulation).
ANGPTL3 = angiopoietin-like protein 3; Apo = apolipoprotein; CE = cholesterol ester; CETP = cholesteryl ester transfer protein; DGAT = diglyceride acyltransferase; ER = endoplasmic reticulum; FA = fatty acid; HSPG = heparin sulfate proteoglycan; GHIHBP1 = glycosylphosphatidylinositol-anchored high-density lipoprotein-binding protein 1; HDL = high-density lipoprotein; HMG-CoA = hydroxymethylglutaryl-coenzyme A; IDL = intermediate-density lipoprotein; LDL = low-density lipoprotein; LDL-R = low-density lipoprotein receptor; LPL = lipoprotein lipase; LRP1 = low-density lipoprotein receptor-related protein; MG = monoglyceride; MGAT = monoglyceride acyl transferase; MTP = microsomal transfer protein; NPLC1L1 = Niemann-Pick C1 like; PCSK9 = proprotein convertase subtilisin/kexin type 9; PPAR- α = peroxisome proliferator-activated receptor; SERBP-2, sterol regulatory element-binding protein 2; TG = triglyceride; VLDL = very low-density lipoprotein
Pathophysiology of TGRL-Mediated Atherosclerosis
There are several proposed mechanisms by which TGRLs both directly and indirectly promote atherosclerosis. The products of LPL-mediated TGRL lipolysis contribute to atherosclerosis via proinflammatory, procoagulant, and proapoptotic gene activation mechanisms. Similar to LDL, TGRLs and their remnants, which are now cholesterol-rich and TG-depleted, can penetrate the arterial wall and can be bound within the connective tissue matrix. From the subendothelial space, they are then scavenged by arterial wall macrophages, contributing to the formation of macrophage foam cells and plaque progression as the cholesterol cannot be metabolized [43,44,45]. Remnant cholesterol levels can be estimated by non-HDL-C minus LDL-C. Unlike LDL, which must undergo oxidative modification in order to be taken up by macrophages, TGRLs need no further modification [46,47,48]. Additionally, their larger size allows them to carry more cholesterol per particle than LDL, making them equally as or more atherogenic than LDL. VLDL receptors on the macrophage surface selectively recognize apoE ligands rather than apoB, allowing them to bind TGRLs and not LDL [49]. The apoE4 isoform specifically has been found to increase the risk of atherosclerosis in part due to its increased association with VLDL and its subsequent enhanced interaction with LDLR in macrophages [50, 51].
Furthermore, endothelial dysfunction occurs as TGRL lipolysis releases oxidized and neutral free fatty acids that stimulate endothelial inflammation, vascular apoptosis, and reactive oxygen species (ROS) production in endothelial cells. ROS can increase the permeability of vascular endothelium, promote leukocyte adhesion, and even lead to cell injury and death [52]. The increased secretion of proapoptotic cytokines, tumor necrosis factor alpha (TNF-α) and interleukin 1 beta (IL-1β), impair endothelium-dependent vasodilation, increase arterial inflammation, and induce endothelial apoptosis [53].
Finally, inflammation activation occurs as the oxidized free fatty acids released from TGRL hydrolysis induce the expression of inflammatory cytokines (TNF-a) and interleukins (IL-1, IL-6, IL-8). TGRL remnants upregulate the expression of proatherogenic adhesion molecules (intracellular adhesion molecule-1 and vascular cell adhesion molecule-1 [VCAM-1]), which facilitate leukocyte migration to areas of inflammation [54]. They also promote the early activation of monocytes and neutrophils. As a result, inflammatory response is enhanced. TGRLs with lower levels of TG have an atheroprotective effect due to decreased VCAM-1 expression and monocyte recruitment [54,55,56].
TGRLs and remnants also have a procoagulant effect as they enhance platelet aggregation and clot formation by promoting prothrombinase complex assembly and upregulating plasminogen activator inhibitor-1 and plasminogen activator inhibitor-1 antigen expression [57].
Data from computed tomography coronary angiography in patients with suspected CVD has shown that remnant cholesterol levels are associated with significant coronary atherosclerotic plaque burden, even when LDL-C were optimal [58]. There is limited data analyzing more invasive measurements of plaque burden in relation to lipid levels. Challenges with such a study include the multifactorial nature of plaque development and the polygenic causes of hypertriglyceridemia.
Support from Genetic Studies
Human genetic studies over the past several decades have supported the hypothesis that TGs causally influence the development of ASCVD (Table 2). A large Mendelian randomization study utilizing the data from over 10,000 Copenhagen City Heart Study subjects found that decreased concentrations of non-fasting TG as a result of genetic variants in LPL were associated with reduced all-cause mortality [59].
Another multivariable Mendelian randomization meta-analysis examined 185 single nucleotide polymorphisms (SNPs) mapped for lipids in 188,578 people and found a strong correlation between the strength of a particular SNP’s effect on TG levels and the magnitude of its effect on CAD risk. These findings were consistent even with adjustment for effects on LDL-C and HDL-C, supporting the causal influence of TGRLs on CAD risk [60]. Similarly, sequence variants in genes encoding LPL and its regulatory proteins demonstrated a strong association between TGRL metabolism and CAD risk in targeted and exome-wide analyses [61,62,63].
As mentioned previously, loss-of-function studies show that apoC-III overexpression results in hypertriglyceridemia and thus with worsening cardiovascular risk [64]. In one such study, an analysis of 75,725 individuals found that when compared to wildtype individuals, those with heterozygous loss-of-function mutations in the APOC3 gene had a 44% reduction in non-fasting TG levels, which corresponded with a 41% reduction in incidence of CVD [65]. Another study identified four loss-of-function mutations in the APOC3 gene in 3734 individuals. Compared to noncarriers, those who were heterozygous carriers for any of these mutations had a 46% lower concentration of circulating apoC-III, resulting in a 39% lower plasma TG levels and corresponding with a 40% lower risk of CAD [66].
Similar conclusions were drawn from studies of loss-of-function variants in the ANGPTL4 and ANGPTL3 genes. When compared to noncarriers, carriers of the ANGPTL4 variant had lower TG levels and a lower incidence of CAD events [67]. Patients with heterozygous loss-of-function variants in ANGPTL3 in the DiscovEHR human genetics study also had significantly lower levels of TG, HDL-C, and LDL-C than noncarriers. These variants were associated with a decreased odds (adjusted odds ratio 0.59, p=0.004) of ASCVD [68].
Meanwhile, contrasting effects were noted in studies with loss-of-function mutations in the APOA5 gene, which encodes for ApoA-V, an LPL activator. Heterozygous carriers of APOA5 mutations have higher TG levels and were at a 2.2-fold higher risk of myocardial infarction (MI) than noncarriers [69]. In addition, a polymorphism in the promoter region of APOA5 demonstrated an elevated risk of genetically increased TG levels and a resultant increase in CAD [70].
Furthermore, individuals with hyperlipoproteinemia type 3, a monogenic disorder of TG metabolism, are known to be predisposed to CAD, suggesting that the accumulation of TG and remnant cholesterol molecules are significant in their contributions to CVD risk [71].
With regards to the role of HDL-C, classic studies, including the Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial (VA-HIT), indicated an inverse association between HDL-C levels and CAD risk [72,73,74]. The Heart Institute of Japan-Proper level of lipid lOwering with Pitavastatin and Ezetimibe in acute coronary syndrome (HIJ-PROPER) study presented an association between lower levels of HDL-C and higher incidence of cardiovascular events in patients with acute coronary syndrome (ACS) [75]. However, per more recent mendelian randomization studies, this relationship does not appear to be causal [76]. This was also demonstrated in the Atherothrombosis Intervention in Metabolic Syndrome with Low HDL/High Triglycerides and Impact on Global Health Outcomes (AIM-HIGH) trial as the addition of niacin did not result in significant clinical benefit despite raising HDL-C levels [77] (Table 2).
Classic Triglyceride-Lowering Therapies
The foundation of hyperlipidemia management is lifestyle modifications. When secondary factors, unhealthy diets, and poor exercise are addressed, a plasma TG level reduction of up to 60% can be seen [78]. In addition to primarily LDL-lowering therapies, such as statins and ezetimibe, there are currently three classes of drugs available for hypertriglyceridemia management: fibrates, niacin, and omega-3 fatty acids.
Fibrates
Fibrates activate peroxisome proliferator-activated receptor alpha (PPAR-α), a nuclear receptor protein that increases the expression and activity of LPL, apoA-I, and other such genes, while reducing the production of apoB, apoC-III, and VLDL, ultimately having a hypotriglyceridemic effect [79]. PPAR-α promotes fatty acid oxidation and ketogenesis during fasting states [80]. In the VA-HIT and the Helsinki Heart Study, gemfibrozil was found to reduce the risk of ASCVD, but no statistically significant improvement in mortality was noted [73]. In the Helsinki Heart Study, gemfibrozil was noted to have a 34% reduction in the incidence of CAD [81]. Of note, gemfibrozil was found to inhibit the glucuronidation of statins and thus reduce their renal clearance, possibly resulting in serious adverse effects, including rhabdomyolysis [82, 83].
In the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study, fenofibrate resulted in a 24% reduction in nonfatal myocardial infarctions and a significant reduction in total cardiovascular events. However, there was no significant reduction in the primary outcome of coronary events [84]. Furthermore, the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study demonstrated that the combination of fenofibrate and simvastatin did not significantly improve CVD risk when compared to simvastatin alone in patients with type 2 diabetes who were at high risk for CVD [85]. However, post hoc analyses of subgroups with high TG and low HDL-C in each of the aforementioned studies suggested that patients with TG levels greater than 200 mg/dL may benefit. Fenofibrate monotherapy reduced TG levels by 25–50% and LDL-C levels, depending on baseline TG and LDL-C levels, and also raises HDL-C levels by 5–15% [86]. In men with hypertriglyceridemia with low HDL-C, treatment with micronized fenofibrate resulted in a 7% decrease in apoB levels [87]. Potential fibrate-related adverse effects to consider include creatinine level elevations, myopathy, rhabdomyolysis, and increased risk of hepatic steatosis.
Niacin
Niacin inhibits lipolysis in adipocytes, thus reducing the production of fatty acids, which further leads to a decrease in VLDL synthesis in the liver. In addition, niacin reduces concentrations of apoB by accelerating its clearance, notably in hepatic cells [88, 89]. Despite the reduction in TG levels, the Heart Protection Study 2–Treatment of HDL to Reduce the Incidence of Vascular Events (HPS2-THRIVE) and the AIM-HIGH studies did not find adding extended-release niacin (ER-niacin) to statin monotherapy to have a significant impact on risk for cardiovascular events [77, 90]. In patients with type 2 diabetes mellitus, dose-related TG level reductions were noted. Those receiving 1000-mg ER-niacin did not have a statistically significant reduction in TG compared to placebo. Those receiving ER-niacin 1500 mg had a median reduction in TG levels of 28–36%. However, worsening of glycemic status was noted in 27% of individuals in the latter group, potentially diminishing the TG-lowering effect of this agent [91]. With ER-niacin, there was a mild 13% decrease in apoB levels at 1 year in the AIM-HIGH trial, but lipoprotein concentration changes did not significantly affect CVD risk [92]. Additionally, niacin use is associated with a high incidence of side effects, including chemical hepatitis, hyperglycemia, myopathy, and, most commonly, flushing due to cutaneous vasodilation.
Omega-3 Fatty Acids
Omega-3 fatty acids are essential in the formation and stability of cell membranes. They also act as precursors for inflammatory mediators, like prostaglandins, eicosanoids, and leukotrienes. They lower TG levels by reducing TG and apoB secretion from the liver and increasing LPL activity and the rate of TG clearance from the circulation [93]. The most common side effects of omega-3 fatty acids are gastrointestinal. Unfortunately, studies examining the cardiovascular outcomes of omega-3 fatty acids have produced inconsistent results.
There are three major omega-3 fatty acids, each of which has overlapping but unique activities: eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and docosapentaenoic acid (DPA). EPA and DHA both downregulate transcription factor SREBP-1c, which controls lipogenesis. However, EPA is a more potent PPAR-a agonist than DHA. Meanwhile, DHA is more involved in the regulation of hepatic nuclear factor-4 alpha, forkhead box O transcription factor O1, and carbohydrate response element-binding protein [94]. Formulations of these omega-3 fatty acids have been shown to reduce plasma TG levels by 25–45% in patients with severe hypertriglyceridemia [95,96,97].
The EpanoVa fOr Lowering Very high triglyceridEs (EVOLVE) trial demonstrated the effectiveness of omega-3 fatty acids in postprandial, exogenous metabolism, reducing TG and non-HDL-C levels [98]. Furthermore, the Japan EPA Lipid Intervention Study (JELIS) showed a significant reduction in major coronary events when EPA was used in addition to a statin compared to statin monotherapy in patients with a history of CAD [99]. When used in high-risk patients in the Reduction of Cardiovascular Events with Icosapent Ethyl–Intervention Trial (REDUCE-IT), high-dose icosapent ethyl, a highly purified formulation of only EPA, resulted in a significant reduction in major adverse cardiovascular events by 25% and other secondary CVD endpoints by 20–35%. TG levels were reduced by a net of 15% and apoB levels by 9.7%. However, there were no significant differences in the clinical impact of icosapent ethyl in patients with lower or higher baseline TG levels or whether posttreatment TG levels were reduced, suggesting that EPA affects ASCVD risk via non-TG-lowering mechanisms, likely through a multitude of ways [100, 101]. Early results of the Effect of Vascepa on Improving Coronary Atherosclerosis in People with High Triglycerides Taking Statin Therapy trial (EVAPORATE; NCT02926027) demonstrated a statistically significant reduction in low-attenuation coronary plaque volume by coronary computed tomographic angiography in patients treated with high-dose icosapent ethyl after 18 months [102]. Meanwhile, the Phase III Statin Residual Risk Reduction with Epanova in High CV Risk Patients with Hypertriglyceridemia (STRENGTH) trial was discontinued in early 2020 after initial data suggested that Epanova, a combination of EPA and DHA, had a low likelihood of clinical benefit [66, 103].
LDL Therapies with Triglyceride-Lowering Efficacy
While not primarily TG-lowering agents, statins can reduce TG levels by 22–45% in those with baseline TG levels >250mg/dL, with more modest reductions for those with lower baseline TG levels [104]. Atorvastatin has been shown to have dose-dependent reduction effects on total serum TG levels when compared to placebo and lowers TGs in all lipoprotein fractions [105]. In patients with TG levels between 300 and 800 mg/dL, high doses of high-potency statins (i.e., atorvastatin 40 and 80 mg daily and rosuvastatin 20 and 40 mg daily) can reduce TG levels by 37 to 43% [106]. These data support the role of statins in lowering VLDL. However, when the fasting TG concentration is greater than 850–880 mg/dL, statins have limited efficacy as chylomicrons are the predominant plasma lipoproteins. Statins also reduce apoB-containing lipoprotein levels by decreasing hepatic VLDL production, and thus apoB secretion, and increasing LDL receptor-mediated clearance [107]. In the Statin Therapies for Elevated Lipid Levels compared Across doses to Rosuvastatin (STELLAR) trial, rosuvastatin was noted to lower apoB levels by 36.7 to 45.3% [108].
Ezetimibe inhibits the Niemann-Pick C1 Like 1 (NPC1L1) transporter protein, which is responsible for absorbing cholesterol in the small intestine. Inhibition of the transporter channels in hepatocytes also results in decreased reabsorption of cholesterol from the intestines, so that there is an increase in cholesterol excretion from the body and decreased production of apoB lipoprotein [109]. Furthermore, there is a resultant increase in hepatic uptake and degradation of apoB-containing lipoproteins [110]. The Efficacy and Safety of Ezetimibe for Japanese Patients with Dyslipidemia (ESSENTIAL) study demonstrated the efficacy of ezetimibe in reducing LDL-C levels when used both as monotherapy and with a statin after 12 weeks in Japanese patients with dyslipidemia [111]. In the Improved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT), ezetimibe-simvastatin combination therapy (32.7% Kaplan-Meier event rate) resulted in a statistically significant absolute risk reduction of 2% compared to simvastatin monotherapy (34.7% event rate), where the primary endpoint was cardiovascular death, nonfatal MI, nonfatal stroke, and unstable angina needing rehospitalization and revascularization more than 30 days after randomization in the study. Rates of adverse effects were similar in both groups [112]. There was a 13% reduction in apoB levels with ezetimibe alone and a 48% reduction with simvastatin-ezetimibe combination therapy [113].
Lomitapide inhibits MTP, thus interfering with the assembly of apoB-containing lipoproteins and resulting in decreased secretion of both VLDL and chylomicron secretion. Lomitapide 40mg daily was shown to significantly reduce LDL-C levels by 50% in patients with homozygous familial hypercholesterolemia. TG, apoB, and total cholesterol levels were also lower in lomitapide-treated patients compared to placebo, with reductions by 45, 49, and 46%, respectively. However, it was also noted to have reduced HDL-C and apoA-1 levels by 12 and 14%, respectively [114]. Additionally, it is associated with adverse effects including severe gastrointestinal disturbances (such as nausea, vomiting, and diarrhea) and hepatotoxicity as transaminitis and steatosis progressed to fibrosis. Lomitapide also has numerous CYP3A4 interactions. Two case studies have demonstrated the utility of lomitapide in patients with familial chylomicronemia. In the first, the patient had a significant history of recurrent near-fatal pancreatitis as a result of severe hypertriglyceridemia. On starting lomitapide, her fasting TG concentration was reduced from greater than 3000 to 525mg/dL and she did not have further episodes of pancreatitis. However, after 12 to 13 years, her pre-treatment fatty liver progressed to steatohepatitis and fibrosis [115]. Recently, another case study of a patient with recurrent pancreatitis in the setting of familial chylomicronemia demonstrated a 67% reduction in TG levels from baseline, though again with persistent liver steatosis [116]. Given the unclear overall effect on lipids and concern for adverse effects, lomitapide is currently only FDA-approved for the treatment of homozygous familial hypercholesterolemia.
Mipomersen is a second-generation antisense oligonucleotide. It binds to apoB mRNA in hepatocytes, causing its degradation and thus reducing apoB production. As a result of decreased levels of apoB, there is also a decrease in production of chylomicrons, VLDL, and LDL particles. Unlike with lomitapide, a meta-analysis demonstrated that mipomersen significantly reduces non-HDL-C, LDL-C, and apoA-I without reducing HDL-C levels. It was found to decrease apoB levels by 38% and lipoprotein(a) levels by 24% [117]. Adverse effects of concern with mipomersen include transaminitis, hepatic steatosis, and injection site reactions. Like lomitapide, it is currently only FDA-approved for the treatment of homozygous familial hypercholesterolemia in the USA, but manufacturing of mipomersen was discontinued in 2018.
Evolocumab is a monoclonal antibody that inhibits the enzyme proprotein convertase subtilisin/kexin type 9 (PCSK9), which normally recycles LDL receptors on the cell surface, decreasing LDL particle ingestion and increasing plasma LDL-C levels. In the large-scale randomized Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects with Elevated Risk (FOURIER) trial, evolocumab reduced LDL-C levels by 59% and reduced the risk of cardiovascular endpoints (9.8% vs 11.3%, P<0.001) when compared to placebo. Injection site reactions were more common with evolocumab, but otherwise, there were no significant differences in rates of adverse events, like new-onset diabetes and neurocognitive events [118]. A secondary ad hoc analysis of the FOURIER trial demonstrated the comparable efficacy of evolocumab in reducing cardiovascular events irrespective of baseline LDL-C levels (less than 70 mg/dL vs at least 70 mg/dL) and whether the background statin was one of maximum potency [119]. In a study of patients with mixed hyperlipidemia and type 2 diabetes, evolocumab lowered fasting and postprandial chylomicrons suggesting that an increase in LDL (apoB/E) receptor facilitates clearance of remnant particles [120]. A pooled analysis of evolocumab phase 2 and 3 trials demonstrated that it results in comparable significant reductions in LDL-C, non-HDL-C, and apolipoprotein B levels both in patients with and without mixed hyperlipidemia. A modest reduction in TG levels and increase in HDL-C were also noted [121].
Alirocumab is another subcutaneously administered monoclonal antibody against PCSK9. The Evaluation of Cardiovascular Outcomes after an Acute Coronary Syndrome During Treatment with Alirocumab (ODYSSEY Outcomes) trial demonstrated that among patients with prior ACS, the addition of alirocumab to a high intensity statin was associated with a lower risk of recurrent ischemic CVD events than among those who received placebo. The absolute benefit was greater in patients with a baseline LDL-C level greater than 100mg/dL when compared to those with lower baseline levels. The incidence of adverse events was similar in the two groups with a slightly higher incidence of injection site reactions with alirocumab [122]. A pooled analysis of eight controlled phase 3 ODYSSSEY trials showed similar significant reductions in LDL-C, non-HDL-C, and apolipoprotein B levels regardless of revascularization status. There was no statistically significant change in TG levels [123]. However, in the Long-term Safety and Tolerability of Alirocumab in High Cardiovascular Risk Patients with Hypercholesterolemia Not Adequately Controlled with their Lipid Modifying Therapy (ODYSSEY LONG TERM) trial, a mean reduction of 15.6% in TG levels was noted among patients at high risk for cardiovascular events being treated with alirocumab compared to a mean increase of 1.8% in the placebo group [124]. PCSK9 inhibition also results in reduction of the pro-atherogenic lipoprotein(a), which is an LDL particle with apo(a) and apoB-100 moieties. A recent post hoc analysis of the ODYSSEY trial determined that reduction in lipoprotein(a) by alirocumab was an independent contributor to the reduction of major adverse cardiovascular events, suggesting that lipoprotein(a) could be a treatment target in post-ACS patients. The baseline levels of lipoprotein(a) predicted the total risk of cardiovascular events and the alirocumab-induced risk reduction [125].
Inclisiran is another PCSK9 inhibitor, but unlike evolocumab and alirocumab, it is a small interfering RNA molecule that binds to the PCSK9 mRNA and promotes its degradation. Inclisiran thus leads to reduced PCSK9, increased LDL receptor, and reduced plasma LDL-C levels. The Inclisiran or Participants with Atherosclerotic Cardiovascular Disease and Elevated Low-Density Lipoprotein Cholesterol ORION 10 and ORION 11 trial demonstrated a 52.3 and 49.9% reduction in LDL-C, respectively, in the inclisiran group compared to the placebo group after 18 months in patients with increased ASCVD risk and elevated LDL-C levels despite maximal statin therapy. Inclisiran also resulted in apoB level reductions of 44.8 and 38.2% in ORION 10 and ORION 11, respectively. A median reduction of 14.9 and 12% in TG levels was noted in the two trials [126]. The ORION 9 trial similarly showed a reduction of 39.7% in LDL-C levels with inclisiran in patients with heterozygous familial hypercholesterolemia [127]. Unlike typical PCSK9 inhibitors which require monthly or bimonthly injections, inclisiran need only be administered biannually. The ongoing ORION 4 trial is examining the long-term cardiovascular outcomes inclisiran use has in patients being treated with statins as well.
Novel Triglyceride-Lowering Therapies
As more is learned from genetic studies about the mechanisms by which TGRLs promote atherosclerosis, new approaches for therapeutic drug targeting are emerging (Table 3). These novel agents differ with respect to mechanisms of triglyceride lowering and reducing apoB concentrations that may impact the effectiveness of these agents in lowering ASCVD events.
Selective Inhibition of apoC-III
Volanesorsen, previously ISIS-APOCIIIRX, is a second-generation antisense oligonucleotide that binds hepatic acpoC3 mRNA, prompting its degradation, and resulting in decreased plasma apoC-III and TG levels. The APPROACH phase 3 trial demonstrated that patients with familial chylomicronemia syndrome who received volanesorsen had a 77% reduction in TG levels compared to an 18% increase in the placebo group, P<0.001. It additionally led to decreases of 76% in apoB-48 levels, 46% in non-HDL-C, and 58% in VLDL-C. Volanesorsen resulted in increases of 46% in HDL-C, 136% in LDL-C, and 20% in total apoB levels [128]. Major adverse effect concerns include thrombocytopenia and injection site reactions [129]. Volanesorsen has been approved for use in the European Union for patients with familial chylomicronemia syndrome at high risk of pancreatitis who did not have adequate response to traditional medications.
There are also promising ongoing phase 1/2a studies of a hepatocyte-targeted APOC3 small interfering RNA (ARO-APOC3) directed against APOC3 mRNA, which can potentially be dosed quarterly or semi-annually, in healthy adults and in patients with severe hypertriglyceridemia and familial chylomicronemia syndrome (NCT03783377).
Selective Inhibition of ANGPTL3
Vupanorsen is an N-acetyl galactosamine-conjugated antisense oligonucleotide targeting hepatic ANGPTL3 synthesis. A phase 2 double-blind, placebo-controlled, dose-ranging study examined the efficacy of vupanorsen in lowering TG and atherogenic lipoproteins in patients with type 2 diabetes, hepatic steatosis, and hypertriglyceridemia. Vupanorsen at a dose of 80mg every 4 weeks resulted in 53% reduction in fasting TG levels and a 59% reduction in ANGPTL3 concentrations at 6 months compared to 16% TG reduction and 8% increase in ANGPTL3 in the placebo group. It was also associated with reductions of 9% in apoB levels, 58% in apoC-III, and 18% in non-HDL-C [130]. Unlike volanesorsen, there were no significant changes noted in platelet counts with vupanorsen. The most common side effect was a mild injection site reaction. The efficacy of antisense oligonucleotides targeting Angptl3 mRNA was also demonstrated in patients with TG levels greater than 90 mg/dL receiving various doses of the treatment. After 6 weeks, those receiving multiple doses per week had reductions from baseline of 46.6 to 84.5% in ANGPTL3 levels, 33.2 to 63.1% in TG levels, 1.3 to 32.9% in LDL levels, 27.9 to 60% in VLDL levels, and 10 to 36.6% in non-HDL levels [131].
Evinacumab, a monoclonal antibody against ANGPTL3, has been shown to have potential benefit in those with homozygous familial hypercholesterolemia. The ELIPSE phase 3 trial found that patients with homozygous familial hypercholesterolemia receiving evinacumab had a 47.1% relative reduction in LDL-C levels compared to an increase of 1.9% in the placebo group, P<0.001. There was also a 41.4% decrease in apoB levels from baseline, as well as a significant reduction in TG levels [132]. Additionally, in patients with TG levels between 150 and 450mg/dL and LDL-C levels more than 100mg/dL, a significant dose-dependent reduction was noted in TG levels [133]. A recent phase 2 trial in patients with refractory hypercholesterolemia demonstrated a significant reduction in LDL-C levels by more than 50% with the maximum dose of weekly evinacumab [134]. There is an ongoing phase 2 trial in patients with severe hypertriglyceridemia (>500 mg/dL) with prior hospitalization for acute pancreatitis (NCT03452228).
Like ARO-APOC3, there are similar ongoing phase 1/2a studies in healthy patients and those with familial hypercholesterolemia and severe hypertriglyceridemia to evaluate the novel RNA-interference-based agent ARO-ANG3 targeting ANGPTL3 mRNA (NCT03747224).
SPPARMs
Pemafibrate is a selective PPAR-α modulator (SPPARM) that results in the reduction of TG levels and increasing HLD-C levels. It also has nonlipid effects as it appears to play a role in increasing hepatic uptake of glucose and improving insulin sensitivity [135]. Pemafibrate monotherapy demonstrated a 30% mean reduction in TG levels and a 10–15% mean increase in HDL-C after 12 weeks when compared to placebo. When pemafibrate was used in conjunction with statin therapy, there was a 50% reduction in TG. However, there was also an increase in medium and large-sized LDL-C fractions, the impact of which on ASCVD is unclear. Pemafibrate also results in a significant dose-dependent reduction in total apoB and apoB-48 levels [136]. Additionally, one study reported a minor elevation in homocysteine levels, also of uncertain long-term impact. Pemafibrate has been shown to be effective and safe in reducing TG levels in patients with chronic kidney disease, regardless of estimated glomerular filtration rate (eGFR), with similar incidences of adverse events across eGFR groups [137]. It is currently approved in Japan for use in patients with dyslipidemia. Phase 3 trials are ongoing in the USA and Europe. The large-scale Pemafibrate to Reduce Cardiovascular Outcomes by Reducing Triglycerides in Patients with Diabetes trial (PROMINENT; NCT03071692) is underway, evaluating cardiovascular outcomes with the use of pemafibrate as adjunctive therapy to statins in patients with hypertriglyceridemia and type 2 diabetes [138].
FGF21
Fibroblast growth factor 21 (FGF21) plays an important role in angiogenesis and metabolism, in addition to other cell functions. It is expressed in higher levels in the liver, adipose, skeletal muscle, and pancreatic tissue, all of which are involved in metabolism. FGF21 leads to increased hepatic gluconeogenesis and fatty acid oxidation. By inhibiting the lipogenic gene encoding sterol regulatory element-binding protein 2 (SERBP-2), a PCSK9 activator, it results in decreased hepatic cholesterol production and reduces serum TG levels [139]. In mice, FGF21 was shown to reduce plasma non-esterified fatty acid levels and hepatic VLDL lipidation, as well as to increase the catabolism of TGRLs in white and brown adipose tissues, ultimately resulting in lower plasma TG levels [140]. Thus, FGF21 has significant therapeutic implications for TG reduction in humans. A study of LY2405319 (NCT01869959), an FGF21 analog, examined its effect on the lipid profile of obese patients with type 2 diabetes. At a dose of 10 mg per day of the subcutaneously injected molecule, there was a significant reduction of 29.5% in LDL-C, 46.2% in TG levels, and 25.1% in apoB levels from baseline. Further work needs to be done to identify the effects on endogenous FGF21 levels. Injection site reactions and hypersensitivity were the most common adverse effects [141].
Conclusion
Statin therapy continues to be the mainstay of primary and secondary prevention of ASCVD given its powerful ability to reduce LDL-C levels and, to a lesser extent, TGs transported by VLDL and IDL particles. However, significant residual cardiovascular risk remains despite maximally tolerated statin doses. New insights from genetics strongly support a causal association between TGRLs and ASCVD. A number of direct and indirect mechanisms, including proinflammatory, proapoptotic, and procoagulant pathways, allow TGRLs to contribute to ASCVD progression. Therefore, guidelines now recommend the use of TG-lowering therapies in patients with persistently elevated TG or non-HDL-C levels following lifestyle modifications and statin therapies. As specific targets in the causal pathway are identified through genetic studies, novel TGRL-lowering therapies are emerging as new agents to reduce the risk of cardiovascular disease (Table 3).
References
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, et al. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141(9):e139–596.
Jellinger PS, Smith DA, Mehta AE, Ganda O, Handelsman Y, Rodbard HW, et al. American Association of Clinical Endocrinologists' Guidelines for Management of Dyslipidemia and Prevention of Atherosclerosis. Endocr Pract. 2012;18(Suppl 1):1–78.
Sampson UK, Fazio S, Linton MF. Residual cardiovascular risk despite optimal LDL cholesterol reduction with statins: the evidence, etiology, and therapeutic challenges. Curr Atheroscler Rep. 2012;14(1):1–10.
Boekholdt SM, Arsenault BJ, Mora S, Pedersen TR, LaRosa JC, Nestel PJ, et al. Association of LDL cholesterol, non-HDL cholesterol, and apolipoprotein B levels with risk of cardiovascular events among patients treated with statins: a meta-analysis. Jama. 2012;307(12):1302–9.
Marston NA, Giugliano RP, Im K, Silverman MG, O'Donoghue ML, Wiviott SD, et al. Association Between Triglyceride Lowering and Reduction of Cardiovascular Risk Across Multiple Lipid-Lowering Therapeutic Classes: A Systematic Review and Meta-Regression Analysis of Randomized Controlled Trials. Circulation. 2019;140(16):1308–17.
Davidson MH. Triglyceride-rich lipoprotein cholesterol (TRL-C): the ugly stepsister of LDL-C. Eur Heart J. 2018;39(7):620–2.
Nordestgaard BG. Triglyceride-Rich Lipoproteins and Atherosclerotic Cardiovascular Disease: New Insights From Epidemiology, Genetics, and Biology. Circ Res. 2016;118(4):547–63.
Rosenson RS, Davidson MH, Hirsh BJ, Kathiresan S, Gaudet D. Genetics and causality of triglyceride-rich lipoproteins in atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2014;64(23):2525–40.
Toth PP. Triglyceride-rich lipoproteins as a causal factor for cardiovascular disease. Vasc Health Risk Manag. 2016;12:171–83.
Feingold KR GC. Introduction to Lipids and Lipoproteins. Endotext; 2018.
Xiao C, Hsieh J, Adeli K, Lewis GF. Gut-liver interaction in triglyceride-rich lipoprotein metabolism. Am J Physiol Endocrinol Metab. 2011;301(3):E429–46.
Ginsberg HN. Lipoprotein physiology. Endocrinol Metab Clin N Am. 1998;27(3):503–19.
Demignot S, Beilstein F, Morel E. Triglyceride-rich lipoproteins and cytosolic lipid droplets in enterocytes: key players in intestinal physiology and metabolic disorders. Biochimie. 2014;96:48–55.
Cases S, Stone SJ, Zhou P, Yen E, Tow B, Lardizabal KD, et al. Cloning of DGAT2, a second mammalian diacylglycerol acyltransferase, and related family members. J Biol Chem. 2001;276(42):38870–6.
Siddiqi SA, Mansbach CM. PKCζ-mediated phosphorylation controls budding of the pre-chylomicron transport vesicle. J Cell Sci. 2008;121(14):2327–38.
Desmarchelier C, Borel P, Lairon D, Maraninchi M, Valéro R. Effect of Nutrient and Micronutrient Intake on Chylomicron Production and Postprandial Lipemia. Nutrients. 2019;11(6):1299.
Kindel T, Lee DM, Tso P. The mechanism of the formation and secretion of chylomicrons. Atheroscler Suppl. 2010;11(1):11–6.
Bouchoux J, Beilstein F, Pauquai T, Guerrera IC, Chateau D, Ly N, et al. The proteome of cytosolic lipid droplets isolated from differentiated Caco-2/TC7 enterocytes reveals cell-specific characteristics. Biol Cell. 2011;103(11):499–517.
Khetarpal SA, Zeng X, Millar JS, Vitali C, Somasundara AVH, Zanoni P, et al. A human APOC3 missense variant and monoclonal antibody accelerate apoC-III clearance and lower triglyceride-rich lipoprotein levels. Nat Med. 2017;23(9):1086–94.
Diffenderfer MR, Brousseau ME, Millar JS, Barrett PH, Nartsupha C, Schaefer PM, et al. Effects of CETP inhibition on triglyceride-rich lipoprotein composition and apoB-48 metabolism. J Lipid Res. 2012;53(6):1190–9.
Thompson BR, Lobo S, Bernlohr DA. Fatty acid flux in adipocytes: the in's and out's of fat cell lipid trafficking. Mol Cell Endocrinol. 2010;318(1-2):24–33.
Adiels M, Matikainen N, Westerbacka J, Söderlund S, Larsson T, Olofsson SO, et al. Postprandial accumulation of chylomicrons and chylomicron remnants is determined by the clearance capacity. Atherosclerosis. 2012;222(1):222–8.
Foley EM, Gordts PLSM, Stanford KI, Gonzales JC, Lawrence R, Stoddard N, et al. Hepatic Remnant Lipoprotein Clearance by Heparan Sulfate Proteoglycans and Low-Density Lipoprotein Receptors Depend on Dietary Conditions in Mice. Arterioscler Thromb Vasc Biol. 2013;33(9):2065–74.
Wong H, Schotz MC. The lipase gene family. J Lipid Res. 2002;43(7):993–9.
Larsson M, Allan CM, Jung RS, Heizer PJ, Beigneux AP, Young SG, et al. Apolipoprotein C-III inhibits triglyceride hydrolysis by GPIHBP1-bound LPL. J Lipid Res. 2017;58(9):1893–902.
Birrane G, Beigneux AP, Dwyer B, Strack-Logue B, Kristensen KK, Francone OL, et al. Structure of the lipoprotein lipase-GPIHBP1 complex that mediates plasma triglyceride hydrolysis. Proc Natl Acad Sci U S A. 2019;116(5):1723–32.
Arora R, Nimonkar AV, Baird D, Wang C, Chiu CH, Horton PA, et al. Structure of lipoprotein lipase in complex with GPIHBP1. Proc Natl Acad Sci U S A. 2019;116(21):10360–5.
Kersten S. Physiological regulation of lipoprotein lipase. Biochim Biophys Acta. 2014;1841(7):919–33.
Kersten S, Mandard S, Tan NS, Escher P, Metzger D, Chambon P, et al. Characterization of the fasting-induced adipose factor FIAF, a novel peroxisome proliferator-activated receptor target gene. J Biol Chem. 2000;275(37):28488–93.
Dijk W, Schutte S, Aarts EO, Janssen IMC, Afman L, Kersten S. Regulation of angiopoietin-like 4 and lipoprotein lipase in human adipose tissue. J Clin Lipidol. 2018;12(3):773–83.
Sukonina V, Lookene A, Olivecrona T, Olivecrona G. Angiopoietin-like protein 4 converts lipoprotein lipase to inactive monomers and modulates lipase activity in adipose tissue. Proc Natl Acad Sci U S A. 2006;103(46):17450–5.
Liu J, Afroza H, Rader DJ, Jin W. Angiopoietin-like protein 3 inhibits lipoprotein lipase activity through enhancing its cleavage by proprotein convertases. J Biol Chem. 2010;285(36):27561–70.
Minicocci I, Santini S, Cantisani V, Stitziel N, Kathiresan S, Arroyo JA, et al. Clinical characteristics and plasma lipids in subjects with familial combined hypolipidemia: a pooled analysis. J Lipid Res. 2013;54(12):3481–90.
Ito Y, Azrolan N, O'Connell A, Walsh A, Breslow JL. Hypertriglyceridemia as a result of human apo CIII gene expression in transgenic mice. Science. 1990;249(4970):790–3.
Pollin TI, Damcott CM, Shen H, Ott SH, Shelton J, Horenstein RB, et al. A null mutation in human APOC3 confers a favorable plasma lipid profile and apparent cardioprotection. Science. 2008;322(5908):1702–5.
Ramms B, Gordts PLSM. Apolipoprotein C-III in triglyceride-rich lipoprotein metabolism. Curr Opin Lipidol. 2018;29(3):171–9.
Gaudet D, Brisson D, Tremblay K, Alexander VJ, Singleton W, Hughes SG, et al. Targeting APOC3 in the Familial Chylomicronemia Syndrome. N Engl J Med. 2014;371(23):2200–6.
Ramms B, Patel S, Nora C, Pessentheiner AR, Chang MW, Green CR, et al. ApoC-III ASO promotes tissue LPL activity in the absence of apoE-mediated TRL clearance. J Lipid Res. 2019;60(8):1379–95.
Tomiyasu K, Walsh BW, Ikewaki K, Judge H, Sacks FM. Differential Metabolism of Human VLDL According to Content of ApoE and ApoC-III. Arterioscler Thromb Vasc Biol. 2001;21(9):1494–500.
Mendivil CO, Rimm EB, Furtado J, Sacks FM. Apolipoprotein E in VLDL and LDL with apolipoprotein C-III is associated with a lower risk of coronary heart disease. J Am Heart Assoc. 2013;2(3):e000130.
Gusarova V, Brodsky JL, Fisher EA. Apolipoprotein B100 exit from the endoplasmic reticulum (ER) is COPII-dependent, and its lipidation to very low density lipoprotein occurs post-ER. J Biol Chem. 2003;278(48):48051–8.
Hamilton RL, Moorehouse A, Havel RJ. Isolation and properties of nascent lipoproteins from highly purified rat hepatocytic Golgi fractions. J Lipid Res. 1991;32(3):529–43.
Nordestgaard BG, Stender S, Kjeldsen K. Reduced atherogenesis in cholesterol-fed diabetic rabbits. Giant lipoproteins do not enter the arterial wall. Arteriosclerosis. 1988;8(4):421–8.
Rapp JH, Lespine A, Hamilton RL, Colyvas N, Chaumeton AH, Tweedie-Hardman J, et al. Triglyceride-rich lipoproteins isolated by selected-affinity anti-apolipoprotein B immunosorption from human atherosclerotic plaque. Arterioscler Thromb. 1994;14(11):1767–74.
Nordestgaard BG, Wootton R, Lewis B. Selective retention of VLDL, IDL, and LDL in the arterial intima of genetically hyperlipidemic rabbits in vivo. Molecular size as a determinant of fractional loss from the intima-inner media. Arterioscler Thromb Vasc Biol. 1995;15(4):534–42.
Batt KV, Patel L, Botham KM, Suckling KE. Chylomicron remnants and oxidised low density lipoprotein have differential effects on the expression of mRNA for genes involved in human macrophage foam cell formation. J Mol Med (Berl). 2004;82(7):449–58.
Goldstein JL, Ho YK, Brown MS, Innerarity TL, Mahley RW. Cholesteryl ester accumulation in macrophages resulting from receptor-mediated uptake and degradation of hypercholesterolemic canine beta-very low density lipoproteins. J Biol Chem. 1980;255(5):1839–48.
Takahashi S, Sakai J, Fujino T, Hattori H, Zenimaru Y, Suzuki J, et al. The very low-density lipoprotein (VLDL) receptor: characterization and functions as a peripheral lipoprotein receptor. J Atheroscler Thromb. 2004;11(4):200–8.
Takahashi S. Triglyceride Rich Lipoprotein -LPL-VLDL Receptor and Lp(a)-VLDL Receptor Pathways for Macrophage Foam Cell Formation. J Atheroscler Thromb. 2017;24(6):552–9.
Altenburg M, Johnson L, Wilder J, Maeda N. Apolipoprotein E4 in macrophages enhances atherogenesis in a low density lipoprotein receptor-dependent manner. J Biol Chem. 2007;282(11):7817–24.
Phillips MC. Apolipoprotein E isoforms and lipoprotein metabolism. IUBMB Life. 2014;66(9):616–23.
Hadi HA, Carr CS, Al SJ. Endothelial dysfunction: cardiovascular risk factors, therapy, and outcome. Vasc Health Risk Manag. 2005;1(3):183–98.
Shin HK, Kim YK, Kim KY, Lee JH, Hong KW. Remnant lipoprotein particles induce apoptosis in endothelial cells by NAD(P)H oxidase-mediated production of superoxide and cytokines via lectin-like oxidized low-density lipoprotein receptor-1 activation: prevention by cilostazol. Circulation. 2004;109(8):1022–8.
Wang YI, Bettaieb A, Sun C, DeVerse JS, Radecke CE, Mathew S, et al. Triglyceride-rich lipoprotein modulates endothelial vascular cell adhesion molecule (VCAM)-1 expression via differential regulation of endoplasmic reticulum stress. PLoS One. 2013;8(10):e78322.
Sun C, Alkhoury K, Wang YI, Foster GA, Radecke CE, Tam K, et al. IRF-1 and miRNA126 modulate VCAM-1 expression in response to a high-fat meal. Circ Res. 2012;111(8):1054–64.
Gower RM, Wu H, Foster GA, Devaraj S, Jialal I, Ballantyne CM, et al. CD11c/CD18 expression is upregulated on blood monocytes during hypertriglyceridemia and enhances adhesion to vascular cell adhesion molecule-1. Arterioscler Thromb Vasc Biol. 2011;31(1):160–6.
Olufadi R, Byrne CD. Effects of VLDL and remnant particles on platelets. Pathophysiol Haemost Thromb. 2006;35(3-4):281–91.
Lin A, Nerlekar N, Rajagopalan A, Yuvaraj J, Modi R, Mirzaee S, et al. Remnant cholesterol and coronary atherosclerotic plaque burden assessed by computed tomography coronary angiography. Atherosclerosis. 2019;284:24–30.
Thomsen M, Varbo A, Tybjærg-Hansen A, Nordestgaard BG. Low nonfasting triglycerides and reduced all-cause mortality: a mendelian randomization study. Clin Chem. 2014;60(5):737–46.
Do R, Willer CJ, Schmidt EM, Sengupta S, Gao C, Peloso GM, et al. Common variants associated with plasma triglycerides and risk for coronary artery disease. Nat Genet. 2013;45(11):1345–52.
Varbo A, Benn M, Tybjærg-Hansen A, Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013;61(4):427–36.
Khera AV, Won HH, Peloso GM, O'Dushlaine C, Liu D, Stitziel NO, et al. Association of Rare and Common Variation in the Lipoprotein Lipase Gene With Coronary Artery Disease. Jama. 2017;317(9):937–46.
Liu DJ, Peloso GM, Yu H, Butterworth AS, Wang X, Mahajan A, et al. Exome-wide association study of plasma lipids in >300,000 individuals. Nat Genet. 2017;49(12):1758–66.
Wyler von Ballmoos MC, Haring B, Sacks FM. The risk of cardiovascular events with increased apolipoprotein CIII: A systematic review and meta-analysis. J Clin Lipidol. 2015;9(4):498–510.
Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG, Tybjærg-Hansen A. Loss-of-function mutations in APOC3 and risk of ischemic vascular disease. N Engl J Med. 2014;371(1):32–41.
Crosby J, Peloso GM, Auer PL, Crosslin DR, Stitziel NO, Lange LA, et al. Loss-of-function mutations in APOC3, triglycerides, and coronary disease. N Engl J Med. 2014;371(1):22–31.
Folsom AR, Peacock JM, Demerath E, Boerwinkle E. Variation in ANGPTL4 and risk of coronary heart disease: the Atherosclerosis Risk in Communities Study. Metabolism. 2008;57(11):1591–6.
Dewey FE, Gusarova V, Dunbar RL, O'Dushlaine C, Schurmann C, Gottesman O, et al. Genetic and Pharmacologic Inactivation of ANGPTL3 and Cardiovascular Disease. N Engl J Med. 2017;377(3):211–21.
Do R, Stitziel NO, Won HH, Jørgensen AB, Duga S, Angelica Merlini P, et al. Exome sequencing identifies rare LDLR and APOA5 alleles conferring risk for myocardial infarction. Nature. 2015;518(7537):102–6.
Sarwar N, Sandhu MS, Ricketts SL, Butterworth AS, Di Angelantonio E, Boekholdt SM, et al. Triglyceride-mediated pathways and coronary disease: collaborative analysis of 101 studies. Lancet. 2010;375(9726):1634–9.
Brahm A, Hegele RA. Hypertriglyceridemia. Nutrients. 2013;5(3):981–1001.
Wilkins JT, Seckler HS. HDL modification: recent developments and their relevance to atherosclerotic cardiovascular disease. Curr Opin Lipidol. 2019;30(1):24–9.
Rubins HB, Robins SJ, Collins D, Fye CL, Anderson JW, Elam MB, et al. Gemfibrozil for the Secondary Prevention of Coronary Heart Disease in Men with Low Levels of High-Density Lipoprotein Cholesterol. N Engl J Med. 1999;341(6):410–8.
Huxley RR, Barzi F, Lam TH, Czernichow S, Fang X, Welborn T, et al. Isolated Low Levels of High-Density Lipoprotein Cholesterol Are Associated With an Increased Risk of Coronary Heart Disease. Circulation. 2011;124(19):2056–64.
Nakazawa M, Arashi H, Yamaguchi J, Ogawa H, Hagiwara N. Lower levels of high-density lipoprotein cholesterol are associated with increased cardiovascular events in patients with acute coronary syndrome. Atherosclerosis. 2020;303:21–8.
Voight BF, Peloso GM, Orho-Melander M, Frikke-Schmidt R, Barbalic M, Jensen MK, et al. Plasma HDL cholesterol and risk of myocardial infarction: a mendelian randomisation study. Lancet. 2012;380(9841):572–80.
Niacin in Patients with Low HDL Cholesterol Levels Receiving Intensive Statin Therapy. N Engl J Med. 2011;365(24):2255–67.
Watts GF, Ooi EM, Chan DC. Demystifying the management of hypertriglyceridaemia. Nat Rev Cardiol. 2013;10(11):648–61.
Staels B, Dallongeville J, Auwerx J, Schoonjans K, Leitersdorf E, Fruchart JC. Mechanism of action of fibrates on lipid and lipoprotein metabolism. Circulation. 1998;98(19):2088–93.
Vega GL, Cater NB, Hadizadeh DR 3rd, Meguro S, Grundy SM. Free fatty acid metabolism during fenofibrate treatment of the metabolic syndrome. Clin Pharmacol Ther. 2003;74(3):236–44.
Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med. 1987;317(20):1237–45.
Chang JT, Staffa JA, Parks M, Green L. Rhabdomyolysis with HMG-CoA reductase inhibitors and gemfibrozil combination therapy. Pharmacoepidemiol Drug Saf. 2004;13(7):417–26.
Kyrklund C, Backman JT, Neuvonen M, Neuvonen PJ. Gemfibrozil increases plasma pravastatin concentrations and reduces pravastatin renal clearance. Clin Pharmacol Ther. 2003;73(6):538–44.
Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet. 2005;366(9500):1849–61.
Ginsberg HN, Elam MB, Lovato LC, Crouse JR 3rd, Leiter LA, Linz P, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1563–74.
Rosenson RS. Fenofibrate: treatment of hyperlipidemia and beyond. Expert Rev Cardiovasc Ther. 2008;6(10):1319–30.
Genest JJ, Nguyen N-H, Theroux P, Davignon J, Cohn JS. Effect of Micronized Fenofibrate on Plasma Lipoprotein Levels and Hemostatic Parameters of Hypertriglyceridemic Patients with Low Levels of High-Density Lipoprotein Cholesterol in the Fed and Fasted State. J Cardiovasc Pharmacol. 2000;35(1):164–72.
Lamon-Fava S, Diffenderfer MR, Barrett PH, Buchsbaum A, Nyaku M, Horvath KV, et al. Extended-release niacin alters the metabolism of plasma apolipoprotein (Apo) A-I and ApoB-containing lipoproteins. Arterioscler Thromb Vasc Biol. 2008;28(9):1672–8.
Jin FY, Kamanna VS, Kashyap ML. Niacin accelerates intracellular ApoB degradation by inhibiting triacylglycerol synthesis in human hepatoblastoma (HepG2) cells. Arterioscler Thromb Vasc Biol. 1999;19(4):1051–9.
Effects of Extended-Release Niacin with Laropiprant in High-Risk Patients. N Engl J Med. 2014;371(3):203–12.
Grundy SM, Vega GL, McGovern ME, Tulloch BR, Kendall DM, Fitz-Patrick D, et al. Efficacy, Safety, and Tolerability of Once-Daily Niacin for the Treatment of Dyslipidemia Associated With Type 2 Diabetes: Results of the Assessment of Diabetes Control and Evaluation of the Efficacy of Niaspan Trial. Arch Intern Med. 2002;162(14):1568–76.
Albers JJ, Slee A, O'Brien KD, Robinson JG, Kashyap ML, Kwiterovich PO Jr, et al. Relationship of apolipoproteins A-1 and B, and lipoprotein(a) to cardiovascular outcomes: the AIM-HIGH trial (Atherothrombosis Intervention in Metabolic Syndrome with Low HDL/High Triglyceride and Impact on Global Health Outcomes). J Am Coll Cardiol. 2013;62(17):1575–9.
Yanai H, Masui Y, Katsuyama H, Adachi H, Kawaguchi A, Hakoshima M, et al. An Improvement of Cardiovascular Risk Factors by Omega-3 Polyunsaturated Fatty Acids. J Clin Med Res. 2018;10(4):281–9.
Chen YJ, Chen CC, Li TK, Wang PH, Liu LR, Chang FY, et al. Docosahexaenoic acid suppresses the expression of FoxO and its target genes. J Nutr Biochem. 2012;23(12):1609–16.
AstraZeneca Epanova Prescribing Information. 2014. http://www.astrazeneca-us.com/pi/epanova.pdf. Accessed Oct 2020.
GlaxoSmithKline. Lovaza Prescribing Information. 2014. https://www.gsksource.com/gskprm/htdocs/documents/LOVAZA-PI-PIL.PDF. Accessed Oct 2020.
Corporation A. Vascepa Prescibing Information. 2014. www.vascepa.com/full-prescribing-information.pdf. Accessed Oct 2020.
Kastelein JJ, Maki KC, Susekov A, Ezhov M, Nordestgaard BG, Machielse BN, et al. Omega-3 free fatty acids for the treatment of severe hypertriglyceridemia: the EpanoVa fOr Lowering Very high triglyceridEs (EVOLVE) trial. J Clin Lipidol. 2014;8(1):94–106.
Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet. 2007;369(9567):1090–8.
Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, et al. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J Med. 2019;380(1):11–22.
Harris WS. Understanding why REDUCE-IT was positive - Mechanistic overview of eicosapentaenoic acid. Prog Cardiovasc Dis. 2019;62(5):401–5.
Budoff MJ, Bhatt DL, Kinninger A, Lakshmanan S, Muhlestein JB, Le VT, et al. Effect of icosapent ethyl on progression of coronary atherosclerosis in patients with elevated triglycerides on statin therapy: final results of the EVAPORATE trial. Eur Heart J. 2020;41:3925–32.
AstraZeneca. Update on Phase III STRENGTH trial for Epanova in mixed dyslipidaemia. 2020. https://www.astrazeneca.com/media-centre/press-releases/2020/update-on-phase-iii-strength-trial-for-epanova-in-mixed-dyslipidaemia-13012020.html. Accessed Oct 2020.
Stein EA, Lane M, Laskarzewski P. Comparison of statins in hypertriglyceridemia. Am J Cardiol. 1998;81(4a):66b–9b.
Bakker-Arkema RG, Davidson MH, Goldstein RJ, Davignon J, Isaacsohn JL, Weiss SR, et al. Efficacy and Safety of a New HMG-CoA Reductase Inhibitor, Atorvastatin, in Patients With Hypertriglyceridemia. JAMA. 1996;275(2):128–33.
Hunninghake DB, Stein EA, Bays HE, Rader DJ, Chitra RR, Simonson SG, et al. Rosuvastatin improves the atherogenic and atheroprotective lipid profiles in patients with hypertriglyceridemia. Coron Artery Dis. 2004;15(2):115–23.
Chapman MJ, Caslake M, Packard C, McTaggart F. New dimension of statin action on ApoB atherogenicity. Clin Cardiol. 2003;26(1 Suppl 1):I7–10.
Jones PH, Hunninghake DB, Ferdinand KC, Stein EA, Gold A, Caplan RJ, et al. Effects of rosuvastatin versus atorvastatin, simvastatin, and pravastatin on non-high-density lipoprotein cholesterol, apolipoproteins, and lipid ratios in patients with hypercholesterolemia: additional results from the STELLAR trial. Clin Ther. 2004;26(9):1388–99.
Basso F, Freeman LA, Ko C, Joyce C, Amar MJ, Shamburek RD, et al. Hepatic ABCG5/G8 overexpression reduces apoB-lipoproteins and atherosclerosis when cholesterol absorption is inhibited. J Lipid Res. 2007;48(1):114–26.
Telford DE, Sutherland BG, Edwards JY, Andrews JD, Barrett PHR, Huff MW. The molecular mechanisms underlying the reduction of LDL apoB-100 by ezetimibe plus simvastatin. J Lipid Res. 2007;48(3):699–708.
Sawayama Y, Maeda S, Ohnishi H, Hayashi S, Hayashi J. Efficacy and safety of ezetimibe for Japanese patients with dyslipidaemia: The ESSENTIAL Study. Clin Drug Investig. 2010;30(3):157–66.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N Engl J Med. 2015;372(25):2387–97.
Ahmed O, Littmann K, Gustafsson U, Pramfalk C, Öörni K, Larsson L, et al. Ezetimibe in Combination With Simvastatin Reduces Remnant Cholesterol Without Affecting Biliary Lipid Concentrations in Gallstone Patients. J Am Heart Assoc. 2018;7(24):e009876.
Cuchel M, Meagher EA, du Toit TH, Blom DJ, Marais AD, Hegele RA, et al. Efficacy and safety of a microsomal triglyceride transfer protein inhibitor in patients with homozygous familial hypercholesterolaemia: a single-arm, open-label, phase 3 study. Lancet. 2013;381(9860):40–6.
Sacks FM, Stanesa M, Hegele RA. Severe Hypertriglyceridemia With Pancreatitis: Thirteen Years’ Treatment With Lomitapide. JAMA Intern Med. 2014;174(3):443–7.
Cefalù AB, Giammanco A, Noto D, Spina R, Cabibi D, Barbagallo CM, et al. Effectiveness and safety of lomitapide in a patient with familial chylomicronemia syndrome. Endocrine. 2020;71:344–50.
Thomas GS, Cromwell WC, Ali S, Chin W, Flaim JD, Davidson M. Mipomersen, an apolipoprotein B synthesis inhibitor, reduces atherogenic lipoproteins in patients with severe hypercholesterolemia at high cardiovascular risk: a randomized, double-blind, placebo-controlled trial. J Am Coll Cardiol. 2013;62(23):2178–84.
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N Engl J Med. 2017;376(18):1713–22.
Giugliano RP, Keech A, Murphy SA, Huber K, Tokgozoglu SL, Lewis BS, et al. Clinical Efficacy and Safety of Evolocumab in High-Risk Patients Receiving a Statin: Secondary Analysis of Patients With Low LDL Cholesterol Levels and in Those Already Receiving a Maximal-Potency Statin in a Randomized Clinical Trial. JAMA Cardiol. 2017;2(12):1385–91.
Rosenson RS, Daviglus ML, Handelsman Y, Pozzilli P, Bays H, Monsalvo ML, et al. Efficacy and safety of evolocumab in individuals with type 2 diabetes mellitus: primary results of the randomised controlled BANTING study. Diabetologia. 2019;62(6):948–58.
Rosenson RS, Jacobson TA, Preiss D, Djedjos CS, Dent R, Bridges I, et al. Efficacy and Safety of the PCSK9 Inhibitor Evolocumab in Patients with Mixed Hyperlipidemia. Cardiovasc Drugs Ther. 2016;30(3):305–13.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome. N Engl J Med. 2018;379(22):2097–107.
Kereiakes DJ, Lepor NE, Gerber R, Veronica Lee L, Elassal J, Thompson D, et al. Efficacy and safety of alirocumab in patients with or without prior coronary revascularization: Pooled analysis of eight ODYSSEY phase 3 trials. Atherosclerosis. 2018;277:211–8.
Robinson JG, Farnier M, Krempf M, Bergeron J, Luc G, Averna M, et al. Efficacy and Safety of Alirocumab in Reducing Lipids and Cardiovascular Events. N Engl J Med. 2015;372(16):1489–99.
Szarek M, Bittner VA, Aylward P, Baccara-Dinet M, Bhatt DL, Diaz R, et al. Lipoprotein(a) lowering by alirocumab reduces the total burden of cardiovascular events independent of low-density lipoprotein cholesterol lowering: ODYSSEY OUTCOMES trial. Eur Heart J. 2020;41:4245–55.
Ray KK, Wright RS, Kallend D, Koenig W, Leiter LA, Raal FJ, et al. Two Phase 3 Trials of Inclisiran in Patients with Elevated LDL Cholesterol. N Engl J Med. 2020;382(16):1507–19.
Raal FJ, Kallend D, Ray KK, Turner T, Koenig W, Wright RS, et al. Inclisiran for the Treatment of Heterozygous Familial Hypercholesterolemia. N Engl J Med. 2020;382(16):1520–30.
Witztum JL, Gaudet D, Freedman SD, Alexander VJ, Digenio A, Williams KR, et al. Volanesorsen and Triglyceride Levels in Familial Chylomicronemia Syndrome. N Engl J Med. 2019;381(6):531–42.
Esan O, Wierzbicki AS. Volanesorsen in the Treatment of Familial Chylomicronemia Syndrome or Hypertriglyceridaemia: Design, Development and Place in Therapy. Drug Des Devel Ther. 2020;14:2623–36.
Gaudet D, Karwatowska-Prokopczuk E, Baum SJ, Hurh E, Kingsbury J, Bartlett VJ, et al. Vupanorsen, an N-acetyl galactosamine-conjugated antisense drug to ANGPTL3 mRNA, lowers triglycerides and atherogenic lipoproteins in patients with diabetes, hepatic steatosis, and hypertriglyceridaemia. Eur Heart J. 2020;41:3936–45.
Graham MJ, Lee RG, Brandt TA, Tai LJ, Fu W, Peralta R, et al. Cardiovascular and Metabolic Effects of ANGPTL3 Antisense Oligonucleotides. N Engl J Med. 2017;377(3):222–32.
Raal FJ, Rosenson RS, Reeskamp LF, Hovingh GK, Kastelein JJP, Rubba P, et al. Evinacumab for Homozygous Familial Hypercholesterolemia. N Engl J Med. 2020;383(8):711–20.
Ahmad Z, Banerjee P, Hamon S, Chan KC, Bouzelmat A, Sasiela WJ, et al. Inhibition of Angiopoietin-Like Protein 3 With a Monoclonal Antibody Reduces Triglycerides in Hypertriglyceridemia. Circulation. 2019;140(6):470–86.
Rosenson RS, Burgess LJ, Ebenbichler CF, Baum SJ, Stroes ESG, Ali S, et al. Evinacumab in Patients with Refractory Hypercholesterolemia. N Engl J Med. 2020;383(24):2307–19.
Yamashita S, Masuda D, Matsuzawa Y. Pemafibrate, a New Selective PPARα Modulator: Drug Concept and Its Clinical Applications for Dyslipidemia and Metabolic Diseases. Curr Atheroscler Rep. 2020;22(1):5.
Ishibashi S, Yamashita S, Arai H, Araki E, Yokote K, Suganami H, et al. Effects of K-877, a novel selective PPARα modulator (SPPARMα), in dyslipidaemic patients: A randomized, double blind, active- and placebo-controlled, phase 2 trial. Atherosclerosis. 2016;249:36–43.
Yokote K, Yamashita S, Arai H, Araki E, Suganami H, Ishibashi S, et al. Long-Term Efficacy and Safety of Pemafibrate, a Novel Selective Peroxisome Proliferator-Activated Receptor-α Modulator (SPPARMα), in Dyslipidemic Patients with Renal Impairment. Int J Mol Sci. 2019;20(3). https://doi.org/10.3390/ijms20030706.
Pradhan AD, Paynter NP, Everett BM, Glynn RJ, Amarenco P, Elam M, et al. Rationale and design of the Pemafibrate to Reduce Cardiovascular Outcomes by Reducing Triglycerides in Patients with Diabetes (PROMINENT) study. Am Heart J. 2018;206:80–93.
Huang Z, Xu A, Cheung BMY. The Potential Role of Fibroblast Growth Factor 21 in Lipid Metabolism and Hypertension. Curr Hypertens Rep. 2017;19(4):28.
Schlein C, Talukdar S, Heine M, Fischer AW, Krott LM, Nilsson SK, et al. FGF21 Lowers Plasma Triglycerides by Accelerating Lipoprotein Catabolism in White and Brown Adipose Tissues. Cell Metab. 2016;23(3):441–53.
Gaich G, Chien JY, Fu H, Glass LC, Deeg MA, Holland WL, et al. The effects of LY2405319, an FGF21 analog, in obese human subjects with type 2 diabetes. Cell Metab. 2013;18(3):333–40.
Author information
Authors and Affiliations
Contributions
Both authors contributed equally to the data acquisition, drafting, and critical revision of the article.
Corresponding author
Ethics declarations
Conflicts of Interest/Competing Interests
Dr. Rosenson reports research funding to the institution from Amgen, Astra Zeneca Medicines Company, National Institutes of Health, Novartis, Regeneron, consulting fees from Amgen, Medicines Company, Novartis, Regeneron and 89 Bio, honoraria for non-promotional speaking fees from Amgen, Kowa and Regeneron, royalties from Wolters Kluwer (UpToDate) and stock holdings in MediMergent, LLC.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the Topical Collection: Translating genome medicine to treatments
Rights and permissions
About this article
Cite this article
Shaik, A., Rosenson, R.S. Genetics of Triglyceride-Rich Lipoproteins Guide Identification of Pharmacotherapy for Cardiovascular Risk Reduction. Cardiovasc Drugs Ther 35, 677–690 (2021). https://doi.org/10.1007/s10557-021-07168-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-021-07168-0