Abstract
Purpose
Previous studies have found that men with diabetes are at reduced risk of prostate cancer compared to men without diabetes. The lower risk could be due to biologic differences and/or a diagnosis bias from use of the prostate-specific antigen (PSA) test as a screening and diagnostic tool. We sought to further examine the relationship between diabetes and incidence of prostate cancer and examine the potential impact of changes in PSA screening guidelines in 2008 and 2012.
Methods
We used 2004–2015 Surveillance, Epidemiology and End Results (SEER)-Medicare data and limited the study population to men aged 67–74 with at least 2 years of continuous enrollment. Using the 5% Medicare sample as the denominator and prostate cancer cases as the numerator, we calculated age-adjusted rate ratios (RR) in 2006–2011 and 2012–2015 by diabetes status, overall and by tumor grade. We used multivariable logistic regression to compare tumor characteristics by diabetes status.
Results
Men with diabetes had lower incidence rates of prostate cancer compared to men without diabetes in 2006–2011 [RR = 0.89 95% confidence interval (CI) 0.87–0.91] and 2012–2015 (RR = 0.92 95% CI 0.89–0.95) but the slight attenuation toward the null in 2012–2015 was primarily due to the change in RRs for low-grade tumors.
Conclusion
We found differences in the risk and characteristics of prostate cancer by diabetes status and that some risks have changed over time as guidelines have changed. With lower PSA use in the more recent time-period, rates of low-grade tumors have become more similar by diabetes status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Previous studies have consistently found lower prostate cancer incidence rates among men with diabetes compared to men without [1,2,3,4,5,6,7,8,9]. The lower rates appear to be limited to low and intermediate-grade tumors, with less evidence of lower rates of high-grade tumors. Men with diabetes have been found to have lower levels of prostate-specific antigen (PSA) [10, 11], which could be an indicator of a biological and/or a detection bias between men with and without diabetes. For example, men with diabetes have been found to have lower androgen levels, such as testosterone, that could possibly slow or inhibit tumor growth [11,12,13]. It has also been suggested that lower PSA levels could contribute to lower rates from a detection bias due to the use of PSA testing being used as a screening test and initial diagnostic test for prostate cancer. The PSA test could potentially miss tumors in men with diabetes if PSA levels fall below those of comparable men with tumors but without diabetes.
In a previous analysis of the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial, we found evidence of detection bias leading to lower prostate cancer incidence rates in men with diabetes [14]. In men screened for prostate cancer with PSA tests at baseline and annually for the following 5 years, those with diabetes and diagnosed with low- or intermediate-grade prostate cancer tumors had a higher percentage of large tumors (TNM stage ≥ T3) and higher PSA levels at diagnosis. This provided indirect evidence that more small tumors were falling below the PSA level threshold for follow-up in men with diabetes. However, this result was not necessarily exclusive of a different biologic pathway.
Using 2004–2015 Surveillance, Epidemiology and End Results (SEER)-Medicare data, we sought to further examine the relationship between diabetes and prostate cancer and compare results from the screening trial to a general study population. In addition, because of changes in US Preventive Services Task Force (USPSTF) guidelines on PSA testing with corresponding changes in PSA test use [15, 16], we wanted to examine the results before and after changes in guidelines. In 2008, the USPSTF provided a recommendation against PSA screening (D rating) among men aged 75 years and older and an I (insufficient evidence) rating in younger men [17]. In 2012, the USPSTF guidelines changed to a recommendation against PSA screening for all ages [18]. Previous studies found decreases in prostate cancer incidence for men above and below age 75, primarily for early-stage disease, that coincided with decreases in PSA testing after 2008 and 2012 [16, 19]. Although beyond the years of the SEER-Medicare data used in this current analysis, the USPSTF changed the recommendation again in 2018 to a C rating for men aged 55 to 69, which recommends that men discuss the benefits and harms of screening before deciding on screening. However, a D rating for men aged 70 years and over remains [20].
We used SEER-Medicare data to estimate prostate cancer incidence rates by diabetes status and among those diagnosed with prostate cancer, compare tumor characteristics and PSA levels at diagnosis. We hypothesized that we would find lower incidence rates of low-grade prostate cancer in men with diabetes using this sample of the general population. The results from this analysis will contribute to the growing literature on diabetes and prostate cancer and can potentially help inform discussions on screening between patients with diabetes and their physicians.
Methods
Study population
More detail about SEER and the SEER-Medicare linkage can be found elsewhere [21]; however, 94% of persons aged 65 years or older in SEER have been linked to Medicare enrollment data. The SEER data were extracted from the 2018 data submission and included incident prostate cancer cases from 18 SEER cancer registries across the US between 2004 and 2015. SEER data include basic patient demographic information and characteristics about each primary cancer diagnosis, including date of diagnosis, tumor stage, and grade; for prostate cancer, it also includes PSA level. Among other information, the Medicare enrollment data indicate when beneficiaries were enrolled, their original and current reason for entitlement, and monthly indicators of entitlement type (e.g., Part A, Part B, etc.).
Prostate cancer cases
We limited the analysis to primary diagnoses of prostate cancer with no prior cancers. Cancers that were diagnosed through autopsy or death certificate only were excluded. In addition, beneficiaries were excluded if they were diagnosed with cancer in the same year as the first record of diabetes or prior to their first diabetes record.
Diabetes classification
We used the Chronic Conditions Flags (CCF) file developed by the Centers for Medicare and Medicaid Services (CMS) to determine diabetes status. The CCF file uses algorithms on the claims files to flag beneficiaries with 27 chronic conditions, including diabetes. The algorithm for diabetes searches for diabetes claims and diagnosis codes and the CCF includes the first occurrence of a claim for each beneficiary since their initial Medicare enrollment. Among participants of the National Health Interview Survey with a self-report of diabetes, in a linkage with Medicare data, the concordance for diabetes from the CCF was 93% [22].
Data analysis
We used the 5% Medicare sample files (with and without cancer) to establish a denominator for rates. These files include a 5% sample of all beneficiaries and their enrollment status over the time-period of our study. Beneficiaries were included in the denominator for each calendar year if they were aged 67–74 years with no previous cancer diagnosis, had at least 6 months of coverage in that year, had a total of 24 months of Part A and B coverage with no Medicare Advantage (Part C) during that time, and age 65 was their original reason for entitlement. The denominator was multiplied by 20 to estimate the full population for the SEER areas and provide more comparable rates to those observed from SEER data alone. Note that, the denominator includes the prostate cancer cases diagnosed in that particular calendar year and those diagnosed in future years.
To create the numerator for rates and compare tumor characteristics, we used the same restrictions on age (67–74 years), coverage type (Part A and B) and duration, and original reason for enrollment (age) as beneficiaries in the denominator.
Crude and age-adjusted rates (per 100,000) were calculated by year and for the time-periods 2006–2011 and 2012–2015 to coincide with the USPSTF change in 2012 for men aged < 75 years. Rates were age-adjusted to the male census population estimates for 2010. We calculated rate ratios (RR) and corresponding 95% confidence intervals (95% CI) to compare rates by diabetes status within each time-period. Rates were calculated overall and by tumor grade based on Gleason score [low-grade (2–6), intermediate-grade (7), high-grade (8–10)].
For comparison of tumor characteristics, we calculated Chi-squared tests and multivariable logistic regression to calculate the association between diabetes status and tumor size (TNM: T1, T2, T3–T4), PSA level at diagnosis (0–9.9 ng/ml, 10–19.9 mg/ml, ≥ 20 ng/ml), tumor grade and tumor stage based on SEER Summary Stage 2000 (local, regional, distant). Using multinomial, multivariable logistic regression, with the least advanced or least aggressive tumors as the reference category, we calculated the associations adjusting for the number of other chronic conditions (0, 1 ≥ 2), marital status (married, other/unknown), age group (67–69, 70–74 years), and race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, Asian/Pacific Islander, other/unknown). Covariates were chosen a priori. The other chronic conditions were based on the CCF and included chronic kidney disease, congestive heart failure, chronic obstructive pulmonary disease, hypertension, stroke, acute myocardial infarction, and ischemic heart disease. We used an interaction term to assess if there was a significant change in the odds ratio by diabetes status across time-periods.
To compare incidence rates with PSA test use over time, we used the 5% sample of beneficiaries without cancer to estimate the use of PSA testing in each year (diagnostic or screening) by diabetes status. In the Carrier and Outpatient files, we selected for claims of PSA testing that included a diagnosis code of V7644 or a HCPCS code of 84152, 84153, 84154 or G0103.
Results
There were 136,083 men aged 67–74 years with a first cancer diagnosis of the prostate between 2006 and 2015. Excluding men who were diagnosed with cancer before diabetes or within the same year (n = 16,720), did not have 24 months of prior Part B enrollment without Medicare Advantage (Part C) enrollment (n = 55,264), and whose original reason for entitlement was not age (n = 6,379), there were 57,720 men with prostate cancer in the study population. There were 17,517 (30.4%) with a record of diabetes and 40,072 (69.6%) without (Table 1). These men were included in the analysis comparing tumor characteristics and as the numerator for rates.
By age group, a significantly higher percentage of men with diabetes were 70–74 at prostate cancer diagnosis (67.5%) compared to men without diabetes (59.0%; Table 1). Men with diabetes were significantly more likely to be non-Hispanic black or Hispanic and have 1 or more comorbid conditions than men without. Approximately 59% (58.5%) of men with diabetes had a record of a PSA test in the 2 years prior to diagnosis (but excluding 6 months prior to diagnosis) compared to 48.6% of men without.
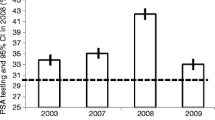
PSA testing
The percentage of men without diabetes who had a PSA test increased slightly from 36.5% in 2006 to 39.1% in 2011 but began to decrease in 2012 (Fig. 1). Usage was essentially parallel by diabetes status; however, men with diabetes had an approximately 9 to 10% points higher usage of PSA testing each year than men without diabetes. For example, in 2015 approximately 33% of men without diabetes had a PSA test compared to 42% of men with diabetes.
Incidence Rates
Overall incidence rates were lower among men with diabetes compared to men without in both time-periods: (2006–2011: RR = 0.89 95% CI 0.87–0.91; 2012–2015: RR = 0.92 95% CI 0.89–0.95) (Table 2). Although the RR in 2012–2015 was slightly attenuated toward the null compared to 2006–2011, the difference was not statistically significant (p value for interaction = 0.09). By grade, for low-grade disease, the change in RR’s from 2006–2011 (RR = 0.85 95% CI 0.82–0.88) to 2012–2015 (RR = 0.92 95% CI 0.87–0.97) was statistically significant (p = 0.009). Conversely, rates of high-grade disease were not significantly different by diabetes status in either time-period. Rates of intermediate-grade tumors were slightly lower in men with diabetes in both time-periods; (2006–2011: RR = 0.90 95% CI 0.87–0.94; 2012–2015: RR = 0.88 95% CI 0.84–0.92) but with little change (p = 0.50).
Annual incidence rates by diabetes status are presented overall and for low-grade tumors in Figs. 2 and 3. Overall incidence rates of prostate cancer were lower in men with diabetes compared to men without diabetes for the entire time-period (Fig. 2). However, the difference in rates decreased after 2008 as the rate among men without diabetes decreased more than in men with diabetes. The difference in rates by diabetes status between 2006 and 2011 appears to be primarily driven by rates of low-grade tumors and was largest between 2006 and 2008 (Fig. 3). Figures for intermediate- and high-grade tumors are available as supplemental figures (Supplemental Figs. 1 and 2).
Tumor characteristics
For tumor characteristics, men with diabetes had a higher percentage of T1 tumors and lower percentages of T2 and ≥ T3 tumors compared to men without diabetes in each time-period (Table 3). The percentage of tumors that were ≥ T3 increased in men with and without diabetes from 2006–2011 to 2012–2015, and the differences were similar by diabetes status across time-periods (p value for overall interaction = 0.17). Men with diabetes had a higher percentage of local stage tumors compared to men without diabetes in both time-periods. From 2006–2011 to 2012–2015, the odds of regional and distant staged tumors were attenuated toward the null for men with diabetes and the change was statistically significant between the two time-periods (p = 0.002). For example, men with diabetes had a 35% reduced odds of a distant staged tumor in 2006–2011 (aOR = 0.65 95% CI 0.57–0.75) and 20% reduced odds in 2012–2015 (aOR = 0.80 95% CI 0.69–0.93).
Men with diabetes had a slightly lower percentage of low-grade tumors diagnosed in 2006–2011 compared to men without diabetes; however, there was no difference in 2012–2015 (Table 3). In comparing adjusted odds ratios across time-periods, in 2006–2011, men with diabetes were slightly more likely to be diagnosed with high-grade tumors (aOR = 1.09 95% CI 1.02–1.17) while there was no difference in 2012–2015 (aOR = 0.99 95% CI 0.90–1.08; p = 0.02). From 2006–2011 to 2012–2015, there was an increased percentage of tumors diagnosed with PSA levels ≥ 10 ng/ml in men with and without diabetes. Although there was a significant interaction by time-period (p = 0.04), the changes were relatively small and the significant interaction seems primarily due to an attenuation toward the null for PSA levels ≥ 20 and away from the null for levels of 10–19.9.
Discussion
Using SEER-Medicare data, which provides a medical history for a large number of cancer cases in older men in the US, we found differences in the risk and characteristics of prostate cancer by diabetes status and that some risks differed over time. Consistent with our hypothesis, incidence rates were lower in men with diabetes than without; however, after the USPSTF change in 2008, overall and low-grade prostate cancer incidence rates decreased more among men without diabetes than men with diabetes. Unlike our analysis using the PLCO Screening Trial, which found men with diabetes had evidence of more advanced tumors at diagnosis, we found that men with diabetes were being diagnosed with smaller, less advanced tumors, consistent with more PSA testing. However, similar to the PLCO analysis, because of the lower rates of low-grade tumors in 2006–2011, men with diabetes were also diagnosed with a higher proportion of high-grade (i.e., more aggressive) tumors than men without diabetes but this difference disappeared in 2012–2015 coinciding with decreases in PSA testing.
The 8–11% lower overall rates of prostate cancer among men with diabetes over the two time-periods in this analysis were less than seen in previous longitudinal studies [10, 23]. However, those studies covered different time-periods with much larger age ranges compared to this analysis. One study included men aged 21–90 years in Israel between 2002 and 2012 and found a 20% lower rate among men with prevalent diabetes [10]. The other analysis included men from the Health Professionals Follow-up Study aged 40–74 years between 1986 and 2004 and found a 17% lower risk [23]. Conversely, in a cohort of Icelandic men aged > 50 years and followed through 2014, men with diabetes had a 59% increased risk of prostate cancer [24]. Because of the different study populations, time-periods, and screening programs, it is difficult to make fair comparisons between studies and the magnitude of results. For example, the prevalence of diabetes in the Icelandic population was low (2.7%) and there was no PSA screening program in the country. Even within the Health Professionals Follow-up Study, risks differed when stratified by time-period before and after widespread screening with PSA tests [23]. Although there is biologic plausibility for a reduced risk of prostate cancer in men with diabetes, the change in risks that coincides with differences in screening uptake and availability appears to indicate at least some role for PSA testing and detection bias in the difference in risks by diabetes status.
While we found PSA testing decreased slightly in the more recent years (2012–2015) for men regardless of diabetes status, testing was consistently about 9–10% points higher in men with diabetes. The higher testing could be indicative of greater interaction with health care providers but studies have been inconsistent when comparing uptake of prostate cancer screening by diabetes status [25]. It should be noted that we compared all PSA testing in this analysis, regardless if it was for screening or diagnostic purposes. With more PSA testing yet lower rates of cancer, this may also be evidence of a biologic difference in tumor development or production of PSA by diabetes status. If there was no difference in the development of tumors by diabetes status, we would expect higher levels of PSA testing to result in the detection of more low-grade tumors in men with diabetes, which was not the case. However, the smaller tumor sizes and localized tumors diagnosed in men with diabetes do not preclude the detection bias that was theorized from our previous analysis with the PLCO [14]. With a higher percentage of men with diabetes being screened for prostate cancer, it makes sense that they would have a higher proportion of smaller tumors diagnosed at an earlier stage than men without diabetes. Another possible explanation that we are unable to explore in this analysis is that men with diabetes may be less likely to be referred for biopsy or to follow-up after a referral. This has been observed in both US and Swedish cohorts [26, 27] and may be more likely to occur with low-grade tumors and lower PSA levels. The relationship between diabetes, PSA levels, screening and prostate cancer is complex and further study is still needed to tease apart the potential contributions of biologic differences and detection biases.
There are a number of potential explanations for the difference in results from the PLCO. In the PLCO, men in the screening arm were invited to be screened annually with approximately 91% of men having been screened at least 3 times during the first 6 study years and 76% screened at least 5 times [28]. The high compliance was useful for identifying a potential detection bias but was not representative of a real world situation. In the current analysis, we found a higher screening rate among men with diabetes compared to those without but we found that only about 60% of men with diabetes had a PSA test in the past 2 years.
With regards to the PSA test for prostate cancer screening, our findings that despite higher PSA test use, men with diabetes still had lower rates of low-grade disease before 2012 may indicate that the PSA test is a better screening test in men with diabetes. One of the main shortcomings of the PSA test as a screening tool is overdiagnosis and identifying tumors that would not have become symptomatic; these are typically low-grade tumors. If men with diabetes have fewer low-grade tumors diagnosed because of lower PSA levels and are diagnosed with a higher proportion of high-grade tumors, this could reduce overdiagnosis with the PSA test. A better understanding of the relationship between diabetes, prostate cancer, and PSA testing can help inform future guidelines and patient/physician discussions regarding screening. To address the question of overdiagnosis in men with diabetes, either a pooled analysis of screening trials is needed or studies will need to rely on modeling. However, because of considerable differences in the study populations of PSA screening trials available and different study designs, a pooled analysis might not be the most appropriate or generalizable to the US population.
As a check of our rates with the SEER-Medicare data, we used SEER 18 Registry data released in 2019 [29], and calculated rates for men aged 65–74 years from 2006 to 2015 and found comparable rates and a similar trend for overall rates. The benefit of the SEER-Medicare data is the ability to calculate the rates by diabetes status. There are few data sources available in which this is possible. Although we had previously calculated rates by diabetes status in the PLCO, it was important to compare results in the general population. Participants in the PLCO have been found to be healthier and have more education compared to the general population [30]. In addition, PSA screening was part of the trial, which affected the rates.
Although the SEER-Medicare data provide a better representation of the general population than the PLCO, our study was limited to men aged 67–74 years enrolled in Medicare fee-for-service. Beneficiaries enrolled in a Medicare Advantage (Part C) were not included because they do not have full claims available for analysis. During the time-period of this SEER-Medicare data (2004–2015), enrollment in Medicare Advantage (Part C) ranged from 16 to 31% [31]; therefore, our results may not be generalizable beyond this age group and/or to all Medicare beneficiaries. However, when we compared tumor characteristics between all prostate cancer cases aged 65–74 to those limited to the study population, results were comparable (results not shown).
Another limitation is that we did not have detail on the type or duration of diabetes in the men in this analysis, only date of first Medicare claim. We did not include men where the first diabetes claim and prostate cancer diagnosis occurred within the same year because studies have shown an increased risk of prostate cancer within a year of a diabetes diagnosis, presumably due to a surveillance bias and/or increased healthcare utilization. However, some but not all studies have found the risk of prostate cancer decreases with increasing time since diabetes diagnosis [25]. Without a date of diagnosis for diabetes, there may be differences by diabetes duration that this analysis did not capture. In addition, we can assume that the results are more generalizable to type II diabetes because of the greater prevalence, but it is unclear if the results would be similar for type I diabetes.
Previous analyses have found that the Chronic Condition Flags (CCF) file tends to overestimate the prevalence of diabetes in Medicare beneficiaries [22, 32]. Among beneficiaries aged 65–74 years with a CCF flag for diabetes, only 72% had self-reported diabetes in a linked self-report survey [22]. The false-positive results are potentially due to people with undiagnosed diabetes and/or more frequent monitoring of patients with pre-diabetes [32]. Although this could alter the magnitude of differences in our results, we feel the direction would likely underestimate the difference since the false-positive misclassification is among those categorized as having diabetes. The analysis was also unable to account for obesity as a potential risk factor and did not account for diabetes medications, such as insulin and Metformin. However, evidence of an association between obesity and prostate cancer and diabetes medications independent of diabetes has been weaker and inconsistent [25].
Overall, use of the large study population from SEER-Medicare allowed us to find differences in prostate cancer rates and characteristics by diabetes status and over time. While previous studies have compared the risk and characteristics of prostate cancer by diabetes status, this is the first that we know of to examine trends and potential changes in relation to the updated USPSTF guidelines in 2008 and 2012. Changes in the RRs since changes in USPSTF guidelines indicate the lower risk among men with diabetes is likely due to some type of detection bias. However, further understanding of the relationship between these diseases is needed to help guide screening recommendations and discussions.
Availability of data and material
Data available by request to SEER-Medicare.
References
Bansal D, Bhansali A, Kapil G, Undela K, Tiwari P (2013) Type 2 diabetes and risk of prostate cancer: a meta-analysis of observational studies. Prostate Cancer Prostatic Dis 16(2):151–158. https://doi.org/10.1038/pcan.2012.40
Bonovas S, Filioussi K, Tsantes A (2004) Diabetes mellitus and risk of prostate cancer: a meta-analysis. Diabetologia 47(6):1071–1078. https://doi.org/10.1007/s00125-004-1415-6
Fall K, Garmo H, Gudbjornsdottir S, Stattin P, Zethelius B (2013) Diabetes mellitus and prostate cancer risk; a nationwide case–control study within PCBaSe Sweden. Cancer Epidemiol Biomark Prev 22(6):1102–1109. https://doi.org/10.1158/1055-9965.EPI-12-1046
Haggstrom C, Van Hemelrijck M, Zethelius B, Robinson D, Grundmark B, Holmberg L et al (2016) Prospective study of Type 2 diabetes mellitus, anti-diabetic drugs and risk of prostate cancer. Int J Cancer. https://doi.org/10.1002/ijc.30480
Harding JL, Shaw JE, Peeters A, Cartensen B, Magliano DJ (2015) Cancer risk among people with type 1 and type 2 diabetes: disentangling true associations, detection bias, and reverse causation. Diabetes Care 38(4):264–270. https://doi.org/10.2337/dc15-er04a
Kasper JS, Giovannucci E (2006) A meta-analysis of diabetes mellitus and the risk of prostate cancer. Cancer Epidemiol Biomark Prev 15(11):2056–2062. https://doi.org/10.1158/1055-9965.EPI-06-0410
Liu X, Hemminki K, Forsti A, Sundquist K, Sundquist J, Ji J (2015) Cancer risk in patients with type 2 diabetes mellitus and their relatives. Int J Cancer 137(4):903–910. https://doi.org/10.1002/ijc.29440
Tsilidis KK, Allen NE, Appleby PN, Rohrmann S, Nothlings U, Arriola L et al (2015) Diabetes mellitus and risk of prostate cancer in the European Prospective Investigation into Cancer and Nutrition. Int J Cancer 136(2):372–381. https://doi.org/10.1002/ijc.28989
Zhu K, Lee IM, Sesso HD, Buring JE, Levine RS, Gaziano JM (2004) History of diabetes mellitus and risk of prostate cancer in physicians. Am J Epidemiol 159(10):978–982
Dankner R, Boffetta P, Keinan-Boker L, Balicer RD, Berlin A, Olmer L et al (2016) Diabetes, prostate cancer screening and risk of low- and high-grade prostate cancer: an 11 year historical population follow-up study of more than 1 million men. Diabetologia 59(8):1683–1691. https://doi.org/10.1007/s00125-016-3972-x
Peskoe SB, Joshu CE, Rohrmann S, McGlynn KA, Nyante SJ, Bradwin G et al (2015) Circulating total testosterone and PSA concentrations in a nationally representative sample of men without a diagnosis of prostate cancer. Prostate 75(11):1167–1176. https://doi.org/10.1002/pros.22998
Barrett-Connor E (1992) Lower endogenous androgen levels and dyslipidemia in men with non-insulin-dependent diabetes mellitus. Ann Intern Med 117(10):807–811
Betancourt-Albrecht M, Cunningham GR (2003) Hypogonadism and diabetes. Int J Impot Res 15(Suppl 4):S14–20. https://doi.org/10.1038/sj.ijir.3901031
Miller EA, Pinsky PF, Pierre-Victor D (2018) The relationship between diabetes, prostate-specific antigen screening tests, and prostate cancer. Cancer Causes Control 29(10):907–914. https://doi.org/10.1007/s10552-018-1067-3
Herget KA, Patel DP, Hanson HA, Sweeney C, Lowrance WT (2016) Recent decline in prostate cancer incidence in the United States, by age, stage, and Gleason score. Cancer Med 5(1):136–141. https://doi.org/10.1002/cam4.549
Negoita S, Feuer EJ, Mariotto A, Cronin KA, Petkov VI, Hussey SK et al (2018) Annual Report to the Nation on the Status of Cancer, part II: Recent changes in prostate cancer trends and disease characteristics. Cancer 124(13):2801–2814. https://doi.org/10.1002/cncr.31549
U. S. Preventive Services Task Force (2008) Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 149(3):185–191
Moyer VA, Force USPST (2012) Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 157(2):120–134. https://doi.org/10.7326/0003-4819-157-2-201207170-00459
Jemal A, Fedewa SA, Ma J, Siegel R, Lin CC, Brawley O et al (2015) Prostate cancer incidence and PSA testing patterns in relation to USPSTF screening recommendations. JAMA 314(19):2054–2061. https://doi.org/10.1001/jama.2015.14905
Force USPST, Grossman DC, Curry SJ, Owens DK, Bibbins-Domingo K, Caughey AB et al (2018) Screening for prostate cancer: US preventive services task force recommendation statement. JAMA 319(18):1901–1913. https://doi.org/10.1001/jama.2018.3710
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF (2002) Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care 40(8 Suppl):IV-3–IV-18. https://doi.org/10.1097/01.MLR.0000020942.47004.03
Day HR, Parker JD (2013) Self-report of diabetes and claims-based identification of diabetes among Medicare beneficiaries. Natl Health Stat Rep 69:1–14
Kasper JS, Liu Y, Giovannucci E (2009) Diabetes mellitus and risk of prostate cancer in the health professionals follow-up study. Int J Cancer 124(6):1398–1403. https://doi.org/10.1002/ijc.24044
Dickerman B, Mucci L (2019) Metabolic factors and prostate cancer risk. Clin Chem 65(1):42–44. https://doi.org/10.1373/clinchem.2018.287243
Pierce BL (2012) Why are diabetics at reduced risk for prostate cancer? A review of the epidemiologic evidence. Urol Oncol 30(5):735–743. https://doi.org/10.1016/j.urolonc.2012.07.008
Beckmann K, Crawley D, Nordstrom T, Aly M, Olsson H, Lantz A et al (2019) Association between antidiabetic medications and prostate-specific antigen levels and biopsy results. JAMA Netw Open 2(11):e1914689. https://doi.org/10.1001/jamanetworkopen.2019.14689
Leitzmann MF, Ahn J, Albanes D, Hsing AW, Schatzkin A, Chang SC et al (2008) Diabetes mellitus and prostate cancer risk in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Cancer Causes Control 19(10):1267–1276. https://doi.org/10.1007/s10552-008-9198-6
Pinsky PF, Black A, Kramer BS, Miller A, Prorok PC, Berg C (2010) Assessing contamination and compliance in the prostate component of the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial. Clin Trials 7(4):303–311. https://doi.org/10.1177/1740774510374091
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER 18 Regs Research Data + Hurricane Katrina Impacted Louisiana Cases, Nov 2018 Sub (2000–2016) <Katrina/Rita Population Adjustment>—Linked To County Attributes—Total U.S., 1969–2017 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2019, based on the November 2018 submission
Pinsky PF, Miller A, Kramer BS, Church T, Reding D, Prorok P et al (2007) Evidence of a healthy volunteer effect in the prostate, lung, colorectal, and ovarian cancer screening trial. Am J Epidemiol 165(8):874–881. https://doi.org/10.1093/aje/kwk075
Kaiser Family Foundation. Medicare Advantage Fact Sheet, June 2019. https://files.kff.org/attachment/Fact-Sheet-Medicare-Advantage. Accessed 13 Dec 2019
Sakshaug JW, Weir DR, Nicholas LH (2014) Identifying diabetics in Medicare claims and survey data: implications for health services research. BMC Health Serv Res 14:150. https://doi.org/10.1186/1472-6963-14-150
Acknowledgments
This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
Funding
None. Work carried out as regular duties as US Government employees.
Author information
Authors and Affiliations
Contributions
EAM: Conceptualization, methodology, formal analysis, writing—review and editing. PP: methodology, writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Miller, E.A., Pinsky, P.F. Examining the relationship between diabetes and prostate cancer through changes in screening guidelines. Cancer Causes Control 31, 1105–1113 (2020). https://doi.org/10.1007/s10552-020-01347-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-020-01347-4