Abstract
Objective
A history of diabetes has been fairly consistently related to a reduced prostate cancer risk, but previous investigations have not always addressed whether the relation with diabetes varies by prostate cancer aggressiveness or the association between diabetes and prostate cancer is modified by physical activity level and body mass, variables closely related to glucose metabolism.
Methods
We prospectively examined the diabetes–prostate cancer risk relationship among 33,088 men in the screening arm of the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial.
Results
During 8.9 years follow-up, we ascertained 2,058 incident prostate cancer cases. Diabetes history was related to decreased risk of total prostate cancer (RR = 0.80, 95% CI = 0.68–0.95). The apparent protection afforded by diabetes was primarily due to the inverse relation with non-aggressive disease (i.e., the combination of low grade (Gleason sum <8) and low stage (clinical stages I or II); RR = 0.75; 95% CI = 0.62–0.91). In contrast, no association was noted between diabetes and aggressive disease (i.e., high grade or high stage (Gleason sum ≥8 or clinical stages III or IV); RR = 1.04, 95% CI = 0.74–1.45). In further analyses, the association between diabetes and aggressive prostate cancer was suggestively positive for men who were lean (RR = 1.64, 95% CI = 0.87–3.07; BMI < 25 kg/m2) and it was positive for men who were the most physically active (RR = 1.63; 95% CI = 1.07–2.62; 3+ hours vigorous activity/week). By comparison, no relations of diabetes to aggressive prostate cancer were noted for their heavier or physically less active counterparts (p-value for tests of interaction = 0.10 and 0.03 BMI and physical activity, respectively).
Conclusion
In this study, diabetes showed divergent relations with prostate cancer by tumor aggressiveness. Specifically, diabetes was inversely associated with early stage prostate cancer but it showed no relation with aggressive prostate cancer. Exploratory analyses suggested a positive association between diabetes and aggressive prostate cancer in the subgroup of men with a low BMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a major source of morbidity in the United States (U.S.), where it has currently affected 10% of the population approximately [1]. The incidence of diabetes has increased markedly over time [1], tracking closely with increasing rates of adiposity [2], decreasing amounts of physical activity [3], and aging of the population. Rates of diabetes are anticipated to continue to rise both nationally and internationally [4].
Prostate cancer is the most commonly diagnosed non-cutaneous solid malignancy in U.S. men, where it ranks second in cancer-related mortality [5]. Despite the high incidence of prostate cancer, its etiology remains poorly understood [6]. Given the substantial incidence rates of both diabetes and prostate cancer, any relation of diabetes to the risk or severity of prostate cancer would have significant public health relevance.
We examined the association between history of diabetes and prostate cancer risk in the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Study. We sought to examine this relationship stratified according to body mass and physical activity, variables closely related to glucose metabolism. A further goal was to investigate whether the association between diabetes and prostate cancer varied by PSA level; the availability of comprehensive, prospective information on PSA concentration allowed us to assess the influence of prostate cancer screening on the relation of diabetes to prostate cancer.
Materials and methods
Study population
This study was conducted in the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial, a randomized controlled, multi-site study (Birmingham, AL; Denver, CO; Detroit, MI; Honolulu, HI; Marshfield, WI; Minneapolis, MN; Pittsburgh, PA; Salt Lake City, UT; St Louis, MO; and Washington, DC) designed to evaluate selected methods for the early detection of these four cancers [7]. Between 1993 and 2001, 38,350 men aged 55–74 years were randomized to the screening arm of the trial. These men received a prostate-specific antigen (PSA) test and a digital rectal exam (DRE) at study entry annually for three years, followed by two years of screening with PSA only. Men with a PSA test result of >4 ng/ml or DRE suspicious for prostate cancer were referred to their medical care providers for follow-up. In addition, each participant was asked to complete a baseline questionnaire and annual follow-up questionnaires regarding cancer diagnoses. The study was approved by the institutional review boards of the U.S. National Cancer Institute and the trial screening centers. Written informed consent was obtained from each study participant.
Out of 38,350 men who were randomly assigned to the screening arm of the trial, we excluded at baseline, men who reported a history of cancer other than non-melanoma skin cancer (n = 1,424); men without an initial PSA test or DRE (n = 2,470); men who received an initial screening examination but with whom there was no subsequent contact (n = 1,045); men who did not complete the baseline questionnaire (n = 898); men whose initial screening examination occurred after 30 September 2002, the censor date for the present analysis (n = 72); and men with missing values for history of diabetes (n = 1,302). After exclusions, the analytic cohort comprised 33,088 men (some participants were included in more than one exclusion category).
Identification of prostate cancer cases
For men with suspected prostate cancer or for those who reported prostate cancer on their annual questionnaire, we requested medical records to confirm the diagnosis and to obtain stage and grade information. We used death certificates, autopsy reports, and supporting medical/pathological records to confirm the information regarding diagnosis, stage, and grade for participants who were deceased. Clinical stage I and II tumors (stage I tumor = occult or incidental finding; stage II tumor = confined to prostate) with Gleason sum <8 were defined as non-aggressive. Clinical stage III and IV tumors (stage III tumor = localized to periprostatic area; stage IV tumor = metastatic disease) and/or tumors with biopsy Gleason sum ≥8 were considered aggressive. We also distinguished between high-grade disease (defined as Gleason sum ≥8) and high-stage disease (defined as stages III or IV). Out of 2,058 total cases, 1,239 (60%) were Gleason sum <7, 596 (29%) were Gleason sum = 7, and 189 (9%) were Gleason sum ≥8. The majority of cases (n = 1,746, 85%) were clinical stages I or II, and 307 cases (15%) were stages III or IV.
Because prostate cancers with Gleason 7 carry a greater risk of cancer progression than Gleason 2–6 tumors, we conducted subanalyses using two alternate levels of low-grade prostate tumors: Gleason ≤6 and Gleason = 7.
Data collection
Information on demographic and medical characteristics, anthropometry, and dietary intakes was collected using the baseline questionnaire. Participants provided information on whether they had been told by a doctor that they had any of 19 listed medical conditions, one of which was diabetes. The questionnaire did not differentiate between type 1 and type 2 diabetes. Approximately 95% of all diabetes cases are type 2 [1]; for the purpose of our analysis, we considered a report of diabetes on the questionnaire to be type 2 diabetes. Our study lacked data regarding the diagnosis date of diabetes. Information on history of diabetes based on self-report has shown excellent agreement (97%) with medical records [8]. We did not update information regarding newly diagnosed diabetes during the study time period. PSA measurements were performed at one central laboratory using a standard assay [9].
Data analysis
Person-years were calculated from the date of the baseline prostate cancer screen at study entry to the date of the most recently completed annual follow-up questionnaire, date of prostate cancer diagnosis, death, or 30 September 2002, whichever came first. We used Cox proportional hazards regression analysis to estimate relative risks (RRs) and 95% confidence intervals (CIs) of prostate cancer with age as the underlying time metric.
We adjusted for body mass index (BMI, <18.5, 18.5–24.9, 25–29.9, and 30 kg/m2 or more), race (Caucasian, African–American, Asian/Pacific Islander, and other), study center (10 categories), family history of prostate cancer (yes/no), smoking status (never, current, and former), attained education (<12 years, 12 years or high school, post high school or college, and college graduation or more), aspirin use (<4 per month, 1–6 per week, 1 per day, and 2+ per day), physical activity (0, 1, 2, 3, 4, and 5 h per week or more), and height (<170, 170–174.9, 175–179.9, 180–184.9, 185–189.9, and 190 cm or more). More rigorous adjustment for BMI (i.e., using a continuous BMI variable) or additional control for intakes of lycopene, selenium supplements, vitamin E, zinc, calcium, dairy products, red meat, dietary fat, and alcohol did not alter the RR estimates.
We examined whether the relation of diabetes to prostate cancer was modified by BMI (using categories of <25, 25–29.9, and 30 kg/m2) and physical activity (using categories of <1, 1–2, and 3+ hours per week). We also conducted an exploratory evaluation of the impact of prostate cancer screening on the relationship of diabetes to prostate cancer by running stratified analyses according to level of PSA at study entry (using categories of <4.0 and ≥4.0 ng/ml). We formally tested for interactions using log-likelihood ratio tests. All p-values were based on two-sided tests.
Results
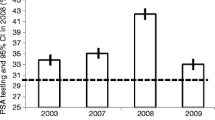
We examined baseline characteristics of the study population according to diabetes history to assess the potential for confounding (Table 1). Men with a history of diabetes were less likely to report a family history of prostate cancer, they were less educated, and they drank less alcohol than men without a history of diabetes. In contrast, men with a history of diabetes were heavier, more sedentary, and more likely to use aspirin than men without a history of diabetes. Men with and without a diabetes history were similarly likely at study entry to report having undergone a PSA test during the past three years or having a previous history of prostate biopsy. However, men with a history of diabetes had a 14% lower baseline PSA concentration than men without a history of diabetes. Although the number of screening examinations during the trial did not vary by history of diabetes, the probability of undergoing prostate biopsy following an abnormal PSA or DRE test during the trial was lower among men with diabetes than men without diabetes.
During 8.9 years follow-up of 33,088 men, 2,058 men were diagnosed with prostate cancer. In multivariate analysis, history of diabetes was associated with a statistically significant decreased risk of total prostate cancer (RR = 0.80, 95% CI = 0.68–0.95; Table 2). The apparent protection afforded by diabetes was primarily due to the inverse relations with low grade or low stage prostate cancer; the RR for non-aggressive disease (i.e., low grade and low stage) was 0.75 (95% CI = 0.62–0.91). In contrast, no association was noted between diabetes and aggressive disease (i.e., high grade or high stage; RR = 1.04, 95% CI = 0.74–1.45). Additional control for history of nocturia and history of BPH did not alter risk estimates (RR for non-aggressive disease = 0.73; 95% CI = 0.60–0.89; RR for aggressive disease = 0.99; 95% CI = 0.71–1.37). Results were similar when we excluded cases diagnosed during the first year of follow-up (RR for non-aggressive disease = 0.69; 95% CI = 0.55–0.88; RR for aggressive disease = 0.74; 95% CI = 0.44–1.24) or excluded cases diagnosed during the first three years of follow-up (RR for non-aggressive disease = 0.58; 95% CI = 0.40–0.83; RR for aggressive disease = 0.65; 95% CI = 0.30–1.43 based on 7 aggressive cases). Overall results for low-grade prostate cancer were similar when we used two alternative definitions of low-grade disease. The RR between diabetes and prostate cancers with Gleason sum ≤6 was 0.72 (95% CI = 0.57–0.90) and the RR between diabetes and prostate cancers with Gleason sum = 7 was 0.88 (95% CI = 0.65–1.18).
We examined whether the effect of diabetes on prostate cancer risk was modified by body mass and physical activity levels, variables closely related to glucose metabolism (Table 3). The inverse association between diabetes and non-aggressive prostate cancer was largely similar across subgroups of BMI, and the inverse relation of diabetes to non-aggressive prostate cancer was somewhat marked among men with low physical activity levels. However, formal tests for interaction revealed that those differences were not statistically significant (p-value for tests of interaction >0.05).
In contrast, the association between diabetes and aggressive prostate cancer was suggestively positive for men who were lean (RR = 1.64, 95% CI = 0.87–3.07; BMI < 25 kg/cm2) and it was positive for men who were the most physically active (RR = 1.63; 95% CI = 1.07–2.62; 3+ hours vigorous activity/week). By comparison, no relations of diabetes to aggressive prostate cancer were noted for their heavier or physically less active counterparts (p-value for tests of interaction = 0.10 and 0.03 BMI and physical activity, respectively).
We conducted an exploratory analysis restricting the sample to men who were PSA negative (<4.0 ng/ml) at study entry (Table 4). A marked inverse association between diabetes and total prostate cancer emerged (RR = 0.65, 95% CI = 0.51–0.83). In this subgroup analysis of PSA-negative men, the inverse relation between diabetes and total prostate cancer held for both non-aggressive disease (RR = 0.64, 95% CI = 0.49–0.83) and aggressive disease (RR = 0.72, 95% CI = 0.41–1.27); statistical power was low in the latter analysis due to small number of cases. In contrast, in the small subgroup of men who were PSA positive (≥4.0 ng/ml) at study entry, diabetes showed a weak positive association with total prostate cancer (RR = 1.27, 95% CI = 1.01–1.61). That relation was largely driven by the positive association with aggressive disease (RR = 1.76; 95% CI = 1.15–2.70), whereas the relation of diabetes to non-aggressive disease was null (RR = 1.12; 95% CI = 0.84–1.50). The observed positive relation with aggressive disease was largely determined by cases diagnosed within one year of the baseline screening examination (RR = 1.86, 95% CI = 1.15–3.01).
Discussion
The main result of the current study is that the history of diabetes was associated with a 20% decrease in risk of total prostate cancer. The apparent protection against prostate cancer afforded by diabetes appeared to be slightly stronger when we repeated our analyses using non-aggressive prostate cancer as the endpoint, showing a 25% decrease in risk. These findings are very similar to a recent meta-analysis that reported a 27% lower risk of prostate cancer among studies that were conducted in the post-PSA screening era [10].
In contrast to the inverse association between diabetes and total and non-aggressive prostate cancer observed in our study, we found no relation with diabetes when we repeated our analyses using aggressive prostate cancer as an alternative study outcome. In fact, when we addressed whether the relation of diabetes to aggressive prostate cancers varied by body mass and physical activity level, we noted a positive association with diabetes among men who were lean or physically active. Thus, our data suggest that diabetes is inversely related to the initiation or detection of prostate cancer, but has little association with prostate cancer progression overall and may have a positive relation to prostate cancer aggressiveness in the particular setting of a low fat mass.
Our finding of a positive relation of diabetes to aggressive prostate cancer in men with low fat mass is in agreement with data showing a positive association between serum insulin and predominantly advanced prostate cancer in a lean Chinese population [11, 12], and it is consistent with one investigation that noted a positive relation of fasting glucose to prostate cancer risk in a largely non-obese group of Icelandic men [13]. In contrast, a U.S. study found no overall association between serum insulin and prostate cancer but did observe a suggestive positive relation in the subgroup of men who were lean [14]. A low or intermediate (as opposed to high) fat mass, also associated with higher physical activity level, has been hypothesized to provide a hormonal milieu supportive of prostate cancer development, such as high levels of testosterone, growth hormone, insulin-like growth factor-1, leptin, and low levels of estrogen [15].
The possibility of an increased risk of aggressive disease among certain subgroups of men with diabetes is supported by data showing that men with a diagnosis of diabetes [16, 17] or those with elevated levels of post-load glucose [18] or insulin [19–21] have been found to present with prostate cancer at later stages or with higher Gleason scores at diagnosis [20, 21], to have increased prostate cancer recurrence [22, 23], and to have greater prostate cancer death [16, 18, 19] than men with normal glucose metabolism. That the adverse effect of diabetes is probably limited to aggressive forms of prostate cancer is consistent with studies showing that C-peptide and a homeostatic model assessment of insulin resistance (HOMA-IR) [24] and fasting glucose [23] are inversely related to non-aggressive prostate cancer but suggestively positively associated with aggressive disease.
It is worth pointing out that previous studies [25–29] examining the association between diabetes and aggressive prostate cancer either found no positive relation of diabetes to aggressive prostate cancer or reported a more pronounced inverse relation of diabetes to aggressive than non-aggressive prostate cancer. However, those studies [25–29] did not specifically evaluate the relation of diabetes to aggressive prostate cancer among lean or physically active men.
In our study, results from an exploratory analyses showed that diabetes was positively associated with total and aggressive prostate cancer among the subgroup of men who were PSA positive at baseline, particularly among cases diagnosed during the one-year interval following the baseline screening examination. This indicates that the baseline screening examination converted a greater proportion of previously undiagnosed prostate tumors to known aggressive prostate cancers among diabetic than non-diabetic men, a commonly observed phenomenon known as a lead time effect [30]. The most likely explanation for the drop-off in the association between diabetes and aggressive prostate cancer we observed after one year on study is culling of aggressive cancers in the first screening round and the overall less aggressive nature of cancers found on subsequent rounds of screening. A similar pattern of elevated prostate cancer risk during the time period immediately following the diagnosis of diabetes and a decline in risk associated with diabetes during the subsequent time period can be found in numerous previous studies [16, 25, 27, 31, 32].
Two recent surveys reported that PSA levels are about 20% lower among men with, as opposed to those without, diabetes, independent of age, race/ethnicity, and body mass [33, 34], consistent with results from our study. One possible mechanism involves lower circulating androgen levels in diabetic men [35], causing a decrease in PSA production via the androgen response element in the PSA promoter region [36]. Because results of PSA screening in conjunction with those from DRE largely determine who receives a biopsy, and biopsy is a major determinant of prostate cancer diagnosis, decreased serum PSA levels could plausibly be related to less prostate cancer detection among diabetic men. The lower PSA among diabetics apparently holds even in the face of a potentially counterbalancing tendency: diabetes is associated with prostatic enlargement [37–39], and PSA is positively correlated with prostate volume [9, 40, 41]. The prostate enlargement associated with diabetes may even enhance screening bias by rendering the detection of prostate cancer more difficult in diabetic men. Because prostate cancer typically involves only a small proportion of the total gland, and comparatively smaller tissue is collected from a large prostate than a small prostate at biopsy, the probability of sampling from the cancer site is decreased [42–46].
Any association between diabetes and prostate cancer would be spurious if prostate cancer diagnoses occurred less frequently among men who had diabetes coinciding with low PSA values and lower probability of prostate cancer detection. Most [28, 31, 47–70], but not all [16, 32] studies of diabetes and prostate cancer that were conducted before the use of PSA screening [28, 47–64] or studies that were carried out in countries without universal PSA screening [16, 31, 32, 65–70] found no association between diabetes and prostate cancer. In contrast, investigations that were conducted after the use of PSA screening fairly consistently reported an inverse association between diabetes and prostate cancer [25–27, 29, 71–74]. A recent meta-analysis reported a null association in studies conducted in the pre-PSA screening era (RR = 0.94; 95% CI = 0.85–1.03; diabetics versus non-diabetics), whereas an inverse relation was detected in studies conducted in the post-PSA screening era (RR = 0.73; 95% CI = 0.64–0.83) [10]. One possible reason for the observed heterogeneity in results between studies that were conducted in the pre-PSA versus post-PSA screening era is a true protective effect of diabetes on prostate cancer that was missed in studies in the pre-PSA screening era. An alternative explanation is detection bias in studies conducted in the post-PSA screening era.
It is noteworthy that studies conducted in the pre-PSA era may not be free of detection bias if the frequency of performing digital rectal examinations, the primary prostate cancer screening test during the pre-PSA era, differed between men with and without diabetes. Data regarding this possibility are sparse, but one study from the pre-PSA era noted that 65% of prostate cancers diagnosed among men with diabetes were first reported on a death certificate, compared to 47% for men without diabetes [56].
Our study has certain limitations. We lacked information on the diagnosis date of diabetes, but given the age range of study participants (55 to 74 years of age) and the mean age at diagnosis of diabetes among U.S. adults (46.7 years) [75], we estimate that the majority of study participants reporting the history of diabetes were probably diagnosed in excess of 10 years prior to entry. We were not able to determine whether the observed relations between diabetes and prostate cancer risk were explained by medications taken to treat diabetes rather than a biologic pathway associated with diabetes itself. We could not examine the relation of diabetes to prostate cancer among non-white men because our study lacked sufficient number of cases among non-white men.
In summary, this study confirms an inverse relation between diabetes and risk for total and non-aggressive prostate cancer. In contrast, we found no association between diabetes and aggressive prostate cancer overall, but we did note a positive relation of diabetes to aggressive prostate cancer among the subset of men who were lean or were physically highly active. These results add support to very limited available evidence of potential growth effects of diabetes and its metabolic sequelae on aggressive prostate cancers, an impact that appears to be amplified in the setting of a low body fat mass. We also present data from exploratory analyses, requiring confirmation, for a direct association between diabetes and aggressive prostate cancer among the very small group of men who were PSA-positive at study baseline. Whether this finding is in part due to underdiagnosis of early prostate cancers with aggressive potential among men with diabetes is speculative. Future studies may test the hypothesis that prostate cancer detection rates are lower among diabetics than non-diabetics and that low biopsy rates due to diminished PSA concentrations among diabetic men are one possible explanation. Should this possibility hold true, further work may clarify whether using a lower PSA concentration as the cut-point for triggering prostate biopsy in diabetics is justified. Additional research may also determine whether prostatic enlargement typically associated with diabetes potentially aggravates detection bias of prostate cancer among diabetic men. Such work should help further clarify the metabolic effects of diabetes on prostate cancer.
Abbreviations
- PLCO:
-
Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial
- PSA:
-
Prostate-specific antigen
- DRE:
-
Digital rectal exam
- RR:
-
Relative risk
- CI:
-
Confidence interval
References
Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM, Saydah SH, Williams DE, Geiss LS, Gregg EW (2006) Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health and Nutrition Examination Survey 1999–2002. Diabetes Care 29:1263–1268. doi:10.2337/dc06-0062
Flegal KM, Carroll MD, Ogden CL, Johnson CL (2002) Prevalence and trends in obesity among US adults, 1999–2000. JAMA 288:1723–1727. doi:10.1001/jama.288.14.1723
WHO (1995) Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 854:1–452
Yach D, Stuckler D, Brownell KD (2006) Epidemiologic and economic consequences of the global epidemics of obesity and diabetes. Nat Med 12:62–66. doi:10.1038/nm0106-62
American Cancer Society (2006) Cancer facts and figures 2006. American Cancer Society, Atlanta
Gronberg H (2003) Prostate cancer epidemiology. Lancet 361:859–864. doi:10.1016/S0140-6736(03)12713-4
Prorok PC, Andriole GL, Bresalier RS, Buys SS, Chia D, Crawford ED, Fogel R, Gelmann EP, Gilbert F, Hasson MA, Hayes RB, Johnson CC, Mandel JS, Oberman A, O’Brien B, Oken MM, Rafla S, Reding D, Rutt W, Weissfeld JL, Yokochi L, Gohagan JK (2000) Design of the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial. Control Clin Trials 21:273S–309S. doi:10.1016/S0197-2456(00)00098-2
Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ (2004) Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol 57:1096–1103. doi:10.1016/j.jclinepi.2004.04.005
Pinsky PF, Kramer BS, Crawford ED, Grubb RL, Urban DA, Andriole GL, Chia D, Levin DL, Gohagan JK (2006) Prostate volume and prostate-specific antigen levels in men enrolled in a large screening trial. Urology 68:352–356. doi:10.1016/j.urology.2006.02.026
Kasper JS, Giovannucci EA (2006) Meta-analysis of Diabetes Mellitus and the Risk of Prostate Cancer. Cancer Epidemiol Biomarkers Prev 15:2056–2062. doi:10.1158/1055-9965.EPI-06-0410
Hsing AW, Chua S Jr, Gao YT, Gentzschein E, Chang L, Deng J, Stanczyk FZ (2001) Prostate cancer risk and serum levels of insulin and leptin: a population-based study. J Natl Cancer Inst 93:783–789. doi:10.1093/jnci/93.10.783
Hsing AW, Gao YT, Chua S Jr, Deng J, Stanczyk FZ (2003) Insulin resistance and prostate cancer risk. J Natl Cancer Inst 95:67–71
Tulinius H, Sigfusson N, Sigvaldason H, Bjarnadottir K, Tryggvadottir L (1997) Risk factors for malignant diseases: a cohort study on a population of 22,946 Icelanders. Cancer Epidemiol Biomarkers Prev 6:863–873
Hubbard JS, Rohrmann S, Landis PK, Metter EJ, Muller DC, Andres R, Carter HB, Platz EA (2004) Association of prostate cancer risk with insulin, glucose, and anthropometry in the Baltimore longitudinal study of aging. Urology 63:253–258. doi:10.1016/j.urology.2003.09.060
Stattin P, Soderberg S, Hallmans G, Bylund A, Kaaks R, Stenman UH, Bergh A, Olsson T (2001) Leptin is associated with increased prostate cancer risk: a nested case-referent study. J Clin Endocrinol Metab 86:1341–1345. doi:10.1210/jc.86.3.1341
Weiderpass E, Ye W, Vainio H, Kaaks R, Adami HO (2002) Reduced risk of prostate cancer among patients with diabetes mellitus. Int J Cancer 102:258–261. doi:10.1002/ijc.10685
Chan JM, Latini DM, Cowan J, Duchane J, Carroll PR (2005) History of diabetes, clinical features of prostate cancer, and prostate cancer recurrence-data from CaPSURE (United States). Cancer Causes Control 16:789–797. doi:10.1007/s10552-005-3301-z
Gapstur SM, Gann PH, Colangelo LA, Barron-Simpson R, Kopp P, Dyer A, Liu K (2001) Postload plasma glucose concentration and 27-year prostate cancer mortality (United States). Cancer Causes Control 12:763–772. doi:10.1023/A:1011279907108
Hammarsten J, Hogstedt B (2005) Hyperinsulinaemia: a prospective risk factor for lethal clinical prostate cancer. Eur J Cancer 41:2887–2895. doi:10.1016/j.ejca.2005.09.003
Lehrer S, Diamond EJ, Stagger S, Stone NN, Stock RG (2002) Serum insulin level, disease stage, prostate specific antigen (PSA) and Gleason score in prostate cancer. Br J Cancer 87:726–728. doi:10.1038/sj.bjc.6600526
Hammarsten J, Hogstedt B (2004) Clinical, haemodynamic, anthropometric, metabolic and insulin profile of men with high-stage and high-grade clinical prostate cancer. Blood Press 13:47–55. doi:10.1080/08037050310025735
Lehrer S, Diamond EJ, Stagger S, Stone NN, Stock RG (2002) Increased serum insulin associated with increased risk of prostate cancer recurrence. Prostate 50:1–3. doi:10.1002/pros.10026
Jee SH, Ohrr H, Sull JW, Yun JE, Ji M, Samet JM (2005) Fasting serum glucose level and cancer risk in Korean men and women. JAMA 293:194–202. doi:10.1001/jama.293.2.194
Stocks T, Lukanova A, Rinaldi S, Biessy C, Dossus L, Lindahl B, Hallmans G, Kaaks R, Stattin P (2007) Insulin resistance is inversely related to prostate cancer: a prospective study in Northern Sweden. Int J Cancer 120:2678–2686. doi:10.1002/ijc.22587
Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Willett WC (1998) Diabetes mellitus and risk of prostate cancer (United States). Cancer Causes Control 9:3–9. doi:10.1023/A:1008822917449
Zhu K, Lee IM, Sesso HD, Buring JE, Levine RS, Gaziano JM (2004) History of diabetes mellitus and risk of prostate cancer in physicians. Am J Epidemiol 159:978–982. doi:10.1093/aje/kwh139
Rodriguez C, Patel AV, Mondul AM, Jacobs EJ, Thun MJ, Calle EE (2005) Diabetes and risk of prostate cancer in a prospective cohort of US men. Am J Epidemiol 161:147–152. doi:10.1093/aje/kwh334
Rosenberg DJ, Neugut AI, Ahsan H, Shea S (2002) Diabetes mellitus and the risk of prostate cancer. Cancer Invest 20:157–165. doi:10.1081/CNV-120001141
Calton BA, Chang SC, Wright ME, Kipnis V, Lawson K, Thompson FE, Subar AF, Mouw T, Campbell DS, Hurwitz P, Hollenbeck A, Schatzkin A, Leitzmann MF (2007) History of diabetes mellitus and subsequent prostate cancer risk in the NIH-AARP Diet and Health Study. Cancer Causes Control 18:493–503. doi:10.1007/s10552-007-0126-y
Rothman KJ, Greenland S (1998) Modern epidemiology, 2nd edn. Lippincott-Raven, Philadelphia
Tavani A, Gallus S, Bosetti C, Tzonou A, Lagiou P, Negri E, Trichopoulos D, La Vecchia C (2002) Diabetes and the risk of prostate cancer. Eur J Cancer Prev 11:125–128. doi:10.1097/00008469-200204000-00003
Adami HO, McLaughlin J, Ekbom A, Berne C, Silverman D, Hacker D, Persson I (1991) Cancer risk in patients with diabetes mellitus. Cancer Causes Control 2:307–314. doi:10.1007/BF00051670
Werny DM, Saraiya M, Gregg EW (2006) Prostate-specific antigen values in diabetic and nondiabetic US men, 2001–2002. Am J Epidemiol 164:978–983. doi:10.1093/aje/kwj311
Fowke JH, Motley SS, Cookson MS, Concepcion R, Chang SS, Wills ML, Smith JA Jr (2007) The association between body size, prostate volume and prostate-specific antigen. Prostate Cancer Prostatic Dis 10:137–142. doi:10.1038/sj.pcan.4500924
Svartberg J, Jenssen T, Sundsfjord J, Jorde R (2004) The associations of endogenous testosterone and sex hormone-binding globulin with glycosylated hemoglobin levels, in community dwelling men. The Tromso Study. Diabetes Metab 30:29–34. doi:10.1016/S1262-3636(07)70086-1
Riegman PH, Vlietstra RJ, van der Korput JA, Brinkmann AO, Trapman J (1991) The promoter of the prostate-specific antigen gene contains a functional androgen responsive element. Mol Endocrinol 5:1921–1930
Berger AP, Deibl M, Halpern EJ, Lechleitner M, Bektic J, Horninger W, Fritsche G, Steiner H, Pelzer A, Bartsch G, Frauscher F (2005) Vascular damage induced by type 2 diabetes mellitus as a risk factor for benign prostatic hyperplasia. Diabetologia 48:784–789. doi:10.1007/s00125-005-1678-6
Dahle SE, Chokkalingam AP, Gao YT, Deng J, Stanczyk FZ, Hsing AW (2002) Body size and serum levels of insulin and leptin in relation to the risk of benign prostatic hyperplasia. J Urol 168:599–604. doi:10.1016/S0022-5347(05)64687-3
Hammarsten J, Hogstedt B (2001) Hyperinsulinaemia as a risk factor for developing benign prostatic hyperplasia. Eur Urol 39:151–158. doi:10.1159/000052430
Bosch JL, Hop WC, Bangma CH, Kirkels WJ, Schroder FH (1995) Prostate specific antigen in a community-based sample of men without prostate cancer: correlations with prostate volume, age, body mass index, and symptoms of prostatism. Prostate 27:241–249. doi:10.1002/pros.2990270503
Collins GN, Lee RJ, McKelvie GB, Rogers AC, Hehir M (1993) Relationship between prostate specific antigen, prostate volume and age in the benign prostate. Br J Urol 71:445–450
Kulkarni GS, Al-Azab R, Lockwood G, Toi A, Evans A, Trachtenberg J, Jewett MA, Finelli A, Fleshner NE (2006) Evidence for a biopsy derived grade artifact among larger prostate glands. J Urol 175:505–509. doi:10.1016/S0022-5347(05)00236-3
Presti JC Jr, O’Dowd GJ, Miller MC, Mattu R, Veltri RW (2003) Extended peripheral zone biopsy schemes increase cancer detection rates and minimize variance in prostate specific antigen and age related cancer rates: results of a community multi-practice study. J Urol 169:125–129. doi:10.1016/S0022-5347(05)64051-7
Kranse R, Beemsterboer P, Rietbergen J, Habbema D, Hugosson J, Schroder FH (1999) Predictors for biopsy outcome in the European Randomized Study of Screening for Prostate Cancer (Rotterdam region). Prostate 39:316–322. doi:10.1002/(SICI)1097-0045(19990601)39:4≤316::AID-PROS14≥3.0.CO;2-O
Ung JO (2003) San Francisco, I. F., Regan, M. M., DeWolf, W. C., and Olumi, A. F. The relationship of prostate gland volume to extended needle biopsy on prostate cancer detection. J Urol 169:130–135. doi:10.1016/S0022-5347(05)64052-9
Stamey TA, Caldwell M, McNeal JE, Nolley R, Hemenez M, Downs J (2004) The prostate specific antigen era in the United States is over for prostate cancer: what happened in the last 20 years? J Urol 172:1297–1301. doi:10.1097/01.ju.0000139993.51181.5d
Glicksman AS, Rawson RW (1956) Diabetes and altered carbohydrate metabolism in patients with cancer. Cancer 9:1127–1134. doi:10.1002/1097-0142(195611/12)9:6≤1127::AID-CNCR2820090610≥3.0.CO;2-4
Checkoway H, DiFerdinando G, Hulka BS, Mickey DD (1987) Medical, life-style, and occupational risk factors for prostate cancer. Prostate 10:79–88. doi:10.1002/pros.2990100111
Henderson BE, Bogdanoff E, Gerkins VR, SooHoo J, Arthur M (1974) Evaluation of cancer risk factors in a retirement community. Cancer Res 34:1045–1048
Kessler II (1970) Cancer mortality among diabetics. J Natl Cancer Inst 44:673–686
Lancaster HO, Maddox JK (1958) Diabetic mortality in Australia. Australias Ann Med 7:145–150
O’Mara BA, Byers T, Schoenfeld E (1985) Diabetes mellitus and cancer risk: a multisite case-control study. J Chronic Dis 38:435–441. doi:10.1016/0021-9681(85)90139-0
Ragozzino M, Melton LJ 3rd (1982) Chu, C. P., and Palumbo, P. J. Subsequent cancer risk in the incidence cohort of Rochester, Minnesota, residents with diabetes mellitus. J Chronic Dis 35:13–19. doi:10.1016/0021-9681(82)90025-X
Steele JM, Sperling WL (1961) Relationship between diabetes mellitus and cancer. A study of the records for eight years at the Robert Packer Hospital. Guthrie Clin Bull 30:63–67
Steenland K, Nowlin S, Palu S (1995) Cancer incidence in the National Health and Nutrition Survey I. Follow-up data: diabetes, cholesterol, pulse and physical activity. Cancer Epidemiol Biomarkers Prev 4:807–811
Will JC, Vinicor F, Calle EE (1999) Is diabetes mellitus associated with prostate cancer incidence and survival? Epidemiology 10:313–318. doi:10.1097/00001648-199905000-00021
Wilson EB, Maher HC (1932) Cancer and tuberculosis with some comments on cancer and other diseases. Am J Cancer 16:227–250
Wynder EL, Mabuchi K, Whitmore WF Jr (1971) Epidemiology of cancer of the prostate. Cancer 28:344–360. doi:10.1002/1097-0142(197108)28:2≤344::AID-CNCR2820280214≥3.0.CO;2-#
Thompson MM, Garland C, Barrett-Connor E, Khaw KT, Friedlander NJ, Wingard DL (1989) Heart disease risk factors, diabetes, and prostatic cancer in an adult community. Am J Epidemiol 129:511–517
Levine W, Dyer AR, Shekelle RB, Schoenberger JA, Stamler J (1990) Post-load plasma glucose and cancer mortality in middle-aged men and women. 12-year follow-up findings of the Chicago Heart Association Detection Project in Industry. Am J Epidemiol 131:254–262
Batty GD, Shipley MJ, Marmot M, Smith GD (2004) Diabetes status and post-load plasma glucose concentration in relation to site-specific cancer mortality: findings from the original Whitehall study. Cancer Causes Control 15:873–881. doi:10.1007/s10552-004-1050-z
Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ (2004) Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol 159:1160–1167. doi:10.1093/aje/kwh161
Rousseau MC, Parent ME, Pollak MN, Siemiatycki J (2006) Diabetes mellitus and cancer risk in a population-based case-control study among men from Montreal, Canada. Int J Cancer 118:2105–2109. doi:10.1002/ijc.21600
Smith GD, Egger M, Shipley MJ, Marmot MG (1992) Post-challenge glucose concentration, impaired glucose tolerance, diabetes, and cancer mortality in men. Am J Epidemiol 136:1110–1114
Mishina T, Watanabe H, Araki H, Nakao M (1985) Epidemiological study of prostatic cancer by matched-pair analysis. Prostate 6:423–436. doi:10.1002/pros.2990060411
Hjalgrim H, Frisch M, Ekbom A, Kyvik KO, Melbye M, Green A (1997) Cancer and diabetes––a follow-up study of two population-based cohorts of diabetic patients. J Intern Med 241:471–475
Wideroff L, Gridley G, Mellemkjaer L, Chow WH, Linet M, Keehn S, Borch-Johnsen K, Olsen JH (1997) Cancer incidence in a population-based cohort of patients hospitalized with diabetes mellitus in Denmark. J Natl Cancer Inst 89:1360–1365. doi:10.1093/jnci/89.18.1360
Hsieh CC, Thanos A, Mitropoulos D, Deliveliotis C, Mantzoros CS, Trichopoulos D (1999) Risk factors for prostate cancer: a case-control study in Greece. Int J Cancer 80:699–703. doi:10.1002/(SICI)1097-0215(19990301)80:5≤699::AID-IJC12≥3.0.CO;2-7
Tavani A, Gallus S, Bertuzzi M, Dal Maso L, Zucchetto A, Negri E, Franceschi S, Ramazzotti V, Montella M, La Vecchia C (2005) Diabetes mellitus and the risk of prostate cancer in Italy. Eur Urol 47:313–317; discussion 317
La Vecchia C, Negri E, Franceschi S, D’Avanzo B, Boyle P (1994) A case-control study of diabetes mellitus and cancer risk. Br J Cancer 70:950–953
Coker AL, Sanderson M, Zheng W, Fadden MK (2004) Diabetes mellitus and prostate cancer risk among older men: population-based case-control study. Br J Cancer 90:2171–2175
Lightfoot N, Conlon M, Kreiger N, Sass-Kortsak A, Purdham J, Darlington G (2004) Medical history, sexual, and maturational factors and prostate cancer risk. Ann Epidemiol 14:655–662. doi:10.1016/j.annepidem.2003.11.006
Gonzalez-Perez A, Garcia Rodriguez LA (2005) Prostate cancer risk among men with diabetes mellitus (Spain). Cancer Causes Control 16:1055–1058. doi:10.1007/s10552-005-4705-5
Gong Z, Neuhouser ML, Goodman PJ, Albanes D, Chi C, Hsing AW, Lippman SM, Platz EA, Pollak MN, Thompson IM, Kristal AR (2006) Obesity, diabetes, and risk of prostate cancer: results from the prostate cancer prevention trial. Cancer Epidemiol Biomarkers Prev 15:1977–1983. doi:10.1158/1055-9965.EPI-06-0477
http://www.cdc.gov/diabetes/statistics/age. Accessed 4 April 2008
Acknowledgments
This research was supported by contracts from the Division of Cancer Prevention, National Cancer Institute, NIH, DHHS. The authors thank Drs. Christine Berg and Philip Prorok, Division of Cancer Prevention, National Cancer Institute, the Screening Center investigators and staff of the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial, Mr. Tom Riley and staff, Information Management Services, Inc., Ms. Barbara O’Brien and staff, Westat, Inc. Most importantly, we acknowledge the study participants for their contributions to making this study possible.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Leitzmann, M.F., Ahn, J., Albanes, D. et al. Diabetes mellitus and prostate cancer risk in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Cancer Causes Control 19, 1267–1276 (2008). https://doi.org/10.1007/s10552-008-9198-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-008-9198-6