Abstract
Purpose
Men with diabetes have been found to have a reduced risk of prostate cancer (PCa), potentially due to detection bias from lower prostate-specific antigen (PSA) levels or inhibition of tumor growth. Understanding if lower PCa rates are due to a lower risk of the disease or a detection bias from PSA testing can help inform the benefits and harms from prostate cancer screening.
Methods
We used data from the Prostate, Lung, Colorectal, and Ovarian (PLCO) Screening Trial to assess the impact of PSA screening on PCa in men with diabetes and the potential role of detection bias and/or slower tumor growth. Comparing men by diabetes status, we calculated age-adjusted incidence rates by tumor grade and compared screening results, PSA levels, and tumor characteristics.
Results
Men with diabetes had lower rates of PCa but was limited to low- and intermediate-grade tumors. Men with diabetes were less likely to be biopsied after their first positive screening test and men diagnosed with low/intermediate-grade tumors had significantly more advanced tumors with higher PSA levels.
Conclusions
Our findings provide additional evidence that detection bias is likely contributing to the lower rates of low- and intermediate-grade prostate cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Numerous studies have examined the relationship between diabetes and prostate cancer, demonstrating a reduced risk of prostate cancer among men with diabetes [1,2,3,4,5,6,7,8,9]. Studies have consistently found lower rates of low-grade tumors in men with diabetes compared to men without [4, 10,11,12,13]. Although inconsistent, there is some evidence that rates of high-grade tumors are lower, as well [10,11,12, 14]. Both biologic mechanisms and detection biases have been postulated as reasons for the lower rates of prostate cancer in men with diabetes. Men with diabetes have been found to have lower prostate-specific antigen (PSA) levels compared to men without diabetes, [10, 15] which may be attributed to lower androgen levels, such as testosterone [15,16,17]. The lower hormonal levels could potentially inhibit or slow tumor growth while lower PSA levels could also contribute to reduced detection of prostate cancer in men with diabetes [10, 18]. Studies have been unable to distinguish the factors that contribute to the lower prostate cancer rates.
The US Preventive Services Task Force (USPSTF) recently released a draft recommendation statement on prostate cancer screening that advises physicians and patients discuss the potential benefits and harms of screening [19]. For men with diabetes, understanding if lower prostate cancer rates are due to a lower risk of the disease or a detection bias from PSA testing can help inform the benefits and harms from prostate cancer screening. Further examining the rates, tumor characteristics, and corresponding PSA levels from a prostate cancer screening trial, could provide clues about the reasons for lower rates. For example, if we assume that tumor growth is similar by diabetes status, despite lower PSA levels in men with diabetes, then PSA testing would miss more tumors that fall below the typical threshold of 4 ng/ml (detection bias) in men with diabetes. In this case, because smaller tumors would be missed, we would expect to find a higher proportion of larger, more advanced tumors compared to men without diabetes (Fig. 1a). Alternatively, if we assume slower tumor growth in men with diabetes—with similar or lower PSA levels compared to tumors in men without diabetes—then we would expect to find a higher proportion or same proportion of smaller, less advanced tumors compared to men without diabetes (Fig. 1b).
a Assuming tumor growth is similar by diabetes status despite lower PSA levels in men with diabetes, if PSA testing misses more tumors that fall below the typical threshold of 4 ng/ml (detection bias), we would expect to find a higher proportion of larger, more advanced tumors compared to men without diabetes. b Assuming tumor growth is slower in men with diabetes, with similar or lower PSA levels, we would expect to find a higher proportion or same proportion of smaller, less advanced tumors than men without diabetes
The Prostate, Lung, Colorectal, and Ovarian (PLCO) Screening Trial provides an opportunity to assess the impact of prostate cancer screening on prostate cancer in men with diabetes and the potential role of detection bias and/or slower tumor growth. First, we examined if incidence rates of all tumor grades are lower in men with diabetes compared to those without. This expands on an earlier analysis of PLCO data [12] by including both study arms, longer follow-up times (maximum of 13 vs. 9 years of follow-up), and three categories of tumor grade vs. two. Secondly, we used the intervention arm of the trial to examine evidence of detection bias by comparing biopsy follow-up after a positive test, tumor stage, and PSA levels between men with and without diabetes.
Methods
The PLCO has been described more in-depth previously [20, 21]. The trial included men and women aged 55–74 years with no previous PLCO cancer or current cancer treatment who were enrolled between 1993 and 2001 from 10 cancer centers across the U.S. Over 76,000 men were randomized into an intervention arm (n = 38,340) or usual care arm (n = 38,345). Men in the intervention arm had PSA levels measured at baseline and then annually in the following 5 years. A positive test was defined as PSA level > 4 ng/ml, and these men were referred to their primary physician for follow-up. Men also underwent a digital rectal examination (DRE) at baseline and annually for the following 3 years.
All participants completed a baseline questionnaire detailing demographic characteristics, smoking history, family and personal history of cancer, and health characteristics. Diabetes was self-reported from the baseline questionnaire and did not differentiate between type I and type II diabetes. During the active screening period, a sample of men in the usual care arm completed a Health Status Questionnaire (HSQ), which included questions about screening tests to assess contamination. During the post-screening period, a sample of men from both arms completed the HSQ.
Men were excluded if they did not return their baseline questionnaire [n = 2,826 (3.7%)], did not have known diabetes status [n = 467 (0.6%)], or had any history of prostate cancer prior to randomization [n = 42 (0.05%)]. After exclusions, the study population included 73,349 men (6,672 with diabetes; 66,677 without diabetes). In the intervention arm, the population included 3,403 men with and 33,869 men without diabetes.
Cancer reporting and tumor characteristics
Cancers were identified either through annual study update forms completed by participants or through follow-up of positive screening tests. Prostate cancers that were only identified through death certificate or self-report without medical record confirmation were not included as cancers (n = 394). Trained medical abstractors reviewed medical records for medical procedures, diagnostic confirmation, and tumor characteristics, including histology, stage, and Gleason score. Biopsies were considered linked to a positive screening test if they occurred within a chain of diagnostic evaluations with no lapses > 9 months from the test.
Using TNM clinical stage, TNM T was categorized as T1–Tc, T2–T2c, ≥ T3. Tumor stage was also dichotomized as localized (stage I/II) or advanced disease (stage III/IV) based on combined clinical and pathologic stage. Tumor grade was based on Gleason score (GS) and categorized into low- (GS: 2–6), intermediate- (GS: 7), and high-grade (GS: 8–10) tumors. Gleason score was determined by prostatectomy, when available, or biopsy at the time of diagnosis. PSA levels were based on the most recent test result prior to diagnosis and were limited to test results within 90 days of diagnosis (approximately 87%) and for diagnostic purposes (i.e., not screening).
Statistical analysis
We compared participant characteristics and screening levels by diabetes status using chi-squared tests. Screening levels included the percent screened before the trial, during the active screening period [Time(T)0–T5], and during extended follow-up (T6–T13).
Using the full male study population, we calculated rates of prostate cancer by diabetes status overall and by study arm. Follow-up for incident prostate cancer was available through 31 December 2009 or 13 years of follow-up, whichever occurred first. We then calculated rates separately for low-, intermediate-, and high-grade tumors. We used Cox proportional hazards regression modeling to calculate hazard ratios comparing men with diabetes to those without, adjusting for age at baseline.
We first examined possible differences in positive PSA or DRE tests at each screening round among men in the intervention arm. Then we assessed follow-up after a first positive test by comparing receipt of a biopsy after a positive PSA test and/or DRE exam. Biopsies were assessed overall and by PSA level under 10 ng/ml (4–6.9 ng/ml and 7–10 ng/ml). To account for multiple tests with different combinations of screening results in the same person, we limited the analysis of biopsies linked to the first positive screening test (PSA and/or DRE). We measured the associations using unadjusted and multivariable logistic regression adjusting for age at baseline (55–59, 60–64, 65–69, 70–74 years), education level (< high school degree, less than college, at least some college), race (white non-Hispanic, black non-Hispanic, Hispanic, other races, and ethnicities), obesity [Body Mass Index (BMI) > 30 kg/m2], and number of other health conditions (≤ 1, ≥ 2; based on self-report of hypertension, coronary heart disease or myocardial infarction, stroke, emphysema, and chronic bronchitis).
We compared diagnostic PSA levels and tumor stage by diabetes status to assess potential evidence of detection bias. We again limited the study population to the intervention arm but only included men with prostate cancer and with a time of diagnosis during or within 1 year of the active screening period (T0–T5). We used this subpopulation because we were interested in the direct results of screening tests vs. the long-term impact on cancer diagnoses. This subpopulation included 2,027 men (141 with diabetes; 1,886 without diabetes). We compared geometric means of PSA levels by diabetes status using a t test and compared levels categorized as < 4, 4–9.9, and ≥ 10 ng/ml with a χ2 test.
Results
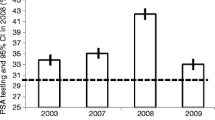
Overall, 9.1% of participants had diabetes at study baseline, with no difference in percentage by study arm (Table 1). Men with diabetes were older than men without diabetes, with approximately 45.3% aged 65 years and over compared to 35.8% among men without diabetes (p < 0.001). Men with diabetes were also more likely to be of other race/ethnicities than non-Hispanic white compared to men without diabetes. The prevalence of diabetes ranged from 8.2% in non-Hispanic white participants to 18.9% in non-Hispanic black participants (results not shown). Although the percentage of men with a family history of prostate cancer was significantly different by diabetes status, the absolute difference was small (1%). Men with diabetes were almost twice as likely to be obese (39.0%) compared to men without diabetes (21.8%; p < 0.001). When we compared screening levels by diabetes status, men with diabetes were slightly more likely to have had a DRE before the trial (61.8% vs. 57.8%; p < 0.001). During the active screening phase of the study, men with diabetes in the intervention arm were slightly less likely to have a PSA or DRE during the trial (PSA: 91.7% vs. 95.3%, p < 0.001; DRE: 90.9% vs. 94.8%, p < 0.001) than men without diabetes but the differences were modest. There was no significant difference in PSA or DRE testing during the active screening phase in the usual care arm or during the follow-up period for both arms combined.
Rates of all prostate cancers were lower in men with diabetes compared to men without, overall and by each study arm (Table 2). Overall, men with diabetes were approximately 26% less likely to be diagnosed with prostate cancer compared to men without (aRR = 0.74 95% CI 0.68–0.81). By tumor grade, the disparity in rates was greatest for low-grade tumors where men with diabetes were 36% less likely to be diagnosed with prostate cancer than men without diabetes (aRR = 0.64 95% CI 0.56–0.72). The association was attenuated but remained significantly lower for intermediate-grade tumors (aRR = 0.79 95% CI 0.68–0.91). Rates were not significantly different by diabetes status for high-grade tumors (aRR = 1.06 95% CI 0.85–1.31). We did not find large differences in relative risks for diabetes status by study arm.
We examined possible differences between positive screening tests at each interval and receipt of biopsy after a first positive test (PSA or DRE) as a contributor to the lower rates (Table 3). Men with diabetes had lower PSA positivity rates than men without diabetes. The lower rates were statistically significant for each screening round except baseline. However, in the multivariable logistic regression models, the positivity rates were significantly lower for all screens including baseline. For all PSA screens combined, men with diabetes had a 28% reduced odds of a positive test compared to men without diabetes. With respect to DRE, across all screening rounds, men with diabetes had a significantly lower screen positivity rate than men without diabetes. (aRR = 0.86 95% CI 0.77–0.95), though rates were not significantly different at any given round.
Among men with a positive screening test, men with diabetes (32.5%) were significantly less likely to have a biopsy linked to their first positive PSA test compared to men without diabetes [38.1%; OR 0.78 (95% CI 0.63–0.97)] (Table 3). However, after adjusting for age, education, race, obesity, and number of other health conditions, the association was no longer statistically significant (aOR = 0.86; 95% CI 0.69–1.07). When we examined biopsies after first positive test by PSA levels between 4 and 10, there was a significant association with PSA levels 4–6.9 ng/ml (aOR = 0.70 95% CI 0.54–0.89) but not 7–10 ng/ml (aOR = 1.06 95% CI 0.61–1.85). There was no association with having a biopsy by diabetes status after a positive DRE.
Finally, we compared tumor characteristics and PSA levels by diabetes status (Table 4). For prostate tumors overall, we found a significantly higher percentage of more advanced (TNM T ≥ T3) tumors in men with diabetes (5.7%) compared to those without (1.7%; p = 0.004) (Table 4). However, there was no difference in overall dichotomized (localized vs. advanced) stage. We did not find significant differences in mean or categorized PSA levels by diabetes status. Because we only found lower rates of prostate cancer in men with diabetes for low- and intermediate-grade tumors, we reran the analysis limited to those tumors. When limited to the low/intermediate-grade tumors, mean PSA levels at diagnosis were higher in men with diabetes (7.40) compared to those without (6.36; p = 0.04). Similarly, for categorized PSA levels, a higher percentage of men with diabetes had PSA levels ≥ 10 ng/ml (10.7%) compared to men without (5.0%; p = 0.04).
Discussion
In our analysis of PLCO data, we found evidence to support lower rates of low and intermediate grade but not high-grade prostate tumors in men with diabetes compared to those without. To explore evidence of detection bias or slower tumor growth contributing to the lower rates, we compared receipt of biopsies, tumor stage, and PSA levels. Men with diabetes were less likely to be biopsied after their first positive screening test and men diagnosed with low/intermediate-grade tumors had significantly more advanced tumors (based on TMN T stage) with higher PSA levels. Our finding provides evidence that detection bias is likely contributing to the lower rates of low- and intermediate-grade prostate cancers.
Previous studies have been conflicting about whether incidence rates of prostate cancer in men with diabetes are lower than in men without diabetes for all tumor grades or just low-grade tumors. For example, two studies using the Health Professionals Follow-up Study Cohort found an approximately 30% reduced risk of high-grade tumors, defined as GS 7–10, in men with diabetes compared to men without diabetes [11, 14]. However, a large prospective study using electronic health records in Israel did not find a significant reduction in risk for high-grade (GS 7–10) tumors (aRR = 0.92 95% CI 0.82–1.03) [10]. An earlier analysis of the intervention arm in the PLCO also did not find a significant reduction in high-grade (GS 8–10) tumors (unadjusted RR = 1.04 95% CI 0.74–1.45) but only had 16 high-grade cases in men with diabetes and was likely underpowered to detect a modest reduction in risk [12]. One possible reason for the inconsistent results could be the cut-off used to define high-grade tumors. In our analysis, we found that compared to men without diabetes, rates were significantly lower in men with diabetes and tumors with GS = 7 (intermediate grade) but not for those with GS = 8–10 (high grade). When we combined GS7–10, the reduced risk of prostate cancer was still significantly lower but attenuated towards the null (RR = 0.86 95% CI 0.76–0.97; results not shown). Previous studies have shown a survival advantage for tumors with grade 7 compared to 8–10, indicating a difference in tumor behavior, which could affect detection by screening [22]. Therefore, analyses combining GS 7 with 8–10 might distort the rate and be dependent on the distribution of tumors by grade present in the study.
Consistent with a detection bias related to lower PSA levels, men with diabetes were significantly less likely to have a positive PSA test, but not a positive DRE, at each screening round compared to men without diabetes. Better evidence of slower growing tumors would include men being less likely to test positive for both DRE and PSA tests. Although we found men with diabetes were less likely to have any positive DRE, the difference was modest and there was no clear pattern by screening round.
We were unable to determine the reason for men with diabetes being less likely to have a biopsy after a positive PSA test but this could potentially contribute to lower cancer rates in men with diabetes. Although likely to be a contributing factor, we are unable to assess if differences in health status contributed to the decision to not undergo a biopsy. However, controlling for other health conditions had little impact on the association. There may be other reasons for difference in care by diabetes status that we are unable to identify with the PLCO data.
Our finding of higher PSA levels and more advanced tumors at diagnosis in men with diabetes suggests that some smaller, less advanced tumors are preferentially not captured by PSA testing in men with diabetes. Although this does not rule out slower growing tumors contributing to lower rates, it provides stronger evidence of detection bias. However, it should be noted that if detection bias is occurring, it is unclear if this finding is detrimental to screening in men with diabetes. Because overdiagnosis of prostate cancer is a substantial concern in balancing the benefits and harms of screening for prostate cancer, missing these less advanced tumors could potentially be beneficial to this balance in men with diabetes. Unfortunately, this study is underpowered to estimate overdiagnosis and assess the effectiveness of screening in the subgroup of men with diabetes.
Our study had a number of limitations that could affect the results or conclusions of our analysis. Diabetes was based on self-report with no differentiation between type I and type II diabetes and we did not account for the duration of the disease nor treatments. Because we do not know what tumors were missed from screening, we can only indirectly assess detection bias as a factor for lower cancer rates. Additionally, because of substantial contamination of screening in the usual care arm, we are unable to assess the impact of PSA testing compared to an unscreened population.
Consistent with previous literature, we found that men with diabetes have lower rates of prostate cancer compared to men without diabetes but the lower rates were limited to low- and intermediate-grade tumors. While our study does not rule out the possibility of differences due to slower growing tumors in men with diabetes, it provides additional evidence that a detection bias contributes to the lower rates. It will be important to understand why men with diabetes are less likely to get appropriate follow-up treatment and if PSA testing impacts their balance of benefits and harms differently than men without diabetes. However, the results in this study can contribute to a better understanding of the relationship of screening and prostate cancer in men with diabetes and help better inform discussions.
Change history
30 November 2018
In the original publication of the article, the categories of PSA levels among the subpopulation of men diagnosed with prostate cancer were published incorrectly in Table 4. The corrected Table 4 is given in this Correction.
30 November 2018
In the original publication of the article, the categories of PSA levels among the subpopulation of men diagnosed with prostate cancer were published incorrectly in Table 4. The corrected Table 4 is given in this Correction.
References
Bonovas S, Filioussi K, Tsantes A (2004) Diabetes mellitus and risk of prostate cancer: a meta-analysis. Diabetologia 47(6):1071–1078
Kasper JS, Giovannucci E (2006) A meta-analysis of diabetes mellitus and the risk of prostate cancer. Cancer Epidemiol Biomarkers Prev 15(11):2056–2062
Bansal D, Bhansali A, Kapil G, Undela K, Tiwari P (2013) Type 2 diabetes and risk of prostate cancer: a meta-analysis of observational studies. Prostate Cancer Prostatic Dis 16(2):151–158
Fall K, Garmo H, Gudbjornsdottir S, Stattin P, Zethelius B (2013) Diabetes mellitus and prostate cancer risk; a nationwide case–control study within PCBaSe Sweden. Cancer Epidemiol Biomark Prev 22(6):1102–1109
Haggstrom C, Van Hemelrijck M, Zethelius B, Robinson D, Grundmark B, Holmberg L et al (2016) Prospective study of type 2 diabetes mellitus, anti-diabetic drugs and risk of prostate cancer. Int J Cancer 140:611–617
Harding JL, Shaw JE, Peeters A, Cartensen B, Magliano DJ (2015) Cancer risk among people with type 1 and type 2 diabetes: disentangling true associations, detection bias, and reverse causation. Diabetes Care 38(4):264–270
Liu X, Hemminki K, Forsti A, Sundquist K, Sundquist J, Ji J (2015) Cancer risk in patients with type 2 diabetes mellitus and their relatives. Int J Cancer 137(4):903–910
Tsilidis KK, Allen NE, Appleby PN, Rohrmann S, Nothlings U, Arriola L et al (2015) Diabetes mellitus and risk of prostate cancer in the European prospective investigation into cancer and nutrition. Int J Cancer 136(2):372–381
Zhu K, Lee IM, Sesso HD, Buring JE, Levine RS, Gaziano JM (2004) History of diabetes mellitus and risk of prostate cancer in physicians. Am J Epidemiol 159(10):978–982
Dankner R, Boffetta P, Keinan-Boker L, Balicer RD, Berlin A, Olmer L et al (2016) Diabetes, prostate cancer screening and risk of low- and high-grade prostate cancer: an 11 year historical population follow-up study of more than 1 million men. Diabetologia 59(8):1683–1691
Kasper JS, Liu Y, Giovannucci E (2009) Diabetes mellitus and risk of prostate cancer in the health professionals follow-up study. Int J Cancer 124(6):1398–1403
Leitzmann MF, Ahn J, Albanes D, Hsing AW, Schatzkin A, Chang SC et al (2008) Diabetes mellitus and prostate cancer risk in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Causes Control 19(10):1267–1276
Xu H, Jiang HW, Ding GX, Zhang H, Zhang LM, Mao SH et al (2013) Diabetes mellitus and prostate cancer risk of different grade or stage: a systematic review and meta-analysis. Diabetes Res Clin Pract 99(3):241–249
Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Willett WC (1998) Diabetes mellitus and risk of prostate cancer (United States). Cancer Causes Control 9(1):3–9
Peskoe SB, Joshu CE, Rohrmann S, McGlynn KA, Nyante SJ, Bradwin G et al (2015) Circulating total testosterone and PSA concentrations in a nationally representative sample of men without a diagnosis of prostate cancer. Prostate 75(11):1167–1176
Barrett-Connor E (1992) Lower endogenous androgen levels and dyslipidemia in men with non-insulin-dependent diabetes mellitus. Ann Intern Med 117(10):807–811
Betancourt-Albrecht M, Cunningham GR (2003) Hypogonadism and diabetes. Int J Impot Res 15(Suppl 4):S14–S20
Pierce BL (2012) Why are diabetics at reduced risk for prostate cancer? A review of the epidemiologic evidence. Urol Oncol 30(5):735–743
US Preventive Services Task Force (2017) U.S. Preventive Services Task Force seeks comments on draft recommendation statement on screening for Prostate Cancer. https://www.uspreventiveservicestaskforce.org/Home/GetFile/6/250/prostate-cancer-draft-bulletin/pdf
Grubb RL 3rd, Pinsky PF, Greenlee RT, Izmirlian G, Miller AB, Hickey TP et al (2008) Prostate cancer screening in the prostate, lung, colorectal and ovarian cancer screening trial: update on findings from the initial four rounds of screening in a randomized trial. BJU Int 102(11):1524–1530
Prorok PC, Andriole GL, Bresalier RS, Buys SS, Chia D, Crawford ED et al (2000) Design of the prostate, lung, colorectal and ovarian (PLCO) cancer screening trial. Control Clin Trials 21(6 Suppl):273S–309S
Rusthoven CG, Carlson JA, Waxweiler TV, Yeh, Raben D, Flaig TW et al (2014) The prognostic significance of Gleason scores in metastatic prostate cancer. Urol Oncol 32(5):707–713
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miller, E.A., Pinsky, P.F. & Pierre-Victor, D. The relationship between diabetes, prostate-specific antigen screening tests, and prostate cancer. Cancer Causes Control 29, 907–914 (2018). https://doi.org/10.1007/s10552-018-1067-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-018-1067-3