Abstract
Screening guidelines recommend that women with 20 % or greater lifetime risk of breast cancer undergo annual breast MRI screening to supplement mammography, irrespective of age. In patients less than 40 years, mammography is often avoided due to concerns about radiation and decreased performance. However, prior studies have been limited by large percentages of women above 40 with decreased breast density. Our purpose was to test whether adding mammography to breast MRI screening compared to breast MRI screening alone in women below 40 increases cancer detection rates. After obtaining IRB approval, chart review identified patients aged 25–40 years undergoing breast MR screening (2005–2014). Demographics, risk factors, BI-RADS assessments, background parenchymal enhancement, and mammographic breast tissue density were recorded. Cancer detection rates, short-term follow-up (BIRADS 3), image-guided biopsy (BIRADS 4,5), and PPV1–3 were calculated. 342 breast MRI exams were identified (average age was 33, 37 % were nulliparous, and 64 % had prior benign biopsy), 226 (66 %) of which underwent concurrent mammography. Risk factors included 64 % with breast cancer in first-degree relative(s), 90 % had heterogeneous or extremely dense breast tissue on mammography, and 16 % were BRCA carriers. Four invasive cancers were detected by MRI (11.7 cancers/1000 examinations, 95 % CI 8.3, 15.1). None of these was detected by mammography, and no cancers were independently identified by mammography. Breast MRI screening in high-risk women under 40 yielded elevated cancer detection rates (11.7/1000). The cancer detection rate for mammography was 0 %, suggesting that MRI alone may be useful in screening high-risk women under 40.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Screening guidelines recommend that women with a 20 % or greater lifetime risk of breast cancer undergo annual breast MR screening to supplement mammography [1]. In patients less than 40 years old who do not have a known germline mutation, however, mammography is often avoided to minimize radiation exposure [2] and because of decreased performance (secondary to increased breast parenchymal density) [3]. Nevertheless, prior studies and the American College of Radiology Appropriateness Criteria (ACR) have suggested that higher-risk women under 40 undergo screening with both breast MRI and mammography [4, 5]; however, prior studies comparing MR and mammography have been limited by study cohort populations which included large percentages of women greater than 40 years old as well as women with lower breast parenchymal density. The purpose of our study was to evaluate the hypothesis that screening with both mammography and breast MRI would not improve cancer detection rates compared to screening with breast MRI alone in women between 25–39 years old.
Materials and methods
To evaluate the main study hypothesis, we conducted a retrospective cohort study after obtaining IRB approval. The study was based in a tertiary care hospital located in an urban setting as well as nearby outpatient suburban satellite locations. Participants were identified using breast MRI procedure codes from radiology databases. The following inclusion criteria were used: women between the ages of 25–39 years who underwent screening breast MRI between 1/1/2005 and 6/30/2014 followed by at least 1 year of follow-up with the last date of clinical follow-up being 6/30/2015. Breast MRIs were considered as screening MRIs, if indication for examination was described as for screening and/or if clinical histories indicated that patients had risk factors for breast cancer which gave them a greater than 20 % lifetime risk of developing breast cancer. Women undergoing breast MRI for evaluation of symptomatic abnormalities (e.g., lump, focal breast pain, and discharge) were excluded. Women with histories of active breast cancer (actively undergoing cancer treatment or have undergone treatment within the last year) were also excluded, while women with more distant (>1 year) histories of cancer remained eligible for inclusion. Clinical histories and variable data for each patient were obtained from searching the electronic medical records.
Variables
Independent variable
The primary independent variable was the presence or absence of mammography performed within 7 months of screening breast MRI. The additional month takes into consideration women who are slightly late for their 6-month visit.
Outcome Variables
Primary outcome variables included cancer detection rate (numbers of cancers detected per year per 1000), abnormal interpretation proportions (BIRADS 0, 3, 4, and 5), short-term follow-up (BIRADS 3), image guided biopsy (BIRADS 4,5), sensitivities, specificities, and positive predictive values were calculated and compared in patients undergoing breast MRI screening with and without mammography. BIRADS diagnoses of all recorded lesions were dichotomized with categories 1 and 2 being considered negative and categories 0, 3, 4, and 5 being considered as positive. Positive histopathologic diagnoses included a diagnosis of invasive or ductal carcinoma in situ with all other benign breast histopathologies being considered negative (including lobular carcinoma in situ). Histopathologic diagnoses were dichotomized, in that a diagnosis of invasive or DCIS cancer was accepted as a malignant diagnosis or disease positive; all other histologic results including lobular carcinoma in situ were categorized as disease negative. In addition, an uneventful follow-up, based on any type of imaging or clinical follow-up at 12 months was accepted as disease negative.
Three positive predictive values were calculated. Positive predictive value 1 (PPV1) refers to the number of true positives/number of positive screening examinations, positive predictive value 2 (PPV2) refers to the number of true positives/number of screening or diagnostic examinations recommended for biopsy, and positive predictive value 3 (PPV3) refers to the number of true positives/number of biopsies.
Predictors, confounders and effect modifiers
Baseline demographics were obtained for each patient (age, race/ethnicity) at the time of first screening breast MRI. Additionally, known risk factors for breast cancer were collected including age at menarche, parity, number of children, age at birth of first child, history of prior breast biopsies, history of atypia or lobular carcinoma in situ, menopausal status, family history of breast or ovarian cancer (including first-degree relatives), BRCA status, oral contraceptive or hormonal therapy usage, alcohol usage, smoking status (current, former, and never), history of ovarian/uterine surgery, usage of chemoprevention, and history of breast cancer (greater than one year). As these variables may lead to the outcome (breast cancer) and may be associated with the exposure (presence or absence of screening mammography), these variables were considered as potential confounders. No variables were hypothesized a priori to be causal intermediates between the exposure (presence/absence of screening mammography) and the outcome (breast cancer), hence no variables were considered to be effect modifiers.
Statistical analysis
Linear and logistic regression analyses were utilized to compare baseline risk factors in patients undergoing breast MRI with and without mammography screening with random effects used to account for multiple screening rounds.
The primary outcomes (cancer detection rates and abnormal interpretation rates) were compared in breast MRI screening rounds with and without screening mammography using logistic regression with random effects models used to account for multiple screening rounds, unadjusted and adjusted for potential confounders. Means, medians, and standard deviations (SD) were reported for continuous outcomes with 95 % confidence intervals. As MRI BIRADS information was not available for only 1/342 patients (0.3 %), additional missing data analyses were not performed.
Sample size was based on comparing the estimated sensitivity of mammography in dense breasts (62 %) [6] to MRI (96 %) [7], yielding an estimated sample size of 19 in each group for 80 % statistical power. Two-sided p values less than 0.05 were considered to be statistically significant. STATA 11 was used to perform analyses (StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP).
Results
A total of 235 patients underwent 342 breast MRI exams of which 66.0 % (226/342) MRI examinations were performed with mammography within 7 months. Mean follow-up time was 1.7 years (median 1, SD 1.4, range 1.6, 1.9) (mean number of exams per patient of 1.455).
Baseline risk factors are described in Table 1 for the patients. At baseline, the mean age of patients was 33.0 years (n = 235, median 34, SD, 4.9, 95 % CI 32.4, 33.7) and 78.2 % of patients were white. Comparing screening rounds in which supplemental mammography was performed to screening rounds in which only screening breast MRI was performed, no statistically significant differences were found in baseline risk factors, except for oral contraceptive usage in which usage was lower in screening rounds in which screening breast MRI was performed without adjunct mammography (19.5 vs. 29.7 %, p = 0.049).
In terms of outcomes, the overall cancer detection rate for screening breast MRI in this cohort was 11.7 per 1000 (8.3, 15.1) (Table 2). Sensitivity was 100 % as no cancers developed on interval imaging or clinical follow-up or presented in between rounds of breast MRI screening with PPV1–3 ranging between 4.2 and 10.8%. Overall abnormal interpretation proportion (MR BIRADS of 0,3,4,5) was 27.9 % with 10.8 % of screening breast MRIs leading to biopsy (n = 341). Analysis of results by round of screening MRI (initial screening breast MRI exam versus subsequent screening breast MRI) found cancer detection rates of 27.5 cancers per subsequent screening round per 1000 (n = 107) compared with 4.3 cancers per initial screening round per 1000 (n = 235), a result which was close to the statistically significant one (p = 0.058) (Table 3). No differences were found in BIRADS distribution comparing initial vs subsequent screening rounds (p = 0.135) and percentage of screening MR examinations leading to biopsies (p = 0.187). Patients were more likely to undergo supplemental mammography (p = 0.022) and ultrasound examinations (p < 0.001) at initial screening rounds compared with subsequent screening rounds. No statistically significant differences were found in abnormal examination proportions comparing initial versus subsequent screening rounds (p = 0.158).
Four invasive cancers were detected by MRI (11.7 cancers detected per 1000 examinations, 95 % CI 8.3, 15.1). Of these four cancers, none of the lesions was detected on mammography (two were given BI-RADS ratings of two, and mammography was not performed for the other two cancers). Regarding the detected cancers, one cancer was a patient with a previous left breast invasive ductal cancer at the age of 29 treated with lumpectomy and radiation therapy and was found to have an ipsilateral recurrence on breast MRI (clumped ductal enhancement) with biopsy-proven ductal carcinoma in situ at age 37 and subsequently underwent mastectomy. Another case involved a 39 year old with a strong family history of breast cancer undergoing high-risk screening breast MRI. She was found to have suspicious nonmass enhancement in her right breast (without mammographic or ultrasound correlate) biopsied with large core needle technique and MRI guidance and found to be infiltrating ductal carcinoma, subsequently treated by lumpectomy (mammography localization of biopsy clip), radiation, and adjuvant chemotherapy. Additionally, a 39-year-old female with a BRCA one mutation and personal history of ovarian cancer was found to have new areas of nonmass enhancement in her right breast. The patient underwent bilateral mastectomies with pathology revealing an infiltrating mammary carcinoma with ductal and lobular features on the right corresponding to the MRI finding. Unfortunately, the patient went on to develop metastases from her ovarian cancer, which was treated with chemotherapy. Finally, a 38-year-old female with history of right breast invasive ductal carcinoma treated with lumpectomy, chemotherapy, and radiation followed by tamoxifen at the age of 35 underwent high screening breast MRI and was found to have new spiculated enhancing mass in the upper outer quadrant of her right breast ultrasound-guided biopsy proven to be infiltrating ductal carcinoma with lobular features. Patient subsequently underwent bilateral total mastectomy and unfortunately was diagnosed with diffuse metastases 7 months later and was subsequently treated with chemotherapy, and palliative brain and spinal radiation.
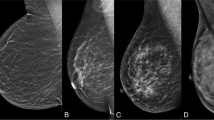
In the population, 64 % had mammography and MRI (219/342 screening rounds) at any time point with 66.5 % of mammography examinations having heterogeneously dense breast parenchymal density and 24.1 % of mammography examinations having extremely dense breast tissue (Table 4). 80.7 % (172/213) of mammography examinations had BIRADS 1 or 2. Of the remaining 41 mammography examinations with abnormal interpretations (BIRADS 0, 3,4, or 5), 9 led to biopsies, all of which were benign. For our primary analysis, no statistically significant differences were found in cancer detection rates (p = 0.483) and abnormal interpretation rates (p = 0.114) comparing rounds of screening breast MRI performed with and without mammography.
Conclusion
In our study, we found elevated incidence rates of breast cancer in high-risk women under 40 (11.7/1000) compared with general population-based SEER estimates of cancer incidence in women under 40 (0.6/1000), a 20-fold increase [8]. The results are consistent with prior literature on screening breast MRI in a wide variety of patient populations with elevated risks of developing breast cancer. In one of the few prospective cohort studies evaluating cancer detection by screening breast MRI in a cohort of women (mean age 44.6) with greater than 20 % lifetime risk of developing breast cancer (BRCAPRO model), Kuhl et al. found a cancer detection rate of 14.9/1000 using screening breast MRI alone [9], comparable to the 11.7/1000 rate found in our study. High-risk cohorts in women with histories of LCIS found cancer detection rates ranging between 16.3 and 17.9 cancers per 1000 screening examinations [10, 11]. Freitas et al. studied 98 women with prior histories of chest radiation therapy, in whom 12 cancers were detected by MRI screening (median latency from completion of radiation to detection of the breast cancer of 18 years) [12]. Kriege et al. studied 1952 women with a lifetime risk of developing breast cancer greater than 15 percent (mean age of 40) and found an overall cancer detection rate of 9.5 per 1000 screening exams with the highest rate in the subgroup of women with genetic mutations (26.5 cancers per 1000) [13]. Finally, Lehman et al. studied 1521 women (88.6 % who were greater than age 40) with personal histories of breast cancer undergoing screening breast MRI and found cancer detection rates of 19.7 per 1000 [14].
We found a cancer detection rate for supplemental mammography of 0 % with 90 % of mammograms demonstrating heterogeneous or extremely dense breast parenchymal density (known to limit mammographic sensitivity) suggesting that MRI alone may be useful in screening high-risk women under 40. The results are similar to the results from the prospective EVA trial by Kuhl et al. [9] in which the combination of screening mammography and MRI did not lead to statistically significantly increased cancer detection rates compared with MRI alone (p = 0.5). The only cancer not visible on MRI in this study was a case in a 52-year-old patient who was found to have calcifications which were biopsied, revealing low-grade DCIS. Studies comparing ultrasound to mammography in women under 40 have reached similar conclusions about the incremental benefits of mammography—Lehman et al. found high sensitivities (95.7 %) for ultrasound in symptomatic women with poor sensitivities for mammography (60.9 %), suggesting that adjunct mammography has limited benefits, likely secondary to elevated levels of breast parenchymal density [15]. Indeed in our study, we found that over 90 % of women under 40 had heterogeneously dense or extremely dense breast parenchymal density, likely contributing to the limited sensitivity of mammography in this setting.
Limitations of our study include reliance on retrospective data collection, data collection from a single institution, small numbers of detected cancers, and relatively low positive predictive values. Though prospective data collection would have enhanced our ability to more closely track baseline risk factors and improve our ability to ascertain outcomes, the results in our study regarding cancer detection rates and the lack of benefits of screening mammography in this age group are similar to previously described prospective cohort studies. Data collection from a single institution limits the generalizability of our study conclusions; however, we collected data from our outpatient sites in both urban and suburban locations. The small number of cancers we detected in our study (four) creates additional uncertainty regarding the true incidence of breast cancer in a high-risk cohort of women under 40. Nevertheless, our cancer detection rate (11.7/1000) is comparable to previously reported cancer detection rates with widely overlapping confidence intervals. Additionally, our cancer detection rate is comparable to the cancer detection rates in other previously reported high-risk cohorts. Finally, we note low positive predictive values in our cohort study (PPV3 of 10.8 %) of screening breast MRI. This is attributable to the bulk of our data collection occurring in an era at our institution in which the large majority of our breast MRIs were read by non-breast imagers. More recent results from dedicated breast imagers in our practice have yielded much higher positive predictive values(unpublished data). With higher positive predictive values and the development of abbreviated low-cost MR protocols [16, 17], these advancements suggest the possibility of increased dissemination of high-risk screening protocols in high-risk women below 40.
In conclusion, breast MRI screening in high-risk women under 40 yielded elevated cancer detection rates (11.7 per 1000) with no evidence of improvements in cancer detection rates by mammography. With a large majority of women under 40 demonstrating high levels of breast parenchymal density, the results suggest that MRI alone may be useful in screening high-risk women under 40. Our findings should be confirmed in future, multicenter prospective trial involving multiple institutions and larger numbers of patients.
References
Lee CH, Dershaw DD, Kopans D et al (2010) Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol 7(1):18–27
Berrington de Gonzalez A, Reeves G (2005) Mammographic screening before age 50 years in the UK: comparison of the radiation risks with the mortality benefits. Br J Cancer 93:590–596
Checka CM, Chun JE, Schnabel FR, Lee J, Toth H (2012) The relationship of mammographic density and age: implications for breast cancer screening. AJR Am J Roentgenol 198(3):W292–W295
Mainiero MB, Lourenco A, Mahoney MC et al (2013) ACR appropriateness criteria breast cancer screening. J Am Coll Radiol 10(1):11–14. doi:10.1016/j.jacr.2012.09.036
Warner E, Messersmith H, Causer P, Eisen A, Shumak R, Plewes D (2008) Systematic review: using magnetic resonance imaging to screen women at high risk for breast cancer. Ann Intern Med 148(9):671–679
Carney PA, Miglioretti DL, Yankaskas BC et al (2003) Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med 138(3):168–1675
Heywang-Köbrunner SH, Bick U, Bradley WG Jr et al (2001) International investigation of breast MRI: results of a multicentre study (11 sites) concerning diagnostic parameters for contrast-enhanced MRI based on 519 histopathologically correlated lesions. Eur Radiol 11(4):531–546
Howlader N, Noone AM, Krapcho M et al (eds) (2016). SEER cancer statistics review, 1975–2013, National Cancer Institute. Bethesda, MD http://seer.cancer.gov/csr/1975_2013/. based on November 2015 SEER data submission, posted to the SEER web site Accessed 15 June 2016
Kuhl C, Weigel S, Schrading S et al (2010) Prospective multicenter cohort study to refine management recommendations for women at elevated familial risk of breast cancer: the EVA trial. J Clin Oncol 28(9):1450–1457
Sung JS, Malak SF, Bajaj P, Alis R, Dershaw DD, Morris EA (2011) Screening breast MR imaging in women with a history of lobular carcinoma in situ. Radiology 261(2):414–420. doi:10.1148/radiol.11110091
Friedlander LC, Roth SO, Gavenonis SC (2011) Results of MR imaging screening for breast cancer in high-risk patients with lobular carcinoma in situ. Radiology 261(2):421–427. doi:10.1148/radiol.11103516
Freitas V, Scaranelo A, Menezes R, Kulkarni S, Hodgson D, Crystal P (2013) Added cancer yield of breast magnetic resonance imaging screening in women with a prior history of chest radiation therapy. Cancer 119(3):495–503. doi:10.1002/cncr.27771
Kriege M, Brekelmans CT, Boetes C et al (2004) Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. New Engl J Med 351(5):427–437
Lehman CD, Lee JM, DeMartini WB et al (2016) Screening MRI in women with a personal history of breast cancer. J Natl Cancer Inst. doi:10.1093/jnci/djv349
Lehman CD, Lee CI, Loving VA, Portillo MS, Peacock S, DeMartini WB (2012) Accuracy and value of breast ultrasound for primary imaging evaluation of symptomatic women 30-39 years of age. AJR Am J Roentgenol 199(5):1169–1177. doi:10.2214/AJR.12.8842
Harvey SC, Di Carlo PA, Lee B, Obadina E, Sippo D, Mullen L (2016) An Abbreviated Protocol for High-Risk Screening Breast MRI Saves Time and Resources. J Am Coll Radiol 13(4):374–380. doi:10.1016/j.jacr.2015.08.015
Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB (2014) Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection-a novel approach to breast cancer screening with MRI. J Clin Oncol 32(22):2304–2310. doi:10.1200/JCO.2013.52.5386
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Narayan, A.K., Visvanathan, K. & Harvey, S.C. Comparative effectiveness of breast MRI and mammography in screening young women with elevated risk of developing breast cancer: a retrospective cohort study . Breast Cancer Res Treat 158, 583–589 (2016). https://doi.org/10.1007/s10549-016-3912-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3912-y