Abstract
Purpose of review
To review the current evidence for the use of magnetic resonance imaging (MRI) as a supplemental breast cancer screening method for women with dense breast tissue and otherwise at average risk, and to answer whether the current evidence supports supplemental screening with breast MRI in this patient population.
Recent findings
The DENSE trial showed a statistically significant decrease in interval cancers with breast MRI screening vs. mammography alone and the EA1141 trial showed a statistically significant increase in cancer detection rate with abbreviated breast MRI compared to digital breast tomosynthesis (DBT). These trials provide evidence to support MRI as a supplemental breast cancer screening method in this population.
Summary
MRI screening has a high detection rate for breast cancer in women with dense breasts with otherwise average risk and is recommended to be considered a supplemental screening method by multiple organizations in the USA and Europe.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Increased breast density is a common concern for women undergoing breast cancer screening as it is associated with higher rates of breast cancer than those with average density breasts [1,2,3]. While mammography remains the gold standard for breast cancer screening, the sensitivity is more limited in women with dense breasts. Supplemental breast magnetic resonance imaging (MRI) screening has shown strong performance among high-risk women and is recommended as an adjunct to screening mammography for this group of women [4,5,6,7]. This review seeks to examine the evidence and review guidelines for MRI screening in women with dense breasts but otherwise at average risk for breast cancer.
Breast Density
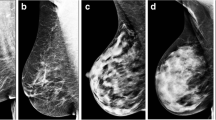
Breast density describes the relative proportion of fat and fibroglandular tissue contributing to the overall composition and imaging appearance of a patient’s breast tissue [8]. The Breast Imaging and Reporting Data System (BI-RADS) Fifth Edition lexicon defines four mammographic categories to standardize clinical reporting of breast composition: (a) The breasts are almost entirely fatty, (b) there are scattered areas of fibroglandular density, (c) the breasts are heterogeneously dense, which may obscure small masses, and (d) the breasts are extremely dense, which lowers the sensitivity of mammography [9]. Patients who fall into the latter two categories, c and d, are considered to have dense breasts (Fig. 1) [10•].
Examples of each category of breast density defined by the American College of Radiology Breast Imaging and Data Reporting System (BI-RADS) Fifth Edition: The breasts are almost entirely fatty (A); there are scattered areas of fibroglandular density (B); the breasts are heterogeneously dense, which may obscure small masses (C); the breasts are extremely dense, which lowers the sensitivity of mammography. Categories C and D are considered “dense”
Dense breasts pose a challenge in breast cancer screening as dense breast tissue can mask cancer on screening mammography, but increased breast density is also an independent risk factor for breast cancer [1]. The distribution of density categories a, b, c, and d within a general screening population has been estimated to be 10%, 40%, 40%, and 10%, respectively, with data from the Breast Cancer Surveillance Consortium finding the distribution in a general screening population of 922,624 women to be 9.0%, 44.2%, 38.2%, and 8.6%, further supporting these estimates [3, 11]. Thus, nearly half of women aged 40- to 74-years-old are estimated to have dense breasts [10•]. Women with “extremely dense” (category d) breasts have been shown to have a four to six times greater risk for breast cancer than women with fatty breasts (category a) [2]. Metanalysis examining breast density as an independent risk factor for breast cancer has shown that there seems to be an increased relative risk associated with breast density, 1.2 in women with heterogeneously dense breasts and 2.1 for breasts that were extremely dense as compared to women with average breast density [3]. Mammography is widely available and remains the mainstay of breast cancer screening, but there is an ongoing investigation into whether or not mammography alone for women with dense breasts is adequate for the detection of breast cancer as well as investigation into supplemental screening methods [12].
Furthering interest in the topic of breast cancer screening for women with dense breasts was the implementation of breast density notification laws. Beginning in 2009, individual states in the USA began implementing breast density notification laws, but there had not been a federally implemented requirement to notify patients of their breast density beyond inclusion in the mammogram report. In March 2023, the Food and Drug Administration issued a final rule amending regulations under the Mammography Quality Standards Act that establishes national reporting requirements that will go in effect September 10, 2024. The rule will require patients to be notified as to whether they have “dense” or “not dense” breast tissue along with one of two breast density notification statements. For those with dense breasts, the notification statement reads “Dense tissue makes it harder to find breast cancer on a mammogram and also raises the risk of developing breast cancer. Your breast tissue is dense. In some people with dense tissue, other imaging tests in addition to a mammogram may help find cancers” [13, 14]. Breast density notification laws have not been implemented outside of the USA [15]. Due to the increasing evidence regarding the limitations of mammography in the screening of breast cancer in women with dense breasts and the increasing public awareness of the implications of this limitation on breast cancer detection, interest in developing robust supplemental screening methods beyond mammography has grown.
Mammography has been demonstrated to result in a significant reduction in breast cancer mortality of approximately 40% and remains the most effective screening method widely available [16, 17]. With the transition from screen-film mammography to full field digital mammography, the Breast Cancer Surveillance Consortium updated its performance benchmarks for breast cancer screening with digital mammography including cancer detection rate, sensitivity, specificity, and false negative rate. After analysis of over 1.6 million screening mammographic examinations, they found the cancer detection rate to be 5.1 per 1000 screenings, sensitivity of 86.9%, specificity of 88.9%, and a false negative rate of 0.8 per 1000 screenings. Seventeen other trials have demonstrated decreasing sensitivity of mammography with increasing breast density, ranging from 85.6 to 88.2% in women with “almost entirely fatty” breasts to 62.2 to 68.1% in women with “extremely dense” breasts [3, 18]. Sensitivity of mammography in the highest risk patients with dense breasts has been reported to be as low as 19–37% [19,20,21,22,23].
Digital breast tomosynthesis (DBT) is an advanced type of mammography that uses multiple low-dose images obtained at different angles as the X-ray source moves over the breast, reducing the effects of superimposition [24]. The use of DBT for routine mammography continues to increase and has been reimbursed in the USA for women of all breast densities since 2015 [25]. While DBT has been shown to increase cancer detection rates as compared to full field digital mammography and reduce false-positive recalls for additional imaging, it is a mammographic and not a functional imaging technique, and limits to its performance remain, especially in women with extremely dense breasts [24, 26].
Investigations into complimentary modalities to supplement mammography for patients with dense breasts who are not otherwise at elevated risk for breast cancer are underway due to both the increased risk for breast cancer development and the decreased sensitivity of mammography. Recent studies support the use of breast MRI as a supplemental screening tool in the setting of increased breast density alone, with a high cancer detection rate and high positive predictive value for biopsy similar to mammography [27, 28]. Discussion of breast MRI as a supplemental screening method for women with dense breasts but otherwise at average risk for breast cancer will be the focus of this review.
Breast MRI Technique
Dynamic contrast-enhanced (DCE) breast MRI is performed with multiple imaging sequences both before and after administration of a gadolinium-based contrast agent (“contrast”). Although there is strong interest and ongoing research in developing a non-contrast breast MRI examination for screening, currently, evaluation for cancer using MRI requires intravenous contrast. Patients are positioned prone with the breasts hanging dependently within a dedicated breast coil and stabilized, but not compressed. Images are obtained on an MRI scanner with a field strength of at least 1.5 Tesla [29]. The most important portion of the breast MRI exam for lesion detection is the DCE sequences, including the pre- and multiple post-contrast T1-weighted images. T2-weighted and T1-weighted imaging without fat suppression (often obtained if the pre- and post-contrast images are obtained with fat suppression) ± diffusion-weighted imaging assist with lesion evaluation [29]. After the exam is completed, subtraction images of the peak post-contrast minus the pre-contrast T1 images, 3D maximum intensity projection (MIP) of the peak subtraction, and multiplanar reformats are often performed to assist with interpretation. Images are commonly obtained in the axial plane to assist with comparison between the two breasts. Examination time is typically less than 30 min on modern scanners. Although body mass index (BMI) can be limiting as the patient needs to fit in the bore of the MRI scanner while positioned prone on the breast coil, the use of wide-bore (70 cm) scanners has significantly reduced this limitation, and it is rare in our practice for a patient to be unable to obtain breast MRI due to weight or body habitus limitations.
Although breast MRI is the most powerful tool for the detection of breast cancer, standard full protocols can be expensive, time intensive, and more complicated to interpret. Abbreviated breast MRI to mitigate these limitations was initially proposed by Dr. Kuhl and colleagues in 2014 [30]. They limited interpretation to the pre- and early post-contrast T1-weighted series (total 3 min of scan time) and subtraction/MIP reconstructions and found equivalent performance compared with a traditional full MRI protocol as described above. Since that time, several studies evaluating full protocol breast MRI and abbreviated breast MRI for screening have shown them to have a similar sensitivity and cancer detection rate [27, 31, 32]. There is no single definition of an abbreviated MRI exam, but many include a 3-plane localizer, T2-weighted series, pre- and single post-contrast T1-weighted series and are performed in 10 min or less [28]. This is consistent with the design of the Eastern Cancer Oncology Group (ECOG)–American College of Radiology Imaging Network (ACRIN) 1141 trial described in further detail below [33•]. The shortened scan time allows for higher patient throughput, improved patient comfort, reduced interpretation time, and reduced cost, potentially extending the benefits of screening breast MRI to broader patient populations, including those with dense breasts [28, 31].
High-quality breast MRI performance requires expert readers, high-quality MRI scanners, dedicated breast coils, routine evaluation of performance, and thoughtful, high-resolution protocol creation. High-quality imaging and breast MRI performance are supported by the American College of Radiology Breast MRI accreditation program and other accreditation programs such as the National Accreditation Program for Breast Centers (NAPBC) [34, 35].
Breast MRI Diagnostic Performance
MRI is widely accepted as the most sensitive imaging modality for the detection of breast cancer [29, 31]. Multiple trials have demonstrated a high incremental cancer detection rate, i.e., additional cancers detected beyond mammography, when MRI is used for screening patients at elevated risk for breast cancer. Breast MRI is recommended as a supplemental screening method in patients with a lifetime risk for breast cancer > 20%, including those with a known genetic mutation increasing the likelihood of developing breast cancer, a strong family history of breast cancer, and a history of radiation therapy to the chest, as supported by the American College of Radiology (ACR), Society of Breast Imaging (SBI), American Cancer Society (ACS), American Society of Breast Surgeons (ASBrS), and National Comprehensive Cancer Network (NCCN) [4, 5, 16, 36, 37]. These recommendations are independent of breast density, i.e., all patients that meet the guidelines are recommended to have annual breast MRI regardless of their breast density.
However, mounting evidence shows that supplemental screening with breast MRI, including abbreviated breast MRI, increases cancer detection rates and lowers the interval cancer rates vs. screening mammography alone in women with dense breasts [33•, 38•, 39•]
DENSE Trial
The Dense Tissue and Early Breast Neoplasm Screening (DENSE) trial is a randomized, controlled multicenter trial designed to study the effect of supplemental screening with MRI on the incidence of interval cancers in women with extremely dense breasts [38•]. Patients were eligible to enroll if they were taking part in the Dutch population-based mammography screening program (ages 50–75), had normal results on mammography, and were found to have extremely dense breast tissue. The Dutch population–based mammography screening program includes biennial screening mammography. Breast density was determined as measured by Volpara imaging software (Volpara Health Technologies) density grade “d” [38•].
A total of 40,373 women were randomly assigned in a 1:4 ratio to either a group invited to undergo supplemental MRI screening (8061 women) or a group assigned to screening with mammography only (32,312 women). MRI exams in the DENSE trial were full protocol (not abbreviated) studies. Median age of participants was 54 years at the time of recruitment. Of those invited for supplemental MRI screening, only 4783 (59.3%) women underwent the supplemental MRI screening in this intention-to-treat analysis. Supplemental MRI screening took place biennially after the regular screening mammogram. The intervention is planned for a total of 6 years consisting of 3 screening rounds. To date, the results of the first two screening rounds have been reported [38•].
The primary outcome of the initial prevalence round of screening was to assess the difference in the incidence of interval cancer rates between the group invited to undergo supplemental MRI screening and the group undergoing screening with mammography only. Secondary outcomes of the prevalence round of screening included recall rate, cancer detection rate, false-positive rate, positive predictive value, and differences in tumor characteristics for cancers identified in either group. Primary outcomes of the incidence round of screening included recall rate, cancer detection rate, false-positive rate, positive predictive value, and differences in tumor characteristics [38•].
Analysis of the interval cancer rate following the prevalence round of screening showed a statistically significant decrease in the interval cancer rate by 2.5 per 1000 screenings (2.5 per 1000 vs. 5.0 per 1000; p < 0.001) within the MRI invitation group compared to the mammography only group. Of the 20 patients with cancer identified in the MRI invitation group, only 4 actually underwent breast MRI. Overall, the cancer detection rate (CDR) for MRI performed was 16.5 per 1000 screenings with a positive predictive value (PPV) for recall of 17.4% and PPV for biopsy performed of 26.3% PPV (79 cancers among 300 women undergoing biopsy). The recall rate was 94.9 per 1000 screenings. The false-positive rate for MRI was found to be 79.8 per 1000 screenings (92% specificity) with a sensitivity of 95.2%. In the MRI screening group, the CDR at the next mammography screening was 2.0 per 1000, compared with 7.1 per 1000 among the MRI non-participants and 6.0 per 1000 in the mammography-only group. The detected cancers on MRI were smaller, with a higher incidence of early stage and node-negative cancers [39•].
Following the incidence round, the cancer detection rate for MRI was found to be 5.8 per 1000 screenings and the recall rate to be 32.0 per 1000 screenings. The false-positive rate for MRI declined to 26.3 per 1000 screenings (97% specificity). The detected cancers in the incidence round were all early stage (Stage 0–1) and were node negative. The decrease in the cancer detection rate between the prevalence and incidence rounds is expected as there would be a greater number of cancers not detected on mammography alone in the prevalence round that are no longer present on subsequent incident rounds of screening. The decrease in the false-positive rate for MRI is also expected due to the availability of a comparison MRI examination [38•].
EA1141 ECOG-ACRIN Trial
The EA1141 trial, “Comparison of Abbreviated Breast MRI and Digital Breast Tomosynthesis in Breast Cancer Screening in Women with Dense Breasts,” was a multicenter, cross sectional study with longitudinal follow-up which compared the diagnostic performance of abbreviated breast MRI and digital breast tomosynthesis (DBT) for screening average-risk women with dense breasts (BI-RADS categories c and d). Patients were eligible to enroll if they were aged 40 to 75 years, clinically asymptomatic, and had dense breasts as described on a previous mammogram. Women with a screening breast US in the past 12 months, those who ever had a breast MRI, molecular breast imaging study, or contrast enhanced mammogram or those who qualify for full breast MRI based on their elevated-risk status were excluded. A total of 1444 women underwent both DBT and abbreviated MRI examinations [33•].
Patients underwent both DBT and abbreviated MRI screening at baseline and then again at 1 year. Both DBT and abbreviated MRI examinations were performed within a 24-h period with each study being interpreted independently of one another with the interpreting radiologist blinded to the results of the other modality. Abbreviated MRI acquisition time was less than 10 min [33•].
The primary outcome of the study was the rate of detection of invasive cancer by each modality. Secondary outcomes of the study included sensitivity, specificity, rate of additional imaging recommendation(s), and positive predictive value of biopsy as confirmed by pathology. The invasive cancer detection rate for abbreviated MRI was 11.8 per 1000 screenings as compared to 4.8 per 1000 screenings for DBT (P = 0.002). Abbreviated MRI detected 22 of 23 total cancers and all invasive cancers (CDR 15.2 per 1000). DBT detected 9 of 23 total cancers (CDR 6.2 per 1000; P = 0.001). The sensitivity for detecting invasive cancer and DCIS was 95.7% for abbreviated MRI as compared to 39.1% for DBT (P = 0.001). The specificity of abbreviated MRI was 86.7% compared to 97.4% for DBT (P ≤ 0.001). Additional imaging recommendation rate was 7.5% with abbreviated MRI vs. 10.1% for DBT (P = 0.02), and the PPV for biopsy performed was 19.6% vs. 31% which was not statistically significant (P = 0.15). Differences in recommending additional imaging were not statistically significant between the two modalities. There were no interval cancers during follow-up and no invasive cancer was identified by DBT alone [33•].
Financial Considerations and Cost-Effectiveness of MRI Screening in Dense Breasts
Studies have demonstrated that breast MRI has a significantly higher cancer detection rate than mammography alone, and if cancers are detected at an earlier stage, they may require less extensive and expensive treatment. Conversely, the false-positive rate and cost when adding MRI are also higher, raising concerns for increased utilization of resources and cost inefficiency. Studies evaluating the cost-effectiveness of breast MRI in screening patients with high-risk genetic predispositions for breast cancer have demonstrated that breast MRI screening in these populations is indeed cost-effective [40,41,42]. More recently, Geuzinge et al. modeled the cost-effectiveness of various screening strategies utilizing breast MRI screening for women with extremely dense breasts utilizing data from the DENSE trial [43]. After comparing several screening strategies including mammography and breast MRI at various intervals, they found that the only cost-effective strategy for screening women with dense breasts was to perform breast MRI every 4 years [43]. Limitations of this study on cost-effectiveness include a question of generalizability as the data used from the DENSE trial only includes Dutch women within the Dutch healthcare system and a 2-year screening interval. Cost-effective screening strategies may vary by country and healthcare system. Additionally, the DENSE trial was a full-protocol breast MRI, not an abbreviated breast MRI which is less expensive and will have a different cost-effectiveness analysis [44•].
Screening breast MRI in patients at high risk for breast cancer is recommended yearly; however, at this time, it is unclear the ideal interval for supplemental screening breast MRI in patients with dense breasts and otherwise average risk and whether it could be extended from 1 to 2 years or longer given the low-interval cancer rates with MRI screening in this population [28, 38$250 to $500, potentially creating disparate access to the technology [28]. Cost-analysis simulations of breast MRI screening have shown that assuming reduced cost of abbreviated breast MRI compared to full-protocol breast MRI may make triennial screening with abbreviated breast MRI more cost-effective than mammography after only 6 years [6].
Current Breast Cancer Screening Guidelines for Women with Dense Breasts
Screening guidelines from various organizations are provided for women of average risk and women of high risk of developing breast cancer. Specific screening recommendations for women with dense breasts, however, are less well-defined. Current recommendations and guidelines offered by various organizations in the USA are provided in Table 1. Recently, the ACR/SBI updated their supplemental screening recommendations for women of intermediate and high risk, including those with dense breasts. This update now includes the recommendation for annual digital mammography with or without DBT and annual MRI for women with dense breasts [4]. Additionally, the European Society of Breast Imaging now recommends supplemental breast cancer screening with MRI every 2–3 years for women with extremely dense breasts [45]. Multiple organizations have a less strong recommendation to consider of breast MRI as a supplement for breast density, including the American Society of Breast Surgeons and the National Comprehensive Cancer Network [5, 37]. The American Cancer Society, American College of Obstetricians and Gynecologists, and the US Preventative Services Task Force all find insufficient evidence to recommend for or against supplemental MRI screening for breast density [46,47,48,49,50].
Clinical Considerations and Shared Decision-Making
Breast MRI is a powerful tool for the detection of breast cancer, but the potential advantages in early detection of breast cancer, improved outcomes, less treatment, and less breast cancer–related morbidity and mortality must be considered along with the disadvantages of higher cost, limited access, and false-positive results. It is important for providers to engage in shared decision-making with patients regarding the advantages and disadvantages of supplemental screening with MRI, their risk profile, and their preferences and values. Contrast-enhanced breast MRI screening may be limited in patients with claustrophobia, elevated body mass index, impaired renal function, allergy to contrast, or with implantable medical devices or metallic foreign bodies that are incompatible with MRI. MRI can be time intensive and expensive and overall less accessible; however, abbreviated MRI protocols are shortening the length of the exam, decreasing cost and improving accessibility [27]. Additionally, concerns have been raised over the implications of repeated administrations of gadolinium-based contrast agents as studies have shown gadolinium deposits in the brain; however, to date, there is no evidence to show that gadolinium deposition is harmful and the International Society of Magnetic Resonance in Medicine (ISMRM) Safety Committee recommends gadolinium-based contrast agents not be withheld from patients who have a clinical indication for contrast-enhanced MRI [52]. Investigation into the use of diffusion-weighted MR techniques is underway, which may allow for future MRI screening without the administration of gadolinium-based contrast agents; however, these techniques have not yet been implemented clinically [53,54,55].
Conclusion
Increased breast density lowers the sensitivity of screening mammography and independently increases the risk for developing breast cancer. Contrast-enhanced breast MRI increases the cancer detection rate beyond mammography and decreases interval cancers found in these women. There are also drawbacks to screening MRI in higher cost, false-positives, and the use of contrast that should be considered with patients during a shared decision-making discussion. Future work further delineating the costs and benefits of abbreviated MRI and diffusion-weighted MRI are needed in addition to studies on the optimal timing and interval of its use. Our recommendation regarding supplemental screening with breast MRI for women with dense breasts aligns with the ACR/SBI recommendation for MRI screening in this population in conjunction with age-appropriate annual mammographic screening.
References
Papers of particular interest, published recently, have been highlighted as: • Of Importance
Nazari SS, Mukherjee P. An overview of mammographic density and its association with breast cancer. Breast Cancer. 2018;25(3):259–67.
Boyd NF, Sun L, Stone J, Fishell E, Jong RA, Chiarelli A. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356:227–36.
Freer PE. Mammographic breast density: impact on breast cancer risk and implications for screening. Radiographics. 2015;35(2):302–15.
Monticciolo DL, Newell MS, Moy L, Lee CS, Destounis SV. Breast cancer screening for women at higher-than-average risk: updated recommendations from the ACR. J Am Coll Radiol. 2023;20(9):902–14.
Bevers TB, Niell BL, Baker JL, Bonaccio E, Camp MS, et al. NCCN Guidelines® insights: breast cancer screening and diagnosis, Version 1.2023: Featured Updates to the NCCN Guidelines. J Natl Compr Canc Netw. 2023;21(9):900–9.
Mango VL, Goel A, Mema E, Kwak E, Ha R. Breast MRI screening for average-risk women: a Monte Carlo simulation cost–benefit analysis. Magn Reson Imaging. 2019;49(7):e216–21.
Saslow, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89.
Throckmorton AD, Rhodes DJ, Hughes KS, Degnim AC, Dickson-Witmer D. Dense breasts: what do our patients need to be told and why? Ann Surg Oncol. 2016;23(10):3119–27.
D’Orsi CJ, Sickles EA, Mendelson EB, Morris EA, et al. ACR BI-RADS® Atlas, breast imaging reporting and data system. VA, American College of Radiology: Reston; 2013.
Sprague BL, Gangnon RE, Burt V, Trentham-Dietz A, Hampton JM, Wellman RD, et al. Prevalence of mammographically dense breasts in the United States. J Natl Cancer Inst. 2014;106(10):dju255. Findings from this study demonstrate the prevalence of dense breasts which was inversely associated with age and BMI.
Kerlikowske K, Zhu W, Hubbard RA, Geller B, Dittus K, Braithwaite D, et al. Outcomes of screening mammography by frequency, breast density, and postmenopausal hormone therapy. JAMA Intern Med. 2013;173(9):807.
Destounis SV, et al. Update on breast density, risk estimation, and supplemental screening. AJR Am J Roentgenol. 2020;214(2):296–305.
Department of Health and Human Services. Food and drug administration mammography quality standards act final rule. Available at: https://public-inspection.federalregister.gov/2023–04550.pdf. Accessed 8 Aug 2023.
Berg WA, Seitzman RL, Pushkin J. Implementing the national dense breast reporting standard, expanding supplemental screening using current guidelines, and the proposed Find It Early Act. Journal of Breast Imaging. 2023;5(6):712–23.
Vegunta S, Kling JM, Patel BK. Supplemental cancer screening for women with dense breasts: guidance for health care professionals. Mayo Clin Proc. 2021;96(11):2891–904.
Lee CS, Monticciolo DL, Moy L. Screening guidelines update for average-risk and high-risk women. Am J Roentgenol. 2020;214(2):316–23.
Tabar L, et al. Insights from the breast cancer screening trials: how screening affects the natural history of breast cancer and implications for evaluating service screening programs. Breast J. 2014;21(1):13–20.
Carney PA, Miglioretti DL, Yankaskas BC, Kerlikowske K, Rosenberg R, Rutter CM, et al. Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med. 2003;138(3):168.
Lo G, Scaranelo AM, Aboras H, et al. Evaluation of the utility of screening mammography for high-risk women undergoing screening breast MR imaging. Radiology. 2017;285(1):36–43.
Narayan AK, Visvanathan K, Harvey SC. Comparative effectiveness of breast MRI and mammography in screening young women with elevated risk of developing breast cancer: a retrospective cohort study. Breast Cancer Res Treat. 2016;158(3):583–9.
Passaperuma K, Warner E, Causer PA, et al. Long term results of screening with magnetic resonance imaging in women with BRCA mutations. Br J Cancer. 2012;107(1):24–30.
Phi XA, Saadatmand S, De Bock GH, et al. Contribution of mammography to MRI screening in BRCA mutation carriers by BRCA status and age: individual patient data meta-analysis. Br J Cancer. 2016;114(6):631–7.
van Zelst JCM, Mus RDM, Woldringh G, et al. Surveillance of women with the BRCA1 or BRCA2 mutation by using biannual automated breast US, MR imaging, and mammography. Radiology. 2017;285(2):376–88.
Gao Y, Moy L, Heller S. Digital breast tomosynthesis: update on technology, evidence, and clinical practice. Radiographics. 2021;41(2):321–37.
Lee CI, Chen LE, Elmore JG. Risk-based breast cancer screening. Med Clin North Am. 2017;101(4):725–41.
Berg WA, Rafferty EA, Friedewald SM, Hruska CB, Rahbar H. Screening algorithms in dense breasts: AJR Expert Panel Narrative Review. Am J Roentgenol. 2021;216(2):275–94.
Wang L, Strigel RM. Supplemental screening for patients at intermediate and high risk for breast cancer. Radiol Clin North Am. 2021;59(1):67–83.
Grimm LJ, Mango VL, Harvey JA, et al. Implementation of abbreviated breast MRI for screening: AJR Expert Panel Narrative Review. AJR Expert Panel Review. 2022;218(2):202–12.
Mann RM, Cho N, Moy L. Breast MRI: state of the art. Radiology. 2019;292(3):520–36.
Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers R, et al. Abbreviated breast MRI: first postcontrast subtracted imaging and MIP – a novel approach to breast cancer screening with MRI. J Clin Oncol. 2014;32(22):2304–10.
Lawson MB, Partridge SC, Hippe DS, Rahbar H, Lam DL, Lee CI, et al. Comparative performance of contrast-enhanced mammography, abbreviated breast MRI, and standard breast MRI for breast cancer screening. Radiology. 2023;308(2): e230576.
Geach R, Jones LI, Harding SA, Marshall A, Taylor-Phillips S, McKeown-Keegan S, et al. The potential utility of abbreviated breast MRI (FAST MRI) as a tool for breast cancer screening: a systematic review and meta-analysis. Clin Radiol. 2021;76(2):154.e11-154.e22.
Comstock CE, Gatsonis C, Newstead GM, Snyder BS, Gareen IF, Bergin JT, et al. Comparison of abbreviated breast MRI vs digital breast tomosynthesis for breast cancer detection among women with dense breasts undergoing screening. JAMA. 2020;323(8):746. Findings from this cross-sectional study demonstrated higher cancer detection for abbreviated MRI compared to digital breast tomosynthesis for dense breasts.
MRI accreditation. American College of Radiology . Available from: https://www.acraccreditation.org/modalities/mri. Cited 2023 Oct 4.
National accreditation program for breast centers [Internet]. American College of Surgeons. Available from: https://www.facs.org/quality-programs/cancer-programs/national-accreditation-program-for-breast-centers. Cited 2023 Oct 4.
Saslow, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57(2):75–89.
Position Statement on screening mammography [Internet]. The American Society of Breast Surgeons. Available from: https://www.breastsurgeons.org/docs/statements/Position-Statement-on-Screening-Mammography.pdf. Cited 2023 Sep 4.
Bakker MF, Lange SV, Pijnappel RM, Mann RM, Peeters PHM, Monninkhof EM, et al. Supplemental MRI screening for women with extremely dense breast tissue. N Engl J Med. 2019;381(22):2091–102 This landmark randomized control trial demonstrated decreased interval cancer detection for women undergoing supplemental screening with MRI.
Veenhuizen SGA, De Lange SV, Bakker MF, Pijnappel RM, Mann RM, Monninkhof EM, et al. Supplemental breast MRI for women with extremely dense breasts: results of the second screening round of the DENSE trial. Radiology. 2021;299(2):278–86. Findings show in the second round of MRI screening a lower incremental cancer detection and reduced false-positive results.
Plevritis SK, Kurian AW, Sigal BM, Daniel BL, Ikeda DM, Stockdale FE, et al. Cost-effectiveness of screening BRCA1/2 mutation carriers with breast magnetic resonance imaging. JAMA. 2006;295(20):2374.
Lee JM, McMahon PM, Kong CY, Kopans DB, Ryan PD, Ozanne EM, et al. Cost-effectiveness of breast MR imaging and screen-film mammography for screening BRCA1 gene mutation carriers. 2010;254(3):793–800.
Geuzinge HA, Obdeijn IM, Rutgers EJT, Saadatmand S, Mann RM, Oosterwijk JC, et al. Cost-effectiveness of breast cancer screening with magnetic resonance imaging for women at familial risk. JAMA Oncol. 2020;6(9):1381.
Geuzinge HA, Bakker MF, Heijnsdijk EAM, Van Ravesteyn NT, Veldhuis WB, Pijnappel RM, et al. Cost-effectiveness of magnetic resonance imaging screening for women with extremely dense breast tissue. J Natl Cancer Inst. 2021;113(11):1476–83.
Emaus MJ, Bakker MF, Peeters PHM, Loo CE, Mann RM, De Jong MDF, et al. MR imaging as an additional screening modality for the detection of breast cancer in women aged 50–75 years with extremely dense breasts: the DENSE trial study design. Radiology. 2015;277(2):527–37. This publication outlines the study design for this landmark MRI supplemental screening study for dense breasts.
Mann RM, Athanasiou A, Baltzer PAT, Camps-Herrero J, Clauser P, Fallenberg EM, et al. Breast cancer screening in women with extremely dense breasts recommendations of the European Society of Breast Imaging (EUSOBI). Eur Radiol. 2022;32(6):4036–45.
Oeffinger KC, Fontham ETH, Etzioni R, Herzig A, Michaelson JS, Shih YCT, et al. Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314(15):1599.
American Cancer Society recommendations for the early detection of breast cancer. American Cancer Society. Available from: https://www.cancer.org/cancer/types/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html . Cited 2023 Sep 9.
Practice Bulletin Number 179. breast cancer risk assessment and screening in average-risk women. Obstet Gynecol. 2017;130(1):e1–16.
Committee Opinion No. 625: management of women with dense breasts diagnosed by mammography. Obstet Gynecol. 2015;125(3):750–1.
Draft recommendation statement breast cancer: screening. U.S Preventative Services Task Force. Available from: https://www.uspreventiveservicestaskforce.org/uspstf/draft-recommendation/breast-cancer-screening-adults#bcei-recommendation-title-area. Cited 2023 Sep 9.
Monticciolo DL, Newell MS, Hendrick RE, Helvie MA, Moy L, Monsees B, et al. Breast cancer screening for average-risk women: recommendations from the ACR Commission on Breast Imaging. J Am Coll Radiol. 2017;14(9):1137–43.
Gulani V, Calamante F, Shellock FG, Kanal E, Reeder SB. Gadolinium deposition in the brain: summary of evidence and recommendations. The Lancet Neurology. 2017;16(7):564–70.
Moran CJ, Cheng JY, Sandino CM, Carl M, Alley MT, Rosenberg J, et al. Diffusion-weighted double-echo steady-state with a three-dimensional cones trajectory for non-contrast breast MRI. Magn Reson Imaging. 2021;53(5):1594–605.
Granlund KL, Staroswiecki E, Alley MT, Daniel BL, Hargreaves BA. High-resolution, three-dimensional diffusion-weighted breast imaging using DESS. Magn Reson Imaging. 2014;32(4):330–41.
Mendez AM, Fang LK, Meriwether CH, Batasin SJ, Loubrie S, Rodríguez-Soto AE, et al. Diffusion breast MRI: current standard and emerging techniques. Front Oncol. 2022;12: 844790.
Author information
Authors and Affiliations
Contributions
T.L. wrote the main manuscript text. R.S. and L.B contributed to the conception and interpretation of the work. T.L. prepared the tables and figures. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Competing interests
Thomas LoDuca and Laura Bozzuto declare that they have no conflicts of interest. Roberta Strigel has received institutional research support from GE Healthcare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
LoDuca, T.P., Strigel, R.M. & Bozzuto, L.M. Utilization of Screening Breast MRI in Women with Extremely Dense Breasts. Curr Breast Cancer Rep 16, 53–60 (2024). https://doi.org/10.1007/s12609-024-00525-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-024-00525-6