Abstract
Obesity and metabolic syndrome are risk and prognostic factors for breast cancer (BC) and are associated with chronic inflammation. We investigated the association between distinct BC subtypes and markers of adiposity, dysmetabolisms, and inflammation. We analyzed 1779 patients with primary invasive BC treated at a single institution, for whom anthropometric and clinical-pathological data were archived. BC subtypes were classified by immunohistochemical staining of ER, PR, HER2, and Ki67, and their relations with the study markers were assessed by multinomial logistic regression. Adjusted odds ratios (ORs) and 95 % confidence intervals (CIs) were calculated taking luminal A as reference. All subtypes more aggressive than luminal A were significantly more frequent in younger (<45 years) than older women. Before menopause, luminal B HER2-negative tumors were positively associated with large waist (OR 2.55, 95 % CI 1.53–4.24) and insulin resistance (OR 1.90, 95 % CI 1.05–3.41); luminal B HER2-positive tumors with large waist (OR 2.11, 95 % CI 1.03–4.35) and triple-negative tumors with overweight (OR 3.04, 95 % CI 1.43–6.43) and high C-reactive protein (p trend = 0.026). In postmenopausal women aged <65, luminal B HER2-negative (OR 1.94, 95 % CI 1.16–3.24) and luminal B HER2-positive tumors (OR 2.48, 95 % CI 1.16–5.27) were positively related with metabolic syndrome. Dysmetabolisms and inflammation may be related to different BC subtypes. Before menopause, triple-negative cancers were related to obesity and chronic inflammation, and aggressive luminal subtypes to abdominal adiposity. After menopause, in women aged <65 these latter subtypes were related to metabolic syndrome. Control of adiposity and dysmetabolism can reduce the risk of aggressive BC subtypes, improving the prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is not one disease but several. Subtypes defined by distinct gene expression profiles differ in terms of natural history, response to treatment, and outcomes [1]. Subtypes defined by estrogen receptor (ER), progesterone receptor (PR), HER2, and Ki67 status approximate the intrinsic subtypes that have emerged from gene expression studies [2] and differ in their responses to treatment and outcomes [3, 4].
Women who are obese, have metabolic syndrome, hyperinsulinemia, or insulin resistance (IR) are at significantly greater risk of BC than women who do not have these disorders [5–8]. Survival is also worse for these women [9–11]. Some studies suggest that the influence of obesity and metabolic syndrome on BC risk varies with subtype and with menopausal status. Thus, in premenopausal women, high body mass index (BMI) has been consistently associated with a lower risk of hormone-positive BC [12–14], while in these same women abdominal rather than general adiposity has been associated with a higher risk of receptor-negative BC [14, 15]. In postmenopausal women, by contrast, high BMI has been associated with an increased risk of hormone-positive BC [12].
Abdominal obesity, hyperinsulinemia, IR, and metabolic syndrome are also associated with chronic inflammation [16]. However, only a few studies have investigated metabolic [17, 18] and inflammatory factors [19] in relation to the risk of specific BC subtypes.
The present cross-sectional study investigated whether markers of adiposity, dysmetabolism, and inflammation relate differently to distinct BC subtypes. We analyzed data from a prospectively maintained hospital-based registry of BC cases, stratifying patients by their menstrual status to take account of possible changes after menopause in adiposity, dysmetabolism, and inflammation.
Materials and methods
Study population
We analyzed data on BC cases prospectively archived in the BC registry of the National Cancer Institute (INT), Milan, Italy [20]. The registry, which started in October 2011, collects anthropometric, clinical, and pathological-biological data on all women with BC who present at the INT. Cases archived up to February 2015 with a diagnosis of primary invasive BC [21] who underwent surgery, not receiving any neoadjuvant treatment, were potentially eligible for inclusion in the study.
According to ICD-O-3 codes [22], tumor morphology was grouped in four categories: infiltrating ductal carcinoma (IDC) (8500), infiltrating lobular carcinoma (ILC) (8520), infiltrating mixed ductal and lobular (8522-8524), and Paget’s disease (8540-8543). Tumors were classified as well differentiated, moderately differentiated, poorly differentiated, and unknown. BC subtypes were defined by ER, PR, HER2, and Ki67 status according to the 2011 St. Gallen Consensus Statement [2] as follows:
-
Luminal A: ER- and/or PR-positive, HER2-negative, Ki67 <14 %;
-
Luminal B (HER2-negative): ER- and/or PR-positive, HER2-negative, Ki67 ≥14 %;
-
Luminal B (HER2-positive): ER- and/or PR-positive, HER2-positive, any Ki67;
-
HER2-positive (non-luminal): ER- and PR-negative, HER2-positive, any Ki67;
-
Triple-negative: ER- and PR-negative, HER2-negative, any Ki67.
Following American Association of Clinical Oncology guidelines [23], ER and PR were considered positive if immunostaining was seen on 1 % or more of tumor nuclei. HER2 was considered positive when (a) the immunohistochemical (IHC) score was 3+ or (b) the IHC was 2+ and fluorescence in situ hybridization (FISH) indicated gene amplification. HER2 was negative when the IHC score was 0–1+. HER2 was considered unknown for IHC scores 2+ and FISH unavailable. The tumor proliferation marker, Ki67 index, was evaluated by IHC visual assessment of Ki67-antigen expression in tissue sample fixed in 10 % buffered formalin. Specifically, the assessment was performed in a selected representative block of each tumor by selecting at least three fields of ‘hot-spots’ at the periphery of tumor edge of invasion and counting ratio between stained and unstained nuclei of about 500 cells.
The following markers of adiposity, dysmetabolism, and inflammation were analyzed:
-
BMI, a measure of general adiposity [classified as <25 kg/m2 (not overweight), 25 to <30 kg/m2 (overweight), and ≥30 kg/m2 (obese)];
-
Waist circumference, a measure of abdominal adiposity (<80 and ≥80 cm);
-
Fasting blood insulin and fasting blood glucose, divided into tertiles after excluding diabetic patients, who formed a separate category;
-
Homeostatic model assessment index of insulin resistance (HOMA-IR);
-
Metabolic syndrome;
-
C-reactive protein (CRP; marker of inflammation).
HOMA-IR, calculated by multiplying fasting blood insulin (mU/L) by fasting blood glucose (mg/dL), and dividing by 405 [24], was classified as <2.5 and ≥2.5. Metabolic syndrome was classified according to the definition proposed in the 2009 Joint Scientific Statement by International Diabetes Federation, National Heart, Lung and Blood Institute, American Heart Association, World Heart Federation, International Atherosclerosis Society, and International Association for the Study of Obesity [25]. In accordance with the Joint Scientific Statement, we took any three of the following five conditions to indicate metabolic syndrome: waist circumference ≥80 cm; triglycerides ≥150 mg/dL or lipid-lowering medication for dyslipidemia; HDL cholesterol ≤50 mg/dL or medication for dyslipidemia; systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥85 mmHg, or antihypertensive medication; fasting glucose ≥100 mg/dL [25]. CRP was classified as absent (0 mg/L) or present (≥1 mg/L), dividing present further as 1 mg/L (mild inflammation), 2–10 mg/L (moderate inflammation), and >10 mg/L (acute inflammation).
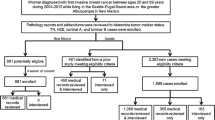
A total of 2054 cases were potentially eligible according to our initial selection criteria. Of these, 75 were excluded because of insufficient information to assign the BC subtype, 125 because of insufficient information to assess the presence of metabolic syndrome, 75 because BMI (7 cases) or information on blood insulin or lipids was missing (38 and 30 cases, respectively). Thus, 1779 cases were available for the analyses and divided into three categories according to their menstrual status. Women whose last menstruation was 12 months or more before diagnosis (810 cases, including 46 with iatrogenic menopause unrelated to BC) or who were 55 years old or more (290 cases) at diagnosis and information on last menstruation was lacking were considered postmenopausal. Women whose last menstruation was 3 months or less before diagnosis (565 cases) or who were under 45 years old (31 cases) and had no information on last menstruation were considered premenopausal. The remaining 83 women were aged 45–54 years; of these, 17 whose last menstruation was more than three but less than 12 months earlier were considered perimenopausal, and 66 with no information on last menstruation were assigned unknown menopausal status, although many were probably perimenopausal.
Statistical methods
Patient and disease characteristics by menstrual status were summarized by descriptive statistics. Differences in the distribution of characteristics between the premenopausal and postmenopausal groups were assessed by the Kruskal–Wallis test for continuous variables, and the χ 2 test or Fisher’s exact test, as appropriate, for categorical variables, excluding women who were perimenopausal or whose menopausal status was unknown. Associations between BMI and other markers (waist circumference, CRP, hyperinsulinemia, IR, metabolic syndrome, and individual factors contributing to metabolic syndrome) were assessed by Spearman’s rank correlation coefficient (ρ) or the χ 2 test, as appropriate. Associations of dysmetabolism markers and disease characteristics with BC subtypes were explored by multinomial logistic regression, making it possible to calculate the odds (as odds ratios, ORs) of events of interest simultaneously taking account of any other events. We used multinomial logistic regression to calculate the minimally adjusted odds of having one of the BC subtypes (luminal B HER2-negative, luminal B HER2-positive, HER2-positive non-luminal, or triple-negative) relative to the reference subtype (luminal A) for each disease characteristic and marker of dysmetabolism and inflammation, adjusting only for age and BMI (where appropriate). The analyses were done on pre- and postmenopausal cases separately, excluding cases with perimenopausal and unknown menopausal status. The Wald test was used to assess the significance of linear trends in ORs with increasing levels of categorical variables. The likelihood ratio test was used to compare models with and without the product term of the interacting variables. Two-sided p values <0.05 were considered significant.
Since there were significant interactions between IR and BMI for luminal B (HER2-negative) subtype, and between metabolic syndrome and age for luminal B (both HER2-negative and HER2-positive) subtypes for postmenopausal women, age-adjusted ORs for IR are presented in strata of BMI (<25 and ≥25 kg/m2) and age- (continuous variable) and BMI-adjusted ORs for metabolic syndrome are presented in strata of age (<65 and ≥65 years).
To account for any reverse causation effect of disease stage on markers of inflammation [26], we did a stratified analysis to assess the association between CRP and BC subtype, doing multinomial logistic regression analyses separately on T1-T2N0 and more advanced cases. Fully adjusted models including age, BMI, metabolic syndrome, and CRP, within groups of tumor stage, were feasible only in the postmenopausal T1-T2N0 group, because of the small numbers of postmenopausal patients with more advanced stage and premenopausal patients with metabolic syndrome.
Analyses were done with the Stata statistical package, release 12.0 (Stata Corporation, College Station, TX, USA).
Results
Table 1 summarizes the characteristics of the 1779 BC cases, by menopausal status. The distributions of markers of adiposity, dysmetabolism, and inflammation differed markedly between the 596 (33 %) premenopausal and 1100 (62 %) postmenopausal patients (all p ≤ 0.001). Only 83 (5 %) cases were perimenopausal/unknown menopausal status. Compared to premenopausal cases, postmenopausal cases were more often overweight (36 vs. 17 %) or obese (18 vs. 5 %), more often had waist circumference ≥80 cm (66 vs. 45 %) and had higher median levels of fasting blood glucose (98 vs. 90 mg/dL), insulin (8.5 vs. 6.9 µIU/mL), and triglycerides (93 vs. 66 mg/dL). There were also more postmenopausal than premenopausal women with high blood pressure (22 vs. 11 %), antihypertensive treatment (46 vs. 5 %), lipid-lowering treatment (19 vs. 1 %), insulin resistance (HOMA-IR ≥2.5: 36 vs. 20 %), diabetes (9 vs. 1 %), metabolic syndrome (49 vs. 7 %), and moderate inflammation (CRP 2–10 mg/L: 46 vs. 21 %). Premenopausal women more often (p < 0.001) had advanced tumors (more than T1-T2N0, 39 vs. 32 %,) and less favorable (p = 0.005) grade distribution (50 vs. 57 % moderately differentiated; 41 vs. 37 % poorly differentiated) than postmenopausal cases. Differences between the two groups were not significant for BC subtype (p = 0.063) or BC morphology (p = 0.887).
BMI correlated strongly (Spearman’s) with waist circumference in the postmenopausal (ρ = 0.791, p < 0.001) and premenopausal women (ρ = 0.688, p < 0.001). Overweight or obese women (BMI ≥25 kg/m2) were more likely to have CRP above zero (94 vs. 73 %, p < 0.001 in the postmenopausal group, and 87 vs. 49 %, p < 0.001 in the premenopausal group), and there were more cases of metabolic syndrome (63 vs. 32 %, p < 0.001 in the postmenopausal group, and 20 vs. 3 %, p < 0.001 in the premenopausal group) than among underweight or normal-weight women (data not shown).
The multinomial logistic regression results are shown in Table 2 for premenopausal women. All BC subtypes biologically more aggressive than luminal A were significantly more frequent among younger (<45 years) than older (≥45 years) women. Luminal B (HER2-negative) disease was more frequent in women with large waist (OR 2.55, 95 % CI 1.53–4.24) than those with waist <80 cm; glucose in the second tertile of the distribution was more frequent (OR 2.04, 95 % CI 1.21–3.41), and the HOMA-IR index (indicating insulin resistance) was higher than in those with a low index (OR 1.90, 95 % CI 1.05–3.41). Luminal B HER2-positive disease was more frequent than luminal A in women with large waist (OR 2.11, 95 % CI 1.03–4.35) and women with high CRP (p trend = 0.048). Waist circumference was unknown in 18 % of women. We examined these cases as a separate category, and no association emerged.
Triple-negative disease was significantly more frequent than luminal A in overweight women (OR 3.04, 95 % CI 1.43–6.43), those with high CRP (ORs 2.62, 95 % CI 1.14–6.01 for low-grade inflammation; 2.82, 95 % CI 1.04–7.69 for moderate-grade inflammation; p trend = 0.026), and those in the second tertile of blood glucose (OR 2.37, 95 % CI 1.06–5.27). HER2-positive (non-luminal) disease was more frequent than luminal A in women in the second tertile of blood glucose (OR 2.32, 95 % CI 0.96–5.64).
All subtypes except HER2-positive (non-luminal), biologically more aggressive than luminal A, were non-significantly more frequent in women with metabolic syndrome.
Stratified analyses done separately on early and more advanced premenopausal BC confirmed the association between increasing CRP and triple-negative tumors only in the early-stage subgroup (T1-T2N0) (age- and BMI-adjusted ORs 3.73, 95 % CI 1.25–11.11 for low-grade inflammation and 4.70, 95 % CI 1.30–16.94 for moderate-grade inflammation; p trend = 0.012) (data not shown).
The multinomial logistic regression results for postmenopausal women are illustrated in Table 3. Luminal B (HER2-negative) disease was significantly more frequent than luminal A in overweight than not overweight women (OR 1.51, 95 % CI 1.14–2.00) and in women with diabetes (OR 1.94, 95 % CI 1.06–3.55) than among those in the lowest glucose tertile. Normal-weight women with IR had a lower frequency of luminal B (HER2-negative) than luminal A disease (OR 0.59, 95 % CI 0.35–1.01).
In younger postmenopausal women aged <65, luminal B cancers (HER2 negative and positive) were associated with metabolic syndrome significantly more frequently than luminal A (respectively OR 1.94, 95 % CI 1.16–3.24 and OR 2.48, 95 % CI 1.16–5.27). No significant associations were seen in older postmenopausal patients.
Triple-negative disease was significantly more frequent than luminal A in women in the second glucose tertile (OR 2.59, 95 % CI 1.31–5.14) than the first. No significant association was found between HER2-positive (non-luminal) disease and any indicator of dysmetabolism. Stratified analyses on postmenopausal CRP levels did not bring to light any association with tumor subtype in either early or more advanced stages.
The fully adjusted multinomial logistic regression model, run separately in younger and older postmenopausal patients with early-stage disease, confirmed the significant relations between metabolic syndrome and luminal B (both HER2-negative and -positive) found by the minimally adjusted model for younger women (luminal B HER2-negative OR 2.20, 95 % CI 1.14–4.27; luminal B HER2-positive OR 3.92, 95 % CI 1.57–9.80). BMI and the luminal B HER2-negative subtype showed a weaker relation, no longer significant (data not shown).
Discussion
This cross-sectional study examined how markers of dysmetabolism and inflammation were related with immunohistochemically defined disease subtypes in a consecutive series of 1779 BC patients diagnosed and treated at a single institute. Before menopause, BC subtypes more aggressive than luminal A were significantly more frequent among younger (<45 years) than older (≥45 years) women, while after menopause HER2-positive (non-luminal) disease was more frequent in the younger (<65 years) than older (≥65 years) women. Similar findings have already been reported [27] and are in line with the generally poorer prognosis in younger than older BC patients [28]. Young age in premenopausal women was most strongly associated with the triple-negative, luminal B (HER2-positive), and HER2-positive (non-luminal) subtypes, which have considerably worse survival than luminal A disease, although this is now somewhat mitigated by the targeted treatments for HER2-positive disease.
We also found that more aggressive BC subtypes were associated with dysmetabolic markers, with some differences according to menstrual status. Previous studies reported that premenopausal obesity reduced the risk of ER- and PR-positive BC [12] and increased the risk of hormone-negative BC (which includes triple-negative) [15, 29, 30]. A recent study found that weight gain in premenopausal women raised the risk of ER-positive and PR-negative and ER- and PR-negative rather than ER- and PR-positive BC [31]. In agreement with these etiological studies, we found that overweight/obesity was significantly associated with the triple-negative subtype in premenopause.
In addition, large waist circumference (adjusted by BMI in the multinomial regression model) was significantly associated with luminal B (HER2-negative and positive) premenopausal BC. Hip circumference and waist-to-hip ratio (indicators of central adiposity) are reported as BC risk factors before menopause [32, 33], suggesting a role of IR. This resistance slows the intake of blood glucose into the cells, with a consequent rise in glycemia, which in turn stimulates insulin secretion (by feed-back regulation). Insulin is a mutagenic agent and hyperinsulinemia lowers the levels of insulin-like growth factor (IGF) 1- and 2-binding protein, increasing the bioavailability of IGF which is known to promote human breast cancer [34]. Insulin may also promote breast cancer growth by inducing aromatase activity and reducing sex hormone-binding globulin production with a consequent increase of mutagenic free estradiol [8].
In postmenopausal women, obesity was associated with luminal B (HER2-negative) BC and in younger postmenopausal women (<65 years) metabolic syndrome was significantly associated with luminal disease (HER2-negative and positive). Obesity is a documented risk factor for postmenopausal hormone receptor-positive BC [12]. The current interpretation of the causal mechanism is that after menopause adipose tissue is the main site of aromatase activity and the obesity-induced reduction in the production of sex hormone-binding globulin may further raise levels of circulating free estrogens, inducing ER and PR expression and stimulation of hormone receptor-positive tumors [35]. This causal relation between obesity and the risk of hormone receptor-positive subtypes might explain why after menopause we find no clear association between obesity and BC subtypes more aggressive than the luminal A.
Metabolic syndrome is a documented risk factor for BC, mainly in postmenopausal women [6, 7]. However, only few studies have analyzed metabolic syndrome in relation to specific BC subtypes. In our study, metabolic syndrome was associated with luminal B HER2-negative and luminal B HER2-positive disease in postmenopausal women under 65 years.
One important finding of the present study is the significant association between high CRP (a marker of chronic inflammatory status which is frequently high in persons with IR) and triple-negative and luminal B HER2-positive BC in premenopause. The standard CRP cut-off of 3 mg/L (separating low from high risk of cardiovascular disease) was not used because only a few cases were ≥3 and ≤10 mg/L, mainly premenopausal women—10 % (postmenopausal women 30 %). Systemic inflammation biomarkers such as CRP have been associated both with cancer risk [36] and tumor progression [37]. A chronic inflammatory status such as that related to obesity, hyperglycemia, or IR could cause oxidative damage and inactivate proteins involved in DNA repair or apoptotic control, thus promoting cancer cell initiation and growth [38]. It is also possible that the host’s immune response is a consequence of the tumor growth itself [26, 39], and there may be a reverse causation effect. Stratified analyses done separately in early and more advanced stages confirmed the association between increasing CRP and triple-negative tumors in premenopausal BC only in the early-stage subgroup (T1-T2N0); this suggests that high CRP levels may be a consequence of the tumor growth, and limits the possibility of identifying potential relations between chronic inflammation and tumor subtypes in patients with advanced disease.
The association between dysmetabolic factors and more aggressive BC subtypes than the referent category of luminal A is in line with the reported detrimental effect on BC prognosis and survival of obesity [9], high insulin levels [11], CRP [40], and metabolic syndrome [10]. Our findings also agree with a recent review on BC heterogeneity and known risk factors, reporting that in premenopause obesity is negatively associated with luminal A subtypes and positively associated with triple-negative disease, whereas in postmenopausal women there are no clear relations between triple-negative subtype risk and obesity [30]. However, that review dealt with established BC risk factors such as reproductive factors, obesity, exogenous hormones, alcohol use, and family history, mainly affecting the risk of luminal A subtype, and the authors highlighted the need for subtype-specific studies on non-hormonal risk factors, including lifestyle factors and exogenous exposures, to clarify the etiology and the mechanism of action of less common subtypes, especially ER-negative ones [30].
In summary, in premenopausal patients overweight and chronic inflammation raised the odds of being diagnosed with triple-negative tumor; IR was associated with higher odds of luminal B HER2-negative subtype. After menopause, metabolic syndrome was associated with higher odds of luminal B HER2-negative and positive subtypes, for women younger than 65. These findings suggest that dysmetabolisms may play a role in the biological determinism of BC subtypes and further investigation is needed on the etiological mechanisms, as well as the roles of inflammatory biomarkers in tumor etiology and progression.
Measures against obesity in young women are important, given the increasing prevalence of overweight among young Italians [41]. Control of metabolic syndrome can help limit the incidence of the very frequent hormone-positive BC subtypes.
Abbreviations
- BC:
-
Breast cancer
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- ER:
-
Estrogen receptor
- FISH:
-
Fluorescence in situ hybridization
- HER2:
-
Human epidermal growth factor receptor 2
- HOMA:
-
Homeostatic model assessment index
- IDC:
-
Infiltrating ductal carcinoma
- IHC:
-
Immunohistochemical
- ILC:
-
Infiltrating lobular carcinoma
- IQR:
-
Interquartile range
- IR:
-
Insulin resistance
- OR:
-
Odds ratio
- PR:
-
Progesterone receptor
References
Sørlie T (2004) Molecular portraits of breast cancer: tumor subtypes as distinct disease entities. Eur J Cancer 40(18):2667–2675
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ, Panel members (2011) Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol 22:1736–1747. doi:10.1093/annonc/mdr304
Minicozzi P, Bella F, Toss A, Giacomin A, Fusco M, Zarcone M et al (2013) Relative and disease-free survival for breast cancer in relation to subtype: a population-based study. J Cancer Res Clin Oncol 139(9):1569–1577. doi:10.1007/s00432-013-1478-1
Ribelles N, Perez-Villa L, Jerez JM, Pajares B, Vicioso L, Jimenez B et al (2013) Pattern of recurrence of early breast cancer is different according to intrinsic subtype and proliferation index. Breast Cancer Res 15(5):R98
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371(9612):569–578. doi:10.1016/S0140-6736(08)60269-X
Bhandari R, Kelley GA, Hartley TA, Rockett IR (2014) Metabolic syndrome is associated with increased breast cancer risk: a systematic review with meta-analysis. Int J Breast Cancer 2014:189384. doi:10.1155/2014/189384
Agnoli C, Grioni S, Sieri S, Sacerdote C, Ricceri F, Tumino R et al (2015) Metabolic syndrome and BC risk: a case-cohort study nested in a multicentre italian cohort. PLoS One 10(6):e0128891. doi:10.1371/journal.pone.0128891
Vona-Davis L, Howard-McNatt M, Rose DP (2007) Adiposity, type 2 diabetes and the metabolic syndrome in breast cancer. Obes Rev 8(5):395–408
Protani M, Coory M, Martin JH (2010) Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat 123(3):627–635. doi:10.1007/s10549-010-0990-0
Berrino F, Villarini A, Traina A, Bonanni B, Panico S, Mano MP et al (2014) Metabolic syndrome and breast cancer prognosis. Breast Cancer Res Treat 147(1):159–165. doi:10.1007/s10549-014-3076-6
Goodwin PJ, Ennis M, Pritchard KI, Trudeau ME, Koo J, Madarnas Y et al (2002) Fasting insulin and outcome in early-stage breast cancer: results of a prospective cohort study. J Clin Oncol 20(1):42–51
Suzuki R, Orsini N, Saji S, Key TJ, Wolk A (2009) Body weight and incidence of breast cancer defined by estrogen and progesterone receptor status—a meta-analysis. Int J Cancer 124(3):698–712. doi:10.1002/ijc.23943
Ritte R, Lukanova A, Berrino F, Dossus L, Tjønneland A, Olsen A et al (2012) Adiposity, hormone replacement therapy use and breast cancer risk by age and hormone receptor status: a large prospective cohort study. Breast Cancer Res 14(3):R76
Fagherazzi G, Chabbert-Buffet N, Fabre A, Guillas G, Boutron-Ruault MC, Mesrine S et al (2012) Hip circumference is associated with the risk of premenopausal ER−/PR− breast cancer. Int J Obes (Lond) 36(3):431–439. doi:10.1038/ijo.2011.66
Harris HR, Willett WC, Terry KL, Michels KB (2011) Body fat distribution and risk of premenopausal breast cancer in the Nurses’ Health Study II. J Natl Cancer Inst 103(3):273–278. doi:10.1093/jnci/djq500
Rodríguez-Hernández H, Simental-Mendía LE, Rodríguez-Ramírez G, Reyes-Romero MA (2013) Obesity and inflammation: epidemiology, risk factors, and markers of inflammation. Int J Endocrinol 2013:678159. doi:10.1155/2013/678159
Davis AA, Kaklamani VG (2012) Metabolic syndrome and triple-negative breast cancer: a new paradigm. Int J Breast Cancer 2012:809291. doi:10.1155/2012/809291
Colonna SV, Douglas Case L, Lawrence JA (2012) A retrospective review of the metabolic syndrome in women diagnosed with breast cancer and correlation with estrogen receptor. Breast Cancer Res Treat 131(1):325–331. doi:10.1007/s10549-011-1790-x
Hong T, Liu A, Cai D, Zhang Y, Hua D, Hang X et al (2013) Preoperative serum C-reactive protein levels and early breast cancer by BMI and menopausal status. Cancer Invest 31(4):279–285. doi:10.3109/07357907.2013.789898
Baili P, Torresani M, Agresti R, Rosito G, Daidone MG, Veneroni S et al (2015) A breast cancer clinical registry in an Italian comprehensive cancer center: an instrument for descriptive, clinical, and experimental research. Tumori 101(4):440–446. doi:10.5301/tj.5000341
UICC (2009) TNM: Classificazione dei Tumori Maligni, Settima Edizione. Raffaello Cortina Editore, Milano
WHO (2005) ICDO-3: classificazione Internazionale delle Malattie per l’Oncologia-Terza Edizione. Inferenze Scarl, Milano
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S et al (2010) American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations for Immunohistochemical Testing of Estrogen and Progesterone Receptors in Breast Cancer. J Clin Oncol 28(16):2784–2795. doi:10.1200/JCO.2009.25.6529
Singh B, Saxena A (2010) Surrogate markers of insulin resistance: a review. World J Diabetes 1(2):36–47. doi:10.4239/wjd.v1.i2.36
Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120:1640–1645
Mantovani A, Allavena P, Sica A, Balkwill F (2008) Cancer-related inflammation. Nature 454(7203):436–444. doi:10.1038/nature07205
McGuire A, Brown JA, Malone C, McLaughlin R, Kerin MJ (2015) Effects of age on the detection and management of breast cancer. Cancers (Basel) 7(2):908–929. doi:10.3390/cancers7020815
Liedtke C, Rody A, Gluz O, Baumann K, Beyer D, Kohls EB et al (2015) The prognostic impact of age in different molecular subtypes of breast cancer. Breast Cancer Res Treat 152(3):667–673. doi:10.1007/s10549-015-3491-3
Cotterchio M, Kreiger N, Theis B, Sloan M, Bahl S (2003) Hormonal factors and the risk of breast cancer according to estrogen- and progesterone-receptor subgroup. Cancer Epidemiol Biomark Prev 12:1053–1060
Barnard ME, Boeke CE, Tamimi RM (2015) Established breast cancer risk factors and risk of intrinsic tumor subtypes. Biochim Biophys Acta 1856(1):73–85. doi:10.1016/j.bbcan.2015.06.002
Rosner B, Eliassen AH, Toriola AT, Hankinson SE, Willett WC, Natarajan L et al (2015) Short-term weight gain and breast cancer risk by hormone receptor classification among pre- and postmenopausal women. Breast Cancer Res Treat 150(3):643–653. doi:10.1007/s10549-015-3344-0
Lahmann PH, Hoffmann K, Allen N, van Gils CH, Khaw KT, Tehard B et al (2004) Body size and breast cancer risk: findings from the European Prospective Investigation into Cancer and Nutrition (EPIC). Int J Cancer 111(5):762–771
Muti P, Stanulla M, Micheli A, Krogh V, Freudenheim JL, Yang J et al (2000) Markers of insulin resistance and sex steroid hormone activity in relation to breast cancer risk: a prospective analysis of abdominal adiposity, sebum production, and hirsutism (Italy). Cancer Causes Control 11(8):721–730
Doyle SL, Donohoe CL, Lysaght J, Reynolds JV (2012) Visceral obesity, metabolic syndrome, insulin resistance and cancer. Proc Nutr Soc 71(1):181–189. doi:10.1017/S002966511100320X
Rose DP, Vona-Davis L (2010) Interaction between menopausal status and obesity in affecting breast cancer risk. Maturitas 66(1):33–38. doi:10.1016/j.maturitas.2010.01.019
Chan DS, Bandera EV, Greenwood DC, Norat T (2015) Circulating C-reactive protein and breast cancer risk-systematic literature review and meta-analysis of prospective cohort studies. Cancer Epidemiol Biomark Prev 24(10):1439–1449. doi:10.1158/1055-9965.EPI-15-0324
Han Y, Mao F, Wu Y, Fu X, Zhu X, Zhou S et al (2011) Prognostic role of C-reactive protein in breast cancer: a systematic review and meta-analysis. Int J Biol Markers 26(4):209–215. doi:10.5301/JBM.2011.8872
Suman S, Sharma PK, Rai G, Mishra S, Arora D, Gupta P et al (2015) Current perspectives of molecular pathways involved in chronic Inflammation-mediated breast cancer. Biochem Biophys Res Commun 472(3):401–409. doi:10.1016/j.bbrc.2015.10.133
Siemes C, Visser LE, Coebergh JW, Splinter TA, Witteman JC, Uitterlinden AG et al (2006) C-reactive protein levels, variation in the C-reactive protein gene, and cancer risk: the Rotterdam Study. J Clin Oncol 24(33):5216–5222
Allin KH, Nordestgaard BG, Flyger H, Bojesen SE (2011) Elevated pre-treatment levels of plasma C-reactive protein are associated with poor prognosis after breast cancer: a cohort study. Breast Cancer Res 13(3):R55. doi:10.1186/bcr2891
ISTAT—Istituto Nazionale di Statistica (2015) Health for all. http://www.istat.it/it/archivio/14562. Accessed 16 December 2015
Acknowledgments
The authors thank Judith Baggott for help with the English.
Authors’ contributions
Conception and design: R. Agresti, M. Sant, E. Meneghini, F. Berrino. Acquisition of data: H. Amash, A.Turco. Analysis and interpretation of data: E. Meneghini, M. Sant, R. Agresti, P. Minicozzi, F. Berrino, E. Tagliabue. Writing, review and/or revision of the manuscript: M. Sant, R. Agresti, E. Meneghini, P. Minicozzi, F. Berrino, E. Tagliabue. Administrative, technical, or material support: P. Baili, I. Cavallo, F. Funaro. Study supervision: M. Sant, R. Agresti, F. Berrino, E. Tagliabue.
Financial support
The INT breast cancer registry is subsidized by the project INT 5 × 1000-year 2012 B52I1200057001 “Implementation of breast cancer clinical registry.”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study has been approved by the Ethical Committee of the National Cancer Institute.
Rights and permissions
About this article
Cite this article
Agresti, R., Meneghini, E., Baili, P. et al. Association of adiposity, dysmetabolisms, and inflammation with aggressive breast cancer subtypes: a cross-sectional study. Breast Cancer Res Treat 157, 179–189 (2016). https://doi.org/10.1007/s10549-016-3802-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3802-3