Abstract
Metabolic syndrome (MS), conventionally defined by the presence of at least three out of five dysmetabolic traits (abdominal obesity, hypertension, low plasma HDL-cholesterol, high plasma glucose and high triglycerides), has been associated with an increased risk of several age-related chronic diseases, including breast cancer (BC). This may have prognostic implications for BC survivors. 2,092 early stage BC survivors aged 35–70, recruited in eleven Italian centres 0–5 years after surgical treatment (1.74 years on average), were followed-up over 2.8 years on average for additional BC-related events, including BC-specific mortality, distant metastasis, local recurrences and contralateral BC. At recruitment, 20 % of the patients had MS. Logistic regression models were carried out to generate OR and 95 % confidence intervals (CI) for new BC events associated with MS, adjusting for baseline pathological prognostic factors. New BC events occurred in 164 patients, including 89 distant metastases. The adjusted ORs for women with MS versus women without any MS traits were 2.17 (CI 1.31–3.60) overall, and 2.45 (CI 1.24–4.82) for distant metastasis. The OR of new BC events for women with only one or two MS traits was 1.40 (CI 0.91–2.16). All MS traits were positively associated with new BC events, and significantly so for low HDL and high triglycerides. MS is an important prognostic factor in BC. As MS is reversible through lifestyle changes, interventions to decrease MS traits in BC patients should be implemented in BC clinics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) incidence is increasing and survival is increasing too [1, 2]. As a consequence, the prevalence of BC survivors is rocketing. An important proportion of BC survivors suffers from co-morbidities that affect the probability not only of dying from other causes, but also of dying from BC. In Western populations, about 2 % of women is living with BC [3, 4] and one third of them suffer from other chronic conditions [2]. A major determinant of the high prevalence of chronic diseases in Western countries is the so called Metabolic Syndrome (MS), conventionally defined as a cluster of dysmetabolic factors, such as abdominal obesity, hypertension, dyslipidemia and high fasting glycaemia [5], with, however, different threshold values adopted by different organizations [6]. Other traits of MS include hyperinsulinemia, insulin resistance, chronic inflammation, non-alcoholic fatty liver disease and in women, high androgen levels. MS, as well as its individual components, has been associated with BC risk in epidemiological studies. The ORDET cohort showed that after menopause the presence of MS is associated with a 2.6 (CI 1.5–4.6) times higher BC risk compared with the absence of any components of MS [7]. Women with MS (3 or more components) had a significantly higher risk of BC than women without MS (less than 3 components): HR 1.58 (CI 1.07–2.33). A recent meta-analysis of five studies showed that the risk of BC is 1.56 (P < 0.017) times higher in postmenopausal women with MS than in women without MS [8]. Obesity is a well-known risk factor for both MS and BC (after menopause [9]) and for BC recurrence and death both before and after menopause [10]. Recent meta-analyses estimated that obesity increases the risk of postmenopausal BC by 21 % [9, 11] and of death in BC patients by 33 % (CI 19–50 %), 22 % for postmenopausal BC and 47 % for premenopausal BC [10]. However, there is reason to suspect that the risk associated with MS is only partially explained by obesity.
Here we report on the prevalence of MS in breast cancer patients and on its association with additional BC-related events in a cohort of 2,092 women who volunteered to participate in a dietary intervention study following a diagnosis of invasive BC.
Materials and methods
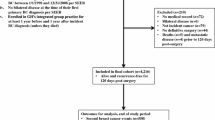
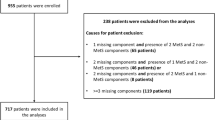
Between 2008 and 2012, 2,092 patients surgically treated for stage I–III invasive BC in the previous 5 years were enrolled into the ongoing DIANA-5 (Diet and Androgen-5) lifestyle intervention study [12] and followed-up to the end of 2013.
At baseline, they were aged 35–70 (mean age 51.4 ± 8.2 standard deviation), were not under chemotherapy, and had no evidence of recurrence. Eleven Italian institutions contributed patients to the study, seven in Northern Italy, one in Central Italy and three in the South (see Appendix). All participants received full information about the study, and provided a written consent.
At baseline, participating women provided a copy of their pathological report, filled-in a questionnaire on lifestyle and BC risk factors, and donated a fasting early morning blood sample to be stored in a centralised −80 °C bio-repository. Plasma glucose, triglycerides, total and HDL cholesterol, serum insulin and testosterone were measured utilizing the routine laboratory techniques of the participating centres. Height and body weight were measured without shoes and heavy clothes; waist circumference was measured with a measuring tape in the mid-point between the lowest rib and the iliac crest during expiration. Blood pressure was taken using the same electronic monitor in all centres. At enrolment, all women received the AICR/WCRF recommendations for the prevention of cancer through diet and physical activity (www.dietandcancerreport.org). They were basically recommended to avoid sugared drinks and processed meat, to limit red meat, calorie dense food, salted food and alcoholic beverages, and to eat predominantly vegetable food, with a variety of unrefined grains, legumes, seasonal vegetables and fruit. Seventy-one percent of patients were considered at high risk of recurrence because of hormonal or metabolic risk factors (oestrogen receptor negative tumours, or metabolic syndrome, or high plasma insulin or testosterone levels). A random sample of these women presumably at high risk was offered to take part in monthly meetings for cooking and exercise classes [12].
The women were followed-up for vital status and the occurrence of new BC events (loco-regional recurrences, distant metastasis and new primary BC), which were obtained by self-report every six months throughout the study and confirmed by a pathologist who examined the clinical and pathological records. In the present analysis, carried out after an average 2.8-year follow-up, we have considered the effects of the baseline characteristics on the study outcome.
Statistical analysis
Statistical analysis focused on the distribution of baseline variables in women with or without MS, and on the association of MS and its component factors with additional BC-related events.
Several different definitions of MS have been used by various investigators. In the present study, MS was defined on the basis of the presence of at least three components out of five, according to the thresholds proposed by the International Diabetic Federation for European women [5] (systolic blood pressure ≥130 and diastolic blood pressure ≥85 mmHg, fasting plasma glucose ≥100 mg/100 ml (5.6 mmol/l) or previously diagnosed type II diabetes, triglycerides ≥150 mg/100 ml (1.7 mmol/l), high-density lipoprotein <50 mg/100 ml (1.03 mmol/l) or receiving treatment for these components) except for waist circumference, for which we used the threshold of ≥85 cm instead of ≥80 cm, because the constitution of Italian women is not as lean as the constitution of the other European women [13]. We carried out, however, sensitivity analyses with different thresholds.
We used logistic regression models to estimate odds ratio (OR) and 95 % confidence intervals (CI). The models included the following covariates: age (4 classes), education (none or primary school, high school, degree or more), parity, oestrogen receptor (ER) and progesterone receptor (PR) status, Ki67 and disease stage at diagnosis (I, IIa, IIb and ≥IIIa). As in Southern Italy, the prevalence of MS is higher than in the rest of the country [14] and the survival of cancer patients is lower [15], we included the region of residence in the model. We analysed additional BC events all together and also separately for distant disease (metastasis). Moreover, we separately analysed the prognostic effect of MS in cases diagnosed with ER+ and ER− cancers, and in cases diagnosed before or after menopause.
In order to test if the association of MS with BC recurrences was mediated by body mass index (BMI), or by homoeostasis model assessment-insulin resistance (HOMA-IR) index, we further adjusted for these variables. HOMA-IR index was calculated by multiplying insulin level by glycaemia concentration and dividing by 22.5 [16].
In order to check whether the association was explained by a single MS component, we analysed every component separately and examined the effect of its exclusion from the MS definition.
The analyses were carried out using Stata (version 12) software. All tests were two-sided and statistical significance was set at P < 0.05.
Results
This cohort of 2,092 BC patients included 419 cases with MS, i.e. with three to five of the traits that define this dismetabolic condition, 962 cases with only one or two traits of MS and 711 cases without any of these traits at the time of recruitment.
Table 1 describes the pathological characteristics of BC at diagnosis and the metabolic characteristics of the participants at recruitment (baseline measurements).
The cases with MS were older (P < 0.001), and had more advanced disease at diagnosis than the cases without any traits of MS (P = 0.06). The cases with one or two traits showed intermediate figures.
Metabolic syndrome was significantly associated with menopause (P < 0.001) and with HOMA-IR index (P < 0.001). Among the five traits defining MS, the most prevalent were waist circumference and hypertension.
The average interval between diagnosis and recruitment into the study was 1.74 (±1.38 SD). In the course of 2.8 years of average follow-up, we registered 164 new BC events, including 89 distant metastases (among which 14 BC deaths), 31 local recurrences and 44 new primary contralateral BCs.
Table 2 shows the ORs of additional BC-related events according to the number of components of MS. Adjusting for age, stage at diagnosis and ER expression, women with MS at baseline had a 2.17 higher risk of developing BC recurrences (CI 1.31–3.60) than women without any MS traits. The OR for women with only one or two MS traits was 1.39 (CI 0.91–2.14). Further adjustments for region of residence, histological grade, PR and Ki67 did not materially change the results.
Restricting the analysis to distant metastases, the adjusted ORs were 2.45 (CI 1.24–4.82) for MS and 1.40 (CI 0.76–2.55) for patients with one or two MS traits.
In our analysis, BMI was not associated with an increase in BC recurrences (OR 1.18, CI 0.73–1.90 for obesity, and 0.92, CI 0.62–1.39 for overweight). As BMI is strongly correlated with waist circumference, which is incorporated in the MS definition, it would not be appropriate to adjust for BMI when analysing the risk associated with MS. Upon adjustment for BMI, however, the OR of MS increased (OR 2.74, CI 1.50–4.98 with respect to women without any MS traits). We found a non-significant positive association between HOMA-IR index and BC recurrences (OR 1.40, CI 0.95–2.05), and after adjustment for HOMA-IR index the OR of MS became 2.10 (CI 1.22–3.62), which suggests that the prognostic effect of MS is not largely explained by insulin resistance.
The association between BC recurrences and MS was similar in women diagnosed before or after menopause and in women recruited before or after the average age at recruitment (51.5 years) (data not shown).
In women with MS, the overall risk was 1.74 (CI 1.16–2.62) times higher than in women without MS (0–2 MS traits). Stratifying by ER status, we found that the risk of recurrences in presence of MS with respect to women without MS was mostly confined to ER-negative cases (OR 4.42, CI 1.70–11.50), while in ER+ cases MS was not significantly associated with recurrences (OR 1.48, CI 0.92–2.37). The interaction test, however, was not significant.
In the present study, MS was defined according to the criteria proposed by the International Diabetic Federation, except for waist circumference, for which we used the threshold of ≥85 cm instead of ≥80 cm. After repeating the analysis using, for waist circumference, the threshold of ≥80 cm in the definition of MS, the ORs of additional BC-related events with respect to women without any MS trait became 1.86 (CI 1.13–3.05).
Table 3 shows the adjusted OR associated with each of the five MS components: all were positively associated with the risk of recurrence, but only low HDL (OR 1.83, CI 1.24–2.70) and high triglycerides (OR 1.58, CI 1.01–2.46) were significantly associated, while fasting glycaemia, blood pressure and waist circumference were not. After reciprocal adjustment, low HDL remained significantly associated (OR 1.60, CI 1.06–2.41). The association of MS with prognosis, however, persisted significant even after excluding HDL cholesterol from the definition of the syndrome (data not shown).
Discussion
Our results suggest that the presence of MS was a major determinant of the occurrence of new BC events in this large cohort of patients operated for BC on average 1.7 years before recruitment. The risk of distant metastases was more than double in patients with MS than in patients without any dismetabolic traits. Such risk is likely to be rather the expression of a general dysmetabolic condition than of a specific dysmetabolic trait. The risk associated with the syndrome, in fact, was higher than the risk associated with any of its components. Each component, however, was associated with an increased risk. In the present dataset, the associations with waist circumference and with glycaemia were not statistically significant, but we and others have found a significant association with glycaemia in previous studies [17–19] and others have found that large waist circumference or waist-to-hip ratio predicts worse prognosis [20, 21].
The single MS component independently associated with recurrences was low HDL cholesterol level. The negative association of total cholesterol with the incidence of BC found in an old prospective study [22] was recently confirmed in the large Me-Can cohort (HR 0.70 CI 0.61–0.81) [23]. The association persisted after excluding the first ten years of follow-up, which indicates that reverse causation is not a likely explanation of the finding. In the French E3N cohort, women under cholesterol lowering drugs had a significantly lower risk of BC [24]. Several other studies, however, did not find the association [25–29]. Most studies suggested a negative association between HDL cholesterol and the subsequent occurrence of BC [30–32] but other studies did not find any association [33]. A study suggested an adverse effect of total cholesterol on BC prognosis [34], but we are not aware of any studies on the prognostic effect of HDL cholesterol.
Epidemiological studies did not usually find an increased risk of BC incidence associated with high plasma triglycerides levels [26, 27] nor an association with prognosis [34]. In the California Teachers Study cohort, the use of antihypertensive medication was associated with an increased risk of invasive BC [35]. In the DOM cohort, the increased risk was no longer statistically significant adjusting for BMI [36]. Hypertension was not associated with BC prognosis in the Shanghai BC Survival Study [37]. In a historical cohort study of women diagnosed with BC in the Kaiser Permanente Northern Californian Medical Care Program, hypertension was associated with total and BC-specific mortality (1.18 CI 1.03–1.35) [38].
In contrast with the above-inconsistent results on MS components and BC, the studies on MS consistently showed a positive association with postmenopausal BC incidence [7, 39–41]. The Osteoporotic Fracture Cohort of women aged ≥65 examined the association of the presence of 2 or 3 MS components with BC incidence by ER expression: the overall HR was 1.3 (CI 1.0–1.7), while the HR for ER-positive cancer was 1.5 (1.1–2.0). Triple negative tumours, however, have been found associated with MS more frequently than non-triple negative tumours [42].
We are not aware of any previous studies of MS and BC prognosis. Healy et al. [43] showed that BC patients with MS more frequently have adverse pathological features, such as advanced stage at diagnosis, nodal involvement and higher plasma levels of CRP. In the present study, however, the prognostic association persisted after adjusting for pathologic risk factors.
The mechanisms by which MS affects prognosis are likely to include higher sex hormone levels, higher levels of insulin and IGF-I, and chronic inflammatory status. Obesity, and particularly abdominal obesity, is associated with higher serum levels of insulin and of both androgens and oestrogens. Insulin stimulates the synthesis of androgens in the ovary. Elevated HOMA-IR scores and high serum levels of insulin and testosterone are associated with a high rate of recurrence and BC mortality [44–47]. Abdominal obesity is also associated with chronic inflammatory status and high circulating levels of C-reactive protein (CRP), and several studies showed an association of CRP levels with poor prognosis [48–50].
The finding that the negative prognostic effect of MS was mostly confined to ER-negative tumours was not unexpected. Goodwin et al. [46] found that high serum insulin levels were more strongly associated with poor prognosis in ER-negative cases, and Chlebowski [51] found that a low-fat diet conducing to weight loss was associated with a lower risk of recurrence only in ER-negative BC cases.
MS is a reversible condition associated with modern western lifestyle, a sedentary lifestyle with a diet characterized by high glycemic index food, sugared beverages and excess intake of proteins, saturated fats, trans fatty acids, salt and alcohol, while physical activity, omega-3 fatty acids and Mediterranean diet are protective. Randomized controlled trials consistently showed that Mediterranean diet can make MS regress [8]. The longest trial showed that the vast majority of MS cases regressed in patients treated with Mediterranean diet for two years [52].
BC clinics should consider offering BC patients with MS personalised nutritional advice in order to reduce MS parameters. Lifestyle recommendations may be particularly important for patients with ER-negative tumours.
References
De Angelis R, Sant M, Coleman MP et al (2014) Cancer survival in Europe 1999–2007 by country and age: results of EUROCARE-5-a population-based study. Lancet Oncol 15:23–34
Edwards BK, Noone AM, Mariotto AB et al. (2013) Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. doi:10.1002/cncr.28509
De Angelis R, Tavilla A, Verdecchia A et al (2009) Breast cancer survivors in the United States: geographic variability and time trends, 2005–2015. Cancer 115:1954–1966
International Agency for Research on Cancer (IARC) 2012 EUCAN http://eco.iarc.fr/EUCAN. Accessed 8 May 2014
Alberti KG, Eckel RH, Grundy SM et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120:1640–1645
Kassi E, Pervanidou P, Kaltsas G, Chrousos G (2011) Metabolic syndrome: definitions and controversies. BMC Med 9:48
Agnoli C, Berrino F, Abagnato CA et al (2010) Metabolic syndrome and postmenopausal breast cancer in the ORDET cohort: a nested case-control study. Nutr Metab Cardiovasc Dis 20:41–48
Esposito K, Chiodini P, Colao A, Lenzi A, Giugliano D (2012) Metabolic syndrome and risk of cancer: a systematic review and meta-analysis. Diabetes Care 35:2402–2411
World Cancer Research Fund, American Institute for Cancer Research (2007) Food, nutrition, physical activity and the prevention of cancer: a global perspective. AICR, Washington
Protani M, Coory M, Martin JH (2010) Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat 123:627–635
Cheraghi Z, Poorolajal J, Hashem T, Esmailnasab N, Doosti IA (2012) Effect of body mass index on breast cancer during premenopausal and postmenopausal periods: a meta-analysis. PLoS ONE 7:e51446
Villarini A, Pasanisi P, Traina A et al (2012) Lifestyle and breast cancer recurrences: the DIANA-5 trial. Tumori 98:1–18
Haftenberger M, Lahmann PH, Panico S et al (2002) Overweight, obesity and fat distribution in 50- to 64-year-old participants in the European prospective investigation into cancer and nutrition (EPIC). Public Health Nutr 5:1147–1162
Istituto Superiore Sanità (ISS) (2013). Progetto Cuore—http://www.cuore.iss.it. Accessed 8 May 2014
Verdecchia A, Sant M, Gatta G, Micheli A, Berrino F, ITACARE Working Group (1997) Survival in adult Italian cancer patients, 1978–1989. Tumori 83:39–425
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Contiero P, Berrino F, Tagliabue G et al (2013) Fasting blood glucose and long-term prognosis of non-metastatic breast cancer: a cohort study. Breast Cancer Res Treat 138:951–959
Goodwin PJ, Ennis M, Pritchard KI et al (2012) Insulin- and obesity-related variables in early-stage breast cancer: correlations and time course of prognostic associations. J Clin Oncol 30:164–171
Minicozzi P, Berrino F, Sebastiani F et al (2013) High fasting blood glucose and obesity significantly and independently increase risk of breast cancer death in hormone receptor-positive disease. Eur J Cancer 49:3881–3888
Borugian MJ, Sheps SB, Kim-Sing C et al (2003) Waist-to-hip ratio and breast cancer mortality. Am J Epidemiol 158:963–968
Kumar NB, Cantor A, Allen K, Cox CE (2000) Android obesity at diagnosis and breast carcinoma survival: Evaluation of the effects of anthropometric variables at diagnosis, including body composition and body fat distribution and weight gain during life span, and survival from breast carcinoma. Cancer 88:2751–2757
Vatten LJ, Foss OP (1990) Total serum cholesterol and triglycerides and risk of breast cancer: a prospective study of 24,329 Norwegian women. Cancer Res 50:2341–2346
Strohmaier S, Edlinger M, Manjer J et al (2013) Total serum cholesterol and cancer incidence in the metabolic syndrome and cancer project (Me-Can). PLoS ONE 8:e54242
Fagherazzi G, Fabre A, Boutron-Ruault MC, Clavel-Chapelon F (2010) Serum cholesterol level, use of a cholesterol-lowering drug, and breast cancer: results from the prospective E3N cohort. Eur J Cancer Prev 19:120–125
Hiatt RA, Friedman GD, Bawol RD, Ury HK (1982) Breast cancer and serum cholesterol. J Natl Cancer Inst 68:885–889
Manjer J, Kaaks R, Riboli E, Berglund G (2001) Risk of breast cancer in relation to anthropometry, blood pressure, blood lipids and glucose metabolism: a prospective study within the Malmo preventive project. Eur J Cancer Prev 10:33–42
Melvin JC, Seth D, Holmberg L et al (2012) Lipid profiles and risk of breast and ovarian cancer in the Swedish AMORIS study. Cancer Epidemiol Biomarkers Prev 21:1381–1384
Schatzkin A, Hoover RN, Taylor PR et al (1988) Site-specific analysis of total serum cholesterol and incident cancer in the national health and nutrition examination survey I epidemiologic follow-up study. Cancer Res 48:452–458
Tornberg SA, Holm LE, Carstensen JM (1988) Breast cancer risk in relation to serum cholesterol, serum beta-lipoprotein, height, weight, and blood pressure. Acta Oncol 27:31–37
Furberg AS, Veierod MB, Wilsgaard T, Bernstein L, Thune I (2004) Serum high-density lipoprotein cholesterol, metabolic profile, and breast cancer risk. J Natl Cancer Inst 96:1152–1160
Hoyer AP, Engholm G (1992) Serum lipids and breast cancer risk: a cohort study of 5,207 Danish women. Cancer Causes Control 3:403–408
Kucharska-Newton AM, Rosamond WD, Mink PJ, Alberg AJ, Shahar E, Folsom AR (2008) HDL-cholesterol and incidence of breast cancer in the ARIC cohort study. Ann Epidemiol 18:671–677
Gaard M, Tretli S, Urdal P (1994) Risk of breast cancer in relation to blood lipids: a prospective study of 31,209 Norwegian women. Cancer Causes Control 5:501–509
Bahl M, Ennis M, Tannock IF et al (2005) Serum lipids and outcome of early-stage breast cancer: results of a prospective cohort study. Breast Cancer Res Treat 94:135–144
Largent JA, Bernstein L, Horn-Ross PL et al (2010) Hypertension, antihypertensive medication use, and breast cancer risk in the California teachers study cohort. Cancer Causes Control 21:1615–1624
Peeters PH, van Noord PA, Hoes AW, Fracheboud J, Gimbrere CH, Grobbee DE (2000) Hypertension and breast cancer risk in a 19-year follow-up study (the DOM cohort). Diagnostic investigation into mammarian cancer. J Hypertens 18:249–254
Nechuta S, Lu W, Zheng Y et al (2013) Comorbidities and breast cancer survival: a report from the Shanghai breast cancer survival study. Breast Cancer Res Treat 139:227–235
Braithwaite D, Tammemagi CM, Moore DH et al (2009) Hypertension is an independent predictor of survival disparity between African–American and white breast cancer patients. Int J Cancer 124:1213–1219
Bjorge T, Lukanova A, Jonsson H et al (2010) Metabolic syndrome and breast cancer in the me-can (metabolic syndrome and cancer) project. Cancer Epidemiol Biomarkers Prev 19:1737–1745
Capasso I, Esposito E, Pentimalli F et al (2010) Metabolic syndrome affects breast cancer risk in postmenopausal women: national cancer institute of Naples experience. Cancer Biol Ther 10:1240–1243
Kabat GC, Kim M, Chlebowski RT et al (2009) A longitudinal study of the metabolic syndrome and risk of postmenopausal breast cancer. Cancer Epidemiol Biomarkers Prev 18:2046–2053
Maiti B, Kundranda MN, Spiro TP, Daw HA (2010) The association of metabolic syndrome with triple-negative breast cancer. Breast Cancer Res Treat 121:479–483
Healy LA, Ryan AM, Carroll P et al (2010) Metabolic syndrome, central obesity and insulin resistance are associated with adverse pathological features in postmenopausal breast cancer. Clin Oncol (R Coll Radiol) 22:281–288
Duggan C, Irwin ML, Xiao L et al (2011) Associations of insulin resistance and adiponectin with mortality in women with breast cancer. J Clin Oncol 29:32–39
Berrino F, Pasanisi P, Bellati C et al (2005) Serum testosterone levels and breast cancer recurrence. Int J Cancer 113:499–502
Goodwin PJ, Ennis M, Pritchard KI et al (2002) Fasting insulin and outcome in early-stage breast cancer: results of a prospective cohort study. J Clin Oncol 20:42–51
Micheli A, Meneghini E, Secreto G et al (2007) Plasma testosterone and prognosis of postmenopausal breast cancer patients. J Clin Oncol 25:2685–2690
Allin KH, Nordestgaard BG, Flyger H, Bojesen SE (2011) Elevated pre-treatment levels of plasma C-reactive protein are associated with poor prognosis after breast cancer: a cohort study. Breast Cancer Res 13:R55
Pierce BL, Ballard-Barbash R, Bernstein L et al (2009) Elevated biomarkers of inflammation are associated with reduced survival among breast cancer patients. J Clin Oncol 27:3437–3444
Villasenor A, Flatt SW, Marinac C, Natarajan L, Pierce JP, Patterson RE (2013) Postdiagnosis C-reactive protein and breast cancer survivorship: findings from the WHEL study. Cancer Epidemiol Biomarkers Prev 22(1):32–41
Chlebowski RT, Blackburn GL, Thomson CA et al (2006) Dietary fat reduction and breast cancer outcome: interim efficacy results from the women’s intervention nutrition study. J Natl Cancer Inst 98:1767–1776
Esposito K, Marfella R, Ciotola M et al (2004) Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA 292:1440–1446
Acknowledgments
We thank the Associazione Vita e Salute, the Fondazione Edo Tempia, the Italian League Against Cancer of Asti and of Busto Arsizio, and the Mantua ASL for logistic support, and dr Penci MT for language support.
Funding
The DIANA-5 study was financed by the Italian Department of Health, Programma Integrato Oncologia (PIO, RFPS-2006-1-339715), and by the Associazione Italiana per la Ricerca sul Cancro (AIRC, IG-2011-11942).
Conflict of interest
All Authors declare no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
The DIANA-5 working group include the authors and the following: Alessiato A, Amerio ML, Carretto R, Gavazza C, Lanfranco C, Micca GM, Piccarolo C, Rabino V, Sterpetti S, Tessa M, Testore F, Piccillo D, Pittarello E (Asti). Paduos A, Allegro G (Biella). Belloti E, Palestra M (Busto Arsizio). Anghinoni E, Arvati M, Bottura P, Chiesa M, Di Marco A, Iridile C, Manzato F, Orsini O, Pecini E, Prati C, Villani P, Volta F (Mantova). Aristarco V, Macis D, Passoni C, Sabbatini A, Serrano D, Varricchio C, Zagallo E (Milano European Institute of Oncology). Alquati E, Angarano A, Bellegotti E,Cavalleri A, Cogliati P, Consorti P, Curtosi P, Di Mauro MG, Ferrante L, Fornaciari G, Guerrini MG, Larossa M, Maule A (Milano National Cancer Institute). Belfiore A, Chiodini P, Cioffi E, d’Agostino MA, Santucci de Magistris M, Gentile M, Giallauria F, Mancini M, Mattiello A, Vigorito C, Vitelli A (Napoli). Campisi I, Dolcemascolo C, Staiti R (Palermo). Bianco T, Pera A, Pirovano DM, Pisanu G, Premori M, Premori P, Rainieri S, Soldi E. (Piacenza). del Riccio L, Napolitano D (Potenza). Bellati C, Feira S, Finocchiaro E, Pezzana A, Ponti A, Rizzi A, Segnan N (Torino).
Rights and permissions
About this article
Cite this article
Berrino, F., Villarini, A., Traina, A. et al. Metabolic syndrome and breast cancer prognosis. Breast Cancer Res Treat 147, 159–165 (2014). https://doi.org/10.1007/s10549-014-3076-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-3076-6