Abstract
This study examines the direct effects of neighborhood supportive mechanisms (e.g., collective efficacy, social cohesion, social networks) on depressive symptoms among females as well as their moderating effects on the impact of IPV on subsequent depressive symptoms. A multilevel, multivariate Rasch model was used with data from the Project on Human Development in Chicago Neighborhoods to assess the existence of IPV and later susceptibility of depressive symptoms among 2959 adult females in 80 neighborhoods. Results indicate that neighborhood collective efficacy, social cohesion, social interactions, and the number of friends and family in the neighborhood reduce the likelihood that females experience depressive symptoms. However, living in areas with high proportions of friends and relatives exacerbates the impact of IPV on females’ subsequent depressive symptoms. The findings indicate that neighborhood supportive mechanisms impact interpersonal outcomes in both direct and moderating ways, although direct effects were more pronounced for depression than moderating effects. Future research should continue to examine the positive and potentially mitigating influences of neighborhoods in order to better understand for whom and under which circumstances violent relationships and mental health are influenced by contextual factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intimate partner violence (IPV) and depression are major public health concerns that are both impacted by neighborhood context (Benson et al. 2003; Kim 2008; Mair et al. 2008; Miles-Doan 1998; Pinchevsky and Wright 2012; Ross 2000). The majority of extant research, however, has tended to focus on the direct and negative impact of neighborhoods on these outcomes, while little research has explored the potential protective effects of positive neighborhood conditions. For instance, there is some research which suggests supportive mechanisms such as social cohesion, social ties, or collective efficacy may protect individuals from IPV or depression and other mental health issues (Aneshensel and Sucoff 1996; Emery et al. 2011; Geis and Ross 1998; Kirst et al. 2015; Pinchevsky and Wright 2012; Ross and Jang 2000; Ross et al. 2000; Wright and Benson 2010, 2011), but most of these studies assess only neighborhood direct effects and treat these outcomes separately. Most notably for the current study, very little research has investigated the potential for neighborhood supportive features to moderate important individual-level relationships, such as the impact of IPV on subsequent depression.
Thus, while we know that neighborhoods can detrimentally impact IPV and depression (Latkin and Curry 2003; Mair et al. 2008; Pinchevsky and Wright 2012), we know less about the positive impact that neighborhood supportive features might have on these problems. Additionally, we do not know whether, or how, neighborhood supportive mechanisms moderate the impact of IPV on subsequent depression. We attempt to add to the sparse research in this area by examining the relationship between intimate partner violence and subsequent depression in neighborhood context. We use data from 2959 females living in 80 neighborhoods in Chicago to investigate the direct effects of neighborhood supportive mechanisms, such as collective efficacy, social cohesion, and interactions with others, on females’ depressive symptoms, as well as to explore whether neighborhood context alleviates the long-term impact of experiencing IPV on later depression among these adults.
Intimate Partner Violence Victimization and Depression
Scholars have suggested that victims of partner violence may be particularly susceptible to experiencing mental health problems in the aftermath of abuse in part because their victimization (and the associated trauma) is inflicted by people whom the victim trusts, loves, or considers to be “safe” (DeMaris and Kaukinen 2005). Along with post-traumatic stress disorder, depression is among the most prevalent mental health consequences of IPV (Caldwell et al. 2012; Campbell 2002), with over 45 % of victims experiencing it (Golding 1999). Although depression among victims may decline if and when the victimization does, long-term effects do linger, but more research in this area is needed, especially among adult populations (Bonomi et al. 2006; Campbell 2002; Coker et al. 2002a; Fletcher 2010; Johnson et al. 2014).
Violence from partners can be linked to depression via mechanisms such as stress, powerlessness, hopelessness, isolation, low self-esteem, and physical pain (Campbell et al. 1996; Goodman et al. 2009). As a source of stress, abuse can contribute to depression by disrupting daily routines, increasing other stressful events in one’s life, lowering the victim’s feelings of security and sense of self-esteem, or increasing their feelings of powerlessness to control the situation (Campbell 2002; Campbell et al. 1996; Goodman et al. 2009). For instance, because of the physical pain and injury that is often a consequence of IPV, victims may develop chronic pain or suffer consequences of the abuse (e.g., episodes of fainting caused by extensive head trauma; sexually transmitted diseases, etc., see Campbell 2002), which may lead to depression over time. In addition, social isolation from others, which is often purposefully achieved by abusers in violent relationships (e.g., Campbell et al. 1996), can also lead to depression because isolated victims may feel that they have no one to turn to for help or support. While there are many avenues by which IPV may lead to depression and other negative mental health dispositions, few studies have examined such relationships with longitudinal data among adults, and more assessment is needed in this area (Campbell 2002; Fletcher 2010). Moreover, research has neglected to examine this relationship from a contextual perspective.
The Importance of Neighborhood Context
Neighborhood context is related to depression and other problematic mental health outcomes among both adults (e.g., Kim 2008; Mair et al. 2008) and children (e.g., Xue et al. 2005). The literature regarding the neighborhood predictors of depression tends to center on socioeconomic, poverty-related, or social disorder variables, and generally demonstrates that lower socioeconomic status (SES) and more neighborhood disorder detrimentally impact depression and other negative mental health outcomes. Mair et al. (2008) found that, of 45 studies on neighborhoods and depression, 37 demonstrated significant neighborhood effects, even after controlling for individual-level factors such as age, race, gender, and indicators of socioeconomic status; in another review, Kim (2008) found that 11 of 22 studies examining neighborhood socioeconomic status showed that neighborhood conditions had significant effects on depression. Mechanisms directly linking neighborhood factors to mental health or depression often revolve around increased stress levels, limited access to or scant resources, disorder, violence, inadequate housing, and a lack of public access or green spaces, such as bike lanes and clean streets or sidewalks (e.g., Kim 2008; Mair et al. 2008; Taylor and Repetti 1997). Accumulating evidence also suggests that perceived disorder and/or dangerousness of the neighborhood increases depression, perhaps in part due to increased fear or mistrust among neighbors (e.g., Ross and Jang 2000; Ross and Mirowsky 2009), social isolation (e.g., Geis and Ross 1998; Ross and Mirowsky 2009), feelings of powerlessness (e.g., Aneshensel and Sucoff 1996; Geis and Ross 1998), or fear and anxiety amongst neighbors (e.g., Hill et al. 2005). In short, unkempt, rundown, disorderly, and disorganized neighborhood environments can be demoralizing, distressing, threatening, and isolating to residents and can send the message that no one cares about their wellbeing or that of the neighborhood (Ross and Mirowsky 2009; Sampson 2013; Wilson and Kelling 1982). All of these factors might, in turn, contribute to depression.
Despite the deleterious effects of neighborhoods on negative outcomes, it is also possible that neighborhoods may mitigate the effects of stressors—including violence such as IPV—by organizing community residents together and fostering social cohesion and/or interconnectedness among them. There is some evidence supporting neighborhood protective effects against mental health outcomes, but this body of research primarily focuses on neighborhood cohesion and collective efficacy. In their review, Mair et al. (2008) found 11 studies that reported that positive interactions between neighbors—including increased social connections and support from residents, increased communication between residents, and reduced social isolation—served as protective factors against depression. Ross and colleagues (Kim and Ross 2009; Ross and Jang 2000) have demonstrated that neighborhood social ties and social support reduce depression and other psychological distress, including perceived powerlessness, fear, and mistrust (see also Kim 2010). Neighborhood social cohesion has also been linked to reduced depression (Mair et al. 2010); Ahern and Galea (2011) suggest that social cohesion within a neighborhood may help residents exert social control, which can provide more support between neighbors, reduce the number of stressors that residents perceive to exist within the neighborhood, and buffer or mitigate the stressors which do occur. Further, they note that cohesion between residents may foster communication—which can keep residents knowledgeable about their community—improve the local services and resources that are available, and increase a personal sense of control, which in turn, can alleviate depressive symptoms (Stafford et al. 2011). Areas where residents know each other, communicate, and interact are, in fact, perceived to foster better mental health among residents: for instance, Toronto residents perceived concepts such as “interaction between neighbors,” “knowing neighbors,” “social cohesion,” and “communication between residents” to be important pieces of neighborhood support which were thought be related to positive mental health (Burke et al. 2009). Indeed, Sampson (2013) suggests that residents in neighborhoods of high collective efficacy (i.e., where there are shared expectations about norms and behavior) are better able to achieve common goals and are more likely to engage in (and benefit from) socially altruistic behaviors.Footnote 1 Such benefits are unsurprisingly associated with better mental health—collective efficacy, for instance, has been found to reduce depression among long-term Latino immigrants in the United States (Vega et al. 2011) as well as among older adults (Ahern and Galea 2011), and is associated with other socially altruistic behaviors such as bystander intervention (Edwards et al. 2014).
It is necessary to account for neighborhood disadvantage when examining the impact of neighborhood protective factors, however, because disadvantage can impede the quality and quantity of the helping mechanisms which are available (Goodman et al. 2009; Sampson 2003). In other words, the mechanisms described above that might mitigate depression among residents may be less likely to be present in disadvantaged neighborhoods. For instance, scholars have suggested that the formation and extent of social ties between residents may be lower in disadvantaged areas (see Kornhauser 1978; Shaw and McKay 1942) potentially because of their fear, mistrust, and perceptions of dangerousness (Ross and Mirowsky 2009; Ross et al. 2001). Having few or weak social ties between neighbors might reduce help-seeking behaviors among victims of partner violence.
Additionally, some of the literature on neighborhood protective effects on depression and mental health outcomes has been limited in other ways. For instance, data that is reported by participants but aggregated to the neighborhood level (e.g., Echeverria et al. 2008; Mair et al. 2010; Rios et al. 2012) risks conflating outcomes with predictor variables (i.e., neighborhood measures). While the research base has examined both neighborhood-level ties and supports, there have also been studies which focus on ties and supportive mechanisms at the individual-level only or use aggregated measures (e.g., Echeverria et al. 2008; Geis and Ross 1998; Rios et al. 2012; Ross and Jang 2000). Further, many studies have utilized cross-sectional designs (Mair et al. 2008), which cannot ascertain whether neighborhood supportive mechanisms precede increased depression or whether people seek out support to help with their depression. Most importantly to the current study, research has neglected to examine the effects of neighborhood supportive mechanisms on the IPV—depression relationship specifically.
Neighborhood Supports May Mitigate the Effect of Partner Violence on Later Depression
We examine whether the relationship between IPV and subsequent depression depends in part upon the neighborhood in which it occurs. Based on previous research and theory, we might expect that neighborhood supportive mechanisms, such as strong social cohesion, collective efficacy, or social networks between residents will both directly decrease depression and alleviate the effects of IPV on depression, despite the level of disadvantage that exists within a neighborhood. Although we do not directly test these mechanisms, we suspect that these neighborhood protective factors will increase the support that is available from others to the victim, leading to lower depression and an attenuated impact of IPV on this outcome. Indeed, Kirst et al. (2015) found that Toronto residents with high perceived social support and larger social networks to draw upon were less likely to experience IPV. Wright (2012) suggested that victims of partner violence may rely on social support from others for emotional and financial help when abuse occurs, and that these support systems may aide the victim in leaving the abusive relationship temporarily or permanently. In addition, supportive networks with others may provide victims with advice regarding safe places to go or the services that are available to them in order to escape the violence (Hadeed and El-Bassel 2006; Moe 2007; Wright 2012). In short, neighborhood supportive mechanisms may provide options for victims to rely on when in need. Second, we believe that communication with residents in the neighborhood may increase the likelihood that victims tell others about their victimization (Browning 2002), and this open communication may help victims cope (Coker et al. 2002b) as well as increase the likelihood that others will learn about the victimization and potentially intervene (Wright 2012; Wright and Benson 2011). Having more avenues available to victims for coping with the violence or seeking help to alleviate the abuse may reduce the stress caused by the victimization. Finally, supportive neighborhoods may reduce residents’ feelings of isolation and/or mistrust, which in turn may reduce victims’ feelings of powerlessness.
We examine these possibilities in the current study and focus on three research questions: (1) what are the long-term effects of experiencing intimate partner violence on the likelihood that females later report depressive symptoms, while controlling for other important individual and neighborhood covariates? (2) what are the direct effects of neighborhood supports (e.g., collective efficacy, social cohesion, and social networks with others) on females’ depressive symptoms, accounting for individual covariates and neighborhood disadvantage? and (3) do these neighborhood supportive mechanisms alleviate the impact of IPV on depressive symptoms 3 years later, after controlling for relevant individual and neighborhood covariates?
Methods
Data
Data for this study were drawn from the Project on Human Development in Chicago Neighborhoods (PHDCN; Earls et al. 2002), a multi-component, multi-wave study which allows for the examination of how neighborhood context may impact individual-level outcomes. This study relies on data from three separate components of the PHDCN: the Longitudinal Cohort Study (LCS), the Community Survey, and the 1990 U.S. Census. PHDCN researchers divided Chicago’s 847 census tracts into 343 geographically continuous neighborhood clusters (NCs). These 343 NCs were then stratified by seven categories of racial/ethnic diversity and three levels of socio-economic status, and 80 NCs were then selected via probability sampling. Within these 80 NCs, multiple cohorts of eligible youth and their primary caregivers (93 % of whom were female) were selected for inclusion in the LCS. The current study utilizes data collected from female caregivers (hereafter referred to as respondents) during the first (1994–1997) and second (1997–2000) waves of the LCS.
Neighborhood measures related to collective efficacy, cohesion, and social interactions or ties were taken from the PHDCN Community Survey while measures for neighborhood disadvantage were abstracted from the 1990 United States Census.Footnote 2 The Community Survey (conducted in 1994–1995) sampled residents from the original 343 NCs and asked about their perceptions of neighborhood social processes, including social networks and interactions between residents, organizational groups, values, and so forth. Using a three-stage sampling design, city blocks were sampled within each NC, dwelling units were sampled within blocks, and one adult resident was sampled within each dwelling unit. Thus, participants of the Community Survey were largely independent of those drawn for the LCS.Footnote 3 The current study includes 2959 female respondents living in 80 neighborhood clusters (hereafter referred to as neighborhoods) who were married, cohabitating, or in a dating relationship at wave one and answered questions related to depressive symptoms at wave two.Footnote 4
Measures
Depression Symptoms
Thirteen depression measures were adapted from the short form of the Composite International Diagnostic Interview (UM-CIDI; Kessler et al. 1998) and were self-reported by the female respondents at wave two. Respondents were first asked questions regarding whether they had felt sad, blue, or depressed for two or more weeks in a row during the past year. If respondents answered affirmatively, they were asked follow-up questions regarding the period of time they experienced depressive symptomology (i.e., during the 2-week period when they felt sad or blue, did they lose interest in most things; feel tired or have low energy; experience a weight change of 10 or more pounds; have trouble falling asleep or concentrating; experience feelings of worthlessness; think about death). Respondents were also asked the same follow-up questions regarding any 2-week (or more) period of time in the past year when they lost interest in most things like hobbies, work, or activities that they usually enjoyed. This 13-item scale had a reliability of .902.
To predict the odds of experiencing depressive symptoms, we used a multivariate, multilevel Rasch model (Raudenbush et al. 2003). The three-level model nests depression item responses within persons within neighborhoods. The level-1 model (items within persons) produces a latent variable that represents each person’s susceptibility for depression symptoms (i.e., their likelihood of experiencing depressive symptoms). This continuous variable is assumed to be normally distributed on a logit metric and is the outcome for the level-two (respondent-level) and level-three (neighborhood level) models (Osgood et al. 2002).
Intimate Partner Violence
Severe IPV was assessed using the Conflict Tactics Scale for Parents and Spouses (Straus 1979) and reflects the prevalence of severe male-partner-perpetrated aggression against the female respondent in the past year. Respondents reported whether their male partner used any of six forms of severe aggression or violence against them in the past year: hit with a fist, hit with something, beat up, choked, threatened with a knife or a gun, or used a knife or a gun (0 = no; 1 = yes). This measure reflects partner victimization at wave one.
Neighborhood Variables
Drawing from prior research (Cerda et al. 2008; Molnar et al. 2004, 2008), concentrated disadvantage was operationalized as a principal components factor analysis including the percentage of residents in a neighborhood who were living below the poverty line, receiving public assistance, and unemployed (alpha = .805). Higher values reflect greater economic disadvantage. Because of the possible confounding effects of disadvantage on neighborhood social support mechanisms, concentrated disadvantage is largely included as a control measure.Footnote 5
We use two measures that reflect the degree of trust and support between neighbors in the community. Following Sampson et al. (1997), neighborhood collective efficacy was based on 10 items from adults participating in the Community Survey and reflects the degree of social cohesion and informal social control between neighbors. Residents were asked how strongly they agreed (on a five-point Likert scale ranging from “strongly disagree” to “strongly agree”) that: people around here are willing to help their neighbors; this is a close-knit neighborhood; people in this neighborhood can be trusted; people in this neighborhood generally don’t get along with each other (reverse coded); and people in this neighborhood do not share the same values (reverse coded). Residents were also asked five items regarding the likelihood (assessed on a five-point Likert scale from “very unlikely” to “very likely”) that their neighbors would intervene if: children were skipping school and hanging out on a street corner; children were spray painting graffiti on a local building; children were showing disrespect to an adult; a fight broke out in front of their house; and the fire station closest to their home was threatened with budget cuts. Following Sampson et al. (1997) and others (Browning et al. 2004; Morenoff et al. 2001), these items were combined into a single measure of collective efficacy using a three-level item response model.Footnote 6 The level-one model adjusted the within-person collective efficacy scores by item difficulty, missing data, and measurement error. The level-two model estimated neighborhood collective efficacy scores adjusting for the social composition of each neighborhood. In particular, potential biases in perceptions of each construct resulting from characteristics related to gender, marital status, homeownership, ethnicity and race, residential mobility, years in the neighborhood, age, and socioeconomic status were controlled at level-two. Finally, the level-three model allowed each neighborhood cluster’s mean collective efficacy score to vary randomly around a grand mean. The empirical Bayes residual from the level-three model constitutes the neighborhood level of collective efficacy after controlling for item difficulty and neighborhood social composition and was therefore used as the ‘true’ neighborhood score on collective efficacy. The internal consistency of this scale at the neighborhood level was .847.
It has been suggested that cohesion between residents may uniquely impact their mental well-being (Stafford et al. 2011), and Kirst et al.’s (2015) findings suggest there are unique contributions of different forms of neighborhood social capital (e.g., collective efficacy, perceived social support, individual network size) with regard to IPV. Therefore, we wished to separate out the effects of social cohesion from social control, as both are captured in the overall collective efficacy measure described above.Footnote 7 We created a separate measure of social cohesion, apart from the collective efficacy measure, and modeled them separately in the analyses. Social cohesion was based on five items asked of the Community Survey participants; residents were asked how strongly they agreed (from “strongly disagree” to “strongly agree”) that: people around here are willing to help their neighbors; this is a close-knit neighborhood; people in this neighborhood can be trusted; people in this neighborhood generally don’t get along with each other (reverse coded); and people in this neighborhood do not share the same values (reverse coded). Independently from collective efficacy, social cohesion was also operationalized using a three-level item response model. As described above, the empirical Bayes residual from the three-level model constitutes the neighborhood score on social cohesion after controlling for social cohesion item-difficulty and neighborhood social composition (e.g., respondent characteristics such as age, race, etc.). The neighborhood-level internal consistency of this scale was .826.
One item tapping the level of social interaction between neighbors was also included in this study. Adults participating in the Community Survey were asked four questions about their social interactions with other neighborhood residents. Respondents were asked how often (on a four-point Likert scale, from “never” to “often”) they and people in the neighborhood: do favors for each other; ask each other advice about personal things; have get-togethers where other people in the neighborhood are invited; and visit in each other’s homes or on the street. Similar to the other neighborhood social processes variables, a three-level item response model was used to create the social interactions scale (see Browning et al. 2004). The internal consistency of this scale at the neighborhood level was .734.
Finally, three measures were included to assess the existence of friend and family social ties in the neighborhood. These measures were also taken from the Community Survey. Any friends and any family were computed based on residents’ answers to whether they had any friends and any relatives or in-laws, respectively, living in their neighborhood (excluding those friends or family members with whom they lived). These responses were then aggregated to the neighborhood-level. Finally, the average number of friends and family represents the number of friends and family/in-laws living in the neighborhood (each on a scale of 0–4, indicating none to 10 or more friends or family/in-laws) averaged, and aggregated to the neighborhood-level.
Control Variables
Additional respondent-level factors demonstrated in prior research to be associated with the odds of depression and intimate partner violence were also included in analyses (Stith et al. 2004). Such variables include demographic predictors (age, race/ethnicity, married [versus dating or cohabiting with a partner], household salary, and employment status), opportunity variables (isolation), and prior life histories (stressful life event, prior depression). Importantly, prior depression (a yes/no indicator self-reported by the respondent) was assessed at wave one, while the depressive symptoms outcome was assessed at wave two, which allowed us to control for the temporal ordering between current and prior depression. Table 1 provides additional information about these control variables.
Statistical Analyses
Following Raudenbush et al. (2003), Sampson et al. (2005), and others (Zimmerman and Messner 2010, 2011), we employ a multilevel logistic regression model to predict the odds that a respondent living in a given neighborhood will report experiencing depressive symptoms. This allows us to utilize all 34,766 responses to the wave two depression symptom items provided by all 2959 of the females living in 80 neighborhoods in our sample. Thus, our analytic technique includes any female who responded to at least one depression symptom item asked at wave two. This technique effectively avoids the loss of data due to missing item responses (Osgood et al. 2002) and takes item difficulty into account (i.e., some depression symptoms are less prevalent than others) (Sampson et al. 2005).
The multivariate multilevel Rasch model is a three-level model in which dichotomous depression items are nested within persons, who are nested within neighborhoods (Raudenbush et al. 2003). The level-one outcome is the log-odds of responding affirmatively to item i of m − 1 depression items, by j person, living in k neighborhood. This variable locates item severities on the logit scale (Raudenbush et al. 2003). Thus, the level-one model adjusts the within-person propensity for depressive symptoms by item severity, missing data, and measurement error. The level-one intercept serves as the outcome for the level-two and level-three models and is assumed to be normally distributed on a logit scale.
The level-two model examines the effects of person-level correlates (e.g., age, marital status, severe IPV) on the level-one intercept (susceptibility for depressive symptoms), while also controlling for item severities at level-one. All of the person-level effects were grand-mean centered. For the neighborhood direct effects models, the effects of all covariates were assumed to be fixed across neighborhoods; however, the analyses examining the cross-level interactions allowed the effect of experiencing severe IPV to vary across neighborhoods (p < .05).
The level-three model allows estimation of the susceptibility of depressive symptoms across neighborhoods. The level-three intercepts-as-outcomes model examines the direct effects of neighborhood disadvantage and supportive mechanisms on the level-two intercept (i.e., the susceptibility of experiencing depression symptoms, controlling for person-level correlates at level-two and item severities at level-one). The level-three slopes-and-intercepts-as-outcomes model allows for examination of the cross-level interaction between neighborhood supportive mechanisms and the level-two relationship between experiencing severe IPV and susceptibility for experiencing depression symptoms, while adjusting for the individual and neighborhood main effects. Multicollinearity was not a problem in any of the models (tolerance values were above .40).
Results
Tables 2 and 3 present the results of our three research questions. Table 2 presents the main effect of experiencing severe IPV from one’s partner at wave one on depressive symptoms approximately 3 years later, controlling for neighborhood variables as well as individual-level factors, such as prior depression and marital status. These analyses do not include the cross-level interaction between neighborhood supportive mechanisms and the IPV—depression relationship. The results of the individual-level models suggest that, as expected, experiencing severe abuse from one’s partner significantly increases the likelihood that females will report subsequent depressive symptoms; importantly, this effect is significant even after controlling for the impact of prior depression. Additionally, struggling with prior depression (compared to not reporting prior depressive symptoms), experiencing a stressful life event (versus not experiencing such events), and having higher household salaries (as opposed to lower salaries) increased the likelihood of experiencing depressive symptoms across all models. Being married (as opposed to dating or cohabiting with a partner) protected women against experiencing depressive symptoms across all models.
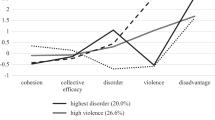
In the bottom half of Table 2, we provide the neighborhood direct effects on depressive symptoms, controlling for the main effect of neighborhood disadvantage and respondent-compositional factors in all analyses. Results of the neighborhood direct effects indicate that many of the neighborhood supportive mechanisms are, in fact, protective against experiencing depressive symptoms, even when neighborhood disadvantage and individual-level prior depression are taken into account. Specifically, women who reside in neighborhoods characterized by higher levels of collective efficacy (Model 1), social cohesion (Model 2), social interactions between residents (Model 3), and neighborhoods in which many people had friends and family members (Model 6) were less likely to report experiencing depressive symptoms than women residing in neighborhoods characterized by less collective efficacy, cohesion, networks, and fewer friends or family members on average. Neighborhood concentrated disadvantage was also significantly (though modestly) associated with a lower likelihood of depressive symptoms when collective efficacy (Model 1) and social cohesion (Model 2) were also included in the analyses, though it was not directly related to depressive symptoms in any of the other models.
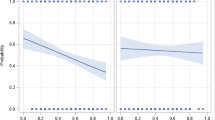
In Table 3, we include the cross-level interactions between neighborhood supports and the IPV—subsequent depression relationship. These are reported in the rows below the Severe IPV variable. These interactions are assessed simultaneously with the individual and neighborhood main effects. No substantive changes in the individual or neighborhood main effects were observed when the cross-level interaction was included in Table 3. As mentioned above, the impact of experiencing severe IPV from one’s partner in fact varied across neighborhoods, and was allowed to vary for the cross-level interaction models (as indicated by the italicized coefficients). The purpose of examining the cross-level interactions was to determine if neighborhood supportive mechanisms, such as collective efficacy, explained this variation, perhaps by mitigating the impact of IPV on depressive symptoms. We found very little evidence that neighborhood supportive mechanisms alleviated the impact of IPV on subsequent depression, and the only two significant moderating effects we found were somewhat counterintuitive. Model 5 in Table 3 indicates that the impact of experiencing severe IPV on later depressive symptoms was significantly stronger for women who resided in neighborhoods characterized by greater proportions of family members in the neighborhood (as reported by respondents of the Community Survey, not the respondents of IPV), while Model 6 demonstrates that the influence of IPV on depressive symptoms was also stronger for women living in neighborhoods characterized by higher average numbers of family and friends living in the same neighborhood (though this effect was modest, reaching significance at the p ≤ .10 level).
Figure 1 depicts the cross-level interaction displayed in Model 5 of Table 3, while Fig. 2 depicts the cross-level interaction in Model 6. As shown, the relationship between IPV and the likelihood of experiencing depressive symptoms was steep and positive in neighborhoods characterized by high (one standard deviation above the mean) family associates (Fig. 1) and friends and family members (Fig. 2) in the neighborhood. The impact of IPV on depressive symptoms weakened (as indicated by the slope tilting in the negative direction) in areas characterized by low (one standard deviation below the mean) family members (Fig. 1) and family and friends (Fig. 2). Thus, although we expected that neighborhood supportive mechanisms, such as ties with others, would potentially shield victims from experiencing depressive symptoms, we found the opposite effect – in some neighborhoods, particularly those characterized by high levels of family members, the impact of being a victim of partner violence on later depressive symptoms was actually worse.
Discussion
Many scholars agree that neighborhood context is important when it comes to both intimate partner violence and depression (or other mental health problems) (e.g., Benson et al. 2003; Goodman et al. 2009; Kim and Ross 2009), and a number of studies have examined the negative or detrimental impacts of neighborhoods with regard to these outcomes (e.g., Mair et al. 2008; Miles-Doan 1998). However, less attention has been paid to the potential protective or health-promoting effects that some types of neighborhoods provide for their residents (for exceptions, see for instance, Ahern and Galea 2011; Kim 2010; Kim and Ross 2009; Mair et al. 2008, 2010; Ross and Jang 2000; Stafford et al. 2011). Additionally, the interplay of partner violence, neighborhood supportive mechanisms, and depressive symptoms, to our knowledge, has not been assessed, limiting our understanding for how the IPV—depression relationship operates when neighborhood context is considered. Our study sought to advance this literature by exploring whether neighborhood supportive mechanisms alleviated the detrimental impact of IPV on subsequent depressive symptoms. Our results suggest that the impact of violent relationships on later mental health outcomes may depend in part on neighborhood characteristics, particularly social ties, but contrary to our expectations, the presence of high levels of neighborhood ties appeared to strengthen rather than attenuate the relationship between IPV and depressive symptoms. We did find, however, that neighborhood supportive mechanisms, particularly those related to collective efficacy, cohesion, and social interactions with neighbors, alleviated the likelihood of experiencing symptoms of depression even after controlling for the effects of prior depression. We discuss our findings below.
Our first goal was to examine the long-term impact of IPV on depressive symptoms using longitudinal data, as few studies have assessed the prospective impact of violent relationships on such an outcome (Campbell 2002; Fletcher 2010; Johnson et al. 2014). We found that experiencing severe IPV significantly increased the likelihood that women reported depressive symptoms years later. The relationship between IPV and depression was robust, maintaining a significant effect despite highly specified models which included several other important covariates, such as prior depression and, perhaps even more importantly, while simultaneously investigating contextual influences (Goodman et al. 2009). Given the strength of our multilevel longitudinal models, our results demonstrate that IPV is a significant risk factor for subsequent mental health problems that is independent from the effects of other predictors of depression, such as prior depression, stressful life events, and isolation. That IPV maintained a strong longitudinal effect on depression in these models suggests that it remains a central public health concern (see also Bonomi et al. 2006; Caetano and Cunradi 2003; DeMaris and Kaukinen 2005; Golding 1999).
Our next goals were to examine several neighborhood-level protective factors—particularly those measuring social connections and cohesiveness among neighbors—which have been suggested as mechanisms that might alleviate mental health symptoms and/or the effects of abuse (Ahern and Galea 2011; Burke et al. 2006; Mair et al. 2008; O’Campo et al. 2005; Stafford et al. 2011). We sought to examine both the direct and moderating influences of these neighborhood characteristics while controlling for important individual-level covariates. Consistent with prior research reporting a direct influence of neighborhoods on depression (e.g., Kim 2010; Mair et al. 2008), we found that neighborhood supportive mechanisms do appear to protect individuals from experiencing symptoms of depression. We suspect that neighborhood factors such as collective efficacy, social cohesion between neighbors, social interactions among residents, and having more family and friends who reside in one’s neighborhood are protective against negative mental health symptoms because they provide support, increase communication, and lower feelings of isolation (e.g., Browning 2002; Sampson 2013; Vega et al. 2011). As sources of support, these ties might also reduce the effects of stress, increase feelings of control, foster altruistic behaviors, or reduce feelings of fear or mistrust, all of which in turn might alleviate feelings of depression (Ahern and Galea 2011; Kim and Ross 2009; Ross and Jang 2000; Sampson 2013; Stafford et al. 2011).
However, we also found that some neighborhood supportive mechanisms are not necessarily protective against depression, particularly when partner violence is concerned. Living in neighborhoods where greater proportions of family members (relatives or in-laws) resided actually exacerbated the negative impact of IPV on depressive symptoms among females. Likewise, we found that women who lived in neighborhoods characterized by higher proportions of family and friend ties were more at-risk for depressive symptoms following IPV than women whose neighborhoods were characterized by fewer such “supports.” While the “family” element may be largely driving this last finding, we still consider both effects noteworthy and unexpected. Although neighborhood social ties—particularly between family and/or friends—is largely deemed a protective mechanism for many outcomes (e.g., Bellair 1997; Wellman and Wortley 1990), including both partner violence (e.g., Agoff et al. 2007; Wright 2012) and depression (e.g., Kim and Ross 2009), we found the opposite to be true, at least regarding the impact of IPV on depressive symptoms. A few possibilities may account for these contradictory findings. Recall that the Community Survey sampled respondents from neighborhoods who were not necessarily participants of the LCS—thus, “family” ties in the neighborhood likely do not reflect the victim’s own family members—they simply reflect that such ties exist within the neighborhood. In this case, women who are being victimized may not have their own family members living close by. Indeed, it is possible that the IPV victims in these neighborhoods actually may have felt doubly isolated if they had no local family or friends while everyone around them was strongly tied into a local familial (or friendship) network. We sought to take this possibility into account, however, by including the females’ level of isolation as an individual-level control. That it was not significant in our models suggests another explanation is warranted. For instance, we do not know if the victimized female actually utilized these ties for help. While some (Browning 2002; Van Wyk et al. 2003; Wright and Benson 2011) have suggested that more social ties may make it more likely that the violence will become public knowledge, it may be that these ties were simply not activated or sought out for help (Wright and Benson 2011). Since IPV is often times considered very private in nature (Straus et al. 2006), this is certainly a possibility. It is also possible that being surrounded by more family ties (even if not one’s own family members) in one’s neighborhood puts pressure on women to stay in the relationship, especially if families in the area do not condone divorce or separation, even from a violent partner (Agoff et al. 2007). Alternatively, it is possible that in the context of partner violence, some social supports are not helpful, and may in fact be harmful by supporting or condoning the use of violence within relationships. We are unable to examine whether the neighborhood ties measured here are supportive of IPV, and therefore cannot test this potential explanation. If the social ties in the neighborhoods were between residents who were supportive of violence in relationships, this could explain the exacerbating effect found between neighborhood social ties and the impact of IPV on later depression. We cannot be sure which explanation, if any, is correct given the available data, but we encourage future research to attempt to disentangle the complex relationship that appears to exist between neighborhood-level social ties (especially with family or relatives) and partner violence.
Aside from the effect of family and friends, we found no other evidence that neighborhood supportive mechanisms (collective efficacy, social cohesion, social interaction) moderated the impact of IPV on subsequent depression. Perhaps the neighborhood supportive mechanisms examined here are too general to alleviate the effects of IPV on mental health—it is possible that other neighborhood constructs geared more specifically to violence and mental health support, intervention, and/or prevention (e.g., counseling services, shelters, etc.) would be more relevant. Future research should consider the potential for such neighborhood supportive mechanisms to ease the effects of specific violence stressors such as IPV and abuse on negative mental health outcomes so that aggregate prevention and interventions can be implemented (see also Cunradi 2010).
Limitations
Unfortunately, our study is not without limitations. We relied solely on data from female caregivers and did not include males as potential victims of IPV. Therefore, we do not know if our findings would generalize to females’ violence perpetrated against males. Similarly, our study does not examine dating violence by adolescents. While we examined the impact of the prevalence of severe IPV on females’ depression, we did not examine the impact of the frequency or chronicity of such violence. It is possible that more frequent or more severe violence, while perhaps more detrimental to depression (Campbell 2002), could be impacted by neighborhood factors differently. Finally, our data were collected from women in one city (Chicago) during the mid-1990s and into the early 2000s; although the PHDCN is a highly respected dataset, we cannot ensure that our results would generalize to other populations or time periods.
Our study adds to burgeoning evidence that neighborhood context impacts various interpersonal outcomes, in both direct and moderating ways. It appears that neighborhood supportive mechanisms may directly protect females from negative mental health problems such as experiencing depressive symptoms. These neighborhood supportive mechanisms, though less often considered, are important to examine for prevention and intervention purposes, and suggest that just as neighborhoods can be detrimental, they can also be positive and protective. Neighborhood collective efficacy, cohesion, and interaction between neighbors might increase feelings of support, belongingness, investment, communication, and other positive attributes, which may in turn reduce depressive symptoms. We believe it is important for researchers to continue to examine the positive and potentially mitigating influences of neighborhoods, as well as their detrimental effects, in order to better understand for whom and under which circumstances violent relationships and mental health are influenced by contextual factors.
Notes
Staff at the Inter-university Consortium for Political and Social Research calculated NC-linked U.S. Census measures in order to ensure the confidentiality of the subjects of the PHDCN.
Although the Community Survey collected information from all 343 NCs about neighborhood conditions via interviews with these residents, this study focuses only on those 80 NCs in which the participants of the LCS were nested.
To arrive at the 2959, a total of 292 cases were deleted due to missing data. The only significant difference between our analysis sample and the eligible sample of female caregivers in a relationship was that our analysis sample had slightly fewer Hispanic women (p < .05). There were no significant differences on the main independent variable of interest or any other control variables.
We control for neighborhood disadvantage in multilevel analyses because, relative to other structural conditions such as residential mobility or ethnic heterogeneity, disadvantage has been found to be the most consistent influence on both IPV and depression (Kim 2008; Mair et al. 2008; Pinchevsky and Wright 2012).
Item response modeling techniques avoid the loss of data from missing responses to a set of questions or indicators (Osgood et al. 2002), take item difficulty into account (i.e., that some indicators of neighborhood constructs may be more difficult and less prevalent than others), and allow simultaneous estimation of the impact of individual-level influences (e.g., age, gender) on perceptions of these constructs (Sampson et al. 2005). The item response models used in this study ultimately provide the neighborhood-level of collective efficacy (or, social cohesion, or social interaction) after these issues have been accounted for.
The same five items that measure social cohesion are also included in the collective efficacy measure. We believe this overlap is conceptually tolerable for the purposes of our inquiry. First, we were interested in the effect of collective efficacy on both depression and the IPV—depression relationship, and thus, needed to include the measure of collective efficacy as it has been examined in prior research (e.g., Sampson et al. 1997). Additionally, there has been some recent attention to the importance of social cohesion with regard to depression (Mair et al. 2010) as well as by itself as a facilitator of positive neighborhood behavior (e.g., informal social control, see Warner 2014). We were interested in its unique effects—apart from collective efficacy—and therefore chose to include a separate measure of social cohesion in our analyses. Collinearity did not present a problem, as we modeled collective efficacy and social cohesion separately.
References
Agoff, C., Herrera, C., & Castro, R. (2007). The weakness of family ties and their perpetuating effects on gender violence: A qualitative study in Mexico. Violence Against Women, 13(11), 1206–1220.
Ahern, J., & Galea, S. (2011). Collective efficacy and major depression in urban neighborhoods. American Journal of Epidemiology, 173(12), 1453–1462.
Aneshensel, C. S., & Sucoff, C. A. (1996). The neighborhood context of adolescent mental health. Journal of Health and Social Behavior, 37(4), 293–310.
Bellair, P. E. (1997). Social interaction and community crime: Examining the importance of neighbor networks. Criminology, 35(4), 677–704.
Benson, M. L., Fox, G. L., DeMaris, A., & Van Wyk, J. (2003). Neighborhood disadvantage, individual economic distress and violence against women in intimate relationships. Journal of Quantitative Criminology, 19(3), 207–235.
Bonomi, A. E., Thompson, R. S., Anderson, M., Reid, R. J., Carrell, D., Dimer, J. A., & Rivara, F. P. (2006). Intimate partner violence and women’s physical, mental, and social functioning. American Journal of Preventive Medicine, 30(6), 458–466.
Browning, C. R. (2002). The span of collective efficacy: Extending social disorganization theory to partner violence. Journal of Marriage and Family, 64(4), 833–850.
Browning, C. R., Feinberg, S. L., & Dietz, R. D. (2004). The paradox of social organization: Networks, collective efficacy, and violent crime in urban neighborhoods. Social Forces, 83(2), 503–534.
Burke, J., O’Campo, P., & Peak, G. L. (2006). Neighborhood influences and intimate partner violence: Does geographic setting matter? Journal of Urban Health, 83(2), 182–194.
Burke, J., O’Campo, P., Salmon, C., & Walker, R. (2009). Pathways connecting neighborhood influences and mental well-being: Socioeconomic position and gender differences. Social Science and Medicine, 68, 1294–1304.
Caetano, R., & Cunradi, C. (2003). Intimate partner violence and depression among Whites, Blacks, and Hispanics. Annals of Epidemiology, 13, 661–665.
Caldwell, J. E., Swan, S. C., & Woodbrown, V. D. (2012). Gender differences in intimate partner violence outcomes. Psychology of Violence, 2(1), 42–57.
Campbell, J. C. (2002). Health consequences of intimate partner violence. Lancet, 359(9341), 1331–1336.
Campbell, J. C., Kub, J. E., & Rose, L. (1996). Depression in battered women. Journal of the American Medical Women’s Association, 51(3), 106–110.
Cerda, M., Sanchez, B. N., Galea, S., Tracy, M., & Buka, S. L. (2008). Estimating co-occuring behavioral trajectories within a neighborhood context: A case study of multivariate transition models for clustered data. American Journal of Epidemiology, 168(10), 1190–1203.
Coker, A. L., Davis, K. E., Arias, I., Desai, R. A., Sanderson, M., Brandt, H. M., & Smith, P. H. (2002a). Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine, 23(4), 260–268.
Coker, A. L., Smith, P. H., Thompson, M. P., McKeown, R. E., Bethea, L., & Davis, K. E. (2002b). Social support protects against the negative effects of partner violence on mental health. Journal of Women’s Health & Gender-Based Medicine, 11(5), 465–476.
Cunradi, C. (2010). Neighborhoods, alcohol outlets and intimate partner violence: Addressing research gaps in explanatory mechanisms. International Journal of Environmental Research and Public Health, 7, 799–813.
DeMaris, A., & Kaukinen, C. (2005). Violent victimization and women’s mental and physical health: Evidence from a national sample. Journal of Research in Crime and Delinquency, 42(4), 384–411.
Earls, F. J., Brooks-Gunn, J., Raudenbush, S. W., & Sampson, R. J. (2002). Project on human development in Chicago neighborhoods (PHDCN). Ann Arbor, MI: Inter-university Corsortium for Political and Social Research.
Echeverria, S., Diez Roux, A. V., Shea, S., Borrell, L. N., & Jackson, S. (2008). Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: The multi-ethnic study of atherosclerosis. Health & Place, 14(4), 853–865.
Edwards, K. M., Mattingly, M. J., Dixon, K. J., & Banyard, V. L. (2014). Community matters: Intimate partner violence among rural young adults. American Journal of Community Psychology, 53, 198–207.
Emery, C. R., Jolley, J. M., & Wu, S. (2011). Desistance from intimate partner violence: The role of legal cynicism, collective efficacy, and social disorganization in Chicago neighborhoods. American Journal of Community Psychology, 48, 373–383.
Fletcher, J. (2010). The effects of intimate partner violence on health in young adulthood in the United States. Social Science and Medicine, 70, 130–135.
Geis, K. J., & Ross, C. E. (1998). A new look at urban alienation: The effect of neighborhood disorder on perceived powerlessness. Social Psychology Quarterly, 61(3), 232–246.
Golding, J. M. (1999). Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence, 14(2), 99–132.
Goodman, L. A., Smyth, K. F., Borges, A. M., & Singer, R. (2009). When crises collide: How intimate partner violence and poverty intersect to shape women’s mental health and coping? Trauma, Violence, & Abuse, 10(4), 306–329.
Hadeed, L. F., & El-Bassel, N. (2006). Social support among Afro-Trinidadian women experiencing intimate partner violence. Violence Against Women, 12(8), 740–760.
Hill, T. D., Ross, C. E., & Angel, R. J. (2005). Neighborhood disorder, psychophysiological distress, and health. Journal of Health and Social Behavior, 46(2), 170–186.
Johnson, W. L., Giordano, P. C., Longmore, M. A., & Manning, W. D. (2014). Intimate partner violence and depressive symptoms during adolescence and young adulthood. Journal of Health and Social Behavior, 55(1), 39–55.
Kessler, R. C., Andrews, G., Mroczerk, D., Ustun, B., & Wittchen, H.-U. (1998). The World Health Organization composite international diagnostic interview short-form (CIDI-SF). International Journal of Methods in Psychiatric Research, 7(4), 171–185.
Kim, D. (2008). Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiologic Reviews, 30, 101–117.
Kim, J. (2010). Neighborhood disadvantage and mental health: The role of neighborhood disorder and social relationships. Social Science Research, 39(2), 260–271.
Kim, J., & Ross, C. E. (2009). Neighborhood-specific and general social support: Which buffers the effect of neighborhood disorder on depression? Journal of Community Psychology, 37(6), 725–736.
Kirk, D. S., & Matsuda, M. (2011). Legal cynicism, collective efficacy, and the ecology of arrest. Criminology, 49(2), 443–472.
Kirst, M., Lazgare, L. P., Zhang, Y. J., & O’Campo, P. (2015). The effects of social capital and neighborhood characteristics on intimate partner violence: A consideration of social resources and risks. American Journal of Community Psychology, 55, 314–325.
Kornhauser, R. R. (1978). Social sources of delinquency: An appraisal of analytic models. Chicago, IL: University of Chicago Press.
Latkin, C. A., & Curry, A. D. (2003). Stressful neighborhoods and depression: A prospective study of the impact of neighborhood disorder. Journal of Health and Social Behavior, 44(1), 34–44.
Mair, C., Diez Roux, A. V., & Galea, S. (2008). Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. Journal of Epidemiology and Community Health, 62(11), 940–946.
Mair, C., Diez Roux, A. V., & Morenoff, J. D. (2010). Neighborhood stressors and social support as predictors of depressive symptoms in the Chicago Community Adult Health Study. Health & Place, 16(5), 811–819.
Miles-Doan, R. (1998). Violence between spouses and intimates: Does neighborhood context matter? Social Forces, 77(2), 623–645.
Moe, A. M. (2007). Silenced voices and structured survival: Battered women’s help seeking. Violence Against Women, 13(7), 676–699.
Molnar, B. E., Cerda, M., Roberts, A. L., & Buka, S. L. (2008). Effects of neighborhood resources on aggressive and delinquent behaviors among urban youths. American Journal of Public Health, 98(6), 1086–1093.
Molnar, B. E., Miller, M. J., Azrael, D., & Buka, S. L. (2004). Neighborhood predictors of concealed firearm carrying among children and adolescents: Results from the project on human development in Chicago neighborhoods. Archives of Pediatrics and Adolescent Medicine, 158(7), 657–664.
Morenoff, J. D., Sampson, R. J., & Raudenbush, S. W. (2001). Neighborhood inequality, collective efficacy, and the spatial dynamics of urban violence. Criminology, 39(3), 517–559.
O’Campo, P., Burke, J., Peak, G. L., McDonnell, K. A., & Gielen, A. C. (2005). Uncovering neighbourhood influence on intimate partner violence using concept mapping. Journal of Epidemiology and Community Health, 59(7), 603–608.
Osgood, D. W., McMorris, B. J., & Potenza, M. T. (2002). Analyzing multiple-item measures of crime and deviance I: Item response theory scaling. Journal of Quantitative Criminology, 18, 267–296.
Pinchevsky, G. M., & Wright, E. M. (2012). The impact of neighborhoods on intimate partner violence and victimization. Trauma, Violence, & Abuse, 12(2), 112–132.
Raudenbush, S. W., Johnson, C., & Sampson, R. J. (2003). A multivariate, multilevel Rasch model with application to self-reported criminal behavior. Sociological Methodology, 33(1), 169–211.
Rios, R., Aiken, L. S., & Zautra, A. J. (2012). Neighborhood contexts and the mediating role of neighborhood social cohesion on health and psychological distress among Hispanic and non-Hispanic residents. Annals of Behavioral Medicine, 43(1), 50–61. doi:10.1007/s12160-011-9306-9.
Ross, C. E. (2000). Neighborhood disadvantage and adult depression. Journal of Health and Social Behavior, 41(2), 177–187.
Ross, C. E., & Jang, S. J. (2000). Neighborhood disorder, fear, and mistrust: The buffering role of social ties with neighbors. American Journal of Community Psychology, 28(4), 401–420.
Ross, C. E., & Mirowsky, J. (2009). Neighborhood disorder, subjective alienation, and distress. Journal of Health and Social Behavior, 50(1), 49–64. doi:10.1177/002214650905000104.
Ross, C. E., Mirowsky, J., & Pribesh, S. (2001). Powerless and the amplification of threat: Neighborhood disadvantage, disorder, and mistrust. American Sociological Review, 66(4), 568–591.
Ross, C. E., Reynolds, J. R., & Geis, K. J. (2000). The contingent meaning of neighborhood stability for residents’ psychological well-being. American Sociological Review, 65(4), 581–597.
Sampson, R. J. (2003). The neighborhood context of well being. Perspectives in Biology and Medicine, 46(3), S53–S73.
Sampson, R. J. (2013). Great American city: Chicago and the enduring neighborhood effect. Chicago, IL: University of Chicago Press.
Sampson, R. J., Morenoff, J. D., & Raudenbush, S. W. (2005). Social anatomy of racial and ethnic disparaties in violence. American Journal of Public Health, 95(2), 224–232.
Sampson, R. J., Raudenbush, S. W., & Earls, F. J. (1997). Neighborhoods and violent crime: A multilevel study of collective efficacy. Science, 277(5328), 918–924.
Shaw, C. R., & McKay, H. D. (1942). Juvenile delinquency and urban areas: A study of rates of delinquents in relation to differential characteristics of local communities in American cities. Chicago, IL: University of Chicago Press.
Stafford, M., McMunn, A., & De Vogli, R. (2011). Neighbourhood social environment and depressive symptoms in mid-life and beyond. Ageing & Society, 31(6), 893–910.
Stith, S. M., Smith, D. B., Penn, C. E., Ward, D. B., & Tritt, D. (2004). Intimate partner physical abuse perpetration and victimization risk factors: A meta-analytic review. Aggression and Violent Behavior, 10(1), 65–98.
Straus, M. A. (1979). Measuring intrafamily conflict and violence: The conflict tactics (CT) scales. Journal of Marriage and Family, 41(1), 75–88.
Straus, M. A., Gelles, R. J., & Steinmetz, S. K. (2006). Behind closed doors: Violence in the American family. New Brunswick, NJ: Transaction Publishers.
Taylor, S. E., & Repetti, R. L. (1997). Health psychology: What is an unhealthy environment and how does it get under the skin? Annual Review of Psychology, 48, 411–447.
Van Wyk, J. A., Benson, M. L., Fox, G. L., & DeMaris, A. (2003). Detangling individual-, partner-, and community-level correlates of partner violence. Crime & Delinquency, 49(3), 412–438.
Vega, W. A., Ang, A., Rodriguez, M. A., & Finch, B. K. (2011). Neighborhood protective effects on depression in Latinos. American Journal of Community Psychology, 47(1–2), 114–126.
Warner, B. D. (2014). Neighborhood factors related to the likelihood of successful informal social control efforts. Journal of Criminal Justice, 42, 421–430.
Wellman, B., & Wortley, S. (1990). Different strokes from different folks: Community ties and social support. American Journal of Sociology, 96(3), 558–588.
Wilson, J. Q., & Kelling, G. L. (1982). The police and neighborhood safety: Broken windows. Atlantic Monthly, 127, 29–38.
Wright, E. M. (2012). The relationship between social support and intimate partner violence in neighborhood context. Crime & Delinquency. doi:10.1177/0011128712466890.
Wright, E. M., & Benson, M. L. (2010). Immigration and intimate partner violence: Exploring the immigrant paradox. Social Problems, 57(3), 480–503.
Wright, E. M., & Benson, M. L. (2011). Clarifying the effects of neighborhood disadvantage and collective efficacy on violence “behind closed doors”. Justice Quarterly, 28(5), 775–798.
Xue, Y., Leventhal, T., Brooks-Gunn, J., & Earls, F. J. (2005). Neighborhood residence and mental health problems of 5- to 11-year olds. Archives of General Psychiatry, 62(5), 554–563.
Zimmerman, G. M., & Messner, S. F. (2010). Neighborhood context and the gender gap in adolescent violent crime. American Sociological Review, 75(6), 958–980.
Zimmerman, G. M., & Messner, S. F. (2011). Neighborhood context and nonlinear peer effects on adolescent violent crime. Criminology, 49(3), 873–903.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wright, E.M., Pinchevsky, G.M., Benson, M.L. et al. Intimate Partner Violence and Subsequent Depression: Examining the Roles of Neighborhood Supportive Mechanisms. Am J Community Psychol 56, 342–356 (2015). https://doi.org/10.1007/s10464-015-9753-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10464-015-9753-8