Abstract
Intimate partner violence (IPV) is a growing public health problem, and gaps exist in knowledge with respect to appropriate prevention and treatment strategies. A growing body of research evidence suggests that beyond individual factors (e.g., socio-economic status, psychological processes, substance abuse problems), neighborhood characteristics, such as neighborhood economic disadvantage, high crime rates, high unemployment and social disorder, are associated with increased risk for IPV. However, existing research in this area has focused primarily on risk factors inherent in neighborhoods, and has failed to adequately examine resources within social networks and neighborhoods that may buffer or prevent the occurrence of IPV. This study examines the effects of neighborhood characteristics, such as economic disadvantage and disorder, and individual and neighborhood resources, such as social capital, on IPV among a representative sample of 2412 residents of Toronto, Ontario, Canada. Using a population based sample of 2412 randomly selected Toronto adults with comprehensive neighborhood level data on a broad set of characteristics, we conducted multi-level modeling to examine the effects of individual- and neighborhood-level effects on IPV outcomes. We also examined protective factors through a comprehensive operationalization of the concept of social capital, involving neighborhood collective efficacy, community group participation, social network structure and social support. Findings show that residents who were involved in one or more community groups in the last 12 months and had high perceived neighborhood problems were more likely to have experienced physical IPV. Residents who had high perceived social support and low perceived neighborhood problems were less likely to experience non-physical IPV. These relationships did not differ by neighborhood income or gender. Findings suggest interesting contextual effects of social capital on IPV. Consistent with previous research, higher levels of perceived neighborhood problems can reflect disadvantaged environments that are more challenged in promoting health and regulating disorder, and can create stressors in which IPV is more likely to occur. Such analyses will be helpful to further understanding of the complex, multi-level pathways related to IPV and to inform the development of effective programs and policies with which to address and prevent this serious public health issue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intimate partner violence (IPV) is a growing public health problem that can affect both women and men, and gaps exist in knowledge with respect to appropriate prevention and treatment strategies. Population estimates of IPV among women worldwide range from 10 to 71 % having experienced physical violence and 3–59 % having experienced sexual violence by a partner (Ansara and Hindin 2011a; Daoud et al. 2012b). Less is known about the global prevalence of IPV among males. A recent Canadian study of a general population sample found that approximately 17 % of men and 18 % of women had experienced emotional or financial abuse from an intimate partner, 6 % of men and women had experienced physical violence by a partner, and 1 % of women had experienced sexual violence by a partner (Ansara and Hindin 2011b). A growing body of research evidence suggests that beyond individual factors (e.g., socio-economic status, psychological processes, substance abuse problems), neighborhood characteristics, such as neighborhood economic disadvantage, high crime rates, high unemployment and social disorder, are associated with increased risk for IPV (O'Campo et al. 1995, 2005; Cunradi et al. 2000; Beyer et al. 2013). However, many of the neighborhood studies that have been conducted suffer from methodological limitations such as failure to account for clustering within neighborhoods and small sample sizes (Li et al. 2010). Moreover, existing research in this area has focused primarily on risk factors inherent in neighborhoods, and few studies have incorporated examination of social resources within social networks and neighborhoods that may buffer or protect against the occurrence of IPV (Browning 2002; Benson et al. 2003; Van Wyk et al. 2003; Lanier and Maume 2009). Much of this research relies on self-reported perceptions of neighborhoods and thus may misrepresent the nature and effects of neighborhoods on IPV. Furthermore, existing research has failed to take into consideration individual and ecological predictors of IPV among both sexes, and focuses primarily on prevalence and impact among women (Ansara and Hindin 2011a).
Using a population-based sample of 2412 randomly selected Toronto adults, this study examines the effects of neighborhood characteristics, such as economic disadvantage and neighborhood problems, and individual and neighborhood resources, such as social capital, on IPV. Furthermore, we examine these individual and neighborhood effects on IPV outcomes among women and men. We explore protective factors through a comprehensive operationalization of the concept of social capital, involving measures of neighborhood collective efficacy, community group participation, social network structure and social support.
Neighborhood Effects and Risk of IPV
A growing body of research is exploring the association between neighborhood structural characteristics, such as neighborhood poverty, racial composition, residential instability, neighborhood concentration of immigrants and/or neighborhood disorder on IPV, primarily among women. This research draws on the hypothesis that these forms of social disorganization diminish community capacity to regulate crime and disorder (Browning 2002). A number of studies have found that women living in more disadvantaged neighborhoods are more likely to experience IPV compared to those living in wealthier neighborhoods (O'Campo et al. 1995; Miles-Doan and Kelly 1997; Miles-Doan 1998; Cunradi et al. 2000; Benson et al. 2003; Pearlman et al. 2003; Van Wyk et al. 2003; Fox and Benson 2006; Pinchevsky and Wright 2012; Golden et al. 2013). Studies have also found that perceived neighborhood disorder is associated with increased risk of IPV (Cunradi 2007, 2009; DeKeseredy et al. 2003; Gracia et al. 2014). A Canadian study found that immigrant women were less likely to experience IPV, even after adjusting for socioeconomic position, family variables and neighborhood characteristics (Daoud et al. 2012a). A few studies have found that residential instability and percent of female-headed households, and not neighborhood poverty, are significant predictors of IPV (Lauritsen and Schaum 2004; Li et al. 2010). In addition to neighborhood factors, Cunradi (2009) found that individual-level alcohol abuse was associated with increased risk of IPV victimization among women. Possible explanations for these findings include risk of victimization by their spouse due to an alcohol problem, or problematic use of alcohol as a coping mechanism for existing IPV victimization (Cunradi 2009).
Studies have also found that increased alcohol availability through alcohol outlet density is associated with increased risk and rates of IPV (McKinney et al. 2009; Cunradi 2010; Cunradi et al. 2011; Livingston 2011; McKinney et al. 2012; Waller et al. 2012; Beyer et al. 2013). These studies suggest that increased availability of alcohol increases problem drinking and the risk of IPV.
A promising area of neighborhood research examines the effects of social capital on health and well-being. Social capital is generally defined as a stock of social resources and networks (e.g., personal and community networks, sense of belonging, civic engagement, norms of reciprocity and trust) that facilitates actions and provides returns in the form of individual or group level benefits such as well-being and good health (Coleman 1988; Putnam 1993; Portes 1998; Lin 2001; Harpham et al. 2004; Kawachi et al. 2008). Social capital is a complex multi-dimensional concept which comprises various levels and components. Individuals can gain access to cognitive and structural social capital via different societal levels, for example, at the individual-level, through the family or social network, and/or from the ecological-level, involving larger social structures such as the neighborhood, community, or state. Cognitive components of social capital refer to cognitive/perceptual aspects of social relationships, such as social support, trust and belongingness. Structural components of social capital relate to behavioural aspects of relationships, such as group participation (Harpham et al. 2004; McKenzie and Harpham 2006).
A small number of studies have examined how social resources in neighborhoods, or social capital, can affect IPV risk. This research draws on the notion that the presence of social capital in the form of social networks and community participation builds strong social ties, social cohesion and collective efficacy within communities (e.g., willingness of neighborhood residents to intervene on behalf of the common good), which allow for greater social control of crime and protection against victimization such as IPV (Browning 2002; Dekeseredy et al. 2003; Sampson et al. 1997). In the area of IPV, studies have found that as social capital (often conceptualized as neighborhood collective efficacy) increases, the likelihood of IPV decreases (O'Campo et al. 1995; Browning 2002; Tomaszewski 2002; Dekeseredy et al. 2003; Zolotor and Runyan 2006; Frye et al. 2008; Caetano et al. 2010; Wright and Benson 2011). However, some studies have noted contextual effects of social capital on IPV. A study conducted in Chicago found that neighborhood collective efficacy, also operationalized as informal social control, cohesion, and trust, has a protective effect on the risk of less severe IPV only when the neighborhood had low nonintervention norms (attitudes preventing intervention in intimate relationships). As non-intervention norms increased, the protective effect of collective efficacy decreased (Browning 2002). Lanier and Maume (2009) found that risk of IPV decreases among women living in rural areas with a greater amount of help from family and friends, whereas this was not the case among women living in urban settings. Van Wyck et al. (2003) found that women with low individual social support, meaning less social contact and less assistance given and received, who live in economically disadvantaged neighborhoods were at the highest risk for IPV (Van Wyk et al. 2003).
A small number of studies have examined effects of social capital on IPV among both sexes. DeKeseredy et al. (2003) found that men and women who perceived collective efficacy in their neighborhood to be low were more likely to have experienced IPV. Jain et al. (2010) observed that higher levels of neighborhood collective efficacy reduced the risk of being a victim of dating violence, particularly for young adult males in low to mid-poverty neighborhoods (Jain et al. 2010). Similarly, Edwards et al. (2014) found a negative relationship between neighborhood collective efficacy and IPV among young adult men, but no relationship for young adult women. A recent study examined whether couples’ perceived neighborhood social cohesion and social control mediated the relation between neighborhood poverty and IPV outcomes. This study found no evidence of a meditational effect of social cohesion and social control on either male to female IPV or female to male IPV (Caetano et al. 2010). Emery et al. (2011) found no relationship between collective efficacy and intimate partner violence desistance over time. The conceptual framework that guides the analysis in the present study is informed by these studies and draws from social disorganization theory and overlapping “neighborhood stress”, “neighborhood structural characteristics” and “neighborhood disorder” models. These models hypothesize that neighborhood structural characteristics such as deteriorated environment, socioeconomic disadvantage, and neighborhood disorder, are stressors related to IPV (Browning 2002; Ross 2000).
We build on existing literature by using ecological, neighborhood measures, including measures of neighborhood income, violent crime and alcohol availability, in addition to self reported perceptual data to provide a more complete assessment of neighborhood characteristics in a representative sample. We further expand upon extant neighborhood research by considering how social capital (individual and neighborhood) and neighborhood structural characteristics affect IPV, and examine these relationships among both women and men. In this study, we hypothesize that:
-
1.
High levels of individual social capital (social network size, frequency of social contact, community group participation) and neighborhood social capital (collective efficacy) will be protective against risk of physical and non-physical IPV;
-
2.
Neighborhood disorder, low neighborhood safety and quality, and low neighborhood socio-economic status will be associated with higher risk of physical and non-physical IPV;
-
3.
Lower levels of (individual and neighborhood) social capital will be associated with increased risk of physical and non-physical IPV among women and men living in neighborhoods characterized by low socio-economic status and disorder.
We also examine whether levels of social capital and neighborhood characteristics explain differences in risk of IPV by gender.
Methods
The Neighborhood Effects on Health and Well-being (NEHW) study is a cross-sectional survey that collects information related to neighborhood and individual stressors and resources that may affect mental health and well-being among a representative sample of Toronto residents (O'Campo et al. 2015). In addition to individual-level survey data, the NEHW study contains a rich set of ecological, neighborhood-level variables through linkage with administrative and commercially available databases, and census data. The Research Ethics Board at St. Michael’s Hospital in Toronto, Canada granted ethics approval for this study.
Sampling and Data Collection
Toronto is the largest city in Canada, with a population of 2.5 million people (Statistics Canada 2012). Fifty of Toronto’s 140 neighborhoods served as the primary sampling units for the study. We randomly selected households within each census tract based on residential address. Our target recruitment number was 30 households per census tract. Household sampling frames were purchased from a commercial marketing company that derives lists of residential addresses and telephone numbers from published directories based on census tract boundaries. Sampling of households was done sequentially, with the selection of 80 households at a time for screening from a list of 300 potential households. Individuals were eligible to participate if they: (a) were a resident of the selected household; (b) were between the ages of 25–64; (c) were able to communicate in English; and (d) had lived in the neighborhood for at least 6 months. Introductory letters were sent to each selected household in advance. Households were then contacted by telephone within 1 week after the initial contact letter was sent. Within each household, interviewers asked to speak with the member of the household who had the closest birthday. After screening, eligible participants were invited to participate in a face to face interview, typically conducted in their homes. All participants provided written informed consent to participate at the time of their interview. Data were collected between March 2009 and June 2011. In total, 2412 participants, representing 50 neighborhoods and 87 census tracts, were included in the study sample.
Measures
Outcomes
Participants were asked if they had experienced any IPV in the last 10 years based on the HITS scale, a short IPV screening tool (Sherin et al. 1998). If they answered yes, they were then asked a series of questions on experience of physical and non-physical intimate partner violence. Physical intimate partner violence is based on an abbreviated version of the Physical Partner Abuse Scale including seven items (Hudson and McIntosh 1981). Participants were asked a series of questions concerning how frequently they had experienced types of physical violence, including being hit, shoved or beaten by their partner. Non-physical intimate partner violence is based on an abbreviated version of the Non-Physical Partner Abuse Scale, including 13 items (Hudson and McIntosh 1981). The scale asks how frequently non-physical partner abuse, such as emotional abuse, restriction of actions, and jealousy, has been experienced. Each scale was scored by summing the item responses. Both scales were dichotomized to reflect having experienced physical or non-physical intimate partner violence in the lifetime, according to cut offs determined by Attala et al. (1994)—above 2 % for the physical violence scale and 15 % for the non-physical violence scale.
Predictors: Level 1
Individual Social Capital: Structural social capital at the individual-level was conceptualized as network size and community group participation. Network size refers to the number of network ties each participant named during the interview. This variable was dichotomized with 1 referring to a network size of three or more members and 0 referring to a network size of less than three members. Frequency of social contact refers to the frequency of contact with neighbors, friends and family (Nyqvist et al. 2008). This measure involves a series of five items asking about the frequency (from everyday to not at all in the last 12 months) with which participants had seen or spoken to relatives and friends, and had spoken with neighbors. Each item was dichotomized to reflect contact at least once or twice a week versus less than weekly, and the items were then summed. Community group participation involved the number of community groups or organizations to which respondents were members, for example women’s groups, sports groups, ethnic groups, church groups (DeSilva et al. 2007). This variable was dichotomized, with 0 representing participation in no community groups and 1 representing participation in one or more groups. Cognitive social capital was conceptualized as perceived social support. Perceived social support was assessed using the Medical Outcomes Study (MOS) Social Support Survey, a reliable and valid multidimensional survey that measures social support across four functional support subscales: tangible social support, affection, positive social interaction, and emotional or informational support (Sherbourne and Stewart 1991). Participants were asked to rate the frequency of perceived availability of support for 19 items according to a five-point Likert scale: none of the time, a little of the time, some of the time, most of the time and all of the time. Item ratings were summed to determine a total score within each subscale. This scale was dichotomized at the highest quartile to reflect high versus low perceived support.
Neighborhood Social Capital: Collective efficacy was measured through a combination of two scales a) informal social control, assessing respondents’ perceptions of the likelihood of neighbors intervening on acts of mischief, and b) social cohesion and trust, assessed through a series of questions on connectedness and trust between neighbors (Sampson et al. 1997). The collective efficacy scale was dichotomized at the highest quartile to reflect high versus low collective efficacy in the neighborhood.
Neighborhood Characteristics: Neighborhood problems were measured through an index comprising 20 items on the presence of physical disorder and deteriorated environment (e.g., graffiti, litter, abandoned buildings, violence) in the neighborhood (O'Campo et al. 1997). Neighborhood quality was measured with a series of 12 questions assessing satisfaction with aspects of the neighborhood such as air quality, green spaces, entertainment, shopping (Coulton et al. 1996). Neighborhood safety was measured with a scale of six questions on concerns of walking, and letting children play or being harmed in the neighborhood (Coulton et al. 1996). The neighborhood problems, quality and safety measures were each summed across participants in the same census tract, and then an average was calculated by neighborhood. Each of these neighborhood variables was then dichotomized at the highest quartile to reflect high versus low levels in the neighborhood. This value was assigned to each participant by census tract. Because we were interested in men and women at highest risk for neighborhood stressors and low levels of social capital, these variables were dichotomized, as has been done in other studies (Caughy et al. 2003; Jain et al. 2010; Kim and Kawachi 2006).
Predictors: Level 2
Data characterizing NEHW neighborhoods at the census tract (CT) level were obtained from a variety of sources. Statistics Canada and the Canadian Centre for Justice Statistics (2010) provided data on the number of violent crimes per CT for 2006, which includes sexual assault, criminal harassment, uttering threats, minor/major assault, and robbery. As alcohol availability (e.g., alcohol outlet density) has been found to be associated with risk of IPV in other research (McKinney et al. 2009; Cunradi 2010; Cunradi et al. 2011; Livingston 2011; McKinney et al. 2012; Waller et al. 2012), we included measures of off-premise and on-premise alcohol availability. Data relating to alcohol availability came from three sources: the Canadian Business Points (number of off-premise retail establishments that sell alcohol) Toronto Dinesafe 2011 (all food establishments also selling alcohol in Toronto) and the Alcohol and Gaming Commission of Ontario registry of establishments with liquor licenses in 2011. Data from the last two sources were combined to reflect a measure of on-premise alcohol availability. These variables reflect the number of on-premise and off-premise alcohol outlets within a km2 in the neighborhood. Neighborhood socio-economic status refers to neighborhood level median after-tax household income derived from the Canadian Census 2006.
Control Variables
Models were adjusted for the following control variables: gender, age, marital status, immigrant status, and education level, as these have been explored as potential confounders in other research (Van Wyck et al. 2003). Previous research has found that problematic alcohol consumption can be related to IPV victimization (Waller et al. 2012; Cunradi 2009), and a variable assessing the frequency of consumption of five or more drinks on one occasion in the last 12 months (binge drinking), derived from the Alcohol Use Disorders Identification Test (AUDIT) (Babor et al. 2001), was controlled for given our interest in the effects of alcohol availability. This variable was dichotomized, with 1 reflecting consumption of five more drinks on one occasion on a monthly basis, and 0 reflecting consumption of five or more drinks on one occasion less than monthly.
Data Analysis
Descriptive statistics were generated to estimate simple associations between predictors and outcome variables. Chi square tests were used to assess differences in experience of IPV between males and females, as well as other socio-demographics and characteristics in the sample. There was a small amount of missing data (approximately 2 %) for certain outcomes of interest and associated predictors in the NEHW Study. These missing values were indicative of questions that were not answered due to participant refusal, items that were inadvertently skipped from being asked or questions that had skip patterns, or participant response of ‘don’t know’. Multiple imputation was conducted to address these missing data. In the first stage of the imputation process, a logistic regression model was used to impute the occurrence of the event. In the second stage, conditional on imputing the occurrence of the event, a linear regression model was used to impute the non-zero values of the variable. Five imputed datasets were created for analyses. Once the five datasets were created, we fit two sets of three multilevel (two-level) models according to our hypotheses, using the variance components covariance-structure. The results were then combined using PROC MIANALYZE. For the binary outcomes (non-physical and physical IPV), we used PROC GLIMMIX to generate the model estimates for each imputed dataset—one set for each outcome of physical IPV and non-physical IPV.
To examine Hypothesis 1, Model 1 assesses the contribution of measures of individual-level social capital to the outcome, adjusted by age, gender, marital status, immigrant status, education, and binge drinking. Model 2 assesses Hypothesis 2 by examining relationships between perceived neighborhood stressors such as neighborhood quality, problems and safety (level 1) and physical neighborhood stressors such as violent crime, alcohol availability, and socio-economic disadvantage (level 2), adjusted by potential confounders and the IPV outcomes. To address the modifiying effects of social capital in Hypothesis 3, Model 3 includes variables combining significant social capital, and neighborhood stressor variables, as well as control variables. Interactions between combined social capital and neighborhood stressors and neighborhood income were added to assess cross-level effects. Interactions between gender, social capital and neighborhood characteristics were also entered into the final models to assess gender differences. In the process of model-building, only variables that reached significance in Models 1 and 2 were added to Model 3. For all analyses, data were weighted by age, sex, household income, household size and immigrant status to correct for any selection biases, using 2006 Census data for the city of Toronto.
Results
Descriptives
Participant demographic characteristics are reported among the total sample in Table 1. Fifty-two percent of the participants were female, and 70 % were between the ages of 25 and 50. Seventy-seven percent of participants had completed some post-secondary education. Seventy-two percent of participants were married or living common-law. Eighty-five percent of participants were either non-recent immigrants or born in Canada. The majority of participants had a household income of lower than $75,000. Fourteen percent of participants had experienced non-physical IPV, and 8 % had experienced physical IPV. Those who had experienced non-physical and physical IPV were younger, never married, had lower educational attainment and lower household incomes than those who had not experienced IPV. Not surprisingly, significantly more females than males had experienced non-physical IPV (20 vs. 12 %; OR 1.77) and physical IPV (10 vs. 6 %; OR 1.75) (not shown).
With respect to social capital (Table 2), the majority of participants (71 %) had a social network size of three or more social network members. Forty-five percent of participants saw relatives in person once a week or more, however, over 70 % spoke to relatives on the phone, saw friends, spoke to friends on the phone and spoke to neighbors on a weekly basis. Sixty-four percent participated in one or more community groups. Seventeen percent reported high collective efficacy in their neighborhoods. With respect to neighborhood characteristics, 17 % of residents perceived high neighborhood quality, 70 % perceived low neighborhood problems, and 20 % perceived high neighborhood safety. More participants who had experienced non-physical and physical IPV reported high neighborhood problems than those who had not experienced IPV. More participants who had experienced physical IPV had greater group participation than those with lower than those who had not experienced IPV.
Multilevel Models
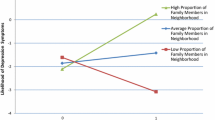
Table 3 presents adjusted associations between social capital, neighborhood characteristics and physical IPV. In Model 1, surprisingly, being involved in one community group or more in the last 12 months, such as sports groups or religious groups, was a significant predictor of physical IPV (p = 0.0007). However, neighborhood residents with social networks of three or more members were less likely to experience physical IPV than those with smaller social networks (OR 0.67; p = 0.0346). Results of model 2 support hypothesis 2, in that those with low perceived neighborhood problems were less likely to experience physical IPV (OR 0.59; p = 0.0002) and those living in neighborhoods with higher median income were less likely to report physical IPV (OR 0.74; p = 0.0497). In Model 3, reflecting hypothesis 3, residents with low group participation (i.e., no involvement in community groups) and low perceived neighborhood problems were 0.27 times less likely to experience physical IPV than those with high group participation and high neighborhood problems. No other social capital or neighborhood characteristic variables, including alcohol availability variables, were significant predictors of physical IPV. Results from these models partially support our hypotheses, in that they show that neighborhood disorder is associated with risk of physical IPV, but do not confirm that greater social capital, through involvement in community groups, is protective against physical IPV. Furthermore, interactions between the combined social capital/neighborhood problems variables and neighborhood income were tested in the final model, but were not significant (not shown).
Table 4 shows adjusted associations between social capital, neighborhood characteristics and non-physical IPV. Our hypotheses for non-physical IPV are partially supported. In Model 1, residents with greater perceived social support were less likely to experience non-physical IPV than those with lower perceived social support (OR 0.71; p = 0.0432). In Model 2, residents with lower perceived problems in the neighborhood were less likely to experience non-physical IPV than those with higher perceived neighborhood problems (OR 0.59; p < 0.0001), and residents in neighborhoods with higher median income were less likely to experience non-physical IPV (OR 0.77; p = 0.0131). In Model 3, residents with high perceived social support and low perceived neighborhood problems were 0.48 times less likely to experience non-physical IPV (p = 0.0005) compared to those with low social support and high neighborhood problems. In addition, residents with low perceived social support and low perceived neighborhood problems were less likely to experience non-physical IPV (OR 0.63; p = 0.0043) than those with low social support and high neighborhood problems. Similar to the physical IPV model, interactions between social capital, neighborhood problems and neighborhood income were not significant for the non-physical IPV outcome.
Interactions between the combined social capital/neighborhood characteristics variables and gender were also examined in the final model for each outcome to address gender differences. No significant interactions between these variables were detected, indicating that the effects of social capital and perceived neighborhood problems on IPV risk do not differ between women and men.
Discussion and Conclusion
Study findings are consistent with hypothesized health effects outlined in social capital theory and with previous studies that have explored social network and neighborhood-level effects on IPV and other health outcomes (O'Campo et al. 1995; Van Wyk et al. 2003), but show contextual effects of different forms of social capital (i.e., structural and cognitive) on the different IPV outcomes. As anticipated in hypothesis 1, findings suggest that higher levels of social support (cognitive social capital) from social networks can be protective against non-physical IPV by providing instrumental, informational, emotional, and even financial assistance that can reduce the risk of IPV among both sexes. However, the finding that involvement in community groups (structural social capital) increases the likelihood of experiencing physical IPV was unexpected and was not consistent with our hypothesis. As articulated in hypothesis 2, higher levels of perceived neighborhood problems can reflect disadvantaged environments that are more challenged in promoting health and regulating disorder, and can create stressors in which intimate partner violence is more likely to occur.
Hypothesis 3 was only partially supported. Greater group participation was associated with increased risk of physical IPV for those living in neighborhoods with high perceived disorder, with no variation by neighborhood income. Furthermore, high social support was associated with decreased risk of non-physical IPV for those living in neighborhoods with lower perceived disorder, but this did not differ by neighborhood income. The counter-intuitive effects of group participation may be due to the fact that the experience of IPV can be socially isolating, and victims may be joining groups and seeking support to overcome this isolation. More longitudinal and qualitative research is needed to further investigate this relationship, and determine the temporal and in-depth nature of this type of help-seeking in relation to IPV victimization. However, in a concept-mapping study, both urban and suburban women identified community resources and support systems as most strongly related to IPV cessation (Burke et al. 2006). Another possible explanation for this unexpected effect could be reflective of the theory of “status incompatibility”. This theory argues that in situations where a partner has lower status (e.g., education, income or social status) than their partner, the lower status partner may feel threatened by their partner’s growth, and the partner with higher status may be at increased risk of interpersonal conflict and violent victimization (Gielen et al. 1994). Thus, women or men who are more engaged in neighborhood groups than their partners may be at increased risk of experiencing IPV because of this status incompatibility. However, one limitation to this explanation is that we do not know the social status of the study participants’ partners.
A number of limitations to this study must be considered when interpreting results. The cross-sectional nature of the data limits the ability to draw causal inferences. The survey was only conducted in English, and only residents with telephone land-lines were sampled, thus limiting the representativeness of the sample. Furthermore, IPV may have been under-reported in the sample given the highly sensitive nature of the issue. In public health research, researchers are often interested in individuals at highest risk because such exploration presents key opportunities for the design of interventions. We dichotomized our social capital and neighborhood characteristic variables because we were interested in such thresholds of risk. Our use of dichotomized variables may have led to a loss of information in the sense that we may have missed associations. If we had used continuous variables, we may have learned that the associations are linear and not based on a threshold. However, our use of dichotomous variables representing high risk categories was justified given our interest in these risk thresholds, and that our data are representative of the city population, as opposed to being reflective of a specialized group (e.g., low income women). General methodological limitations to neighborhood research also apply to this study, including the subjectivity of the definition of neighborhood, and lack of consideration of compositional effects that may determine residency in certain neighborhoods.
Overall, study findings highlight the importance of examining social capital and contextual characteristics at multiple levels; that is, both social network- and neighborhood-level factors are relevant for different types of IPV. Future work in this area should also pay greater attention to gender differences given the prevalence of IPV among both women and men in the sample. Analyses such as these can inform the development of community-based interventions to address complex social network- and neighborhood-level contextual factors related to IPV in an effort to prevent and reduce this serious public health problem.
References
Ansara, D., & Hindin, M. (2011a). Psychosocial consequences of intimate partner violence for women and men in Canada. Journal of Interpersonal Violence, 26(8), 1628–1645.
Ansara, D., & Hindin, M. (2011b). Exploring gender differences in the patterns of intimate partner violence in Canada: A latent class analysis. Journal of Epidemiology and Community Health, 64, 849–854.
Attala, J., Hudson, W. W., & McSeeney, M. (1994). A partial validation of two short-form partner abuse scales. Women and Health, 21(2–3), 125–139.
Babor, T. F., et al. (2001). AUDIT: The alcohol use disorders identification test (2nd ed.). Geneva: Department of Mental Health and Substance Dependence, World Health Organization.
Benson, M., Fox, G., et al. (2003). Neighbourhood disadvantage, individual economic distress and violence against women in intimate relationships. Journal of Quantitative Criminology, 19, 207–235.
Beyer, K., Baber Wallis, A., Hamberger, L. K. (2013). Neighborhood environmentand intimate partner violence: A systematic review. Trauma, Abuse and Violence, December, Online First, 1–32.
Browning, C. (2002). The span of collective efficacy: Extending social disorganization theory to partner violence. Journal of Marriage and Family, 64, 833–850.
Burke, J., O'Campo, P., et al. (2006). Neighborhood influences and intimate partner violence: Does geographic setting matter? Journal of Urban Health, 83(2), 182–194.
Caetano, R., Ramisetty-Mikler, S., et al. (2010). Neighbourhood characteristics as predictors of make to female and female to male partner violence. Journal of Interpersonal Violence, 25(11), 1986–2009.
Caughy, M. O., O'Campo, P., & Muntaner, C. (2003). When being alone might be better: Neighborhood poverty, social capital and child mental health. Social Science and Medicine, 57(2), 227–237.
Coleman, J. (1988). Social capital in the creation of human capital. American Journal of Sociology, 94(Supplement), S95–S120.
Coulton, C. J., Korbin, J. E., & Su, M. (1996). Measuring neighbourhood context for young children in an urban area. American Journal of Community Psychology, 24, 5–32.
Cunradi, C. (2007). Drinking level, neighborhood social disorder, and mutual intimate partner violence. Alcoholism: Clinical and Experimental Research, 31(6), 1012–1019.
Cunradi, C. (2009). Intimate partner violence among Hispanic men and women: The role of drinking, neighbourhood disorder, and acculturation-related factors. Violence and Victims, 24(1), 83–97.
Cunradi, C. (2010). Neighbourhood, alcohol outlets and intimate partner violence: Addresing research gaps in explanatory mechanisms. International Journal of Environmental Research and Public Health, 7, 799–813.
Cunradi, C., Caetano, R., et al. (2000). Neighbourhood poverty as a predictor of intimate partner violence among White, Black and Hispanic couples in the United States: A multilevel analysis. Annals of Epidemiology, 10, 297–308.
Cunradi, C., Mair, C., et al. (2011). Alcohol outlets, neighbourhood characteristics, and intimate partner violence: Ecological analysis of a California city. Journal of Urban Health, 88(2), 191–200.
Daoud, N., O'Campo, P., Urquia, M., & Heaman, M. (2012a). Neighborhood context and abuse among immigrant and non-immigrant women in Canada: Findings from the Maternity Experiences Survey. International Journal of Public Health, 57, 679–689.
Daoud, N., Urquia, M., O'Campo, P., Janssen, P. A., Smylie, J., & Thiessen, K. (2012b). Prevalence of abuse and violence before, during and after pregnancy in a national sample of Canadian women. American Journal of Public Health, 102, 1893–1901.
Dekeseredy, W., Schwartz, M., et al. (2003). Perceived collective efficacy and women’s victimization in public housing. Criminal Justice, 3(1), 5–27.
DeSilva, M. J., Huttly, S. R., Harpham, T., & Kenward, M. G. (2007). Social capital and mental health: A comparative analysis of four low income countries. Social Science and Medicine, 64, 5–20.
Edwards, K. M., Mattingly, M. J., Dixon, K. J., & Banyard, V. L. (2014). Community matters: Intimate partner violence among rural young adults. American Journal of Community Psychology, 53, 198–207.
Emery, C. R., Jolley, F. M., & Wu, S. (2011). Desistance from intimate partner violence: the role of legal cynicism, collective efficacy, and social disorganization in Chicago neighborhoods. American Journal of Community Psychology, 48, 373–383.
Fox, G., & Benson, M. (2006). Household an neighbourhood contexts of intimate partner violence. Public Health Reports, 121, 419–427.
Frye, V., Galea, S., et al. (2008). The role of neighbourhood environment and risk of intimate partner femicide in a large urban area. American Journal of Public Health, 98, 1473–1479.
Gielen, A. C., O’Campo, P. J., Faden, R. R., Kass, N. E., & Xu, A. (1994). Interpersonal conflict and physical violence during the childbearing year. Social Science and Medicine, 39(6), 781–787.
Golden, S., Perreira, K., et al. (2013). Troubled times, troubled relationships: How economic resources, gender beliefs, and neighbourhood disadvantage influence intimate partner violence. Journal of Interpersonal Violence, 28(10), 2134–2155.
Gracia, E., Lopez-Quilez, A., Marco, M., Liadiosa, S., & Lila, M. (2014). Exploring neighborhood influences on small-area variations in intimate partner violence risk: A Bayesian random-effects modeling approach. International Journal of Environmental Research in Public Health., 11, 866–882.
Harpham, T., Grant, E., et al. (2004). Mental health and social capital in Cali, Colombia. Social Science and Medicine, 58, 2267–2277.
Hudson, W., & McIntosh, S. (1981). The assessment of spouse abuse: The two quantifiable dimensions. Journal of Marriage and Family, 43(4), 873–885.
Jain, S., Buka, S., et al. (2010). Neighbourhood predictors of dating violence victimization and perpetration in young adulthood: A multilevel study. American Journal of Public Health, 100, 1737–1744.
Kawachi, I., Subramanian, S. V., & Kim, D. (2008). Social capital and health: A decade of progress and beyond. In I. Kawachi, S. V. Subramanian, & D. Kim (Eds.), Social capital and health (pp. 1–26). New York, NY: Springer.
Kim, D., & Kawachi, I. (2006). A multilevel analysis of key forms of community and individual-level social capital as predictors of self-rated health in the United States. Journal of Urban Health, 83(5), 813–826.
Lanier, C., & Maume, M. (2009). Intimate partner violence and social isolation across the rural/urban divide. Violence Against Women, 15, 1311–1330.
Lauritsen, J., & Schaum, R. (2004). The social ecology of violence against women. Criminology, 42(2), 323.
Li, Q., Kirby, R., et al. (2010). A multilevel analysis of individual, household, and neighbourhood correlates of intimate partner violence among low-income pregnant women in Jefferson County, Alabama. American Journal of Public Health, 100(3), 531–539.
Lin, N. (2001). Building a network theory of social capital. Social capital: Theory and Research. In N. Lin, K. Cook, & R. Burt (Eds.), New York: Aldine de Gruyter, (pp. 3–29).
Livingston, M. (2011). A longitudinal analysis of alcohol outlet density and domestic violence. Addiction, 106, 919–925.
McKenzie, K., & Harpham, T. (2006). Meanings and uses of social capital in the mental health field. In K. McKenzie & T. Harpham (Eds.), Social capital and mental health (pp. 11–23). London: Jessica Kingsley Publishers.
McKinney, C., Caetano, R., et al. (2009). Alcohol availability and intimate partner violence among US couples. Alcoholism, Clinical and Experimental Research, 33, 169–176.
McKinney, C., Chartier, K., et al. (2012). Alcohol availability and neighbourhood poverty and their relationship to binge drinking and related problems among drinkers in committed relationships. Journal of Interpersonal Violence, 27(13), 2703–2727.
Miles-Doan, R. (1998). Violence between spouses and intimates: Does neighbourhood context matter? Social Forces, 77, 623–645.
Miles-Doan, R., & Kelly, S. (1997). Geographic concentration of violence between intimate partners. Public Health Reports, 112, 135–141.
Nyqvist, F., Finnas, F., Jakobsson, G., & Koskinen, S. (2008). The effect of social capital on health: the case of two language groups in Finland. Health and Place, 14, 347–360.
O'Campo, P., Burke, J. G., et al. (2005). Uncovering neighbourhood influences on intimate partner violence using concept mapping. Journal of Epidemiology and Community Health, 59, 603–608.
O'Campo, P., Gielen, A., et al. (1995). Violence by male partners against women during the childbearing year: A contextual analysis. American Journal of Public Health, 85, 1092–1097.
O'Campo, P., O'Brien Caughy, M., et al. (1997). A comparison of two analytic methods for the identification of neighborhoods as intervention and control sites for community-based programs. Evaluation and Program Planning, 20(4), 405–414.
O’Campo, P., Wheaton, B., Nisenbaum, R., Glazier, R. H., Dunn, J. R., & Chambers, C. (2015). The Neighborhourhood Effects on Health and Well-being (NEHW) study. Health and Place, 31, 65–74.
Pearlman, D., Zierler, S., et al. (2003). Neighbourhood environment, racial position, and risk of police-reported domestic violence: A contextual analysis. Public Health Reports, 118, 44–58.
Pinchevsky, G. M., & Wright, E. M. (2012). The impact of neighbourhoods on intimate partner violence and victimization. Trauma, Violence and Abuse, 13(2), 112–132.
Portes, A. (1998). Social capital: Its origins and applications in modern sociology. Annual Review of Sociology, 24, 1–12.
Putnam, R. (1993). Making democracy work: Civic traditions in modern Italy. Princteon: Princeton University Press.
Ross, C. E. (2000). Neighborhood disadvantage and depression. Journal of Health and Social Behavior, 41(2), 177–187.
Sampson, R., Raudenbush, S., et al. (1997). Neighbourhoods and violent crime: A multilevel study of collective efficacy. Science, 277, 918–924.
Sherbourne, C., & Stewart, A. (1991). The MOS social support study. Social Science and Medicine, 32(6), 705–714.
Sherin, K. M., Sinacore, J. M., Li, X. Q., et al. (1998). HITS: A short domestic violence screening tool for use in a family practice setting. Family Medicine, 30(7), 508–512.
Tomaszewski, E. (2002). “Public” and “Private” crimes against women in Eastern Ontario public housing: The role of perceived collective efficacy. Ottawa: Carleton University.
Van Wyk, J., Benson, M., et al. (2003). Detangling individual-, partner-, and community-level correlates of partner violence. Crime and Delinquency, 49(3), 412–438.
Waller, M., Iritani, B., et al. (2012). Relationships among alcohol outlet density, alcohol use, and intimate partner violence victimization among young women in the United States. Journal of Interpersonal Violence, 27(10), 2062–2086.
Wright, E. M., & Benson, M. (2011). Clarifying the effects of neighbourhood disadvantage and collective efficacy on violence “behind closed doors”. Justice Quarterly, 28, 775–798.
Zolotor, A., & Runyan, D. (2006). Social capital, family violence and neglect. Pediatrics, 117(6), e1124–e1131.
Acknowledgments
Project NEHW was funded through research grants from the Canadian Institutes of Health Research and the Social Sciences and Humanities Research Council. We would like to thank Kristen O’Brien and Rosane Nisenbaum for their contributions to the data analyses.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kirst, M., Lazgare, L.P., Zhang, Y.J. et al. The Effects of Social Capital and Neighborhood Characteristics on Intimate Partner Violence: A Consideration of Social Resources and Risks. Am J Community Psychol 55, 314–325 (2015). https://doi.org/10.1007/s10464-015-9716-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10464-015-9716-0