Abstract
Numerous contextual factors contribute to risky sexual decision-making among men who have sex with men (MSM), with experimental laboratory-based studies suggesting that alcohol consumption, sexual arousal, and partner familiarity have the potential to impact condom negotiations during sexual encounters. The purpose of the current study was to extend this line of inquiry outside of the laboratory and into the everyday lives of MSM. We collected six weeks of daily data on alcohol consumption and sexual behaviors from 257 moderate- and heavy-drinking MSM to examine the within- and between-subjects effects of alcohol consumption, average daily sexual arousal, and partner familiarity on condom negotiation processes during sexual encounters. We hypothesized that alcohol consumption, higher levels of average daily sexual arousal, and greater partner familiarity would all contribute to a reduced likelihood of condom negotiation prior to sexual activity, and that they would also affect the difficulty of negotiations. Contrary to hypotheses, none of these three predictors had significant within-subjects effects on condom negotiation outcomes. However, partner familiarity and average daily sexual arousal did exert significant between-subjects effects on the incidence of negotiation and negotiation difficulty. These findings have important implications for risk-reduction strategies in this population. They also highlight the challenges of reconciling results from experimental laboratory research and experience sampling conducted outside of the laboratory on sexual risk behavior.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Men who have sex with men (MSM) are at disproportionate risk for contracting HIV and account for approximately 70% of the 40,000 new cases of HIV that are diagnosed in the United States each year [1]. New HIV infections among MSM are almost universally the result of engaging in either insertive or receptive condomless anal intercourse (CAI) with an infected partner [2]. While there are now biomedical preventions like pre-exposure prophylaxis (PrEP) that can prevent HIV infection with a daily pill [3, 4], condoms remain the most common method of HIV infection prevention across the globe [5]. Most intervention approaches to preventing HIV infection focus on education, skill-building, and structural changes around condoms, including increasing condom use, improving condom use skills, and making condoms more widely accessible to those who need them [6,7,8]. Even with efforts to increase condom usage, however, there is compelling epidemiological and experimental evidence that alcohol and substance use directly increases the likelihood that MSM will demonstrate changes in intentions and/or attitudes toward having sex without a condom, increasing the likelihood of infection by HIV and other STIs [9,10,11,12,13,14]. Identifying the mechanisms by which alcohol and other substances exert their influence on decisions about condom use, as well as what individual differences may make certain people more or less susceptible to their risk-enhancing effects, is a matter of urgent public health inquiry.
Associations between alcohol use and subsequent CAI among MSM have been examined through laboratory-based alcohol administration studies and epidemiological studies [12, 13, 15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34], and daily diary, timeline follow-back, and event-level (ecological momentary assessment [EMA] or experience sampling method [ESM]) studies [35,36,37,38,39]. In the laboratory, alcohol administration (especially in doses that produce a blood alcohol level of 0.075% or higher [24]) has been shown to promote CAI [36] by increasing intentions to engage in condomless sex [12, 13, 21, 22] and decreasing the effectiveness of communication about safer sexual behavior [21, 22]. In addition, epidemiological studies have shown that the association between alcohol use and sexual risk behavior is moderated by a number of individual difference factors [23, 24], including cognitive schemas like sexual alcohol expectancies [25,26,27], sexual sensation seeking [18, 19], impulsivity [17, 20], cognitive reserve and executive functioning [15, 16], and history of sexual abuse or sexual victimization [28,29,30,31,32,33,34]. Daily diary and event-level studies, which examine the association between alcohol consumption and sexual behavior in the real world (e.g., outside of the laboratory, with fewer experimental controls), have not provided similarly conclusive evidence about alcohol’s effects on risky sexual behavior, however [37,38,39]. In this regard, they have suggested that moderating variables like motivation for having sex, perceptions of risk, availability of condoms, and partner familiarity [36, 39] may also significantly impact alcohol-involved sexual decision-making. Simons et al. [35] and Maisto et al. [36] reported non-linear associations between alcohol consumption and the likelihood of condomless sex, such that among heterosexual young adults [35] and MSM [36], condomless sex on a given day was more likely when intoxication exceeded an individual’s average daily level of alcohol consumption. These results paint a complex picture in which sexual risk behavior can be affected not only by person-level factors but also by the “dynamic situational and relationship factors” (p. 319) that influence sexual decision-making within-persons as they occur in the natural environment [40]. Event and daily-level studies permit the modeling of within-person effects by examining how situational factors, which include both internal states and external contexts, affect decisions about sexual health and sexual risk. In the present study we sought to capitalize on the unique insights that can be gained by examining how changes in environment may contribute to event-level, within-subjects decisions about the use of condoms during sexual encounters.
One important determinant of condomless intercourse appears to be whether partners discuss condom use prior to engaging in sexual activity [41,42,43]. In a meta-analysis of 53 studies that included heterosexual couples as well as MSM, Noar et al. [42] found a modest positive relationship (r = .25) between communication/negotiation about condom use and subsequent condom usage. This finding has been replicated in a number of additional studies, including a meta-analysis of interventions to increase safer-sex communication between partners [41], which found that participants in the active intervention conditions both discussed condom use and actually used condoms more frequently than those in control conditions. Another study in the southern United States found that young Black men who engaged in condom use discussion with partners had a significantly reduced incidence of STI infection than those who did not [44]. Widman et al. [45] found that HIV-positive individuals who had greater intentions to discuss condom use and engaged in more condom discussion behavior had significantly less condomless sex than those with weaker intentions and less frequent condom discussion behavior. Other findings include the fact that men (both those who have sex with women and those who have sex with men) tend to be more reluctant to initiate discussions about condom use than women [46] and that MSM tend to assume that their partners have similar attitudes toward condom use and thus may shy away from condom use discussions or safe sex negotiations [46]. While there are individual difference factors that predict condom-use negotiations with sexual partners (e.g., intentions to have negotiations [45, 47]), research has also indicated that “the decision to use condoms…with a particular partner is highly situational, and the same person often chooses to use condoms with some partners and not others, or during some sex acts versus others” (p. 1852) [48]. Other factors that may contribute to the decision to use condoms and have been studied include feeling conflicted about using a condom versus experiencing potentially more thrill or greater pleasure with condomless intercourse [49, 50], having a history of intimate partner violence [51], and equating the suggestion of condom use with mistrust [52]. Still other potential contributors to situational differences in the difficulty of negotiation may include challenges associated with curtailing arousal and potentially delaying intercourse to have a discussion about using condoms, or fearing rejection from a partner who might prefer to forgo condom use. Expanding our understanding of the situational factors that contribute to decisions about condom negotiation is likely of critical importance to developing more effective approaches to HIV prevention.
Although alcohol intoxication is a key situational factor that affects sexual decision-making, only a few published experimental studies have examined the effects of alcohol on condom negotiation skills among MSM [21, 22]. These studies have shown that condom negotiation skills are less proficient for participants who consume alcohol compared to those who do not. For example, in one laboratory-based alcohol administration study of 117 MSM, Maisto and colleagues [21] found that participants who received alcohol scored lower on measures of condom negotiation compared to participants who received a control or placebo beverage. In a secondary analysis of these data, Buckheit et al. [53] found an interaction between sexual arousal and perceived intoxication on condom negotiation skills: at low levels of sexual arousal, perceived intoxication actually increased condom negotiation skills, perhaps due to a reduction in anxiety around discussing condom use. At high levels of sexual arousal, however, perceived intoxication was related to decrements in condom negotiation skills. This work suggests that situational factors can both directly impair and interact with one another to significantly affect condom negotiation during sexual encounters.
A number of other situational factors linked to sexual decision-making have also been proposed in the HIV prevention literature, including partner familiarity (or lack thereof) [40, 54] and sexual arousal [15, 53, 55,56,57,58,59]. Partner familiarity is a complex construct that has often been defined by asking participants to rate how well they know a partner using Likert-like scale items, or to characterize partners in categorical terms such as primary (whether monogamous or non-monogamous), casual, or anonymous [36, 60, 61]. Studies of partner familiarity have reported conflicting findings. For example, condoms are used less-often during sexual encounters with familiar or primary partners, compared to casual or anonymous partners [60,61,62]; this is hypothesized to stem from the questionable assumption that more familiar partners present less risk for HIV and other STIs [61]. Other research suggests that for intoxicated individuals, condomless sex becomes more likely with less-familiar partners [63,64,65], though this has not been an unequivocal finding [35, 66]. Like partner familiarity, sexual arousal has been studied extensively. In laboratory studies, higher self-reported assessments of subjective sexual arousal have been linked to greater intentions to engage in condomless sex across populations, including among men who have sex with women [56, 57, 67,68,69,70] and MSM [13, 14, 21, 53], with one recent study of MSM [71] demonstrating an interaction effect between alcohol consumption and sexual arousal on CAI indirectly through implicit approach biases toward sexual stimuli relative to condoms. Interestingly, objective measures of sexual arousal, like autonomic or physiological arousal (as might be measured by penile plethysmography) have not been consistently linked to increased intentions to engage in condomless intercourse [72, 73].
Purpose of the Current Study
The purpose of this research was to examine the interactive, situation-specific effects of alcohol, partner familiarity, and sexual arousal on the likelihood that MSM would engage in condom use discussions with a potential partner prior to sexual intercourse. Previous research has suggested that whether such discussions occur is critical to subsequent condom-use decisions [42, 43] and laboratory-based alcohol administration studies have confirmed that alcohol consumption impairs condom negotiation skills [21, 22, 53]. Better understanding of the impact of these situation-specific factors has the potential to improve HIV prevention interventions by identifying the situation(s) in which condom negotiation is likely and unlikely to occur among MSM; education and training to recognize these situations may help reinforce the importance of condom use discussions and negotiations. We hypothesized that within subjects: (1) alcohol intoxication would decrease the likelihood of condom use discussion/negotiation prior to sexual activity, and (2) greater sexual arousal and greater partner familiarity would interact with alcohol consumption to further decrease the likelihood of condom use discussion/negotiation. In addition, a secondary aim was to examine how alcohol consumption, sexual arousal, and partner familiarity affected the self-reported ease with which condom use discussions occurred.
Use of Experience Sampling Method
Accurate modeling of the within-subjects effects of situation-specific factors requires the use of intensive longitudinal data [74, 75]. For this study, participants first completed two laboratory-based visits; thereafter, longitudinal data were collected via the experience sampling method (ESM), in which participants completed up to nine daily survey assessments through a smartphone-based mobile application platform. The analyses in this paper involve the ESM data only. Research has indicated that MSM are receptive to ESM-based study designs [22, 39, 76], particularly as smartphone ownership has expanded and mobile apps have been developed for the specific purpose of collecting ESM data [77, 78].
Methods
Participants
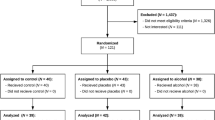
Participants were 257 men aged 21 to 50 years (M = 28.09 years, SD = 6.82 years) who were recruited via print and electronic means (e.g., advertisements in social media apps like Facebook, Grindr, and Scruff) in urban areas in the northeastern United States. See Table 1 for additional demographic data. Data were collected between May 2016 and March 2020. Of the 257 men, 208 were included in the analyses. Eighteen were excluded because they reported zero instances of oral or anal sex during the ESM portion of the study. An additional 22 were excluded because they responded to less than 33% of either the morning or random surveys (this a priori decision to exclude participants with response rates below 33% was also applied to the data analyses in the Maisto et al. paper [36] using this same dataset). The decision to exclude these participants was based on concerns that data collected from participants with low response rates might reflect a non-representative sample of their behavior. Finally, 9 additional participants were excluded because they never enrolled in the ESM portion of the study after giving consent. The 49 excluded participants did not differ from the 208 included participants in age, PrEP use, lifetime number of sexual partners, or frequency of condom use. They did differ in terms of number of past-year and past-90-day sexual partners, however, with the included participants having, on average, approximately 4 more past-year (t = -2.743, p = .007) and 1 more past-90-day sexual partners (t = -2.073. p = .041).
Inclusion criteria for the study included being (1) 21–50 years old, (2) a moderate or heavy drinker as per the Quantity-Frequency-Variability (QFV) Questionnaire [79] (the QFV asks participants about how frequently they consume beer, wine, and higher-proof alcohol and then uses a matrix to classify each participant as a light, moderate, or heavy drinker), (3) sexually active with other men (with an average of at least one same-sex sexual encounter per month during the three months prior to enrollment in the study), (4) gay or bisexual (as indicated by a score of three or higher on the Kinsey Scale [80]), and (5) single or in a non-monogamous sexual relationship. Because the primary study included an alcohol administration component in the laboratory [71], additional exclusionary criteria included (1) current medical conditions that are incompatible with alcohol administration, (2) current diagnosis of a psychiatric disorder, (3) regular use of medications (both prescribed and over the counter), supplements, and herbs that contraindicate alcohol consumption, (4) current diagnosis of an alcohol or substance use disorder, (5) alcohol treatment within the past three years, (6) substance use disorder or mental health treatment during the past three months (except for purely supportive therapy for individuals never diagnosed with a mental disorder), and (7) history of treatment for either schizophrenia or bipolar disorder.
Procedure
After responding to an advertisement, interested individuals were contacted by a research assistant and completed an initial telephone screen. If eligible, participants were scheduled to attend two laboratory sessions and thereafter were enrolled into the ESM portion of the study. The ESM portion was divided into two “bursts” of three weeks each with a three-week break between the first and second burst. Total ESM enrollment time was therefore nine weeks, but data collection occurred during only the first three weeks and the final three weeks. In addition, two extra days were included in each burst (i.e., 23 days of data collection instead of 21) to increase the likelihood of 21 complete days of data collection. Informed consent was obtained from all participants for both the laboratory and ESM portions of the study.
ESM data collection occurred via the MetricWire research platform (MetricWire, Inc.), which features a participant-side smartphone app and a researcher-side website. Participants completed two types of surveys during the two bursts: a morning survey, which was triggered at 8 am each morning (with a 10 am reminder if the participant had not yet responded to the survey), and random surveys, which were triggered at random times in two-hour blocks between 10 am and 2 am, for a total of eight random surveys per 24-hour period. Random surveys expired 30 min after being triggered, with a reminder sent after 15 min to encourage prompt responding. The morning survey collected data about alcohol consumption and sexual encounters during the previous evening; the random surveys collected data about alcohol consumption within the previous 30 min.
During the two ESM bursts, research assistants contacted each participant at least weekly to provide feedback on response rates, to either praise participants for completing 85% or more of the random surveys or to ask them to increase their response rates to 85% or above. Participants earned $3.00 per each completed morning assessment, $1.00 for each random assessment, and a $23.00 bonus for completing an uninterrupted week of morning assessments. Participants could earn up to $100 per week (or $14.29 per day) if they completed all assessments. Compensation was paid in cash at the end of each burst.
Measures
Experience Sampling
Discussion of Condom Use. Data on discussion of condom use was collected as part of the morning assessment using a question constructed for this study that was adapted from similar questions used during previous research that inquired about the likely difficulty of condom negotiation in a hypothetical situation [81]. For each sexual partner from the previous evening, the participant answered the question: How easy/difficult was it to discuss the use of a condom with this partner? (answer choices: N/A [did not discuss], very difficult, somewhat difficult, somewhat easy, easy, very easy). Answer choices were recoded to indicate whether discussion occurred (Yes/No), and if so, how easy the discussion was (1 = very easy, 5 = very difficult).
Intoxication. A standardized estimate of intoxication during each evening was created by averaging three standardized variables derived from the ESM data: (1) the number of drinks each participant consumed during the 30 min prior to each random assessment during the previous evening, (2) an estimate of the maximum blood alcohol content (BAC) level during the previous evening, calculated from reports of the numbers of drinks consumed and the number of hours spent drinking, and (3) each participant’s subjective assessment of his own level of intoxication (1–7 scale: 1 = not at all, 7 = extremely) during the previous evening. This yielded a composite variable that was used to represent intoxication during each evening in the ESM portion of the study. Examination of the intoxication variable identified two data points as outliers because they were more than three standard deviations away from the sample mean; per the recommendations of Tabachnick and Fidell [82], those two outliers were recoded to one unit greater than the nearest data point prior to analyses. Reliability analysis of the composite variable revealed high levels of both within-persons (McDonald’s Omega = 0.85) and between-persons (McDonald’s Omega = 0.89) reliability [36, 83].
Sexual Arousal. Sexual arousal scores were derived from random assessment data: for each day, an average daily sexual arousal score was computed by averaging the sexual arousal scores (1 = not at all, 7 = very aroused) reported during all completed random assessments during the day.
Partner Familiarity. Partner familiarity was assessed during each morning assessment. A single question asked participants to report how well they knew each partner. Answers were provided on a 7-point scale (1 = not at all, 7 = very well).
Use of “riskiest sexual encounter” data. For days on which participants reported having a sexual encounter with more than one partner, we used the condom discussion and partner familiarity data from the partner with whom each participant had the riskiest sexual encounter. The riskiest sexual encounter was defined using the following hierarchy, from riskiest to least risky: (1) participant had condomless receptive anal intercourse, (2) participant had condomless insertive anal intercourse, (3) participant had receptive anal intercourse with a condom, (4) participant had insertive anal intercourse with a condom, and (5) participant engaged in oral sex only.
Data Analysis Plan
Data were analyzed using logistic and linear multilevel structural equation modeling (MSEM) with random slopes in Mplus version 8.5 [84]. Using logistic models, we first estimated the within- and between-subjects effects of intoxication, average daily sexual arousal, and partner familiarity on the likelihood that condom discussion occurred, with a categorical outcome: yes and no. At level 1, intoxication, average daily sexual arousal, partner familiarity, intoxication x average daily sexual arousal, intoxication x partner familiarity, elapsed days in the study, and six day of the week indicators (with Sunday as the reference day) were used as predictors. At level 2, study site (either Boston, MA or Syracuse, NY), intoxication, average daily sexual arousal, partner familiarity, intoxication x average daily sexual arousal, intoxication x partner familiarity, age, and PrEP use were predictors. Continuous level 1 variables were centered at the person-mean and the level 2 variables were centered at the grand-mean to allow decomposition and estimation of within- and between-subjects effects [85]. Linear multilevel models were constructed in the same fashion to predict ease of discussion as a continuous outcome variable. All variables used in these models were observed; no latent variables were included in the analyses.
Results
Protocol Compliance
Participants included in the analyses completed 93% (SD = 0.09, median = 0.96) of the morning assessments administered during the ESM portion of the study. For the random assessments, the response rate was 72% (SD = 0.11, median = 0.74). This amounted to 9,301 individual morning assessments from the 208 participants, with an average of 42.8 (SD = 4.5, median = 44) completed morning surveys per participant (range, 12–65).Footnote 1
Descriptive Statistics for the ESM Portion of the Study
Of the 9,301 days of data collected during the study, participants reported having some sort of sexual contact on 1,775 days (19.1% of days). Four hundred and thirty-nine of those instances did not include oral or anal sex (4.7% of days), 420 included oral sex only (4.5% of days), and 915 included anal sex (9.8% of days). During those 915 days of anal sex, participants reported 640 insertive sex acts and 545 receptive sex acts, for a total of 1,185 anal sex acts. Most of those instances of anal sex occurred without the use of condoms: of the 640 insertive anal sex acts, 238 (37.2%) occurred with a condom and 402 (62.8%) occurred without a condom. Of the 402 acts of condomless insertive anal intercourse, 126 (31.3%) occurred among participants who reported PrEP use and 276 (68.7%) occurred among non-PrEP users. Similarly, of the 545 receptive anal sex acts, 179 (32.8%) occurred with a condom and 366 (67.2%) occurred without a condom. Of the 366 condomless acts of receptive anal intercourse, 122 (33.3%) occurred among participants who reported PrEP use and 244 (66.6%) occurred among non-PrEP users. When combined, these statistics indicate that of the 1,185 acts of anal sex reported during the ESM portion of the study, 417 (35.2%) involved condom use, and of the 768 condomless anal sex acts, 248 (32.3%) involved participants using PrEP and 520 (67.7%) involved participants not using PrEP. Discussions about using condoms proceeded anal sex on 499 (54.5%) of the days on which anal sex acts were reported. The average discussion difficulty rating was 1.7 out of 5.0.
Multilevel Structural Equation Models
Condom Use Discussion
Preliminary analyses revealed that neither intoxication (b = 0.093, p = .571) nor average daily sexual arousal (b = 0.200, p = .239) had significant variation in slope across participants, so those effects were fixed in the final analysis rather than allowed to vary randomly. Intoxication did not moderate the relationship between partner familiarity and the likelihood of condom use discussion at the within- (odds ratio [OR] = 0.943, p = .339) or between-subjects (OR = 2.073, p = .126) levels, nor did intoxication moderate the association between average daily sexual arousal and discussion occurrence at the within- (OR = 1.121, p = .382) or between-subjects (OR = 1.923, p = .426) levels. As such, the interaction terms were dropped from the final model (see Table 2 for final model output). The removal of the interaction terms led to an improvement in model fit per the Akaike Information Criterion (AIC): the original model, with the interactions, had an AIC of 951.459 while the final model had an AIC of 941.316, a decrease of 10.143 AIC units [86, 87]. Contrary to hypotheses, there were no within-subjects effects of intoxication (OR = 1.173, p = .288), average daily sexual arousal (OR = 0.926, p = .521), or partner familiarity (OR = 0.851, p = .296) on the likelihood of having a condom use discussion with a potential sexual partner, nor did the day of the week indicators show significant effects for particular days of the week. At the between-subjects level (i.e., level 2), however, partner familiarity was a significant predictor of having a condom use discussion along with covariates PrEP use and age. Between subjects, increases in partner familiarity predicted a significant decrease in the likelihood of condom use discussion, OR = 0.514, p = .001 for each unit increase in partner familiarity, 95% CI for OR = 0.342, 0.771. The odds ratio for PrEP use was 0.162, p = .020, 95% CI for OR = 0.035, 0.750 so that PrEP users were significantly less likely to have condom use discussions than non-users. Finally, older participants were less likely to have condom use discussions than younger participants, with an OR of 0.901, p = .030, 95% CI for OR = 0.820, 0.990, for each year increase in age.
Difficulty of Condom Discussion
Similar to the findings above, none of the three variables had significant variation in slope across clusters (intoxication, b = 0.003, p = .799; average daily sexual arousal, b = 0.017, p = .240; partner familiarity, b = 0.022, p = .228), so all were treated as fixed effects at the within-subjects level. As above, the hypothesized interaction effects were non-significant (intoxication did not moderate the association between partner familiarity and the difficulty of condom use discussion at the within- [b = 0.000, p = .988] or between-subjects [b = -0.043, p = .693] levels, nor did intoxication moderate the association between average daily sexual arousal and discussion difficulty at the within- [b = -0.023, p = .192] or between-subjects [b = -0.021, p = .893] levels) and as such were dropped from the final model (see Table 3 for final model output). As with the analysis of condom use discussion, removal of the interaction terms resulted in an improvement in model fit per AIC: with interactions, the AIC was 1620.711, whereas the AIC decreased to 1614.806 when the interaction terms were removed, resulting in a decrease of 5.905 AIC units [86, 87]. There were no within-subjects effects of intoxication (b = -0.014, p = .656), average daily sexual arousal (b = 0.006, p = .824), or partner familiarity (b = -0.023, p = .230) at the within-subjects level, nor were there significant effects from any of the six day of the week indicators. At the between-subjects level, there were significant effects of average daily sexual arousal (b = 0.197, p = .027) and partner familiarity (b = -0.095, p = .004) on the difficulty of condom discussion, indicating that between subjects, difficulty increased with average daily sexual arousal and decreased with partner familiarity. Neither PrEP use (b = -0.121, p = .350) nor age (b = 0.009, p = .379) were significant predictors of discussion difficulty at the between-subjects level.
Discussion
Previous research has identified alcohol consumption as a causal contributor to risky sexual behavior in analogue laboratory tasks, especially when blood alcohol levels of 0.075% or higher have been recorded [24, 36, 88]. Laboratory studies of the effects of alcohol on condom negotiation among MSM have yielded similar results, with intoxication associated with impaired condom negotiation skills [21, 22]. Given that context, the results of the present study were largely contrary to expectations. Using longitudinal data from 9,301 daily surveys across 208 MSM participants, we did not find within- or between-subjects effects of alcohol intoxication on either the likelihood of condom use discussion prior to a sexual encounter or the difficulty of such discussions when they occurred. This finding with event-level data is inconsistent with laboratory-based research conducted over the past decade in which alcohol was found to impair condom negotiation skills, decrease the efficacy of safer sex negotiations, and increase intentions to engage in condomless intercourse [13, 21, 22, 53, 58, 89], though such differences may be due to a variety of factors, including the fact that condom-related constructs examined in laboratory studies were measured differently than in the current study. For example, Maisto and colleagues’ protocol [21] required all participants to complete a series of video-based tasks that included a condom negotiation exercise. In our study, by contrast, participants reported on their real-world negotiation behavior, which was not prompted or encouraged by any external source. Indeed, our data suggest that actual instances of condom negotiation between two MSM sexual partners in the “real world” occur prior to anal sex only a little more than half the time. Additionally, condom negotiation difficulty was operationalized differently in the present study (a simple ranking of each participant’s own interpretation of “difficulty” on a 5-point Likert scale) than in past laboratory research [81] during which participants were asked to estimate how difficult it would be to enact condom negotiation skills. Inconsistencies between results from laboratory-based and longitudinal EMA study designs have been noted in the sexual risk literature for more than two decades [36, 37], and our present results may be yet another example of that phenomenon. It is also possible that the relative infrequency with which negotiations occurred in our survey data limited our ability to detect significant intoxication effects.
The absence of within-subjects effects for average daily sexual arousal and partner familiarity was also unexpected, given findings from previous studies using daily diary data [48], but that absence nonetheless provides important insight into sexual decision-making processes among MSM. We expected that differences in arousal and partner familiarity would lead individual participants to have condom use discussions with some partners and not others, but we found that variation in these important contextual factors within participants did not significantly affect either the likelihood of discussion or the difficulty with which such discussions were carried out. Instead, we observed effects at the between-subjects level, both for partner familiarity and average daily sexual arousal. Higher average partner familiarity between participants was associated with lower likelihood of having condom use discussions. For discussion difficulty, however, higher average daily sexual arousal was associated with more difficult condom use discussions whereas higher partner familiarity was associated with greater ease. These findings suggest that individual participants are less influenced by changing environmental factors than we had hypothesized, and that they instead tend to have similar approaches to having discussions about condom use across partners, so that discussions were less likely, on average, for those with more familiar partners. For discussion difficulty, participants who reported greater average daily arousal found discussions to be more difficult, but those with greater average familiarity reported easier discussions. These findings suggest that individual differences for familiar sexual partners may be a function, at least in part, of perceptions that those partners may be more receptive to having discussions about condoms (and perhaps other matters of sexual health) prior to having sex. Since these findings occurred at the between-subjects rather than the within-subjects level, another possibility is that the partner familiarity variable might reflect individual differences in study participants’ preferences for sexual relationships: for example, participants with lower average partner familiarity ratings might prefer more casual relationships or experience lower levels of intimacy in sexual relationships than participants who reported higher average levels of partner familiarity. Future research in this area would likely benefit from assessing partner familiarity with a more nuanced set of questions to better understand how different facets of familiarity may affect discussions about condom use.Footnote 2 The increased difficulty of having condom discussions for participants with greater average levels of daily arousal may reflect a potential fear of loss: for example, it might be associated with concerns that engaging in condom use discussions could interrupt or end the sexual encounter, which might be less acceptable for individuals with higher average daily levels of sexual arousal. These between-subjects findings accord with past research into contextual influences on sexual decision-making, which have identified both sexual arousal [15, 53, 55,56,57,58,59] and partner familiarity [40, 54] as important influences on decision-making processes.
Our findings of these between-subjects effects have important implications. First, they both replicate and extend the results of the experimental studies cited above by confirming that the relationships between sexual arousal, partner familiarity, and sexual decision-making identified in those studies extend to real-world sexual encounters. Second, they demonstrate the benefit of combining laboratory-based and ESM data collection approaches when studying a complex phenomenon like sexual decision-making. Laboratory-based research has provided a wealth of information on specific processes that have been hypothesized to influence sexual encounters [72], but laboratory methods are necessarily limited in their ability to replicate the contexts in which decisions about sexual encounters are made. ESM research, on the other hand, allows researchers to collect data about “heat of the moment” processes in those contexts, so that the resulting data can be assumed to capture variation due to contextual effects, but at the cost of the strict controls that can be instituted in a laboratory. Careful comparison and combination of results from both types of research will be of great value in advancing our understanding of the mechanisms that affect the risk associated with sexual encounters and the development of interventions to reduce that risk.
Our findings also have important implications for sexual risk reduction efforts in MSM populations. First, the significant between-subjects effects suggest that intervention approaches which seek to educate and teach skills, like those based on the Information-Motivation-Behavior (IMB) skills model [90], can focus on education about avenues of risk that occur more generally between individuals rather than risk that derives from moment-to-moment changes in environmental conditions that may inconsistently affect CAI from person to person. The knowledge that participants in this study did not vary their behavior related to condom discussion in significant ways while intoxicated, contemplating intercourse with partners of differing familiarity, or during periods of differing levels of average daily sexual arousal, offers intervention developers valuable information about how to improve the approach and efficacy of their interventions. Second, the results imply that there may be contextual factors other than intoxication, sexual arousal, and partner familiarity that may be of greater importance to predicting condom use discussions within subjects: elucidation of these factors may be critical for the development of more efficacious risk-reduction approaches. One potentially important factor that was not a focus of the current study is the perceived “riskiness” of sexual partners, as determinations about risk are likely antecedents to decisions about whether to discuss condom use with any partner. If a partner is judged to present relatively little risk, then there may be no impetus to discuss condom usage prior to having sex. Risk perception is a complex process at the best of times, with research showing that assessments about risk can be influenced by intoxication [58, 91,92,93], the relationship “potential” of partners [31, 94, 95], whether the partner is new or already known [94], the goals and motivations that are attached to the sexual encounter [96], and the relative strength of impelling and inhibiting risk-related cues in the environment [68, 72, 97]. Not all of these cited studies were conducted with MSM populations, but they together demonstrate the many ways in which context can influence risk perception and thus decisions about the necessity of discussing condom use prior to having sex. A third implication of our findings is that they suggest that individuals who tend to become more sexually aroused as well as those who tend to have sex with less-familiar partners might derive particular benefit from interventions that encourage having discussions about condom use and provide skills to make those conversations easier.
There are several limitations to our study that are important to consider. First, the manner of our data collection (i.e., using data collected during the morning after sexual encounters) means that most of the data used in the analyses were based on retrospective reports rather than assessments contemporaneous to when decisions about condom use discussions were being made. Second, while our measurement of condom negotiation difficulty was necessarily limited to discussions that did occur, we had no way to assess whether high anticipated difficulty contributed to a decision not to engage in negotiations: this may be one reason why the average rating of discussion difficulty was relatively low in this dataset, with few examples of more difficult discussions. Third, the use of single nightly intoxication and average daily sexual arousal scores means that our analyses were based on the average sexual arousal and average nightly intoxication conditions that the participant experienced each day during the study rather than the particular intoxication and arousal conditions that existed as participants were deciding whether to discuss condom use with their partners. These limitations might have been avoided had we asked participants to self-initiate data collection surveys immediately before or after sexual encounters—it’s possible, for example, that intoxication and sexual arousal were significantly different from their average, evening-wide values during these critical periods when participants were considering whether to speak to their partners about using a condom. Research is needed to determine whether study participants would be willing and/or able to pause their sexual activities to provide data during these most intimate of occasions. If so, such data could provide more accurate representations of the context in which these important decisions are made.
Finally, this study did not capture information on how participants met their partners, which may have important implications for condom negotiation. For example, if some participants met their partners on geospatial networking (GSN) apps (e.g., Grindr, Scruff), individual profiles may have provided detailed information about sexual risk variables (e.g., HIV status, date of last HIV/STI testing, and PrEP use) and condom use preference (e.g., a preference for or against using a condom), which may have obviated the need for robust condom negotiation discussions. However, recent research has shown that men who use GSN apps like Grindr tend to report more risky sexual outcomes than those who do not [98, 99]: for example, in one recent study, participants who had used Grindr in the seven days prior to data collection reported more male sexual partners, more CAI, and more diagnoses of STIs like gonorrhea and chlamydia than those who had not used Grindr during the same period [100]. These findings suggest that gleaning information about sexual risk from online profiles does not necessarily reduce sexual risk, and that condom negotiation discussions may be beneficial for MSM partners even when information about sexual risk and preference variables are readily available on GSN app profiles.
To our knowledge, this was the first ESM study to examine on a within- and between-subjects basis how intoxication, average daily sexual arousal, and partner familiarity may impact the likelihood of condom negotiation in a sample of MSM at high risk of exposure to HIV and other STIs. Our findings underscore the importance of extending findings from previous laboratory-based experimental studies into the natural environment as the current findings do not appear to be consistent with previous laboratory data on the causal effects of intoxication, sexual arousal, and partner familiarity on condom use negotiation between MSM partners prior to engaging in anal sex. Inconsistencies between laboratory findings and data collected in naturalistic settings are not new, especially in research on sexual health and decision-making [37,38,39], and should serve as reminders that these two approaches and their respective characteristics—high levels of internal control with potentially low external validity in the laboratory alongside minimal internal controls with high levels of external validity in naturalistic settings—can both yield valuable insights. More research, including laboratory-based studies that can investigate theoretical constructs with great precision and environmental-based studies that can capture data as sexual decision-making processes are unfolding “in the heat of the moment”, will be required to advance this important line of inquiry and help develop intervention approaches to increase both the likelihood that condom use discussions will occur before having sex and the ease with which individuals will be able to engage in such conversations.
Data Availability
The data collected during this study are available on request from the authors.
Code Availability
Not applicable.
Notes
Two participants provided more than six weeks of survey data. They were both unable to complete one of the ESM bursts, the first due to lack of internet access during international travel and the second due to a broken phone. Both asked if they could re-enroll in the missed burst and we decided to allow them to do so. During analyses, we included all ESM data collected from both participants as a way of respecting the effort they had committed to the study.
We appreciate the comments of one of our reviewers for offering this perspective on these results.
References
Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2018 (updated) [Internet]. 2020 May. Available from: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html.
Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380:367–77. https://doi.org/10.1016/S0140-6736(12)60821-6.
Liu AY, Cohen SE, Vittinghoff E, Anderson PL, Doblecki-Lewis S, Bacon O, et al. Preexposure prophylaxis for HIV infection integrated with municipal- and community-based sexual health services. JAMA Intern Med. 2016;176:75. https://doi.org/10.1001/jamainternmed.2015.4683.
Young I, McDaid L. How acceptable are antiretrovirals for the prevention of sexually transmitted HIV? A review of research on the acceptability of oral pre-exposure prophylaxis and treatment as prevention. AIDS Behav. 2014;18:195–216. https://doi.org/10.1007/s10461-013-0560-7.
Krishnaratne S, Hensen B, Cordes J, Enstone J, Hargreaves JR. Interventions to strengthen the HIV prevention cascade: a systematic review of reviews. Lancet HIV. 2016;3:e307–17. https://doi.org/10.1016/S2352-3018(16)30038-8.
Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho M-H. A test of major assumptions about behavior vhange: a comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull. 2005;131:856–97. https://doi.org/10.1037/0033-2909.131.6.856.
Fishbein M, von Haeften I, Appleyard J. The role of theory in developing effective interventions: implications from Project SAFER. Psychol Health Med. 2001;6:223–38. https://doi.org/10.1080/13548500123176.
Traube DE, Holloway IW, Smith L. Theory development for HIV behavioral health: empirical validation of behavior health models specific to HIV risk. AIDS Care. 2011;23:663–70. https://doi.org/10.1080/13548500123176.
Hojilla JC, Vlahov D, Glidden DV, Amico KR, Mehrotra M, Hance R, et al. Skating on thin ice: stimulant use and sub-optimal adherence to HIV pre-exposure prophylaxis. J Int AIDS Soc. 2018;21:e25103. https://doi.org/10.1002/jia2.25103.
Oldenburg CE, Mitty JA, Biello KB, Closson EF, Safren SA, Mayer KH, et al. Differences in attitudes about HIV pre-exposure prophylaxis use among stimulant versus alcohol using men who have sex with men. AIDS Behav. 2016;20:1451–60. https://doi.org/10.1007/s10461-015-1226-4.
Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr. 2007;45:85–92. https://doi.org/10.1097/QAI.0b013e3180417c99.
Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: systematic review and meta-analysis of experimental studies. Addict. 2012;107:51–9. https://doi.org/10.1111/j.1360-0443.2011.03621.x.
Shuper PA, Joharchi N, Monti PM, Loutfy M, Rehm J. Acute alcohol consumption directly increases HIV transmission risk: a randomized controlled experiment. J Acquir Immune Defic Syndr. 2017;76:493–500. https://doi.org/10.1097/QAI.0000000000001549.
Shuper PA, Fisher WA. The role of sexual arousal and sexual partner characteristics in HIV + MSM’s intentions to engage in unprotected sexual intercourse. Health Psychol. 2008;27:445–54. https://doi.org/10.1037/0278-6133.27.4.445.
Abbey A, Saenz C, Buck PO, Parkhill MR, Hayman LW. The effects of acute alcohol consumption, cognitive reserve, partner risk, and gender on sexual decision making. J Stud Alcohol. 2006;67:113–21. https://doi.org/10.15288/jsa.2006.67.113.
Tahaney KD, Palfai TP, Luehring-Jones P, Maisto SA, Simons JS. Working memory moderates the association between condom use intentions and behavior among moderate-to-heavy drinking men who have sex with men. J Behav Med. 2019;43:666–71. https://doi.org/10.1007/s10865-019-00090-9.
Justus AN, Finn PR, Steinmetz JE. The influence of traits of disinhibition on the association between alcohol use and risky sexual behavior. Alcohol Clin Exp Res. 2000;24:1028–35. https://doi.org/10.1111/j.1530-0277.2000.tb04646.x.
Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual sensation seeking: Scale development and predicting AIDS-risk behavior among homosexually active men. J Pers Assess. 1994;62:385–97. https://doi.org/10.1207/s15327752jpa6203_1.
Kalichman SC, Heckman T, Kelly JA. Sensation seeking as an explanation for the association between substance use and HIV-related risky sexual behavior. Arch Sex Behav. 1996;25:141–54. https://doi.org/10.1007/BF02437933.
Townshend JM, Kambouropoulos N, Griffin A, Hunt FJ, Milani RM. Binge drinking, reflection impulsivity, and unplanned sexual behavior: impaired decision-making in young social drinkers. Alcohol Clin Exp Res. 2014;38:1143–50. https://doi.org/10.1111/acer.12333.
Maisto SA, Palfai T, Vanable PA, Heath J, Woolf-King SE. The effects of alcohol and sexual arousal on determinants of sexual risk in men who have sex with men. Arch Sex Behav. 2012;41:971–86. https://doi.org/10.1007/s10508-011-9846-x.
Wray TB, Celio MA, Pérez AE, DiGuiseppi GT, Carr DJ, Woods LA, et al. Causal effects of alcohol intoxication on sexual risk intentions and condom negotiation skills among high-risk men who have sex with men (MSM). AIDS Behav. 2019;23:161–74. https://doi.org/10.1007/s10461-018-2243-x.
Brown JL, Gause NK, Northern N. The association between alcohol and sexual risk behaviors among college students: a review. Curr Addict Rep. 2016;3:349–55. https://doi.org/10.1007/s40429-016-0125-8.
Palfai TP, Luehring-Jones P. How alcohol influences mechanisms of sexual risk behavior change: contributions of alcohol challenge research to the development of HIV prevention interventions. AIDS Behav. 2021;25(Suppl 3):314–32. https://doi.org/10.1007/s10461-021-03346-1.
Davis KC. The influence of alcohol expectancies and intoxication on men’s aggressive unprotected sexual intentions. Exp Clin Psychopharmacol. 2010;18:418–28. https://doi.org/10.1037/a0020510.
Hendershot CS, Stoner SA, George WH, Norris J. Alcohol use, expectancies, and sexual sensation seeking as correlates of HIV risk behavior in heterosexual young adults. Psychol Addict Behav. 2007;21:365–72. https://doi.org/10.1037/0893-164X.21.3.365.
Newcomb ME, Clerkin EM, Mustanski B. Sensation seeking moderates the effects of alcohol and drug use prior to sex on sexual risk in young men who have sex with men. AIDS Behav. 2011;15:565–75. https://doi.org/10.1007/s10461-010-9832-7.
George WH, Davis KC, Masters NT, Jacques-Tiura AJ, Heiman JR, Norris J, et al. Sexual victimization, alcohol intoxication, sexual-emotional responding, and sexual risk in heavy episodic drinking women. Arch Sex Behav. 2014;43:645–58. https://doi.org/10.1007/s10508-013-0143-8.
George WH, Davis KC, Masters NT, Kajumulo KF, Stappenbeck CA, Norris J, et al. Partner pressure, victimization history, and alcohol: women’s condom-decision abdication mediated by mood and anticipated negative partner reaction. AIDS Behav. 2016;20:134–46. https://doi.org/10.1007/s10461-015-1154-3.
Gilmore AK, Schacht RL, George WH, Otto JM, Davis KC, Heiman JR, et al. Assessing women’s sexual arousal in the context of sexual assault history and acute alcohol intoxication. J Sex Med. 2010;7:2112–9. https://doi.org/10.1111/j.1743-6109.2010.01786.x.
Masters NT, George WH, Davis KC, Norris J, Heiman JR, Jacques-Tiura AJ, et al. Women’s unprotected sex intentions: roles of sexual victimization, intoxication, and partner perception. J Sex Res. 2014;51:586–98. https://doi.org/10.1080/00224499.2012.763086.
Schacht RL, George WH, Heiman JR, Davis KC, Norris J, Stoner SA, et al. Effects of alcohol intoxication and instructional set on women’s sexual arousal vary based on sexual abuse history. Arch Sex Behav. 2007;36:655–65. https://doi.org/10.1007/s10508-006-9147-y.
Schacht RL, George WH, Davis KC, Heiman JR, Norris J, Stoner SA, et al. Sexual abuse history, alcohol intoxication, and women’s sexual risk behavior. Arch Sex Behav. 2010;39:898–906. https://doi.org/10.1007/s10508-009-9544-0.
Staples JM, George WH, Stappenbeck CA, Davis KC, Norris J, Heiman JR. Alcohol myopia and sexual abdication among women: examining the moderating effect of child sexual abuse. Addict Behav. 2015;41:72–7. https://doi.org/10.1016/j.addbeh.2014.09.014.
Simons JS, Simons RM, Maisto SA, Hahn AM, Walters KJ. Daily associations between alcohol and sexual behavior in young adults. Exp Clin Psychopharmacol. 2018;26:36–48. https://doi.org/10.1037/pha0000163.
Maisto SA, Simons JS, Palfai TP, Moskal D, Luehring-Jones P. Daily associations among alcohol intoxication, partner familiarity, participant effortful control, urgency, and PrEP uptake on sexual behavior in men who have sex with men. Arch Sex Behav. 2021;50:2843–60. https://doi.org/10.1007/s10508-020-01852-2.
Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annu Rev Sex Res. 2000;11:125–57. https://doi.org/10.1080/10532528.2000.10559786.
Freeman RC. Toward development of enhanced preventive interventions for HIV sexual risk among alcohol-using populations: confronting the ‘mere pause from thinking’. AIDS Behav. 2016;20:1–18. https://doi.org/10.1007/s10461-015-1179-7.
Wray TB, Kahler CW, Monti PM. Using ecological momentary assessment (EMA) to study sex events among very high-risk men who have sex with men (MSM). AIDS Behav. 2016;20:2231–42. https://doi.org/10.1007/s10461-015-1272-y.
Cooper ML. Toward a person × situation model of sexual risk-taking behaviors: Illuminating the conditional effects of traits across sexual situations and relationship contexts. J Pers Soc Psychol. 2010;98:319–41. https://doi.org/10.1037/a0017785.
Gause NK, Brown JL, Welge J, Northern N. Meta-analyses of HIV prevention interventions targeting improved partner communication: effects on partner communication and condom use frequency outcomes. J Behav Med. 2018;41:423–40. https://doi.org/10.1007/s10865-018-9916-9.
Noar SM, Carlyle K, Cole C. Why communication is crucial: Meta-analysis of the relationship between safer sexual communication and condom use. J Health Commun. 2006;11:365–90. https://doi.org/10.1080/10810730600671862.
Schroder KEE, Johnson CJ, Wiebe JS. An event-level analysis of condom use as a function of mood, alcohol use, and safer sex negotiations. Arch Sex Behav. 2009;38:283–9. https://doi.org/10.1007/s10508-007-9278-9.
Crosby R, Skakoon-Sparling S, Milhausen RR, Sanders S, Graham CA, Yarber WL. The protective value of discussing condom use: a study of young black men attending STI clinics in the southern United States. Health Educ Behav. 2018;45:706–13. https://doi.org/10.1177/1090198118775496.
Widman L, Golin CE, Noar SM. When do condom use intentions lead to actions? Examining the role of sexual communication on safer sexual behavior among people living with HIV. J Health Psychol. 2013;18:507–17. https://doi.org/10.1177/1359105312446769.
Skakoon-Sparling S, Cramer KM. Are we blinded by desire? Relationship motivation and sexual risk-taking intentions during condom negotiation. J Sex Res. 2020;57:545–58. https://doi.org/10.1080/00224499.2019.1579888.
Pines HA, Gorbach PM, Weiss RE, Reback CJ, Landovitz RJ, Mutchler MG, et al. Individual-level, partnership-level, and sexual event-level predictors of condom use during receptive anal intercourse among HIV-negative men who have sex with men in Los Angeles. AIDS Behav. 2016;20:1315–26. https://doi.org/10.1007/s10461-015-1218-4.
Wray TB, Monti PM. Characteristics of sex events, partners, and motivations and their associations with HIV-risk behavior in a daily diary study of high-risk men who have sex with men (MSM). AIDS Behav. 2020;24:1851–64. https://doi.org/10.1007/s10461-019-02760-w.
Bauermeister JA, Carballo-Diéguez A, Ventuneac A, Dolezal C. Assessing motivations to engage in intentional condomless anal intercourse in HIV risk contexts (bareback sex) among men who have sex with men. AIDS Educ Prev. 2009;21:156–68. https://doi.org/10.1521/aeap.2009.21.2.156.
Carballo-Diéguez A, Ventuneac A, Dowsett GW, Balan I, Bauermeister J, Remien RH, et al. Sexual pleasure and intimacy among men who engage in bareback sex. AIDS Behav. 2011;15:57–65. https://doi.org/10.1007/s10461-011-9900-7.
Stephenson R, Freeland R, Finneran C. Intimate partner violence and condom negotiation efficacy among gay and bisexual men in Atlanta. Sex Health. 2016;13:366. https://doi.org/10.1071/SH15212.
Brady SS, Iantaffi A, Galos DL, Rosser BRS. Open, closed, or in between: relationship configuration and condom use among men who use the internet to seek sex with men. AIDS Behav. 2013;17:1499–514. https://doi.org/10.1007/s10461-012-0316-9.
Buckheit KA, Mitzel LD, Maisto SA, Palfai T, Vanable P. Moderated mediation of perceived intoxication and sexual arousal on determinants of sexual risk behavior in men who have sex with men. AIDS Behav. 2019;23:1460–70. https://doi.org/10.1007/s10461-018-2343-7.
Vanable PA, McKirnan DJ, Buchbinder SP, Bartholow BN, Douglas JM, Judson FN, et al. Alcohol use and high-risk sexual behavior among men who have sex with men: the effects of consumption level and partner type. Health Psychol. 2004;23:525–32. https://doi.org/10.1037/0278-6133.23.5.525.
Ariely D, Loewenstein G. The heat of the moment: the effect of sexual arousal on sexual decision making. J Behav Decis Mak. 2006;19:87–98. https://doi.org/10.1002/bdm.501.
Davis KC, George WH, Norris J, Schacht RL, Stoner SA, Hendershot CS, et al. Effects of alcohol and blood alcohol concentration limb on sexual risk-taking intentions. J Stud Alcohol Drug. 2009;70:499–507. https://doi.org/10.15288/jsad.2009.70.499.
Ebel-Lam AP, MacDonald TK, Zanna MP, Fong G. An experimental investigation of the interactive effects of alcohol and sexual arousal on intentions to have unprotected sex. Basic Appl Soc Psychol. 2009;31:226–33. https://doi.org/10.1080/01973530903058383.
MacDonald TK, Zanna MP, Fong GT. Why common sense goes out the window: Effects of alcohol on intentions to use condoms. Pers Soc Psychol Bull. 1996;22:763–75. https://doi.org/10.1177/0146167296228001.
Scott-Sheldon LAJ, Huedo-Medina TB, Warren MR, Johnson BT, Carey MP. Efficacy of behavioral interventions to increase condom use and reduce sexually transmitted infections: a meta-analysis, 1991 to 2010. J Acquir Immune Defic Syndr. 2011;58:489–98. https://doi.org/10.1097/QAI.0b013e31823554d7.
Boyer CB, Greenberg L, Korelitz J, Harper GW, Stewart-Campbell R, Straub D, et al. Sexual partner characteristics, relationship type, and HIV risk among a community venue–based sample of urban adolescent and young adult men who have sex with men. Youth Soc. 2019;51:219–46. https://doi.org/10.1177/0044118X16669259.
Storholm ED, Volk JE, Marcus JL, Silverberg MJ, Satre DD. Risk perception, sexual behaviors, and PrEP adherence among substance-using men who have sex with men: a qualitative study. Prev Sci. 2017;18:737–47. https://doi.org/10.1007/s11121-017-0799-8.
Martinez JE, Jonas KJ. Pre-exposure prophylaxis sorting among men who have sex with men. AIDS Care. 2019;31:388–96. https://doi.org/10.1080/09540121.2018.1533229.
Brown JL, Vanable PA. Alcohol use, partner type, and risky sexual behavior among college students: findings from an event-level study. Addict Behav. 2007;32:2940–52. https://doi.org/10.1016/j.addbeh.2007.06.011.
Kiene SM, Barta WD, Tennen H, Armeli S. Alcohol, helping young adults to have unprotected sex with casual partners: findings from a daily diary study of alcohol use and sexual behavior. J Adolesc Health. 2009;44:73–80. https://doi.org/10.1016/j.jadohealth.2008.05.008.
LaBrie J, Earleywine M, Schiffman J, Pedersen E, Marriot C. Effects of alcohol, expectancies, and partner type on condom use in college males: event-level analyses. J Sex Res. 2005;42:259–66. https://doi.org/10.1080/00224490509552280.
Scott-Sheldon LAJ, Carey MP, Carey KB. Alcohol and risky sexual behavior among heavy drinking college students. AIDS Behav. 2010;14:845–53. https://doi.org/10.1007/s10461-008-9426-9.
George WH, Davis KC, Norris J, Heiman JR, Stoner SA, Schacht RL, et al. Indirect effects of acute alcohol intoxication on sexual risk-taking: the roles of subjective and physiological sexual arousal. Arch Sex Behav. 2009;38:498–513. https://doi.org/10.1007/s10508-008-9346-9.
MacDonald TK, MacDonald G, Zanna MP, Fong G. Alcohol, sexual arousal, and intentions to use condoms in young men: applying alcohol myopia theory to risky sexual behavior. Health Psychol. 2000;19:290–8. https://doi.org/10.1037/0278-6133.19.3.290.
Norris J, Stoner SA, Hessler DM, Zawacki T, Davis KC, George WH, et al. Influences of sexual sensation seeking, alcohol consumption, and sexual arousal on women’s behavioral intentions related to having unprotected sex. Psychol Addict Behav. 2009;23:14–22. https://doi.org/10.1037/a0013998.
Wray TB, Simons JS, Maisto SA. Effects of alcohol intoxication and autonomic arousal on delay discounting and risky sex in young adult heterosexual men. Addict Behav. 2015;42:9–13. https://doi.org/10.1016/j.addbeh.2014.10.037.
Maisto SA, Simons JS, Palfai TP, Moskal D, Sheinfil AZ, Tahaney KD. Effects of alcohol intoxication on sexual decision-making among men who have sex with men: Alcohol’s influences on self-control processes. Clin Psychol Sci. 2023;11:40–58. https://doi.org/10.1177/21677026221079780.
George WH. Alcohol and sexual health behavior: what we know and how we know it. J Sex Res. 2019;56:409–24. https://doi.org/10.1080/00224499.2019.1588213.
Maisto SA, Simons JS. Research on the effects of alcohol and sexual arousal on sexual risk in men who have sex with men: implications for HIV prevention interventions. AIDS Behav. 2016;20:158–72. https://doi.org/10.1007/s10461-015-1220-x.
Bolger N, Laurenceau J-P. Intensive longitudinal methods: an introduction to diary and experience sampling research. New York, NY: Guilford Press; 2013.
Little TD. Longitudinal structural equation modeling. New York: The Guilford Press; 2013.
Simons JS, Maisto SA, Palfai TP. Using the experience sampling method to study sexual risk behavior among men who have sex with men (MSM). J Sex Res. 2019;56:1147–54. https://doi.org/10.1080/00224499.2019.1663479.
Chavez K, Palfai TP. Feasibility of a mobile messaging-enhanced brief intervention for high risk heavy drinking MSM: a pre-pilot study. Alcohol Treat Q. 2020;38:87–105. https://doi.org/10.1080/07347324.2019.1653240.
Podsakoff NP, Spoelma TM, Chawla N, Gabriel AS. What predicts within-person variance in applied psychology constructs? An empirical examination. J Appl Psychol. 2019;104:727–54. https://doi.org/10.1037/apl0000374.
Calahan D, Cisin IH, Crossley HM. American drinking practices: a national study of drinking behavior and attitudes. Monogr Rutgers Cent Alcohol Stud. 1969;6:260.
Kinsey AC, Pomeroy WB, Martin CE, Gebhard P. Sexual behavior in the human male. Philadelphia, PA: W.B. Saunders Company; 1948.
Woolf-King SE, Maisto SA. The effects of alcohol, relationship power, and partner type on perceived difficulty implementing condom use among african american adults: an experimental study. Arch Sex Behav. 2015;44:571–81. https://doi.org/10.1007/s10508-014-0362-7.
Tabachnick BG, Fidell LS. Using multivariate statistics. 3rd ed. New York, NY: HarperCollins College Publishers; 1996.
Geldhof GJ, Preacher KJ, Zyphur MJ. Reliability estimation in a multilevel confirmatory factor analysis framework. Psychol Methods. 2014;19:72–91. https://doi.org/10.1037/a0032138.
Muthén B, Muthén L. Mplus statistical modeling software: release 8.5. Los Angeles, CA: Authors; 2021.
Hoffman L. On the interpretation of parameters in multivariate multilevel models across different combinations of model specification and estimation. Adv Methods Pract Psychol Sci. 2019;2:288–311. https://doi.org/10.1177/2515245919842770.
Finch WH, Bolin JE. Multilevel modeling using Mplus. Boca Raton, FL: CRC Press; 2017.
Burnham KP, Anderson DR. Multimodel inference: understanding AIC and BIC in model selection. Sociol Methods Res. 2004;33:261–304. https://doi.org/10.1177/0049124104268644.
Scott-Sheldon LAJ, Carey KB, Cunningham K, Johnson BT, Carey MP, The MASH Research Team. Alcohol use predicts sexual decision-making: a systematic review and meta-analysis of the experimental literature. AIDS Behav. 2016;20:19–39. https://doi.org/10.1007/s10461-015-1108-9.
Gordon CM, Carey MP, Carey KB. Effects of a drinking event on behavioral skills and condom attitudes in men: implications for HIV risk from a controlled experiment. Health Psychol. 1997;16:490–5. https://doi.org/10.1037/0278-6133.16.5.490.
Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–74. https://doi.org/10.1037/0033-2909.111.3.455.
Fromme K, Katz E, D’Amico E. Effects of alcohol intoxication on the perceived consequences of risk taking. Exp Clin Psychopharmacol. 1997;5:14–23. https://doi.org/10.1037/1064-1297.5.1.14.
Fromme K, D’Amico EJ, Katz EC. Intoxicated sexual risk taking: an expectancy or cognitive impairment explanation? J Study Alcohol. 1999;60:54–63. https://doi.org/10.15288/jsa.1999.60.54.
Stoner SA, Norris J, George WH, Morrison DM, Zawacki T, Davis KC, et al. Women’s condom use assertiveness and sexual risk-taking: Effects of alcohol intoxication and adult victimization. Addict Behav. 2008;33:1167–76. https://doi.org/10.1016/j.addbeh.2008.04.017.
Jacques-Tiura AJ, Norris J, Kiekel PA, Davis KC, Zawacki T, Morrison DM, et al. Influences of acute alcohol consumption, sexual precedence, and relationship motivation on women’s relationship and sex appraisals and unprotected sex intentions. J Soc Pers Relatsh. 2015;32:197–221. https://doi.org/10.1177/0265407514528101.
Purdie MP, Norris J, Davis KC, Zawacki T, Morrison DM, George WH, et al. The effects of acute alcohol intoxication, partner risk level, and general intention to have unprotected sex on women’s sexual decision making with a new partner. Exp Clin Psychopharmacol. 2011;19:378–88. https://doi.org/10.1037/a0024792.
Norris J, Masters NT, Zawacki TM. Cognitive mediation of women’s sexual decision making: the influence of alcohol, contextual factors, and background variables. Annu Rev Sex Res. 2004;15:258–96. https://doi.org/10.1080/10532528.2004.10559821.
Steele CM, Josephs RA. Alcohol myopia: its prized and dangerous effects. Am Psychol. 1990;45:921–33. https://doi.org/10.1037/0003-066X.45.8.921.
Holloway IW, Pulsipher CA, Gibbs J, Barman-Adhikari A, Rice E. Network influences on the sexual risk behaviors of gay, bisexual and other men who have sex with men using geosocial networking applications. AIDS Behav. 2015;19:112–22. https://doi.org/10.1007/s10461-014-0989-3.
Winetrobe H, Rice E, Bauermeister J, Petering R, Holloway IW. Associations of unprotected anal intercourse with Grindr-met partners among Grindr-using young men who have sex with men in Los Angeles. AIDS Care. 2014;26:1303–8. https://doi.org/10.1080/09540121.2014.911811.
Hoenigl M, Little SJ, Grelotti D, Skaathun B, Wagner GA, Weibel N, et al. Grindr users take more risks, but are more open to human immunodeficiency virus (HIV) pre-exposure prophylaxis: could this dating app provide a platform for HIV prevention outreach? Clin Infect Dis. 2020;71:e135–40. https://doi.org/10.1093/cid/ciz1093.
Funding
This study was funded by grant 5R01 AA022301 (MPI: Maisto, Palfai, Simons) from the National Institute on Alcohol Abuse and Alcoholism. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
TPP, JSS, and SAM designed the original study and obtained the funding listed below. DF, PLJ and TPP conceptualized the study described herein. PLJ and JSS performed the data analyses. PLJ drafted the manuscript and all authors contributed to subsequent manuscript revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no competing interests to declare that are relevant to the content of this article.
Ethics Approval
Approval for this study was granted by Institutional Review Boards at Boston University and Syracuse University. The study was performed in accordance with the 1964 Declaration of Helsinki and its later amendments.
Consent
All research participants provided informed consent prior to enrollment in this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luehring-Jones, P., Fulford, D., Palfai, T.P. et al. Alcohol, Sexual Arousal, and Partner Familiarity as Predictors of Condom Negotiation: An Experience Sampling Study. AIDS Behav 28, 854–867 (2024). https://doi.org/10.1007/s10461-023-04189-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-023-04189-8