Abstract
Alcohol use is a key risk factor for HIV infection among MSM, in part because intoxication may interfere with the use of prevention methods like condoms. However, few studies have examined whether this is due to alcohol’s pharmacological or expectancy effects or explored the specific aspects of sexual decision-making that may be affected. In this study, high-risk, heavy drinking MSM (N = 121) were randomly assigned to receive either (1) alcohol beverages, (2) placebo beverages, or (3) control beverages, before navigating a video-based sexual risk scenario that assessed several aspects of sexual decision-making. Results showed that condom use intentions and negotiation behaviors were lower among alcohol and placebo participants compared with controls, but that few significant differences emerged between the alcohol and placebo groups. These findings contrast with similar past studies, and suggest that alcohol’s expectancy effects may play a role in sexual decision-making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, rates of new HIV infections in the United States (US) have declined overall, but incidence remains high specifically among men who have sex with men (MSM; [1, 2]). In 2015, MSM continued to account for the largest percentage of new infections, at 67% [2]. Recent estimates from the US Centers for Disease Control and Prevention suggest that, if this trend continues, 1 in 6 MSM will be diagnosed with HIV in their lifetime [3]. The bulk of these new infections are a direct result of sexual risk behavior, specifically having insertive or receptive anal sex without using some form of prevention [1, 4]. For this reason, behavioral approaches to prevention, including interventions designed to increase the use of protection during sex, continue to be a key strategy for curbing new infections [5]. While other emerging advances in biomedical prevention, such as pre-exposure prophylaxis (PrEP) and microbicides, hold considerable promise for helping to increase the use of protection and may be more acceptable to many MSM [6,7,8], condoms continue to be the most widely accessible and most frequently used form of protection from HIV across the globe [9]. Moreover, condoms are the only effective form of protection against many other sexually-transmitted infections [10], which contribute to the global burden of disease [11, 12]. Together, these factors highlight the need for continued research aimed at improving our understanding of factors involved in the failure to use condoms, particularly among at-risk populations like MSM.
Alcohol use is a key risk factor for HIV infection among MSM [13,14,15], and recent research suggests that this may be due in large part to its tendency to interfere with the use of prevention methods like condoms [16, 17]. Cross-sectional studies have shown that heavier patterns of alcohol use are related to less frequent condom use during sex, both among MSM [18] and heterosexual men and women [19, 20]. A meta-analysis of event-level studies also showed that binge drinking (5+ drinks on a single occasion) prior to or during a sex event was one of only two drugs that were associated with an increased odds of engaging in condomless anal sex (CAS), although more moderate alcohol use was not associated with risk behavior [21]. Further, daily recall studies have also shown that the odds of CAS with serodiscordant partners were 4–6 times higher on days marked by very heavy drinking (12+ drinks; [22]). Although studies like these provide strong support for alcohol’s influence on HIV-risk behavior, their reliance on retrospective recall methods limits their ability to establish the temporal precedence of alcohol use relative to sex, and therefore cannot definitively confirm alcohol’s causal role in this association. Moreover, these studies cannot distinguish between alcohol’s pharmacological effects on sexual behavior and its expectancy effects. Alcohol’s sex-related expectancy effects have been well-documented, and involve beliefs about the effects that alcohol will have on sexual behavior and feelings [23, 24]. Expectancy theory suggests that those who have strong beliefs that consuming alcohol will lead them to become less inhibited and more likely to do something sexually risky may be more likely to engage in risk behavior after drinking because of these beliefs, independent of alcohol’s true drug effects [25]. Disentangling alcohol’s pharmacological effects from its expectancy effects has critical implications for interventions which aim to reduce alcohol’s influence on HIV-risk behavior, since strong expectancy effects could suggest this influence might be attenuated by challenging these expectancies [26, 27], while true drug effects might suggest that interventions should focus on reducing alcohol use.
Randomized, placebo-controlled experimental studies are well-equipped to evaluate the potential causal role of alcohol intoxication on HIV-risk behavior, and can help distinguish between its pharmacological and expectancy effects. In such studies, alcohol-experienced participants are typically randomly assigned to receive either alcoholic beverages, placebo beverages intended to mimic the experience of consuming alcohol without producing pharmacological effects, or control (non-alcoholic) beverages. In each condition, participants are often then asked to navigate a hypothetical sexual scenario that uses a written story, audio clip, or video to depict a scene that sets the context for assessing participants’ decisions about sex and prevention that they might make in a similar situation in the “real world” [28]. Although this approach does not afford the direct assessment of sexual risk behavior itself, it enables researchers to assess several different facets of decision-making and antecedents of risk behavior, such as participants’ intentions to use condoms, their ability to negotiate their use with a partner, and their perceptions of the risks and benefits of each option [28, 29]. Understanding the unique and common effects of alcohol and alcohol-related expectancies on each of these specific processes could similarly help improve interventions for alcohol-involved risk by incorporating content that targets the specific elements of decision-making that are affected. A large body of randomized controlled studies have been conducted among heterosexual men and women, and a meta-analysis of these studies has shown that consuming alcohol increased participants’ self-reported intentions to engage in condomless sex and impaired objectively-assessed condom negotiation behaviors when compared to both placebo and non-alcohol control conditions [29]. However, only one of the 30 included studies focused exclusively on MSM [30], a critical limitation since the consequences of sexual risk behavior may be more severe among these men due to higher population-level prevalence of HIV in MSM [31]. We are aware of just two published studies that have used randomized, placebo-controlled designs to explore the effects of acute alcohol consumption on sexual decision-making among MSM, and these studies report somewhat inconsistent results. In a study of 283 HIV-negative and HIV-positive MSM, those who consumed alcohol reported higher intentions to engage in CAS after viewing a video-based hypothetical sexual scenario, compared with non-alcohol control and placebo condition participants, and CAS intentions did not differ across the placebo and control groups [32]. However, no other outcomes relevant to sexual decision-making were reported. In a study of 117 HIV-negative MSM, CAS intentions assessed after a similar scenario did not significantly differ across those who drank alcohol versus a combined placebo and no-alcohol control condition, but ratings of participants’ condom negotiation behaviors were lower among those in the alcohol condition compared with the placebo/control group [30]. No differences were observed in participants’ perceptions of the risk involved in CAS across the beverage conditions. Together, these studies provide conflicting findings about alcohol’s influence on CAS intentions in MSM, and only one reported on alcohol’s effects on other aspects of decision-making, highlighting the need for more randomized, placebo-controlled studies that examine alcohol’s effects across many facets of sexual decision-making (e.g., intentions, condom negotiation skills, risk/benefit perceptions).
In this study, we explored the pharmacological and expectancy effects of alcohol on CAS intentions, risk/benefit perceptions of CAS, and condom negotiation skills in a randomized, placebo-controlled study in which high-risk, heavy drinking MSM in the northeastern US were assigned to receive either alcohol [target breath alcohol content (BrAC) = 0.08], placebo, or control beverages and asked to navigate a video-based sexual risk scenario that has been used in past studies [28, 30]. This scenario was used to provide context for objectively assessing how participants would respond if a similar partner insisted on condomless sex, their intentions for engaging in CAS, and their perceptions of the risks/benefits involved in having CAS with a similar partner. We selected this target BrAC, because it reflects the National Institute on Alcohol Abuse and Alcoholism’s definition of “binge drinking” [33] and is the most common target BrAC used in similar past studies of sexual decision-making among heterosexual men and women [29]. We expected that those who consumed alcohol would report higher CAS intentions, have poorer condom negotiation skills, and have lower risk perceptions/higher benefit perceptions of CAS, compared to both the control and placebo beverage groups.
Methods
Participants
High-risk MSM (N = 121) were recruited from gay-oriented smartphone dating apps (e.g., Grindr, Scruff), social networking sites (e.g., Facebook, Instagram), and via in-person outreach (e.g., flyers, business cards) in the Providence, RI and Boston, MA areas from May 2014 to November 2017. Eligible participants were (1) aged 21–50, (2) assigned male sex at birth, (3) able to speak and read English, (4) reported having had CAS with a casual male partner within the past year, (5) not currently in a sexually exclusive relationship with a single partner of longer than 3 months, and (6) classified as “hazardous drinkers” according to NIAAA criteria, which involves consuming (a) an average of 14+ drinks per week or (b) 5 or more drinks on a single occasion at least once in the past month. Participants were excluded if they (1) were HIV-positive, (2) had engaged in any injection drug use in the past 3 months, (3) reported significant current drug-related problems (defined as a score of > 4 of the Short Drug Abuse Screening Test [34]), (4) reported currently receiving medications or psychotherapy for alcohol/drug-related problems, (5) reported significant current alcohol-related problems (defined as a score of > 2 on the dependence symptoms subscale of the Alcohol Use Disorders Identification Test [35, 36], (6) had a history of complex alcohol withdrawal or (7) abnormal liver enzyme tests, (8) reported medical problems or medications for which alcohol use is contraindicated, or (9) had a history of severe mental illness. Those who reported (10) currently taking pre-exposure prophylaxis (PrEP) to prevent HIV infection were also excluded, since the study’s primary outcomes focused on condom use.
Measures
Screening and Baseline Measures
Alcohol Use Disorders Identification Test (AUDIT; [36])
The AUDIT is a 10-item measure that was used to assess alcohol-related problems in the past 12 months for screening purposes. The AUDIT is one of the most commonly used screening instruments for alcohol use disorders and has excellent reliability and validity [37, 38]. Those who scored > 2 on the dependence symptoms subscale were excluded from participation (35).
Short Drug Abuse Screening Test (DAST-10; [34])
The DAST-10 is a 10-item measure used to assess risk of current drug-related problems. The DAST-10 has excellent reliability and validity [39], and those who scored > 4 were excluded from participation.
Timeline Followback (TLFB; [40, 41])
Participants completed an online TLFB of their sexual behavior for 30 days prior to enrollment. In this task, participants are presented with a calendar of the past 30 days and asked to identify days on which they had oral, anal, or vaginal sex. After identifying all days, they indicate the number of sex partners they had on each day (up to 4), as well as each partner’s gender, whether they were a new partner, were a casual or committed partner, whether they asked about each partner’s HIV status or the last time they tested, and if so, what their status was. They are then asked to report which sex acts they engaged in with each partner (oral, insertive anal, receptive anal, vaginal sex) and whether they used a condom for each act. Past research provides strong evidence that online TLFBs are reliable and valid for assessing alcohol use, drug use, and sexual behavior [42,43,44,45]. Responses from the TLFB were used to explore the validity of participants’ ratings during the sexual risk scenario.
Sexual Behavior Survey (SBS; [46])
The SBS was used to assess participants’ lifetime and past-year sexual behavior and condom use, but was modified to fit MSM. As such, this version assessed the number of oral and anal/vaginal sex partners participants had of each gender over each of these time frames, as well as a general rating of the frequency of condom use during insertive and receptive anal and vaginal sex events over the past year (ranging from [1] never to [5] always). SBS items were used to examine whether there were risk-related differences between the experimental groups, as well as the validity of participants’ sexual risk scenario ratings.
UCLA Multidimensional Condom Attitudes Scale (MCAS; [47])
The MCAS is a 25-item measure of participants’ attitudes toward condoms. Each item is rated on a 1 (strongly disagree) to 7 (strongly agree) scale. Although the MCAS assesses five subscales, only two were used for the current study: The “Embarrassment about Negotiation and Use” subscale was used to explore the validity of the study’s key outcome measures, and the “Pleasure” subscale was used as a covariate when modeling the study’s primary outcomes to control for the influence of those with especially strong attitudes toward condoms. Reliabilities for these subscales in this sample were α = 0.84 and α = 0.71, respectively.
Sex-Related Alcohol Expectancies (SAEs; [48])
Leigh’s 13-item measure of SAEs was used to assess participants’ beliefs about how alcohol will affect their sexual responses, feelings, and behaviors. Example items include “After drinking alcohol … I am more likely to enjoy sex more,” and each item is rated on a 1 (not at all) to 4 (very much) scale. The reliability of this scale was α = 0.91 in this sample.
Marlowe–Crowne Social Desirability Scale—Form A (SDS; [49, 50])
The SDS is an 11-item scale that assesses participants’ tendency to present themselves favorably to others. Each item (e.g., “I am sometimes irritated by people who ask favors of me”) is rated yes/no, with higher total scores representing a greater tendency to present oneself favorably. This score was used as a covariate in primary outcome models to control for overly favorable responses.
Manipulation Check Measures
Breath alcohol concentration (BrAC)
BrAC was collected every 15 min during the experimental session using an Alco-Sensor FST® (Intoximeters, St. Louis, MO).
Perceptions of Amount of Alcohol Consumed and Intoxication
Single items assessed participants’ perceptions of the amount of alcohol they believed they consumed during the study procedure (number of “standard drinks” from 0 to 15) and their level of intoxication (rated from 1 [not at all] to 10 [more intoxicated than you’ve ever been]). These items were collected every 15 min during the experimental session.
Subjective Sexual Arousal
Sexual arousal was assessed using a single item, rated on a 9-point scale (1 [not at all] to 9 [extremely]), similar to past studies [30, 51]. Participants responded to this item before and after viewing an erotic sexual priming film clip that was intended to induce sexual arousal, as well as before and after viewing the sexual scenario film clips.
Primary Outcome Measures
Sexual Risk Scenario
A film segment, developed by Woolf-King et al. [28] and employed in Maisto et al. [30], was used to provide context for measures of sexual decision-making. The clip depicts a situation in which two male partners who meet at a party are attempting to make decisions about whether or not to use condoms when having sex for the first time. Participants were asked to assume the role of one of the characters (“Dave”) and respond as they would if they were in a similar situation. As the scenario unfolds, the other character (“Jim”) expresses his desire to have sex without a condom, and attempts to persuade Dave to do so with several escalating comments. Participants were prompted to respond to these comments twice during the scenario, speaking into a microphone connected to the computer that recorded their responses. The first of these prompts (Prompt #1) comes after the participant’s character first suggests using a condom and “Jim” expresses his desire to have sex without one (saying, “You don’t need that. I’m safe. You know you can trust me.”). The prompt (Prompt #2) comes after “Jim” again suggests that the participant’s character put the condom away, offering further reasons to forego condom use (e.g., “You know it feels much better without that. […] You know I’m clean. […] Don’t you trust me?”). After the scenario was complete, participants were then asked to rate survey items assessing condom use intentions, risk perceptions, arousal, and whether the situation depicted was realistic/attractive. Although the scenario itself did not involve explicitly erotic content, it was intended to be arousing and depicted sexual/romantic behaviors (e.g., kissing, touching, “dirty talk”). Together, this sequence produced the following key outcome measures:
CAS Intentions
Four items assessed participants’ intentions to engage in insertive and/or receptive anal sex with and without a condom if they were in a situation that was similar to the one depicted in the scenario. Response options ranged from 1 (strongly disagree) to 9 (strongly agree). Participants’ ratings were reversed, summed, and standardized into a single score, so that higher values reflected stronger CAS intentions for use in outcome analyses.
Perceptions of the Risks and Benefits of CAS
Four items adapted from the Cognitive Appraisal of Risky Events (CARE) scale [52] were used to assess participants’ perceptions of the likelihood and severity of negative consequences (e.g., getting “sick, … embarrassed, or feel badly about yourself”) they might experience if they had insertive and/or receptive CAS in a similar situation. Four additional items assessed participants’ perceptions of the likelihood and severity of positive consequences (e.g., “experiencing pleasure or feeling good about yourself”) they might experience if they had insertive and/or receptive CAS in a similar situation. For each perception (CARE-negative, CARE-positive), the four items were summed and standardized to form a score prior to modeling.
Condom Negotiation Skill Verbal Ratings [30]
Two recordings (Prompts #1 and #2) of participants’ verbal responses to “Jim” during the role play were reviewed, transcribed, and then rated by independent, trained members of the research staff. Staff rated each response according to whether they included: (1) an “I” statement of intention to use condoms or refusal of condomless sex, (2) a positive statement about the partner, (3) a specific reason for wanting to use condoms, (4) a suggestion of an alternative, safer behavior, and (5) a rating of whether the response was “direct, serious, and clear.” Each dimension was assigned a rating from 0 to 4 (with higher scores suggesting better communication) based on specific criteria included in a rating manual used extensively in past research [53,54,55]. For each prompt, the two ratings for each dimension were summed and standardized to form overall scores for both Prompt #1 and #2. Rating reliabilities are reported in the results section.
Procedures
Interested participants were first required to complete an online screening survey that assessed basic eligibility criteria. Those eligible were then contacted by study staff to arrange an appointment to conduct the experimental session. Participants were required to abstain from alcohol, illicit drugs, and over-the-counter medications for at least 24 h prior to their scheduled sessions, were asked to avoid eating or drinking anything (aside from water) for at least 3 h prior to their session, and were informed that transportation home would be provided after each appointment. Upon presenting for their session, research staff first verified participants’ compliance with the pre-appointment instructions, and then obtained informed consent. Staff then collected participants’ BrAC and conducted a drug screen via urinalysis. Participants with BrACs > 0.000 or with positive screens for drug classes that could present safety problems for alcohol use (e.g., sedatives, opioids, benzodiazepines) were either dismissed or asked to re-schedule and to follow pre-appointment instructions. Participants’ height and weight were then collected to determine an appropriate volume of alcohol and/or control beverage to administer, before they were randomly assigned to a study condition using a random number generator.
Participants in the alcohol condition received beverages consisting of vodka and tonic water in a 1:4 parts ratio, with dashes of lime juice and mint simple syrup, in amounts designed to achieve a target peak BrAC of 0.08% after 40 min. Alcohol dose amounts were calculated using a well-validated algorithm [56]. Placebo participants were explicitly told that they would receive alcoholic beverages intended to achieve a target BrAC of 0.08 and were provided with beverages consisting of tonic water, lime juice, and mint syrup, with a vodka “floater” in glasses with rims soaked in vodka to provide olfactory cues associated with alcohol. Both placebo and alcohol beverages were mixed in full view of participants, though the placebo preparation involved a vodka bottle full of flat tonic water. Control participants received beverages consisting solely of tonic water and were informed of their contents. Beverage volume was consistent across all three conditions. Participants were given 15 min to consume their assigned beverages, which was followed by a 10 min absorption period.
After the absorption period, staff guided participants through completing several behavioral tasks that were administered as part of a broader study. After approximately 30 min, participants began the sexual risk scenario. The scenario first collected ratings of subjective sexual arousal, before showing a 3 min erotic priming film clip designed to induce sexual arousal. Participants again rated their sexual arousal afterward before viewing the scenario itself. Participants were prompted to respond to one of the characters twice during this scenario and were given 30 s to speak into a microphone to do so. After the scenario was complete, participants then provided ratings of CAS intentions and the CARE. Participants were provided with complete privacy during these tasks, and the video sequence paused automatically to allow participants to respond when needed to avoid the need for staff to enter the room or interrupt. After these procedures were completed, participants were debriefed, and if they consumed alcohol, they were encouraged to remain in the lab until their BrAC returned to 0.020. BrAC readings were collected after the absorption period was complete, immediately prior to beginning the scenario (i.e., after the prime clip), immediately after the scenario, and then every 30 min until participants reached the release value of BrAC. All participants were provided with transportation home, and were paid $80 for completing all procedures, plus an additional $10 per hour for alcohol participants who elected to stay until their BrAC had decreased. All procedures were approved by the Brown University Institutional Review Board.
Analysis
Descriptive statistics for demographic characteristics, alcohol use, and sexual behavior were first calculated by study condition to explore whether there were baseline differences between the groups. To explore the face validity of the sexual scenario, descriptive statistics were calculated for participants’ ratings of the scenario’s realism, attractiveness, and their interest in sex with the depicted partners. Next, to explore the reliability of our ratings of participants’ verbal condom negotiation responses, we calculated Cohen’s kappa statistics to examine the agreement between raters for each of the five dimensions within each prompt. We then explored the validity of participants’ ratings of CAS intentions and staff ratings of negotiation skill responses by exploring semipartial correlations between these variables and related items from the TLFB/SBS, removing variance associated with condition assignment. To confirm that the beverage and sexual arousal manipulations had their intended effects, we used ANOVA models to test whether BrAC, perceived number of standard drinks, and ratings of subjective intoxication varied across the experimental conditions, as well as whether ratings of subjective sexual arousal varied before and after the prime and scenario film clips.
Finally, we used linear regression models to test between-group differences in five key outcome variables: CAS intentions, condom negotiation skills (Prompt #1, Prompt #2), and perceptions of the risks (CARE-negative) and benefits (CARE-positive) of engaging in CAS. Effect codes for both beverage conditions (placebo, alcohol) were included in each model to test for differences in each outcome across these conditions. Age, social desirability, and MCAS-pleasure scores were also included in each model to control for their potential influence. Given that some past studies have shown that sexual arousal may potentiate associations between alcohol intoxication and sex risk, we also tested a two-way interaction between arousal and beverage condition in each model. Similarly, to explore whether the effects of manipulated expectancies are particularly pronounced among those with strong SAE beliefs, we also tested a two-way interaction between SAEs and beverage condition in each model. These interactions were tested using a backward elimination strategy, and non-significant interaction terms were dropped prior to estimating the final model for each outcome. All analyses were conducted in Stata 14.
Results
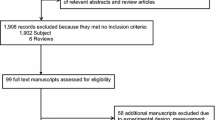
Figure 1 presents the flow of study participants. Two participants who were randomized to a study condition were excluded from further analyses for failing to follow staff instructions and attend to tasks administered during the experimental session, leaving a final sample size of 119. See Table 1 for demographic characteristics. There were no differences in demographic or behavioral characteristics between the beverage conditions at baseline (see Table 2).
Reliability and Validity of Primary Outcome Measures
Overall, participants rated the sexual risk scenario as quite realistic (M = 5.8, SD= 2.5, Mdn = 6), but had modest interest in sex with the depicted partners (M = 4.3, SD= 2.5, Mdn = 4) and were only moderately attracted to them (M = 4.4, SD= 2.5, Mdn = 5). Scale reliability for the CAS intention items was fair (α = 0.72). The convergent validity of these items was similarly fair when they were compared to both the percentage of anal sex events with casual partners that were condomless in the past month (sr = 0.39, p < 0.05), as well as their general rating of condom use frequency during anal sex over the past year (sr = 0.33, p < 0.05). Reliabilities for the five dimensions of participants’ condom negotiation skill ratings ranged from fair to substantial for both Prompt #1 (Cohen’s κ = 0.47–0.69, all p < 0.05) and Prompt #2 (Cohen’s κ = 0.41–0.58, all p < 0.05). However, neither prompt’s ratings were correlated with participants’ scores on the MCAS-negotiation subscale (sr1= 0.09, p >0.05, sr2= 0.02, p > 0.05), although much of this discrepancy could represent the variance in rater and method across these two measures. Finally, reliabilities of both CARE scales were excellent in this sample (α = 0.83 for negative, and α = 0.88 for positive), and previous studies have shown strong support for its validity [52]. Together, these results suggest that the sexual risk scenario was likely realistic and interesting enough to help participants accurately reflect what they might say and do in a similar situation.
Manipulation Checks
Mean peak BrAC was .084 (SD= 0.018, range 0.052–0.112) among participants in the alcohol condition, and .000 in both the placebo and control conditions. Participants’ mean ratings of the perceived number of standard drinks they consumed differed significantly across the study conditions, F(2, 119) = 23.28, MS = 38.42, p < 0.001. Pairwise comparisons showed that, while those in both the alcohol and placebo conditions perceived consuming more drinks than those in the control group (t = 2.18, p < 0.05 and t = 2.47, p < 0.05), these perceptions did not differ across alcohol and placebo participants (t = 0.30, p = 0.720). Marginal means were control: 0.51, placebo: 3.11, alcohol: 3.41. Participants’ mean ratings of subjective intoxication also differed significantly across the study conditions, F(2, 119) = 107.69, MS = 103.4, p < 0.001. Marginal means were, control: 1.16, placebo: 2.27, and alcohol: 4.27. Finally, participants’ subjective sexual arousal ratings also differed significantly over time, such that increases in arousal observed after participants viewed the priming video clip were significantly higher than their baseline reported level, F(3) = 45.85, MS = 91.5, p < 0.001. However, participants’ arousal declined substantially after viewing the actual risk scenario film clips (see Time 3 in Fig. 2), suggesting that an erotic prime film is likely necessary in order to induce a more realistic degree of arousal. Overall, these results suggest that both the beverage and sexual arousal manipulations were successful.
Primary Outcomes
The results of all final regression models are presented in Table 3. In the first model of CAS intentions, hypothesized two-way interactions were not significant and were dropped. In the final model, an overall main effect of beverage condition emerged, F(2) = 4.52, p = 0.013, and planned contrasts suggested that ratings of CAS intentions in both the alcohol (F[1] = 6.35, p = 0.013) and placebo conditions (F[1] = 7.23, p = 0.008) were significantly higher than controls. However, CAS intentions were not significantly different across the placebo and alcohol groups, F(1) = 0.02, p = 0.897 (see Fig. 3, left panel). Negative attitudes about the effects of condoms on sexual pleasure and higher levels of subjective sexual arousal were also generally positively associated with higher CAS intentions.
In models of participants’ condom negotiation skills, none of the hypothesized two-way interactions or main effects were significantly associated with ratings in Prompt #1. Two-way interactions were also not significant in the model for Prompt #2 and thus were dropped from subsequent models. However, a significant main effect of beverage condition emerged in the Prompt #2 model, F(2) = 2.92, p = 0.048. Effect codes suggested that ratings of participants’ condom negotiation skills were significantly lower in the alcohol condition when compared to controls, but ratings among placebo participants were not significantly different than controls. However, planned contrasts showed that negotiation skill ratings were not significantly different across the placebo and alcohol conditions, F(1) = 0.05, p = 0.832 (see Fig. 3, middle panel).
In models of risk perceptions, effect codes suggested that placebo group participants viewed the negative consequences of engaging in CAS as significantly less likely/severe than control participants (see Fig. 3, right panel). However, there was no difference in CARE-negative ratings across the alcohol and control conditions. Planned contrasts also suggested that CARE-negative ratings were not significantly different across the alcohol and placebo groups, F(1) = 2.21, p = 0.140. No other covariates were significantly associated with participants’ CARE-negative ratings. In the model of participants’ perceptions of the likelihood/intensity of positive consequences of engaging in CAS, the two-way interaction between SAEs and beverage condition was not significant and was dropped from subsequent models. However, a significant two-way interaction between sexual arousal and beverage condition emerged, F(2) = 3.57, p = 0.032. Pairwise follow-up contrasts suggested that the form and strength of this slope among alcohol participants was significantly different when compared to control participants (F[1] = 7.10, p = 0.009), but there were no other significant differences between the groups. Specifically, sexual arousal and CARE-positive ratings were positively and more strongly associated among those in the alcohol condition when compared with control participants, who showed a negative, weaker association. Exploring the values of sexual arousal at which these condition slopes were different showed that CARE-positive ratings were higher among both alcohol and placebo participants compared to control specifically at moderate/high levels of sexual arousal (i.e., X > 4–5, or somewhat aroused). However, CARE-positive ratings were significantly lower among alcohol participants compared to placebo participants, specifically at very low levels of sexual arousal (i.e., X < 2, or not at all aroused; see Fig. 4). Negative condom attitudes were also significantly positively associated with CARE-positive ratings, and age was significantly negatively associated. See Table 4 for marginal means for each outcome by beverage condition.
Discussion
In this randomized, placebo-controlled study, we explored whether alcohol intoxication caused changes in sexual decision-making among MSM that could ultimately lead to higher risk of HIV. Our findings suggest that both actual alcohol intoxication and simply believing one had consumed alcohol increased participants’ intentions for having condomless anal sex (CAS) when compared with control group participants. However, our results also showed that CAS intentions were not substantially different among MSM who were actually intoxicated versus those who merely believed they had consumed alcohol. Since those in the alcohol condition both expected to receive alcohol and experienced alcohol’s drug effects and did not show discernable differences from the placebo group for either outcome, this pattern of results suggests that alcohol’s pharmacological effects did not contribute additional increases beyond beverage expectancy effects. As such, these results are most consistent with the interpretation that alcohol’s effects on CAS intentions among MSM are primarily accounted for by alcohol’s expectancy effects. These results contrast starkly with similar past studies conducted both among heterosexual men and women [16, 29] and among MSM [30, 32], since the majority of these studies did not find significant placebo effects on condomless sex intentions. Indeed, a meta-analysis of these studies, the majority of which were conducted among heterosexual men and women, found no differences between placebo and control conditions on condomless sex intentions [29]. Moreover, the two similar previously published placebo-controlled studies that focused on MSM ultimately combined their control and placebo conditions since there were no differences between these two groups on intentions [30, 32]. One possible explanation for our results could be that the placebo manipulations we used in this study might have been more effective than those in previous studies, and thus more effective in producing expectancy effects. However, this seems unlikely, given past studies show differences in perceived intoxication and the amount of alcohol consumed that are of similar magnitude as those reported here [30, 32]. As such, our findings could suggest that alcohol’s expectancy effects on intentions may be stronger among MSM than previously understood. It is surprising, however, that if alcohol’s effects on CAS intentions were primarily due to expectancy effects, CAS intentions were not particularly high specifically among those who expected alcohol and had stronger SAEs. However, the SAE measure we used only assessed participants’ explicit expectations that alcohol affects sexual responding. So, it is possible that expecting to receive alcohol beverages itself may increase CAS intentions even among those who do not openly endorse SAEs because it may activate expectancies that are implicit or that participants are unwilling to acknowledge. However, it is difficult to draw confident conclusions regarding these effects given the limited number of studies available among MSM, and further research is needed.
The influence of beverage condition on participants’ ability to clearly and assertively communicate with a hypothetical partner about condom use differed across each of the two responses that participants provided (Prompt #1 and #2). Specifically, there was no main or group effect of beverage condition on communication skills for Prompt #1, but these skills were significantly lower among participants in the alcohol group relative to controls for Prompt #2. Although communication skills for Prompt #2 were also generally lower among placebo participants than controls and slightly higher than among alcohol participants, they were not significantly different than either group. This pattern of results appears to suggest that alcohol’s combined pharmacological and expectancy effects may impair communication skills relative to those who are sober, and that alcohol’s pharmacological effects may contribute enough to this impairment for these differences to emerge, but that drug effects did not impair these skills significantly more than expectancy effects alone. Further, they suggest that this effect is unique to Prompt #2. One of the key differences between the two prompts is that the partner in the scenario (“Jim”) attempts to persuade the participants’ character more intensely in Prompt #2, so these results could suggest that alcohol’s effects on communication about condom use may be most pronounced when partners are more adamantly resistant to using condoms. That is, intoxicated MSM may be less assertive about using a condom or more likely to coalesce to their partners’ wishes when they are pressured by their partner to not use one. However, the two prompts also differed in terms of time and likely BrAC, so these factors could explain these differences, as well. Overall, these findings also contrast with the only similar study of MSM that examined alcohol’s effects on communication skills and used the same approach [53], which found that, across both prompts, communication skills were impaired specifically among those in the alcohol condition compared with a combined placebo and control group. Still, our findings and this previous study both show that alcohol intoxication can impair the ability of MSM to clearly and effectively communicate their desire to use a condom to a potential sex partner.
The next model showed that placebo group participants viewed the negative consequences of CAS as significantly less likely or severe than control participants, but again, the placebo group was not significantly different than the alcohol group. These results suggest that one pathway whereby alcohol’s expectancy effects could uniquely lead to risk behavior among MSM is the belief that consuming alcohol will lead them to care less about the potentially negative consequences of having sex without a condom. In the final model, sexual arousal moderated the association between beverage condition and participants’ ratings of the likelihood and severity of potential benefits of engaging in CAS. Further investigation showed that this interaction was primarily driven by differences in the slope of the relationship between sexual arousal and perceiving benefits of CAS specifically across the control and alcohol groups. Specifically, those in the alcohol condition generally perceived more benefits of engaging in CAS at increasing levels of sexual arousal, whereas those in the control condition saw fewer benefits of engaging in CAS as their sexual arousal increased. This negative but weak slope among control participants was unexpected, but could suggest that sober MSM are better able to understand and recognize the effects of sexual arousal on both their perceptions and decisions, and thus may be more vigilant about its effects. Slopes among both the alcohol and placebo participants were in the more intuitive, positive direction, but those experiencing both the pharmacological and expectancy effects of alcohol (alcohol group) reported lower perceived benefits of CAS specifically at lower levels of sexual arousal when compared to those who experienced expectancy effects alone. This pattern could suggest that alcohol’s expectancy effects may lead MSM to see more benefits of engaging in CAS when they are not aroused than alcohol’s pharmacological effects do, but that true drug effects potentiate sexual arousal’s effects on positive perceptions as arousal increases. Together, these results suggest that alcohol’s drug and expectancy effects could also lead to increased HIV risk behavior by leading MSM to perceive more benefits of engaging in CAS, but that these effects depend on their level of sexual arousal.
Limitations
Although this study adds critical knowledge to the existing literature on the relationship between alcohol use and HIV-risk behavior among MSM, several limitations are important to note. First, while experimental designs like these allow researchers to understand alcohol’s effects on sexual decision-making in close detail and control the influence of many confounding variables, they cannot study enacted risk behavior and instead must focus on exploring antecedents of risk behavior, like intentions, behavioral skills, and perceptions. As such, the findings reported here may differ from alcohol’s true effects on sexual risk behaviors. However, it is important to note that past studies suggest that intentions are among the strongest predictors of behavior, with correlations ranging from r = 0.42–0.60 [57], and our results on the convergent validity of scenario intention ratings roughly corresponded with participants’ tendency to engage in similar behaviors in the past. Thus, intention measures collected in the context of a realistic hypothetical scenario may provide an acceptable and valid analogue of behavior. Second, and similarly, the video-based scenario we used in this study produced ratings of attractiveness, interest, and arousal that were well below the mid-point of their respective scales. One reason for this may be that the scenario is dated, but another is that video-based approaches to creating the context for assessing sexual decision-making shows partners with circumscribed characteristics. Other approaches, like written vignettes, often allow participants to imagine the characteristics of partners and situations they find most attractive, and so, may be more effective tools for similar future research. Third, while we employed a well-validated alcohol dosing procedure that has been used in a number of past studies, there was still a wide range in the peak BrACs of alcohol condition participants (range 0.052–0.112). As a result, the effect size of alcohol intoxication on the study’s primary outcomes may be imprecise. Future research might incorporate steps to reduce this variability (e.g., idiographically determined absorption periods; [58]). Fourth, this study focused exclusively on MSM and our sample was predominantly white, so its results may not generalize to other populations. Finally, this study also focused exclusively on condom use, since it is currently the most widely accessible and broadly used method of prevention. However, several other effective prevention methods are available, including pre- and post-exposure prophylaxis (PrEP and PEP). Alcohol’s effects on the uptake and use of these prevention methods may be distinct from its effects on condom use, and so the implications of the results reported here apply only to those who rely on condoms as their sole method of prevention.
In summary, the results of this study provide support for several key mechanisms whereby alcohol, whether via its pharmacological or placebo effects, can increase risk for HIV among MSM: (1) by increasing their willingness to engage in anal sex without a condom, (2) impairing their ability or willingness to be assertive when negotiating condom use with a resistant partner, (3) decreasing their perceptions of the potential negative consequences of engaging in sex without a condom, (4) increasing their perceptions of its benefits, or (5) all of these. However, our findings also provide broader support for the role of alcohol’s expectancy effects than similar past studies. Further research is needed to better understand alcohol’s drug and expectancy effects on sexual decision-making among MSM in order to improve the specificity and effectiveness of interventions that aim to reduce HIV risk by addressing alcohol use.
References
Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380:367–77.
Centers for Disease Control and Prevention. Trends in HIV diagnoses, 2005–2014 Atlanta, GA: U.S. Department of Health and Human Services; 2016. http://www.webcitation.org/6vAPQZG6c. Accessed 2 Nov 2017.
Centers for Disease Control and Prevention. Lifetime risk of HIV diagnosis Atlanta, GA: National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; 2016. https://www.cdc.gov/nchhstp/newsroom/2016/croi-press-release-risk.html. Accessed 10 Dec 2017.
Centers for Disease Control and Prevention. Estimates of New HIV Infections in the United States. Atlanta, GA: National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; 2016.
Centers for Disease Control and Prevention. HIV Prevention: Progress to Date. Atlanta, GA: U.S. Department of Health and Human Services; 2013.
Van der Elst EM, Mbogua J, Operario D, Mutua G, Kuo C, Mugo P, et al. High acceptability of HIV pre-exposure prophylaxis but challenges in adherence and use: qualitative insights from a phase I trial of intermittent and daily PrEP in at-risk populations in Kenya. AIDS Behav. 2013;17(6):2162–72.
Young I, McDaid L. How acceptable are antiretrovirals for the prevention of sexually transmitted HIV?: a review of research on the acceptability of oral pre-exposure prophylaxis and treatment as prevention. AIDS Behav. 2014;18(2):195–216.
McGowan I. Rectal microbicides: can we make them and will people use them? AIDS Behav. 2011;15(1):66–71.
Kirby T, Thornber-Dunwell M. Uptake of PrEP for HIV slow among MSM. Lancet. 2014;383(9915):399.
Smith D, Grant R, Weidle P, Lansky A, Mermin J, Fenton K. Interim guidance: preexposure prophylaxis for the prevention of HIV infection in men who have sex with men. MMWR Morb Mortal Wkly Rep. 2011;60(3):65–8.
Uthman OA. Global, regional, and national life expectancy, all-cause and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–544.
Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA. CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63:3–27.
Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, et al. Risk factors for HIV infection among men who have sex with men. Aids. 2006;20(5):731–9.
Sander PM, Cole SR, Stall RD, Jacobson LP, Eron JJ, Napravnik S, et al. Joint effects of alcohol consumption and high-risk sexual behavior on HIV seroconversion among men who have sex with men. AIDS. 2013;27(5):815.
Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. Int J Pub Health. 2010;55(3):159–66.
Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: systematic review and meta-analysis of experimental studies. Addiction. 2012;107(1):51–9.
Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS—a systematic review. Alcohol Alcohol. 2010;45(2):159–66.
Bruce D, Kahana S, Harper GW, Fernández MI. ATN t. Alcohol use predicts sexual risk behavior with HIV-negative or partners of unknown status among young HIV-positive men who have sex with men. AIDS Care. 2013;25(5):559–65.
Sen B. Does alcohol-use increase the risk of sexual intercourse among young people? Evidence from the NLSY97. J Health Econ. 2002;21:1085–93.
Grossman M, Markowitz S. I did what last night?! Adolescent risky sexual behaviors and substance use. East Econ J. 2005;31:383–405.
Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16(6):1394–410.
Kahler CW, Wray TB, Pantalone DW, Kruis RD, Mastroleo NR, Monti PM, et al. Daily associations between alcohol use and unprotected anal sex among heavy drinking HIV-positive men who have sex with men. AIDS Behav. 2015;19(3):422–30.
Dermen KH, Cooper ML. Sex-related alcohol expectancies among adolescents: I. Scale development. Psychol Addict Behav. 1994;8(3):152.
Leigh BC. The relationship of sex-related alcohol expectancies to alcohol consumption and sexual behavior. Addiction. 1990;85(7):919–28.
Jones BT, Corbin W, Fromme K. A review of expectancy theory and alcohol consumption. Addiction. 2001;96(1):57–72.
Darkes J, Goldman MS. Expectancy challenge and drinking reduction: process and structure in the alcohol expectancy network. Exp Clin Psychopharmacol. 1998;6(1):64.
Scott-Sheldon LA, Terry DL, Carey KB, Garey L, Carey MP. Efficacy of expectancy challenge interventions to reduce college student drinking: a meta-analytic review. Am Psychol Assoc. 2012;26:393.
Woolf-King SE, Maisto S, Carey M, Vanable P. Selection of film clips and development of a video for the investigation of sexual decision making among men who have sex with men. J Sex Res. 2010;47(6):589–97.
Scott-Sheldon LA, Carey KB, Cunningham K, Johnson BT, Carey MP, Team MR. Alcohol use predicts sexual decision-making: a systematic review and meta-analysis of the experimental literature. AIDS Behav. 2016;20(1):19–39.
Maisto SA, Palfai T, Vanable P, Heath J, Woolf-King S. The effects of alcohol and sexual arousal on determinants of sexual risk in men who have sex with men. Arch Sex Behav. 2012;41(4):971–86.
Centers for Disease Control and Prevention. Fact Sheet: Today’s HIV Epidemic Atlanta, GA: U.S. Department of Health and Human Services; 2016. http://www.webcitation.org/6vAPiBrwN. Accessed 2 Nov 2017.
Shuper PA, Joharchi N, Monti PM, Loutfy M, Rehm J. Acute alcohol consumption directly increases HIV transmission risk: a randomized controlled experiment. J Acquir Immune Defic Syndr. 2017;76(5):493–500.
National Institute on Alcohol Abuse and Alcoholism. Overview of Alcohol Consumption: Drinking Levels Defined Rockville, MD: U.S. Department of Health and Human Services; 2017. https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking. Accessed 4 June 2018.
Skinner H. The drug abuse screening test. Addict Behav. 1982;7:363–71.
Donovan DM, Kivlahan DR, Doyle SR, Longabaugh R, Greenfield SF. Concurrent validity of the Alcohol Use Disorders Identification Test (AUDIT) and AUDIT zones in defining levels of severity among out-patients with alcohol dependence in the COMBINE study. Addiction. 2006;101(12):1696–704.
Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804.
Allen JP, Litten RZ, Fertig JB, Babor T. A review of research on the Alcohol Use Disorders Identification Test (AUDIT). Alcohol Clin Exp Res. 1997;21(4):613–9.
Reinert DF, Allen JP. The alcohol use disorders identification test (AUDIT): a review of recent research. Alcohol Clin Exp Res. 2002;26(2):272–9.
Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. J Subst Abuse Treat. 2007;32(2):189–98.
Sobell LC, Sobell MB. Timeline follow-back. Measuring alcohol consumption. New York: Springer; 1992. p. 41–72.
Sobell LC, Brown J, Leo GI, Sobell MB. The reliability of the Alcohol Timeline Followback when administered by telephone and by computer. Drug Alcohol Depend. 1996;42(1):49–54.
Maisto SA, Conigliaro JC, Gordon AJ, McGinnis KA, Justice AC. An experimental study of the agreement of self-administration and telephone administration of the Timeline Followback interview. J Stud Alcohol Drugs. 2008;69(3):468–71.
Rueger SY, Trela CJ, Palmeri M, King AC. Self-administered web-based timeline followback procedure for drinking and smoking behaviors in young adults. J Stud Alcohol Drugs. 2012;73(5):829–33.
Schroder KE, Johnson CJ, Wiebe JS. Interactive voice response technology applied to sexual behavior self-reports: a comparison of three methods. AIDS Behav. 2007;11(2):313–23.
Wray TB, Kahler CW, Monti PM. Using ecological momentary assessment (EMA) to study sex events among very high-risk men who have sex with men (MSM). AIDS Behav. 2016;20(10):2231–42.
Gordon CM, Carey MP, Carey KB. Effects of a drinking event on behavioral skills and condom attitudes in men: implications for HIV risk from a controlled experiment. Health Psychol. 1997;16(5):490.
Helweg-Larsen M, Collins BE. The UCLA Multidimensional Condom Attitudes Scale: documenting the complex determinants of condom use in college students. Health Psychol. 1994;13(3):224.
Leigh BC. Alcohol expectancies and reasons for drinking: Comments from a study of sexuality. Psychol Addict Behav. 1990;4(2):91.
Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Psychol. 1960;24(4):349.
Reynolds WM. Development of reliable and valid short forms of the Marlowe–Crowne social desirability scale. J Clin Psychol. 1982;38(1):119–25.
George WH, Davis KC, Norris J, Heiman JR, Stoner SA, Schacht RL, et al. Indirect effects of acute alcohol intoxication on sexual risk-taking: the roles of subjective and physiological sexual arousal. Arch Sex Behav. 2009;38(4):498–513.
Fromme K, D’Amico EJ, Katz EC. Intoxicated sexual risk taking: an expectancy or cognitive impairment explanation? J Stud Alcohol Drugs. 1999;60(1):54.
Maisto SA, Carey MP, Carey KB. Effects of alcohol and expectancies on HIV-related risk perception and behavioral skills in heterosexual women. Exp Clin Psychopharmacol. 2004;12(4):288–97.
Maisto SA, Carey MP, Carey KB, Gordon CM. The effects of alcohol and expectancies on risk perception and behavioral skills relevant to safer sex among heterosexual young adult women. J Stud Alcohol. 2002;63(4):476–85.
Maisto SA, Carey MP, Carey KB, Gordon CM, Schum JL, Lynch KG. The relationship between alcohol and individual differences variables on attitudes and behavioral skills relevant to sexual health among heterosexual young adult men. Arch Sex Behav. 2004;33(6):571–84.
Curtin JJ, Fairchild BA. Alcohol and cognitive control: Implications for regulation of behavior during response conflict. J Abnorm Psychol. 2003;112(3):424–36.
Albarracin D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: a meta-analysis. Psychol Bull. 2001;127(1):142.
Schacht RL, Stoner SA, George WH, Norris J. Idiographically determined versus standard absorption periods in alcohol administration studies. Alcohol Clin Exp Res. 2010;34(5):925–7.
Acknowledgements
This manuscript was supported by P01AA019072 (to PM), L30AA023336 (to TW), K05AA019681 (to PM), and K08AA024056 (to MC) from the National Institute on Alcohol Abuse and Alcoholism.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wray, T.B., Celio, M.A., Pérez, A.E. et al. Causal Effects of Alcohol Intoxication on Sexual Risk Intentions and Condom Negotiation Skills Among High-Risk Men Who Have Sex with Men (MSM). AIDS Behav 23, 161–174 (2019). https://doi.org/10.1007/s10461-018-2243-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2243-x