Abstract
Although alcohol consumption is frequently perceived as a driver of condomless sex and subsequent HIV acquisition, the causal nature of this relationship remains unclear, and little is known about alcohol’s direct versus indirect impact on the sexual risk dynamics of those who are HIV-positive. To address this gap, we present the protocol for an in-progress NIAAA-funded controlled experiment, wherein a sample of HIV-positive men-who-have-sex-with-men (MSM) undergoes an alcohol consumption manipulation (alcohol/placebo/control) and sexual arousal induction (sexually aroused/non-aroused), and then reports intentions to engage in condom-protected and condomless sexual acts with hypothetical sexual partners differing in HIV serostatus (HIV+/HIV−/HIV status unknown), condom use preference (use/don’t use/not stated), and physical attractiveness (attractive/unattractive). Study outcomes will identify alcohol’s impact on HIV-positive MSM’s condomless sex intentions in the context of experimentally-manipulated factors as well as risk-relevant personality traits and alcohol-related expectancies. Detailed experimental procedures, ethical considerations, and potential implications for HIV prevention are discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Human immunodeficiency virus (HIV) continues to pose a public health threat, with recent estimates indicating 1.3 million North Americans living with HIV [1], as well as increasing rates of HIV incidence among some subpopulations [2, 3]. Mainly fueling this persistent HIV epidemic is condomless sex between HIV-infected and non-infected individuals. It is estimated that over 70 % of people living with HIV (PLWH) maintain sexual activity after diagnosis [4], and roughly one third of PLWH continue to engage in condomless sex [5]. The occurrence of such sexual acts has significantly contributed toward the marked resurgence of the HIV epidemic among North American men who have sex with men (MSM) [6], with new HIV infections among MSM in the United States increasing by more than 50 % in recent years [7].
Although alcohol consumption is often deemed to be a driver of condomless sex, this supposition has not been without controversy [8–11]. On the one hand, it has been theorized that alcohol directly impacts condom use decisions, whereby consuming alcohol causes individuals to experience alcohol myopia; a state in which a constraint in cognitive capacity leads to a focus on limited, risk-impelling cues (e.g., sexual arousal) and a disregard of risk-inhibiting cues (e.g., HIV transmission) [12]. On the other hand, the alcohol-condomless sex link may be indirect, resulting from underlying alcohol-related expectancies [9, 13–19] or risky personality traits, such as sensation seeking [20–23] or sexual compulsivity [24–27] (see also [10, 28–31]). Consequently, these theoretical controversies are reflected in the primarily cross-sectional empirical literature, which overall has yielded mixed evidence for a direct alcohol-condomless sex association [10].
Given these complexities, there has been a growing emphasis on conducting experiments to better assess the possible causal linkages between alcohol and condomless sex [9, 32]. Although such investigations focus on condomless sex intentions rather than actual risk behavior due to ethical and practical considerations [32], meta-analyses have demonstrated moderate to strong correlations (.44–.46) between intentions and condom use, suggesting that intentions are suitable surrogate indicators of actual sexual risk behavior [33, 34]. Despite being few in number [32], experiments have tended to support the notion of a causal association between alcohol consumption and condomless sex (see [35] for a review), and in accordance with alcohol myopia theory [12], the associations have often been moderated by sexual arousal [36–39] and impelling cognitions [40]. Within the context of these experiments, support for the role of personality factors [41, 42] and alcohol expectancies [18, 19, 43] has also been yielded, albeit to a lesser extent [44].
In spite of this much needed experimentally-derived insight, no experiments to date have assessed the impact of alcohol consumption on sexual risk intentions among PLWH. This is a considerable limitation, given not only the direct relevance of PLWH’s condomless sex to the ongoing HIV epidemic, but also recognizing that PLWH may possess distinct underlying risk-relevant motivations and personality traits.
From a motivational perspective, whereas HIV-negative individuals’ decisions to use condoms may be driven by a “self-protection” motivation, the decision for PLWH may be primarily driven by an impetus to protect their partners from becoming infected with the virus [21, 45, 46]. Contextualizing this within an alcohol myopia framework, for HIV-negative individuals, the prospect of acquiring HIV would typically serve as a risk-inhibiting cue. However, for many of those not infected with the virus, the perceivably remote possibility of HIV acquisition may be a cue that is too weak or too distal to the point where it is readily ignored under conditions of intoxication. In contrast, for many PLWH, transmitting one’s HIV through condomless sex would be recognized as a serious, immediate concern. It remains unclear, however, whether this unique, generally robust underlying factor would continue to be both salient and strong enough to inhibit condomless sex decisions among PLWH under conditions of intoxication, especially when risk-impelling cues may also be present.
With respect to personality, it is possible that as a result of previous behavioral patterns that initially led to HIV acquisition, PLWH may possess riskier personality traits than non-infected individuals [47]. These personality disparities, in turn, may be linked to differential proclivities to engage in riskier sexual behaviors. Furthermore, the possible riskier personality profiles among PLWH may underpin greater motivation to attend to risk-impelling cues, and/or poorer ability to attend to multiple cues that are available. These risk-biased mechanisms may subsequently become exacerbated when consuming alcohol, resulting in even further diminished condom use intentions under such circumstances.
The Present Investigation
In recognizing that there has been limited experimental work on alcohol and HIV that has simultaneously examined moderating factors within the purview of alcohol myopia theory, and acknowledging the necessity of including PLWH in such experiments, we developed an innovative experimental approach to identify the extent to which acute alcohol consumption can causally increase condomless sex intentions among HIV-positive MSM. Furthermore, to account for theorized moderators of the alcohol-condomless sex association, our experimental protocol was designed to assess alcohol’s causal impact in the context of personality traits, sex-related alcohol expectancies, and risk-relevant partner characteristics.
This investigation has received funding from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (4R21AA020236-02) and is currently in progress. The present manuscript (1) provides a detailed overview of the study protocol, (2) presents a number of ethical considerations, and (3) discusses potential study-related implications for HIV prevention.
Study Overview and Hypotheses
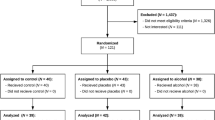
The current investigation involves a controlled experiment in which HIV-positive MSM undergo an alcohol manipulation (control/placebo/alcohol), receive an arousal induction (no arousal/sexual arousal), and indicate their intentions to engage in condom-protected and condomless anal sexual acts with hypothetical sexual partners differing by HIV serostatus (HIV+/HIV−/HIV status unknown), preference for condom use (use/don’t use/not stated), and physical attractiveness (unattractive/attractive). To account for possible moderating risk factors that cannot be experimentally manipulated, HIV-positive MSM also complete measures of sexual sensation seeking [20], sexual compulsivity [48], and alcohol expectancies [49]. An overview of the study design is shown in Fig. 1. Study hypotheses are as follows:
Experimental design. The experiment is based on the random allocation of two between-subjects factors. Factor 1 involves alcohol with three levels: no alcohol, placebo alcohol to isolate the effect of expectancies, and alcohol (target BAC of 0.08 %). Factor 2 involves sexual arousal with two levels: non-aroused and sexually aroused. Both factors are crossed to create six cells. In addition, descriptions of potential hypothetical sexual partners are provided, forming three within-subject factors, with partners differing in terms of HIV serostatus (HIV+/HIV−/HIV status unknown), preference for condom use (use/don’t use/not stated), and level of physical attractiveness (unattractive/attractive). Participants’ levels of sexual compulsivity, sexual sensation seeking, and sex-related alcohol expectancies are included as moderators
Hypothesis 1: Acute Alcohol Consumption. In accordance with alcohol myopia theory [12], compared to HIV-positive MSM receiving no alcohol (control/placebo), HIV-positive MSM in the alcohol condition will attend less to risk-inhibiting cues and thus report stronger intentions to engage in condomless sex. Although expectancy effects associated with the placebo condition will also be explored, based on the results from previous experiments examining alcohol and risk intentions [15, 42, 50–54], we anticipate that risky sex intentions will be similar for participants in the placebo and control conditions.
Hypothesis 2: Sexual Arousal. Because sexual arousal can serve as a salient risk-impelling cue [55], HIV-positive MSM receiving the sexual arousal induction will report stronger intentions to engage in condomless sex than those in the “no arousal” condition.
Hypothesis 3: Acute Alcohol Consumption × Sexual Arousal. Given that sexual arousal will be an especially salient risk-impelling cue through the alcohol myopic lens of acute alcohol consumption [56], an interaction between alcohol and arousal is predicted such that over and above the impact of the main effects for these two factors, intentions to engage in condomless sex will be strongest among HIV-positive MSM who have both received alcohol and experienced a sexual arousal induction.
Hypothesis 4. Higher-order interactions among acute alcohol consumption, sexual arousal, and partner factors will be statistically tested in accordance with the propositions of alcohol myopia theory. For example, among HIV-positive MSM consuming alcohol, we will assess whether the presence of multiple highly salient and in-the-moment risk-inhibiting cues (e.g., partner is HIV-negative and prefers to use condoms) can diminish the impact of a risk-impelling cue (e.g., partner is attractive [19]; being sexually aroused).
Hypothesis 5: Acute Alcohol Consumption × Personality. The causal association between acute alcohol consumption and condomless sex intentions will be moderated by personality, such that the association will be higher for HIV-positive MSM who are higher in sexual sensation seeking and/or sexual compulsivity compared to those who are lower on these dimensions.
Hypothesis 6: Acute Alcohol Consumption × Alcohol Expectancies. The causal association between acute alcohol consumption and condomless sex intentions will be moderated by sex-related alcohol expectancies, such that the association will be higher for HIV-positive MSM who possess higher expectancies compared to those who possess lower expectancies.
Method
Participants
The study involves the participation of 140 HIV-positive MSM recruited from a clinic specializing in HIV care in Toronto, Canada. Individuals must (1) be 19 years of age or older (i.e., legal drinking age in Ontario); (2) be HIV-positive; (3) report insertive or receptive anal sex with a man in the past 6 months; (4) be a social drinker; (5) report no recent history of problematic alcohol/substance use; and (6) have no contraindications for consuming alcohol to a BAC of approximately 0.10 % (Note: Due to inter-person variability in absorption, etc., the BAC of some individuals could go higher than a maximum BAC of 0.08 % that is targeted in the present experiment, and as a result, physicians’ screening employs the stricter alcohol standard of 0.10 % BAC). Details pertaining to the assessment of eligibility criteria can be found in the below section entitled “Screening.”
Materials and Procedure
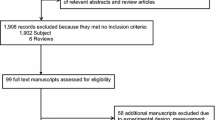
Overview
A flowchart depicting the study components can be found in Fig. 2. Individuals are screened for eligibility, and qualifying participants attend a single-day study session, which involves (1) supplementary screening and consent; (2) a comprehensive assessment; (3) the experimental procedures; and (4) detoxification, supplementary assessment, and debriefing. Medical chart extraction is also performed separately after the session.
Screening
To ensure the health and safety of participants, and building on procedures from past alcohol administration experiments [18, 36–38, 41, 42, 50–52, 54, 57], a thorough screening process is employed. To be eligible, participants must receive approval from their medical doctor at the HIV clinic. Doctors are fully informed of the study procedures, and they may deem an individual as ineligible to participate if there are any known or suspected contraindications for consuming alcohol to a conservative BAC of approximately 0.10 % (e.g., contraindications include interactions between alcohol and medications; hepatitis coinfection or liver issues; relevant alcohol, substance use, or mental health concerns). In addition to receiving approval from one’s doctor, a 12-item screener, delivered by a research team member, is employed to assess additional eligibility requirements including recent (i.e., past 6-months) anal sex with a man; identification as a “social drinker” (adapted from Davis et al. [36], defined as consuming at least five drinks/week on average and consuming five or more drinks in one episode during the past 6 months); no recent history (i.e., past 5 years) of alcohol-related problems, concern, or treatment; and no allergies to alcoholic beverage ingredients or citrus products.
Study Session
Eligible participants are scheduled for a 1-day study session that is conducted in specialized research laboratory facilities at an addictions and mental health hospital in Toronto, Canada. Two research assistants (RAs) administer the study, with each RA being assigned specific tasks to ensure experimental integrity (e.g., blinding) as well as participant safety.
Supplementary Screening and Consent
Upon arriving at the research facility, RA1 and the participant go through a brief, supplementary screening checklist to verify that all day-of study requirements have been met (e.g., not driving to the site; fasting from food and beverages for 3 h prior to the session, etc.). Participants are provided with two public transit tokens to cover their travel to and from the site. A breathalyzer test is also performed using an AlcoSensor IV (Intoximeters Inc.), and if a reading other than 0.000 % is yielded, the participant is not allowed to continue. Eligible participants are asked to provide written consent.
Assessment
Participants are weighed and asked for their height, and then complete a self-report questionnaire assessing demographics, alcohol and substance use, risk-relevant personality traits, sex-related alcohol expectancies, and recent sexual history. The questionnaire is delivered via touch-screen tablet computer programmed with MediaLab v.2010.3 [58].
Demographics
Demographic items assess age, race/ethnicity, sexual orientation, education, employment, and partnership status.
Alcohol and Substance Use
The 10-item alcohol use disorders identification test (AUDIT) [59] assesses the degree to which participants consume alcohol, and two additional questions assess alcohol use in sexual contexts (i.e., “In the last six months, about how often did you consume alcohol immediately before or during sex?,” “In the last six months, about how often would you say that alcohol use made it more difficult for you to have safer sex?;” 4-point scales, “Never”-“All the Time”). The NIDA Drug Use Screening Tool [60] is also employed to identify lifetime and recent (i.e., past 3 months) use of a variety of substances.
Personality Factors and Expectancies
Measures of risk-relevant personality constructs include Kalichman et al.’s 10-item sexual compulsivity scale [48] and Kalichman et al.’s 11-item sexual sensation seeking scale [20]. Additionally, Leigh’s 13-item scale is used to assess participants’ sex-related alcohol expectancies [49].
Sexual Behavior
The sexual behavior assessment is based on a questionnaire previously employed in a large-scale investigation of MSM [61]. Items assess the number of HIV-positive, HIV-negative, and HIV status unknown male sexual partners a in the past 6 months, and follow-up questions ask about the total number as well as the number of condom-protected and condomless oral, receptive anal, and insertive anal acts engaged in, all by partner serostatus.
Experiment
Upon completing the computer-based assessment, RA2 takes the participant to a specialized laboratory that resembles a real-life barroom. In addition to the multiple alcohol-related visual cues located throughout the barroom lab that enhance the realism of the setting (e.g., alcohol bottles on shelves, alcohol signage, etc.), 30 ml of vodka is poured in a shallow container out of sight behind the bar approximately 20 min prior to the participant’s arrival, which provides a strong alcohol olfactory cue that can be sensed immediately upon entering the barroom. Once the participant has been seated on the patron side of the bar, RA2 stands behind the bar and provides an overview of the beverage consumption procedures. RA2 then holds up two small sealed envelopes, and explains that each envelope contains a card that either says “ALCOHOL” or “WATER,” which will determine the participant’s beverage condition (Note—alcohol and placebo cards are identical—both say “ALCOHOL” in capital letters—with the exception of one differentiation only perceptible to the RA). Cards within the envelopes have been pre-randomized so that the likelihood of receiving alcohol, placebo alcohol, or water, is 50, 25, and 25 %, respectively. Participants are asked to select one envelope and are shown the card. It should be noted that this active selection process capitalizes on the “illusion of control” phenomenon [62], where choice leads to greater confidence in the outcome; thus, placebo participants who end up selecting a card that says “ALCOHOL” should in turn be relatively more convinced by the placebo manipulation. The beverage administration procedure then follows steps similar to those used in past alcohol experiments and is detailed as follows:
Alcohol Condition
Participants assigned to the alcohol condition are instructed that they will be receiving alcohol and that their blood alcohol concentration might go up to a level of around 0.080 %. They are also told that people react differently to alcohol, and that they may feel the effects of alcohol a little bit or a lot.
The administration commences with RA2 placing a bottle of Smirnoff Vodka on the bar, along with three cans of Canada Dry tonic water. With the participant watching, vodka and tonic are measured by RA2 using graduated cylinders, based on a formulation of 0.7 g alcohol/kg body weight, and derived from vodka and tonic water in a 1:3 ratio. Once mixed together, 1/3 of the total volume of the vodka-tonic mix is poured into a cup, with 5 ml of lemon/lime juice poured on top from a lime juice container, and 5 ml of vodka poured on top from a lemon juice container (note—this 5 ml of vodka per cup is accounted for in the alcohol formulation). The participant is then given the cup and asked to consume the drink within 5 min, and a timer is placed on the bar in front of the participant. Two additional cups are prepared in the same manner, each containing 1/3 of the original total volume, and the same consumption schedule is followed. Therefore, by the end of the administration, participants will have consumed one third of the total volume every 5 min over the course of the 15-min consumption period.
Placebo Condition
Procedures and instructions for participants in the placebo condition are identical to those in the alcohol condition except that instead of actual Smirnoff Vodka, a Smirnoff Vodka bottle that has been pre-filled with flat tonic water is used. Additionally, the rims of each of the three beverage cups are dipped in vodka prior to being filled. This vodka around the rim combined with the vodka floated on top of each drink (poured from the lemon juice container immediately prior to serving) provides a strong alcohol taste, thus enhancing the perception of actual alcohol consumption.
Water (Control) Condition
In the control condition, participants are told that they will be consuming water, and three sealed 500 ml bottles of Nestle brand water are placed on the bar. RA2 measures a volume of water matching the total volume of fluid that would have been provided in the other beverage conditions. One third of the total volume of water is poured into a cup, and similar to the above procedures, participants are asked to consume one cup every 5 min over the course of the 15-min consumption period.
Absorption Period—All Beverage Conditions
After the 15-min consumption period, a timer is started, and all participants are asked to sit on a couch in the barroom where they can read magazines that have been pre-selected based on the absence of sexual content. At the 8-min point, participants are asked to rinse their mouths with water, which serves to reduce any alcohol residue that may be present in a participant’s saliva, and at the 10- and 13-min points, participants are breathalyzed, and values are recorded by RA2. Participants are not provided with any feedback regarding their breathalyzer test results. Following the second breathalyzer test, RA2 administers an alcohol manipulation check, which asks participants to indicate how intoxicated they feel at that moment using a 10-point scale ranging from “Not at all intoxicated” to “Very intoxicated.” RA2 then summons RA1, who was not in the barroom during the beverage administration and is therefore completely blind to beverage condition.
It should be noted that initially, a time-to-criterion BAC procedure was called for, in which alcohol condition participants would continue to be breathalyzed beyond the 13-min absorption period until their BAC reached a level of 0.045 % [37], at which point they would move on to the next part of the experiment. This procedure also called for each control and placebo participant to be yoked to an alcohol condition participant who had already completed the study (see [37]). However, in piloting these procedures, all individuals who consumed alcohol showed a BAC greater than 0.045 % by the end of the 13-min absorption period. We therefore opted to instead maintain a consistent time interval for all participants, in which they would commence the next phase of the experiment exactly 13 min after their last beverage.
Computer-Based Experimental Stimuli and Outcome Assessment
RA2 leaves the barroom when RA1 arrives, and RA1 sets up a touch-screen tablet laptop on the bar and explains the remaining procedures. Participants are told that they will watch two brief video clips that may contain sexual content, and that they will be asked to rate the clips based on a variety of criteria. They are also informed that after watching the clips, they will be presented with a series of hypothetical sexual partners and will be asked to indicate their intentions to engage in a range of sexual acts with each partner. Both video- and partner-based aspects are built into an integrated computer program, which is derived from the work of Shuper and Fisher [55] and was designed using MediaLab v.2010.3 [58]. RA1 then leaves the barroom and the participant is left alone to complete the program at his own pace.
Video Clips—Sexual Arousal Manipulation
Two sets of videos, each comprised of two 3-min video clips, constitute the sexual arousal manipulation and are randomly assigned by the program. Similar to Shuper and Fisher [55], the two videos designed to elicit feelings of sexual arousal each depict two men engaged in kissing, heavy petting, and oral sex without a condom (anal sex with or without condoms is not shown). In contrast, videos for the non-arousal condition depict two men engaged in a discussion about sporting events. Videos were selected based on pilot testing with a sample of MSM receiving care from the same clinic at which current study participants are recruited. Manipulation check items follow each video, which include general questions about the video (e.g., “How enjoyable was the video?” 10-point response scale: “Not at all Enjoyable” to “Very Enjoyable”), as well as questions about participants’ current level of sexual arousal (e.g., “How sexually aroused are you right now?” 10-point response scale “Not at all Sexually Aroused” to “Very Sexually Aroused”).
Hypothetical Sexual Partners and Sexual Risk Outcomes
Following the videos, a series of 18 hypothetical sexual partner profiles are presented in random order. Each profile consists of a photograph of a potential male partner (physically attractive/physically unattractive, as determined through pilot testing with MSM from the clinic), along with a brief, non-eroticized text description of the individual who is portrayed as someone who was just met, and who varies based on HIV serostatus (HIV-positive/HIV-negative/HIV status unknown) and preference for condom use (prefers to use a condom/not use a condom/no preference stated). A sample partner description reads as follows: “This is the first time that you met John. He is HIV-negative. John says that he prefers not to use condoms when he has sex.” A set of six corresponding sexual behavior items accompany each partner profile, in which participants are asked “Which of the following would you consider doing with this partner?” The list of sexual behaviors that follows includes mutual masturbation, insertive oral sex without a condom, and both receptive and insertive anal sex, with and without condoms. Intentions for each behavior are assessed using five-point scales ranging from “Definitely” to “Definitely Not.” The main study outcomes are based on these measures, focusing on participants’ intentions to engage in condomless receptive and condomless insertive anal sexual acts.
After responding to all 18 hypothetical sexual partners, manipulation check items assess perceived sexual arousal and perceived intoxication using the same items described above. The participant then summons an RA who obtains a breathalyzer reading (non-control participants).
Detoxification, Supplementary Assessment, and Debriefing
After completing the barroom activities, the participant is escorted to a laboratory room with comfortable seating, magazines, movies, and cable television. Furthermore, brochures about alcohol and substance use, HIV, and safer sex are present. Participants are offered snacks and non-alcoholic beverages, and a full meal is provided. For participants who received alcohol, breathalyzer tests are completed every 15–30 min, and following NIAAA guidelines [63], participants remain at the facility until they provide two consecutive breathalyzer readings below 0.040 % BAC. Participants in the placebo condition are informed that they had received only a very low dose of alcohol, and that this minimal amount has been cleared from their system.
A brief, supplementary self-report assessment is administered to identify year of diagnosis, perceived route of HIV infection, and if on ART, month and year of ART initiation and ART adherence. Two validated scales are employed to assess adherence, which include (1) a visual analogue scale (VAS) to identify the percentage of ART doses taken over the past month [64], and (2) an ACTG-based assessment that queries the number of doses of each ART medication missed over the past 4 days [65].
At the end of the session, participants are debriefed regarding study procedures and purpose. A process debriefing procedure [66] is also enacted to reduce any lingering feelings of sexual arousal as a result of having viewed the sexually arousing videos. Briefly, this procedure entails a discussion about the nature of the sexual arousal manipulation and the feelings it was designed to elicit. Participants are asked to indicate the level of sexual arousal that they were experiencing at the beginning of the study versus at the present moment, and if a higher present versus initial arousal level is reported, an additional discussion ensues that focuses on getting the participant back to his initial arousal level. In such instances, participants are required to remain at the site, and their perceived sexual arousal levels are assessed approximately every 10 min until they report an arousal level that matches their baseline.
Once participants have been fully debriefed, are at an acceptable BAC level (breathalyzer), and also indicate (via self-report) that they do not feel intoxicated, they are provided with monetary compensation as well as condoms. Control and placebo participants receive $50 for taking part in the study, whereas alcohol participants receive $50 for the study as well as $15 for each additional hour they are required to remain for detoxification.
Medical Chart Extraction
Clinic medical chart extraction is performed after a session to identify indicators of HIV disease progression and status, including month and year of HIV diagnosis, CD4 cell count, and HIV viral load. Liver enzymes levels (e.g., ALT, AST), medications prescribed, and other health concerns are also identified.
Statistical Analyses
The core of the proposal is an experiment with randomized allocation to alcohol and arousal conditions to test the main hypotheses. Analysis of variance (ANOVA) will be used as the main statistical tool [67] to test the hypotheses as follows: Hypothesis 1 will be tested by a contrast of cells involving alcohol versus cells involving placebo and control groups [68]. Hypothesis 2 will be tested by the ANOVA main effect for arousal. Hypothesis 3 concerns the interaction between alcohol and arousal, tested by contrast analyses that will give specific contrast weights to the cell arousal+ and alcohol+, with a postulation that the effect will exceed the sum of the expected main effects by 50 %. Hypothesis 4 will involve more exploratory analyses where within-subjects partner factors will be included as independent variables into the analyses (repeated measures ANOVA). The main focus of these analyses will be the differential impact of alcohol in combination with arousal on cue discrimination. Statistically, this will correspond with the testing of higher order interactions.
Hypotheses 5 and Hypothesis 6 concern potential moderating effects of personality and alcohol expectancies, respectively. The former will not be experimentally manipulated, whereas the latter should be at least in part impacted by the placebo condition for alcohol. For statistical analyses, we will mainly compare the effect of alcohol consumption for different levels of the moderator [69, 70]. Additionally, path models will be employed to estimate the relative strengths of direct or indirect effects as well as exploring more complex moderated mediation models [71].
Ethical Considerations
All aspects of the study have been approved by the Research Ethics Board (REB) at the Centre for Addiction and Mental Health (#034/2010) and adhere to NIAAA guidelines for alcohol administration in human experimentation [63]. Furthermore, a comprehensive data and safety monitoring plan has been implemented to identify adverse events and guide corresponding action. The primary ethical considerations inherent in the present investigation relate to alcohol administration, sexual arousal induction, sensitive questions, and confidentiality.
Alcohol Administration
All prospective participants are recruited from a medical clinic specializing in HIV care, and clinic medical staff only refer/approve HIV-positive MSM patients for whom the consumption of alcohol to a conservative level of 0.10 % BAC is not medically contraindicated. A complementary screening assessment is also conducted by a research team member who is not a clinic staff member, and this process helps identify alcohol-related or other relevant issues that may not have been disclosed to one’s medical provider. Additionally, only participants who are classified as “social drinkers” (described above) can take part in this research. Therefore, the amount of alcohol that participants consume over the course of the study is similar to an amount that they would have recently consumed on their own. Taken together, the use of these stringent referral and screening procedures, which build on those used by past investigations in this area [18, 36–38, 41, 42, 50–52, 54, 57], and which adhere to NIAAA guidelines [63], minimize risk by excluding individuals for whom the alcohol manipulation could have potentially been a concern.
Measures to reduce possible risks associated with the alcohol manipulation have also been built into the consent process and supplementary screening. During consent, participants are made well aware that they may consume alcohol in the study, and that the level consumed targets a BAC level of 0.08 %, which reflects the legal intoxication cut-off. Participants are also made aware of the risks associated with consuming alcohol, and due to safety reasons, they are informed that they have to remain in the study room until their BAC has dropped to a level of 0.04 % or lower, and that they cannot operate a vehicle after the study session. If prior to commencing the study a participant reports that he is unable to remain in the study room for the required period, or if it is known or suspected that the participant intends on operating a vehicle afterwards, the study session will not be initiated. Participants are further informed that they can stop their participation and/or stop consuming the alcoholic beverages at any time without penalty or consequences, and to notify the RA immediately should they begin to feel ill or uncomfortable. Finally, participants are instructed that they may consume lemon and lime juice, and to notify research personnel if they have a known or suspected citrus allergy.
Along with the above-mentioned safeguards, additional protective procedures have been implemented throughout the experimental session. Participants who receive alcohol are administered breathalyzer tests during the experiment (as described above) and throughout the detox period, and BAC levels are closely monitored by RAs. Two RAs are always on hand while the experiment is taking place, and all RAs have received first-aid training. As the research is being conducted at an addictions and mental health hospital, the research lab facilities are close in proximity to the hospital’s emergency department. Thus, even though medical emergencies are not anticipated, appropriate assistance is readily available if necessary.
Sexual Arousal Induction
Participants in the sexual arousal condition are presented with video clips depicting sexual content, which could make some individuals feel uncomfortable. However, participants are informed of the sexual nature of the clips prior to the study and during the consent process, and it is likely that individuals who would not feel comfortable watching such videos would choose not to take part. Furthermore, those who do choose to participate are informed that they can skip any or all parts of the videos, and this does not affect their participation.
Additionally, process debriefing (described above) directly addresses two ethical concerns associated with the sexual arousal manipulation. First, as with any research, participants should leave a study in the same state of mind in which they arrived. Second, an elevated level of sexual arousal at study departure could increase the likelihood of seeking out a sexual partner and potentially engaging in condomless sex. Process debriefing therefore helps dissipate any lingering arousal that may have resulted from the experimental manipulation.
Sensitive Questions
In the consent process, participants are made aware of the questioning surrounding alcohol use, substance use, and sex. Furthermore, participants are informed that they do not have to answer any questions that they feel uncomfortable answering, and that the program has been designed to allow for questions to be skipped.
Confidentiality
In recognizing the population under investigation and the sensitive nature of the questions being asked, the maintenance of participant confidentiality becomes paramount, and several steps have thus been implemented to protect the privacy of participants and the data they provide. First, participants are assigned a unique study ID number, and study data are identifiable by this number only. Second, participants enter their data on password-protected and encrypted computers, and all data are devoid of protected health information (PHI). Third, data are transferred from study computers to a password-protected location on a secure hospital server using encrypted flash drives. Fourth, medical chart review data are recorded by study ID number only and do not include PHI, and these data are entered into an electronic database stored on the above-mentioned secure server. Finally, data are accessible only by authorized study personnel and are not provided to clinic staff.
Potential Implications for HIV Prevention
It is conceivable that the findings will have considerable impact on HIV prevention initiatives, particularly with respect to (1) allowing for the identification of PLWH who may be most at risk for engaging in condomless sex; and (2) developing interventions that address underlying and in-the-moment drivers of condomless sex among high-risk PLWH subgroups.
Identifying PLWH Subgroups at Risk for HIV Transmission
Although HIV prevention efforts have traditionally been targeted toward HIV-negative individuals [72], there has recently been an increased impetus for conducting HIV intervention research with those who are already infected with HIV [73, 74]. The premise behind this shift toward “prevention-with-positives” stems from the actuality that every new case of HIV derives from someone who is already infected with the virus, and thus, in order to have the strongest possible impact on the HIV epidemic, it is crucial to address the condom-related decision making processes enacted by PLWH. Within the context of alcohol-related risk, given that levels of alcohol consumption and alcohol abuse are particularly high among PLWH [75, 76], and recognizing the potentially unique alcohol-related risk dynamics associated with PLWH’s personality traits and motivations, prevention efforts that account for alcohol’s possible direct and/or indirect impact on sexual risk would likely be necessary to effectively promote safer sex among PLWH.
Results from our investigation will thus provide much needed insight regarding which PLWH subgroups would be most at risk for engaging in condomless sex and transmitting HIV. For example, findings indicating that alcohol intoxication can causally increase condomless sex intentions would suggest that PLWH should be screened for alcohol use at the clinic level, and PLWH demonstrating specified alcohol use patterns could in turn be offered appropriate interventions which have shown evidence to reduce risky drinking occasions [77] (see next section below). In contrast, results could demonstrate that alcohol on its own may not cause increased risk intentions, but rather that the desire to engage in condomless sex may be linked to underlying risky personality traits and/or sex-related alcohol expectancies. These latter factors could also be easily identified through a brief, clinic-based screening process, which could then be followed by the administration of appropriate intervention efforts.
Implementing Targeted Interventions
Once “high-risk” PLWH have been identified, interventions that directly address the underlying drivers of sexual risk behavior could be developed and implemented within HIV clinical care settings. Based on a demonstrated direct causal impact of alcohol on condomless sex, the delivery of brief alcohol-reduction interventions would be recommended [59], which could lead to a decrease in alcohol use and/or binge drinking, and in turn, a corresponding decrease in the occurrence of condomless sex. On the other hand, should personality or expectancies be identified as the primary precursors of risk, behavior change approaches, such as those based on the Information–Motivation–Behavioral Skills (IMB) model [72, 78, 79], could be tailored to address associated deficits in safer sex-related motivation and skills. Along with these behavioral methods, pharmacological treatments could also be offered not only to reduce alcohol consumption, but also to dampen the manifestation of risk-prone personality traits such as sexual compulsivity; both of which could possibly diminish the likelihood of condomless sex [80, 81].
Study findings could additionally help identify significant in-the-moment risk-impelling and risk-inhibiting factors. Within this realm, the impact of impelling cues such as sexual arousal could potentially be attenuated through interventions that increase one’s recognition of such cues as powerful in-the-moment drivers of risk [42]. Training could also be undertaken through which the onset of sexual arousal would become a trigger to seek condoms or even to remove oneself from a potentially risky situation [38]. Along similar lines, PLWH could be trained to focus on simple yet diagnostic inhibiting cues [53] such as a partner’s stated seronegativity, or to rely on heuristics such as “always use a condom when you don’t know a partner’s serostatus,” [55] when intoxicated. Finally, situationally-based in-the-moment “reminders” of previously-acquired safer sex intervention content could be delivered to PLWH through either low-tech (e.g., bracelets—see [82]) or high-tech (e.g., mobile media) means.
Conclusion
In all, the current investigation entails a comprehensive appraisal of whether alcohol is capable of having a causal impact on condomless sex intentions among HIV-positive MSM; taking into account personality, expectancies, and “in the moment” contextual factors [32]. Study results will not only have the potential to impact future alcohol-risky sex investigations, but they could also form the evidentiary basis that potentially underpins effective intervention efforts aimed at reducing HIV transmission risk behavior among PLWH.
References
UNAIDS report on the global AIDS epidemic 2013. UNAIDS 2013. http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf. Accessed 6 July 2015.
Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report, 2007. Vol. 19 [inclusive page numbers]. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. http://www.cdc.gov/hiv/pdf/statistics_2007_HIV_Surveillance_Report_vol_19.pdf. Accessed 6 July 2015.
Public Health Agency of Canada. HIV and AIDS in Canada. Surveillance Report to December 31, 2008. Surveillance and Risk Assessment Division, Centre for Communicable Diseases and Infection Control, Public Health Agency of Canada. 2009.
Crepaz N, Marks G. Towards an understanding of sexual risk behavior in people living with HIV: a review of social, psychological, and medical findings. AIDS. 2002;16(2):135–49.
Kalichman SC. HIV transmission risk behaviors of men and women living with HIV-AIDS: prevalence, predictors, and emerging clinical interventions. Clin Psychol. 2000;7:32–47.
AIDS Epidemic Update. UNAIDS 2009 http://data.unaids.org/pub/Report/2009/JC1700_Epi_Update_2009_en.pdf. Accessed 6 July 2015.
Hall HI, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520–9.
Cooper ML. Alcohol use and risky sexual behavior among college students and youth: evaluating the evidence. J Stud Alcohol Suppl. 2002;14:101–17.
George WH, Stoner SA. Understanding acute alcohol effects on sexual behavior. Annu Rev Sex Res. 2000;11:92–124.
Shuper PA, Neuman M, Kanteres F, Baliunas D, Joharchi N, Rehm J. Causal considerations on alcohol and HIV/AIDS—a systematic review. Alcohol Alcohol. 2010;45(2):159–66.
Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annu Rev Sex Res. 2000;11:125–57.
Steele CM, Josephs RA. Alcohol myopia. Its prized and dangerous effects. Am Psychol. 1990;45(8):921–33.
Bryan A, Ray LA, Cooper ML. Alcohol use and protective sexual behaviors among high-risk adolescents. J Stud Alcohol Drugs. 2007;68(3):327–35.
Crowe LC, George WH. Alcohol and human sexuality: review and integration. Psychol Bull. 1989;105(3):374–86.
Gordon CM, Carey MP, Carey KB. Effects of a drinking event on behavioral skills and condom attitudes in men: implications for HIV risk from a controlled experiment. Health Psychol. 1997;16(5):490–5.
Hull JG, Bond CF Jr. Social and behavioral consequences of alcohol consumption and expectancy: a meta-analysis. Psychol Bull. 1986;99(3):347–60.
LaBrie J, Earleywine M, Schiffman J, Pedersen E, Marriot C. Effects of alcohol, expectancies, and partner type on condom use in college males: event-level analyses. J Sex Res. 2005;42(3):259–66.
Maisto SA, Carey MP, Carey KB, Gordon CM. The effects of alcohol and expectancies on risk perception and behavioral skills relevant to safer sex among heterosexual young adult women. J Stud Alcohol. 2002;63(4):476–85.
Murphy ST, Monahan JL, Miller LC. Inference under the influence: the impact of alcohol and inhibition conflict on women’s sexual decision making. Pers Soc Psychol Bull. 1998;24(5):517–28.
Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual sensation seeking: scale development and predicting AIDS-risk behavior among homosexually active men. J Pers Assess. 1994;62(3):385–97.
Kalichman SC, Heckman T, Kelly JA. Sensation seeking as an explanation for the association between substance use and HIV-related risky sexual behavior. Arch Sex Behav. 1996;25(2):141–54.
Kalichman SC, Weinhardt L, DiFonzo K, Austin J, Luke W. Sensation seeking and alcohol use as markers of sexual transmission risk behavior in HIV-positive men. Ann Behav Med. 2002;24(3):229–35.
Zuckerman M. Biological expression and biological bases of sensation seeking. New York: Cambridge University Press; 1994.
Benotsch EG, Kalichman SC, Kelly JA. Sexual compulsivity and substance use in HIV-seropositive men who have sex with men: prevalence and predictors of high-risk behaviors. Addict Behav. 1999;24(6):857–68.
Benotsch EG, Kalichman SC, Pinkerton SD. Sexual compulsivity in HIV-positive men and women: prevalence, predictors, and consequences of high-risk behaviors. Sex Addict Compuls. 2001;8(2):83–99.
Kalichman SC, Rompa D. Sexual sensation seeking and Sexual Compulsivity Scales: reliability, validity, and predicting HIV risk behavior. J Pers Assess. 1995;65(3):586–601.
Kalichman SC, Cain D. The relationship between indicators of sexual compulsivity and high risk sexual practices among men and women receiving services from a sexually transmitted infection clinic. J Sex Res. 2004;41(3):235–41.
Dingle GA, Oei TP. Is alcohol a cofactor of HIV and AIDS? Evidence from immunological and behavioral studies. Psychol Bull. 1997;122(1):56–71.
Fisher JC, Bang H, Kapiga SH. The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sex Transm Dis. 2007;34(11):856–63.
Stall R, Leigh B. Understanding the relationship between drug or alcohol use and high risk sexual activity for HIV transmission: where do we go from here? Addiction. 1994;89(2):131–4.
Woolf SE, Maisto SA. Alcohol use and risk of HIV infection among men who have sex with men. AIDS Behav. 2009;13(4):757–82.
Hendershot CS, George WH. Alcohol and sexuality research in the AIDS era: trends in publication activity, target populations and research design. AIDS Behav. 2007;11(2):217–26.
Sheeran P, Orbell S. Do intentions predict condom use? Meta-analysis and examination of six moderator variables. Br J Soc Psychol. 1998;37(Pt 2):231–50.
Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: a meta-analysis. Psychol Bull. 1999;125(1):90–132.
Rehm J, Shield KD, Joharchi N, Shuper P. Alcohol consumption and the intention to engage in unprotected sex: systematic review and meta-analysis of experimental studies. Addiction. 2012;107:51–9.
Davis KC, Hendershot CS, George WH, Norris J, Heiman JR. Alcohol’s effects on sexual decision making: an integration of alcohol myopia and individual differences. J Stud Alcohol Drugs. 2007;68(6):843–51.
Davis KC, George WH, Norris J, et al. Effects of alcohol and blood alcohol concentration limb on sexual risk-taking intentions. J Stud Alcohol Drugs. 2009;70(4):499–507.
George WH, Davis KC, Norris J, et al. Indirect effects of acute alcohol intoxication on sexual risk-taking: the roles of subjective and physiological sexual arousal. Arch Sex Behav. 2009;38(4):498–513.
MacDonald TK, MacDonald G, Zanna MP, Fong GT. Alcohol, sexual arousal, and intentions to use condoms in young men: applying alcohol myopia theory to risky sexual behavior. Health Psychol. 2000;19(3):290–8.
Norris J, Stoner SA, Hessler DM, et al. Cognitive mediation of alcohol’s effects on women’s in-the-moment sexual decision making. Health Psychol. 2009;28(1):20–8.
Maisto SA, Carey MP, Carey KB, Gordon CM, Schum JL, Lynch KG. The relationship between alcohol and individual differences variables on attitudes and behavioral skills relevant to sexual health among heterosexual young adult men. Arch Sex Behav. 2004;33(6):571–84.
Norris J, Stoner SA, Hessler DM, et al. Influences of sexual sensation seeking, alcohol consumption, and sexual arousal on women’s behavioral intentions related to having unprotected sex. Psychol Addict Behav. 2009;23(1):14–22.
Fromme K, D’Amico EJ, Katz EC. Intoxicated sexual risk taking: an expectancy or cognitive impairment explanation? J Stud Alcohol. 1999;60(1):54–63.
Testa M, Fillmore MT, Norris J, et al. Understanding alcohol expectancy effects: revisiting the placebo condition. Alcohol Clin Exp Res. 2006;30(2):339–48.
Parsons JT, Vicioso KJ, Punzalan JC, Halkitis PN, Kutnick A, Velasquez MM. The impact of alcohol use on the sexual scripts of HIV-positive men who have sex with men. J Sex Res. 2004;41(2):160–72.
Parsons JT, Vicioso K, Kutnick A, Punzalan JC, Halkitis PN, Velasquez MM. Alcohol use and stigmatized sexual practices of HIV seropositive gay and bisexual men. Addict Behav. 2004;29(5):1045–51.
Shuper PA, Joharchi N, Rehm J. Personality as a predictor of unprotected sexual behavior among people living with HIV/AIDS: a systematic review. AIDS Behav. 2014;18(2):398–410.
Kalichman SC, Rompa D. The Sexual Compulsivity Scale: further development and use with HIV-positive persons. J Pers Assess. 2001;76(3):379–95.
Leigh BC. Alcohol expectancies and reasons for drinking: comments from a study of sexual experiences. Psychol Addict Behav. 1990;4:91–6.
Abbey A, Saenz C, Buck PO. The cumulative effects of acute alcohol consumption, individual differences and situational perceptions on sexual decision making. J Stud Alcohol. 2005;66(1):82–90.
Abbey A, Saenz C, Buck PO, Parkhill MR, Hayman LW Jr. The effects of acute alcohol consumption, cognitive reserve, partner risk, and gender on sexual decision making. J Stud Alcohol. 2006;67(1):113–21.
Kruse MI, Fromme K. Influence of physical attractiveness and alcohol on men’s perceptions of potential sexual partners and sexual behavior intentions. Exp Clin Psychopharmacol. 2005;13(2):146–56.
MacDonald TK, Fong GT, Zanna MP, Martineau AM. Alcohol myopia and condom use: can alcohol intoxication be associated with more prudent behavior? J Pers Soc Psychol. 2000;78(4):605–19.
Maisto SA, Carey MP, Carey KB, Gordon CM, Schum JL. Effects of alcohol and expectancies on HIV-related risk perception and behavioral skills in heterosexual women. Exp Clin Psychopharmacol. 2004;12(4):288–97.
Shuper PA, Fisher WA. The role of sexual arousal and sexual partner characteristics in HIV + MSM’s intentions to engage in unprotected sexual intercourse. Health Psychol. 2008;27(4):445–54.
Ebel-Lam AP, MacDonald TK, Zanna MP, Fong GT. An experimental investigation of the interactive effects of alcohol and sexual arousal on intentions to have unprotected sex. Basic Appl Soc Psychol. 2009;31:226–33.
George WH, Davis KC, Norris J, et al. Alcohol and erectile response: the effects of high dosage in the context of demands to maximize sexual arousal. Exp Clin Psychopharmacol. 2006;14(4):461–70.
Jarvis BG. MediaLab. New York: Empirisoft Corporation [computer program]. Version 2010.3. 2010.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Care. World Health Organization Department of Mental Health and Substance Dependence. 2001.
National Institute on Drug Abuse. Resource Guide: Screening for Drug Use in General Medical Settings. https://www.drugabuse.gov/publications/resource-guide (2012). Accessed 6 July 2015.
The Explore Team. Effects of a behavioural intervention to reduce acquisition of HIV infection among men who have sex with men: the EXPLORE randomised controlled study. Lancet. 2004;364:41–50.
Langer E. The illusion of control. J Pers Soc Psychol. 1975;32:311–28.
National Advisory Council on Alcohol Abuse and Alcoholism—Recommended Council Guidelines on Ethyl Alcohol Administration in Human Experimentation. NIAAA. http://www.niaaa.nih.gov/Resources/ResearchResources/job22.htm (2005).
Walsh JC, Mandalia S, Gazzard BG. Responses to a 1 month self-report on adherence to antiretroviral therapy are consistent with electronic data and virological treatment outcome. AIDS. 2002;16(2):269–77.
Chesney MA, Ickovics JR, Chambers DB, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG). AIDS Care. 2000;12(3):255–66.
Ross L, Lepper MR, Hubbard M. Perseverance in self-perception and social perception: biased attributional processes in the debriefing paradigm. J Pers Soc Psychol. 1975;32(5):880–92.
Box GEP, Hunter WG, Hunter JS. Statistics for experimenters—design, innovation and discovery. New York: John Wiley and Sons; 2005.
Rosenthal R, Rosnow RL, Rubin DB. Contrasts and effect sizes in behavioral research: a correlational approach. New York: Cambridge University Press; 2000.
Aneshensel CS. Theory-based data analysis for the social sciences. Thousand Oaks: Pine Forge Press; 2002.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–82.
Edwards JR, Lambert LS. Methods for integrating moderation and mediation: a general analytical framework using moderated path analysis. Psychol Methods. 2007;12(1):1–22.
Fisher JD, Fisher WA, Shuper PA. The information-motivation-behavioral skills model of HIV preventive behavior. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging theories in health promotion practice and research. 2nd ed. San Francisco: Jossey-Bass; 2009. p. 21–63.
Centers for Disease Control and Prevention. Incorporating HIV prevention into the medical care of persons living with HIV: recommendations of CDC, the Health Resources and Services Administration, the National Institutes of Health, and the HIV Medicine Association of the Infectious Disease Society of America. MMWR. 2003;52(RR-12):1–24.
Janssen RS, Holtgrave DR, Valdiserri RO, Shepherd M, Gayle HD, De Cock KM. The serostatus approach to fighting the HIV epidemic: prevention strategies for infected individuals. Am J Public Health. 2001;91(7):1019–24.
Galvan FH, Bing EG, Fleishman JA, et al. The prevalence of alcohol consumption and heavy drinking among people with HIV in the United States: results from the HIV Cost and Services Utilization Study. J Stud Alcohol. 2002;63(2):179–86.
Cook RL, Sereika SM, Hunt SC, Woodward WC, Erlen JA, Conigliaro J. Problem drinking and medication adherence among persons with HIV infection. J Gen Intern Med. 2001;16(2):83–8.
Kaner EF, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2007;(2):CD004148.
Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–74.
Fisher WA, Fisher JD, Shuper P. Social psychology and the fight against AIDS: an information-motivation-behavioral skills model for the prediction and promotion of health behavior change. In: Olson J, Zanna M, editors. Elsevier; 2014.
Drumright LN, Colfax GN. HIV risk and prevention for non-injection substance users. In: Mayer KH, Pizer H, editors. HIV prevention: a comprehensive approach. Burlington: Academic Press; 2009. p. 340–75.
Kalichman SC, Greenberg J, Abel GG. HIV-seropositive men who engage in high-risk sexual behaviour: psychological characteristics and implications for prevention. AIDS Care. 1997;9(4):441–50.
Dal Cin S, MacDonald TK, Fong GT, Zanna MP, Elton-Marshall TE. Remembering the message: the use of a reminder cue to increase condom use following a safer sex intervention. Health Psychol. 2006;25(3):438.
Acknowledgments
Funding for this work was provided by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (4R21AA020236-02, PI: Shuper). We would like to thank the patients and staff at the Maple Leaf Medical Clinic for their collaboration and support. We would also like to thank Dr. Peter Monti, Ioana-Smarandita Arbone, Sulagna Sarker, Christina Schell, Shayna Skakoon-Sparling, and Rose Wang for their contributions to this project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shuper, P.A., Joharchi, N. & Rehm, J. Protocol for a Controlled Experiment to Identify the Causal Role of Acute Alcohol Consumption in Condomless Sex among HIV-Positive MSM: Study Procedures, Ethical Considerations, and Implications for HIV Prevention. AIDS Behav 20 (Suppl 1), 173–184 (2016). https://doi.org/10.1007/s10461-015-1128-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1128-5