Summary
Differentiating between sarcoidosis as an autonomous disease and sarcoid-like reactions requires considerable efforts. The epithelioid cell granuloma is not equivalent to sarcoidosis because it may be identified in a number of infectious and noninfectious disorders, including neoplastic diseases. At the current state of knowledge, accurate distinction between different causes of epithelioid cell granulomas is in many cases not possible. Despite being characteristic of sarcoidosis and sarcoid-like reactions, the epithelioid cell granuloma is not their synonym, as numerous other causes can give rise to such a type of granulomatous infiltrate. Its etiology should be sought through careful additional investigations, including the genetic signature of both conditions.
Sarcoid-like reactions may be grouped generally into several subtypes. The differentiation between each one of them requires a certain combination of diagnostic tests. The major objective of these tests is to exclude or to prove the presence of an infectious, tumoral, or immunogenic antigen on the one hand, and to characterize the genetic profile of the affected patients (for example, sarcoidosis-specific genes) on the other. Only thus may one accurately differentiate between the two pathologic conditions described earlier in the abstract.
The clear differentiation between sarcoidosis as a separate disease and sarcoid-like pathologies leads to the more precise clarification of the final diagnosis, which may in turn allow for a more appropriate therapy and improvement in the quality of life of the patients. Equating sarcoid granulomas with sarcoidosis can lead to serious consequences in a number of patients. Sadly enough, after scrutinizing the current available data in the world literature, one cannot find criteria to allow such distinction in a high percentage of the investigated cases.
This critical review provides a completely new pathogenetic and diagnostic algorithm, helping in the differentiation between the disease sarcoidosis and the sarcoid-like pathologies with different etiology. An update on the inclusion criteria from the ATS/ERS/WASOG (American Thoracic Society/European Respiratory Society/World Association of Sarcoidosis and other Granulomatous Disorders) statement (which at the current state of knowledge seems to be ineffective) for the diagnosis of sarcoidosis is also suggested.
In conclusion, molecular mimicry may be seen as the main pathogenic generator not only of sarcoidosis but also of sarcoid-like reactions. A completely new and exact definition of the notion of or the sarcoidosis disease itself will be possible only after
-
1.
defining the genetic risk for the development of sarcoidosis as an autonomous disease and supplementing the sarcoidosis consensus of ATS/ERS/WASOG from 1999 with this important information, and
-
2.
defining the notion of a sarcoid-like reaction and its subforms.
Zusammenfassung
Die Unterscheidung von Sarkoidose als eigenständiger Erkrankung und sarkoidaler Reaktion erfordert erhebliche Anstrengungen. Der Nachweis epitheloidzelliger Granulome ist nicht der Diagnose einer Sarkoidose gleichzusetzen, da diese bei einer Vielzahl von infektiösen und nicht infektiösen Erkrankungen, einschließlich der Tumore, auftreten können. Mit unserem derzeitigen Wissensstand ist die exakte Differenzierung bezüglich ihrer Ursachen aus nicht immer möglich. Obwohl die epitheloidzelligen Granulome charakteristisch für Sarkoidose und sarkoidale Reaktionen sind, können zahlreiche andere Ursachen für ihre Entstehung verantwortlich sein. Ihre Ätiologie sollte durch sorgfältige zusätzliche Untersuchungen einschließlich der genetischen Signatur beider Erkrankungen geklärt werden.
Sarkoidale Reaktionen können in verschiedene Subtypen klassifiziert werden. Deren Unterscheidung bedarf einer gewissen Kombination der Untersuchungsverfahren. Hauptanliegen dieser Untersuchungen ist die Verifizierung bzw. der Ausschluß infektiöser, tumoraler oder immunogener Antigene einerseits und die Beschreibung des genetischen Profils des betroffenen Patienten (z.B. sarkoidose-spezifische Gene) andererseits. Nur hierdurch wird eine exakte Differenzierung beider Pathologien (Sarkoidose, sarkoidal) möglich.
Die eindeutige Differenzierung von Sarkoidose und sarkoidaler Reaktion als verschiedene Erkrankungen erlaubt eine präzisere Diagnose, eine zielgerichtetere Behandlung und die Verbesserung der Lebensqualität der Patienten. Umgekehrt kann die Nichtbeachtung dieses Grundsatzes zu ernsten Konsequenzen für betroffene Patienten führen. Leider ist bietet die wissenschaftliche Weltliteratur bislang keine Kriterien, die eine klare Unterscheidung beider Pathologien bei einem hohen Prozentsatz der Patienten erlaubt.
Diese kritische Übersicht entwickelt einen komplett neuen pathogenetischen und diagnostischen Algorithmus zur Differenzierung von Sarkoidose und sarkoidaler Reaktion verschiedener Ätiologien. Ein Update der Einschlußkriterien der ATS/ERS/WASOG (American Thoracic Society/European Respiratory Society/World Association of Sarcoidosis and other Granulomatous Disorders) für die Sarkoidose-Diagnose wird ebenfalls vorgeschlagen.
Schlußfolgerungen: Molekulare Mimikry kann als wesentlicher Motor nicht allein für die Sarkoidose, sondern auch die sarkoidale Reaktion angesehen werden. Eine komplett neue und exakte Definition der Diagnose Sarkoidose wird nur dann möglich werden, wenn:
-
1.
Das genetische Risiko der Sarkoidoseentwicklung bestimmt und der Konsensus der ATS/ERS/WASOG von 1999 implementiert wird.
-
2.
Die sarkoidale Reaktion und ihre Subtypen bestimmt werden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sarcoidosis or a sarcoid-like reaction
Currently, a number of authors hold the belief that sarcoidosis may be viewed as a kind of paraneoplastic disease, morphologically characterized by the manifestation of epithelioid cell granulomas of variable location [1–3]. This view has been the major cause of many problems related to the interpretation of the available data in current-day literature: are we discussing sarcoidosis or a sarcoid-like reaction? The most common modern understanding is that in predisposed subjects, sarcoidosis may be induced by a cross-reaction to de novo-appearing tumor antigens or immunogenes, which are, as a rule, noninfectious structures or proteins with diverse nature (bacterial, viral antigens, and other inorganic components) in the tissue [3, 4]. There are no investigations that may serve to indicate the degree to which a certain genetically determined form of sarcoidosis—as an autonomous disease—is associated with various types of tumors. In most cases, the authors associate epithelioid cell granuloma with sarcoidosis [5, 6]. Data related to the identification of the respective tumor antigens in sarcoid granulomas in patients with a concomitant neoplasm are also hard to come by [7]. Some authors describe such cases and make us think whether in many instances, the conditions identified as sarcoidosis are indeed sarcoidosis as an autonomous disease or, instead, a sarcoid-like reaction [7–10].
The percentage of cases described in the literature that may relate to the generation of a sarcoid-like reaction to tumor microantigens in the tissue is also unclear [7, 9, 10]. As there are no specific tests or algorithms to confirm these hypotheses or assertions, skepticism is appropriate. The major question is as follows: sarcoidosis or sarcoid-like reactions? Such roundabout ways, or bearing points, should have two major objectives based on the well-known fact that, as a rule, sarcoidosis is a noncontagious disease [11]. Secondly, the patients suffering from sarcoidosis should be genetically predisposed, and this predisposition should be proved [12, 13]. Even the genetic predisposition criteria have been not added to the sarcoidosis inclusion criteria. In itself, such verification requires the implementation of certain new diagnostic panels containing a sufficient amount of data, the subsequent interpretation of which should lean the scales in favor of one or the other of these claims [11–15].
Subtypes of sarcoid-like reactions and panels for the identification and correct assessment of the reaction and the type of the disease
-
1.
The sarcoid-like reaction can be the result of a local reaction to certain infectious antigens (leprosy, certain forms of leishmaniasis, deep fungal infections, tertiary syphilis, atypical (nontuberculous) mycobacterial infections, etc.) [16, 17]. Practically, in such cases, one observes a sarcoidal granulomatous infiltrate to a given specific infectious antigen [16, 17].
-
2.
However, sarcoid-like reactions are also known to occur in association with antigens of noninfectious nature (tumor antigens, inorganic substances). The differentiation of this subtype of sarcoid reactions is possible only when based on an additional genetic analysis and more specifically in the course of proving the presence—or absence—of disease-specific genes for sarcoidosis, for example [11–13]. With this subtype of reactions, the problems relating to the interpretation of the reaction’s pathological mechanisms spring from the fact that these key pathogenic antigens may be identified in the sarcoidal granulomas, but they may also be identified in sarcoid-like reactions [3].
-
Thinking of the future, it might be of significant benefit to categorize genes that may serve to characterize the sarcoid-like reactions, or to establish the degree to which genetic polymorphisms described in the literature conform to a case of sarcoidosis as an autonomous disease or are more characteristic of the sarcoid-like reactions.
-
3.
The third subtype of sarcoid-like reaction may be observed in association with immunogenic but noninfectious antigens, possibly relating to an infectious disease suffered in the past or a secondary contamination or incorporation of such antigens in the tissue (bacterial, viral antigens in the tissue proven by, for example, polymerase chain reaction (PCR) or immunochistochemistry) [6].
-
Regarding this group of patients, it is highly recommendable or obligatory to try to apply or establish genetic maps for the exclusion of disease-specific genes for sarcoidosis [11–13], and they are probably the only possible way to differentiate sarcoidosis as an autonomous disease [11–13]. This type of sarcoid-like reaction should be the most difficult to separate because it demands a number of additional tests for the identification of the respective bacterial, viral, and parasitic antigens.
Differentiating the diagnosis of sarcoidosis from a sarcoid-like reaction, within the framework of clinical practice, is often very problematic, particularly when one is faced with the absence of additional data supplied by certain diagnostic tests, namely: (1) (see Table 1), which is aimed at identifying a sarcoid-like reaction—cultures, immunohistochemical staining, and PCR in the tissue—the major objective of which is the identification of a given pathogenic agent, the force of its infectious effects, and its immunogenic features [6, 18, 19]; and (2) (see Table 2)—serological and genetic tests aimed at proving the presence of sarcoidosis as an autonomous disease (for example, angiotensin-converting enzyme, HLA/non-HLA alleles, disease-specific genes for sarcoidosis) [11–13, 19].
In addition, (see Table 3) might (1) pursue the objective of identifying tumor microantigens in sarcoid granulomas in the case of a known associated tumor, or (2) attempt to identify a certain type of tumor antigens in the case of a neoplastic disease that is unknown by the time of the diagnosis of the granulomatous reaction [7, 8].
Data in the literature on the aforementioned issues are frequently contradictory [6]. For example, the question remains as to whether the proven presence of spirochetes in Western Austria in cases diagnosed as sarcoidosis actually represented sarcoidosis or, alternatively, a sarcoid-like reaction to certain bacterial antigens that have been able to retain their immunogenic properties [6]. Given the absence of genetic analysis in these cases, it is unavoidable that this question will remain without an answer [11–13].
After careful analysis of the greater part of the single cases and case series of sarcoidosis published during the past 15 years, one comes to the conclusion that the differentiation between sarcoidosis as an autonomous disease and sarcoid-like reactions frequently has not been accurately performed [20, 21]. In the publications from the past several years, the claims raised by many colleges are becoming more differentiated and accurate [22–25]. Cases are no longer described as sarcoidosis associated with a given type of tumor but rather as a sarcoid-like reaction associated with a neoplasm [25–33]. The need for a genetic analysis as a means to define the individual susceptibility to the development of sarcoidosis in such patients is of particular importance and attracts a growing number of adherents [11–13]. It would be highly beneficial if future research be directed toward the characterization of a new genetic profile, namely that of the patients with sarcoid-like reactions and sarcoidosis.
The implementation of certain additional standard diagnostic panels could be an important step forward in solving the enigma presented by these cases. Proving the existence of disease-specific genes for sarcoidosis in the respective geographical regions could support a more accurate differentiation between sarcoidosis and sarcoid-like reactions.
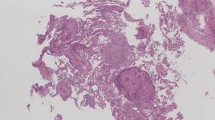
Epithelioid cell granuloma: algorithm for clinical behavior
The role of certain infectious antigens in the pathogenesis of sarcoidosis has been the subject of spirited debates. A number of authors believe that some infectious antigens—like mycobacteria, propionibacteria, human herpes virus 8, hepatitis viruses, and others—are capable of provoking sarcoidosis in genetically predisposed individuals [34–38]. Some perplexing literary data, for example, offer information about a conveyable antigen, capable of causing sarcoidosis after transplantation [39–40]. It is highly unlikely that this may include patients with similar predisposition to the development of sarcoidosis. In this case, it would be more appropriate to speak of a sarcoid-like reaction with an obscure genesis (Figs. 1, 2, and 3).
As far as sarcoidosis and the sarcoid-like reaction is concerned, the role of each separate pathogenetic inducer could be clarified thanks to additional diagnostic steps taken to reveal whether the case at hand is (1) an infectious type of antigen or only an (2) immunogenic antigen that lacks infectiousness. In case the results obtained prove to be negative (both for infectious and noninfectious, but still an immunogenic agent), one should think firstly of the epithelioid cell granuloma resulting from cross-reactivity to possible tumor macro- or microantigens or some other inorganic compounds. In other words, the entire screening of the patients as well as immunohistochemical staining in lesional tissue that may contribute to establish the presence or absence of infectious or tumoral microantigens becomes mandatory.
It follows, therefore, that it would be particularly difficult to differentiate between a case of sarcoidosis associated with a neoplasm and a sarcoid-like reaction within the framework of the tumoral disease itself. The latter hypothesis appears to be logically better placed, at least in the absence of available data supporting a genetic background of sarcoidosis.
Despite the fact that the available literature does not present data on more than 60 % of the cases—information that could serve to differentiate between the two possibilities described earlier in the text—all of them have been described more like a sarcoidosis disease potentiated by the effects of immune suppression therapy [41, 42]. Although the etiology of sarcoidosis remains unknown, recent molecular, genetic, and immunologic studies strengthen the association of sarcoidosis with infectious antigens [42]. Currently, the most strongly associated agents include Propionibacterium and Mycobacterium species [42]. Independent studies report the presence of microbial nucleic acids and proteins within sarcoidosis specimens [42]. Unfortunately, the genetic background of the patients from these investigations has not been added to the internationally accepted inclusion criteria for the diagnosis of sarcoidosis.
Of considerable interest has been a recent publication of a randomized, placebo-controlled research, which shows an improvement in the clinical condition of patients with a chronic form of sarcoidosis after the implementation of antimycobacterial therapy [43]. The question remains, however, as to whether the 30 patients observed have shown instead a sarcoid-like reaction, and whether their genetic background was known prior to administering the treatment. Given the absence of information on (1) sarcoidosis-specific genes, (2) immunohistochemical staining in the tissue to detect the presence of tumor microantigens, and (3) complementary diagnostic tests in lesional tissue aimed at identifying infectious or noninfectious, but immunogenic, antigens, one should at least consider the possibility of a sarcoid-like reaction [42].
The work of other researchers has led to similar results in that they have found data on mycobacterial antigens in cases that have been definitely identified as sarcoidosis [44]. Results from that study led to the conclusion that malignancy-associated “pseudosarcoid” granulomas do not differ antigenically from genuine sarcoid granulomas [44].
New hopes for the genetic analysis: disease-specific genes for sarcoidosis? Tuberculosis vs. sarcoidosis vs. sarcoid-like reactions
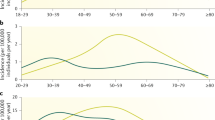
To a certain extent, genetic samples may be able to classify one or another disease or one or another type of reaction helping, in this way, to better clarify a given diagnosis or the pathogenetic background [11]. A relatively recent investigation has revealed certain similarities in the genetic profiles of patients with sarcoidosis and tuberculosis (TB), which is, indirectly, an alarming signal with respect to the etiopathogenesis of sarcoidosis and the possible connection to the sarcoid-like reactions [11].
To a certain extent, this publication comes as a direct support to the thesis of immunogenic, noninfectious antigens as possible generators of molecular mimicry, triggering the clinical manifestations of sarcoidosis or sarcoid-like reactions [3, 4, 11].
A further step in this direction could be the comparison of genetic sarcoidosis samples with those of sarcoid-like reactions and healthy individuals. In this way, genes could be grouped and categorized according to their association with a given type of disease or reaction [11].
It will be of importance to define the variants common to both diseases (as currently described for sarcoidosis and TB) [11], and also the ones specific for sarcoidosis and for sarcoid-like reactions.
There are prerequisites for data to be entered in the Kyoto Encyclopedia of Genes and Genomes (KEGG) database, which will be of considerable help in the process of not only identifying the susceptibility of certain groups of patients to sarcoidosis (the genes in the KEGG pathway, KEGG ID hsa05152; i.e., genes with established significant relation to TB), but also trying to identify the genetic signature of patients with sarcoid-like reactions.
The objective of these investigations is to identify disease-specific genes [11]. For the time being, the set of genes specific for sarcoidosis includes the overexpression or adjustment of the gene matrix metalloproteinase 14 (MMP14) and a decreased expression of genes cluster of differentiation (CD)247, CD8A, and CD8B, which may reflect abnormally low T-cell counts in a substantial number of SARC patients as described previously [11].
SARC patients also displayed a significant number of unique features, with the most striking being the increased expression of MMP14. This report links MMP14 to SARC, which also is distinct from its expression in TB and in healthy individuals.
The next important step, however, is to perform additional investigations regarding the degree to which MMP14 is associated to or expressed in patients with sarcoid-like reactions.
The similarity between the expressional samples of the active form of pulmonary sarcoidosis and TB, for example, is of considerable importance when defining the possible common pathophysiological pathways [45, 46]. A comparison of these samples, thanks to the KEGG TB pathway, points to a very similar expression of certain genes in patients with active lung sarcoidosis and TB [45, 46].
At this point, one may wonder whether sarcoidosis indeed exists as an autonomous disease. Or are we simply observing sarcoid-like reactions to diverse immunogenic antigens?
Can one establish the existence of a common pathogenic pathway for an infectious disease like pulmonary TB conforming to the sarcoidosis pathway, which—by definition—should be a noninfectious, immunologic disease?
Do genes exist that may characterize not only the type of disease but also the type of reaction?
The considerable overlap of differentially expressed genes between TB and SARC within these published TB-related signatures, as shown by several authors, indicates that these signatures do not reliably distinguish between the two diseases [11, 45, 46]. At this particular point, we may ask ourselves once again how two diseases with different etiopathogenesis (sarcoidosis and TB) can demonstrate a similar genetic profile?
Should we not consider the possibility that sarcoidosis is a reaction pattern to a variety of immunogenic stimuli rather than a single autonomous disease?
Antigen mimicry and its role in sarcoidosis and in a proportion of patients suffering from sarcoidal granulomas
One result from this type of cross-reactivity, which is known in the literature as antigenic mimicry, is the appearance of an immunological reaction directed to similar antigenic structures [3]. Until disease-specific genes for sarcoidosis are not identified and added to the inclusion diagnostic criteria, this process should be probably better characterized as a sarcoid-like reaction rather than sarcoidosis [10, 13, 15]. The fact that there are isolated publications describing certain tumor microantigens in sarcoid granulomas should require that, in addition to tests aimed at identifying infectious or other immunogenic agents, one should also be able to identify the presence of common tumor antigens in the tissue containing sarcoidal granulomas (Tables 1 and 3) [7, 16, 17, 47, 48].
Sarcoid-like diseases could be probably also due to the similarity of certain amino acid sequences between the proteins of the tumor and the host but it may also be due to the so-called momentary imitation followed by an immunological reaction, as recently described in sarcoidosis [49]. In other words, it can manifest itself clinically and be established histopathologically without the presence of a similarity in the sequence of the amino acids of the antigen and the respective tissue equivalent [49].
“Momentary imitation” is a condition that may be additionally influenced, or potentiated, by various hydrophilic or hydrophobic interactions, the electrostatic charge of the molecules at a certain point in time, or by the temporary activation of the immune system [49]. The basic theory, which is becoming increasingly accepted, is that the appearance of a sarcoid-like reaction in association with certain tumors appears to be more probable than sarcoidosis as an individual autonomous disease associated with cancer [24–33]. This is especially true if no data are available to confirm the genetic predisposition of a given patient to sarcoidosis [12-15] or to exclude the role of certain infectious and/or immunogenic antigens as generators of one of the two conditions. Due to these facts, for the time being the management of these two conditions (sarcoidosis and sarcoid-like reactions) is rather dependent on each clinician, and there may be significant differences according to different practices in various geographical areas, and even between different institutions in the same region.
In clinical practice, the following scenarios seem possible, according to the different availability of diagnostic tests, including genetic investigation:
-
1.
Sarcoidosis with proven immunogenic but, as a rule, in the current moment, noninfectious antigens (bacterial, viral, parasitic) plus a proven genetic background (according to the latest view on the pathogenesis) [3, 11]).
-
2.
Sarcoidosis with no available data for immunogenic noninfectious (bacterial, viral, parasitic) antigens after performing the appropriate diagnostic tests; with or without data for tumoral disease; presence of a genetic predisposition (disease-specific sarcoidosis genes) [11–13, 15].
-
3.
Sarcoidal granulomatous reaction associated with an infectious agent, confirmed by ancillary methods; no need for further testing, namely genetic predisposition for sarcoidosis [4, 11].
-
4.
Sarcoid-type reaction with no evidence of an infectious trigger; possible reaction to tumor antigens or inorganic material; negative genetic testing for sarcoidosis.
-
5.
Sarcoid-type reaction with available data for a secondary noninfectious (primary infectious bacterial, viral or parasitic components, or later incorporation from immunogenic noninfectious components) but immunogenic antigens; negative genetic testing for sarcoidosis.
-
6.
Sarcoid-type reaction with available data for primary noninfectious but immunogenic antigens; negative genetic testing for sarcoidosis.
This would demand the performance of a complete set of tests, the objective of which would be to identify the pathogenesis of a given epithelioid cell granuloma:
-
bacterial and fungal cultures, histopathological examination, immunohistochemistry, molecular biology techniques, and PCR;
-
genetic analysis with the aim of excluding the presence of disease-specific genes of sarcoidosis [11];
-
identification of tumor microantigens in the tissue and in the human body.
Toll-like receptors (TLRs) are major components of the innate immune system and microbial sensors of the human body. Ten different TLRs have been identified and mapped to seven chromosomal segments.
Gene polymorphism of respiratory epithelial cells represents a defense mechanism in innate immunology. The TLRs are involved in this immune response. Inflammatory cytokines can upregulate TLR expression. In cell culture, both tumor necrosis factor alpha (TNF-α) and interferon-gamma (IFN-γ) enhance the expression of TLR2 by respiratory epithelial cells. Dexamethasone synergistically increase TLR2 expression in combination with either TNF-α or IFN-γ [83]. This results in induction of cytokines such as interleukin (IL)-6 and -8, and beta-defensin in response to peptidoglycan stimulation [83]. Another group of microbial sensors is the family of nucleotide-binding domain, leucine-rich repeat containing receptors (Nod-like receptors or NLR). They also trigger immune responses to bacterial peptidoglycan. These molecules stimulate proinflammatory cytokines and antimicrobial peptides.
Sarcoidosis is considered an altered immune response to a yet-unidentified microbial stimulus. Gene polymorphism and mutations of TLR may be implicated on the pathogenesis sarcoidosis. The genetic background can vary between different populations, creating more complexity.
TLR2 polymorphism has been studied in 419 sarcoidosis patients and 196 healthy controls from The Netherlands [84]. The prevalence of AA genotype at promoter location 16934 was significantly higher in chronic vs. acute or self-limiting disease: 34.5 vs. 15.9 % [84]. Further analysis, however, suggested that TLR2 polymorphism might play a role in only a small group of patients [84]. This could not be confirmed in a Japanese study in 257 sarcoidosis patients and 193 controls [85].
TLR2 might play a role in the granulomatous inflammatory reaction observed in sarcoidosis. Serum amyloid A could be localized to macrophages and to giant cells in sarcoid granulomas and correlated to CD3-positive T lymphocytes. The effect of serum amyloid A on TLR2 expression was investigated in vitro using transformed human cell lines and bronchoalveolar lavage (BAL) cells from sarcoidosis patients. Serum amyloid A activated nuclear factor κB in those cells expressing TLR2. As a consequence of that, pro-inflammatory cytokines such as TNF-α, IL-10, and IL-18 were stimulated in cells from sarcoidosis patients. Cytokine secretion could be inhibited by blocking TLR2. These data suggest that serum amyloid A is involved in the granulomatous inflammatory reaction in sarcoidosis [86]. Studying alveolar macrophages from sarcoidosis patients, Wikén et al. [87] observed a reduced expression of TLR2 mRNA compared to controls.
TLR1, TLR6, and TLR10 act as co-receptors of TLR2. They are located on chromosome 6 in a common gene cluster. The expression of the common haplotype in the gene cluster TLR10-TLR1-TLR6 increases the risk of chronicity in patients with sarcoidosis [88].
In a study involving Greek patients, both G908R mutation of the CARD15/NOD2 gene as well as T allele and TT genotype of the CD14 promoter were associated with increased susceptibility for pulmonary sarcoidosis [89]. TLR4 and CD14 are essential receptors for the recognition of lipopolysaccharides of gram-negative bacteria.
In a study from Germany, Asp299Gly and Thr399Ile polymorphisms of TLR4 gene were investigated. Among 141 sarcoidosis patients, the prevalence of Asp299Gly and Thr399Ile mutant allele was 15.6 %. These mutations would lead to a change in the extracellular matrix domain of TLR4 and possibly impair lipopolysaccharide recognition. In the control group (n = 141), the prevalence was significantly lower at 5.7 %. Patients with chronic pulmonary sarcoidosis showed a highly significant association to TLR4 gene polymorphism [90].
In another German study analyzing linkage of TLR using closely flanking microsatellite markers in 83 families, a significant linkage was found between TLR4 and sarcoidosis. No other known gene locus disclosed such an association. The TLR4 association was further confirmed by a subsequent analysis of another 1,203 sarcoidosis patients. The study did not confirm Asp299Gly and Thr399Ile as susceptibility markers [91].
This might be involved in the chronic antigenic stimulus supposed to play a pivotal role in sarcoidosis pathogenesis.
Among 200 Dutch patients suffering from sarcoidosis, a statistically significant difference in mutant Asp299Gly allele prevalence was not confirmed [92].
A Greek study analyzing 109 sarcoidosis patients and 209 controls could not confirm increased susceptibility for sarcoidosis due to Asp299Gly and Thr399Ile polymorphisms either [93]. The same was true for a Japanese investigation in sarcoidosis-related uveitis [94]. This argues clearly in favor of a heterogeneous genetic background in sarcoidosis.
TLR9 recognizes bacterial CpG-DNA motifs. Pabst et al. [95] found a significantly higher prevalence of the C-allele of T1237C single-nucleotide polymorphism in patients with chronic sarcoidosis.
TLR9 genetics were not different between sarcoidosis patients and controls in a study from The Netherlands. On stimulation with TLR9 agonists, however, sarcoidosis patients produced not only less IFN-γ, but also more IL-23 [96].
An upregulated TLR9 and TLR7 expression was observed in a Greek study using BAL cells [97].
Mutations in Nod1 and Nod2 have been identified in early-onset sarcoidosis among other granulomatous disorders like Crohn’s disease [98].
Using blood mononuclear cells, expression of TLR2 and TLR4 was significantly higher in sarcoidosis patients compared with controls. Combined stimulation of TLR2 and Nod2 by specific ligands resulted in a 13-fold increase of IL-1β secretion in sarcoidosis patients. In healthy controls, IL-10 was synergistically induced [99].
Recognition of bacterial moieties by both TLR and NLR evokes a sequential activation of mitogen-activated protein kinases (MAPKs). Stimulation of BAL cells from sarcoidosis with either TLR4 or Nod1 failed to induce MAPK phosphatase 1. Enhanced p38 signaling in response to microbial stimuli was observed that could be due to an abnormal MAPK pathway [100].
Nicotine treatment restored peripheral immune responsiveness to TLR2 and TLR9 in patients with active pulmonary sarcoidosis. This has led to an immune phenotype closely resembling asymptomatic patients [101].
What about sarcoid-like reactions?
There is an increasing number of reports of sarcoid-like reactions to medical drugs, from chemotherapy agents to biologicals, malignancies, and chronic infections. Paradoxically, even TNF-α inhibitors may cause sarcoid-like reactions [25, 102, 103]. The role of TLRs and NLRs in these reactions has to be studied.
The characteristic abnormalities in innate immune mechanisms might provide a molecular base for differentiation.
In conclusion, a number of studies pointed to the occurrence of either genetic or functional abnormalities of selected TLRS and related NLRs. Available data argue more for a disease-modifying influence of TLRs and NLRs than a causative relationship to (pulmonary) sarcoidosis. There is a remarkable heterogeneity on a genetic background of different populations. First therapeutic approaches need confirmation. Data on cutaneous sarcoidosis and sarcoid-like reactions are completely missing.
It is exactly these facts that bring to the necessity of a clear and exact definition—subsequently the differentiation—between these two conditions (sarcoidosis and sarcoid-like reactions) and their subforms.
The similar histopathological findings and the heterogeneous location of the granulomatous infiltrates in sarcoidosis and sarcoidal granulomas with a different genesis raise the possibility of a unified immunological mechanism, probably directed at various antigenic determinants.
When the aforementioned is combined with certain diagnostic algorithms, the diagnosis could weigh either in favor of a sarcoid-like reaction or of sarcoidosis as an autonomous disease. In the absence of additional data, or the impossibility of performing a given set of tests (Table 1–3), it would be more appropriate—initially at least—for one to speak of a sarcoid-like reaction with a currently undefined genesis.
Conclusions
-
1.
The sarcoid-like reaction is not the equivalent of a sarcoidosis.
-
2.
Sarcoidosis, the sarcoid-like reaction, and their variable genetically based clinical manifestations may, in many cases, be based on the molecular mimicry phenomenon. Molecular mimicry seems to be one of the main pathogenetic triggers in autoimmune dermatologic diseases, as recently described by some authors [104].
-
3.
An update of the inclusion criteria for sarcoidosis from 1999 is strongly recommended.
-
4.
The additional characterization of the genetic risk for the sarcoidosis disease and its integration as a standard genetic panel will serve as a decisive support for the placing of the following clinical management.
-
5.
Sarcoid-like reactions have to be analyzed and classified additionally.
References
Alexandrescu DT, Riordan NH, Ichim TE, Kauffman CL, Kabigting F, Dutton CT, Dasanu CA. On the missing link between inflammation and cancer. Dermatol Online J. 2011 Jan 15;17(1):10.
Alexandrescu DT, Kauffman CL, Ichim TE, Riordan NH, Kabigting F, Dasanu CA. Cutaneous sarcoidosis and malignancy: an association between sarcoidosis with skin manifestations and systemic neoplasia. Dermatol Online J. 2011 Jan 15;17(1):2.
Tchernev G, Ananiev J, Cardoso JC, Wollina U, Verma SB, Patterson JW, Dourmishev LA, Tronnier M, Okamoto H, Mizuno K, Kanazawa N, Gulubova M, Manolova I, Salaro C. Sarcoidosis and molecular mimicry—important etiopathogenetic aspects: current state and future directions. Wien Klin Wochenschr. 2012 Apr;124(7–8):227–38.
Ali MM, Atwan AA, Gonzalez ML. Cutaneous sarcoidosis: updates in the pathogenesis. J Eur Acad Dermatol Venereol. 2010 Jul;24(7):747–55.
Adam A, Thomas L, Bories N, Zaharia D, Balme B, Freymond N, Dalle S. Sarcoidosis associated with vemurafenib. Br J Dermatol. 2013 Jul;169(1):206–8.
Derler AM, Eisendle K, Baltaci M, Obermoser G, Zelger B. High prevalence of ‘Borrelia-like’ organisms in skin biopsies of sarcoidosis patients from Western Austria. J Cutan Pathol. 2009 Dec;36(12):1262–8.
Kestlmeier R, Busch R, Fellbaum C, Boettcher K, Reich U, Siewert JR, Höfler H. Incidence and prognostic significance of epithelioid cell reactions and microcarcinoses in regional lymph nodes in stomach carcinoma. Pathologe. 1997 Mar;18(2):124–30.
Tana C, Giamberardino MA, Di Gioacchino M, Mezzetti A, Schiavone C. Immunopathogenesis of sarcoidosis and risk of malignancy: a lost truth? Int J Immunopathol Pharmacol. 2013 Apr-Jun;26(2):305–13.
Tjan-Heijnen VC, Vlasveld LT, Pernet FP, Pauwels P, De Mulder PH. Coincidence of seminoma and sarcoidosis: a myth or fact? Ann Oncol. 1998 Mar;9(3):321–5.
Pavic M, Debourdeau P, Vacelet V, Rousset H. [Sarcoidosis and sarcoid reactions in cancer]. Rev Med Interne. 2008 Jan;29(1):39–45.
Maertzdorf J, Weiner J 3rd, Mollenkopf HJ; TBornotTB Network, Bauer T, Prasse A, Müller-Quernheim J, Kaufmann SH. Common patterns and disease-related signatures in tuberculosis and sarcoidosis. Proc Natl Acad Sci U S A. 2012 May 15;109(20):7853–8.
Spagnolo P, Schwartz DA. Genetic predisposition to sarcoidosis: another brick in the wall. Eur Respir J. 2013 Apr;41(4):778–80.
Spagnolo P, Grunewald J. Recent advances in the genetics of sarcoidosis. J Med Genet. 2013 May;50(5):290–7.
Martin WJ 2nd, Iannuzzi MC, Gail DB, Peavy HH. Future directions in sarcoidosis research: summary of an NHLBI working group. Am J Respir Crit Care Med. 2004 Sep 1;170(5):567–71.
Spagnolo P, Luppi F, Roversi P, Cerri S, Fabbri LM, Richeldi L. Sarcoidosis: challenging diagnostic aspects of an old disease. Am J Med. 2012 Feb;125(2):118–25.
Böer A, Blödorn-Schlicht N, Wiebels D, Steinkraus V, Falk TM. Unusual histopathological features of cutaneous leishmaniasis identified by polymerase chain reaction specific for Leishmania on paraffin-embedded skin biopsies. Br J Dermatol. 2006 Oct;155(4):815–9.
Nascimento CR, Delanina WF, Soares CT. Paracoccidioidomycosis: sarcoid-like form in childhood. An Bras Dermatol. 2012 May-Jun;87(3):486–7.
Tchernev G, Patterson JW, Nenoff P, Horn LC. Sarcoidosis of the skin—a dermatological puzzle: important differential diagnostic aspects and guidelines for clinical and histopathological recognition. J Eur Acad Dermatol Venereol. 2010 Feb;24(2):125–37.
Tchernev G. Cutaneous sarcoidosis: the “great imitator”: etiopathogenesis, morphology, differential diagnosis, and clinical management. Am J Clin Dermatol. 2006;7(6):375–82.
Marak CP, Alappan N, Chopra A, Dorokhova O, Sinha S, Guddati AK. Uterine sarcoidosis: a rare extrapulmonary site of sarcoidosis. Case Rep Rheumatol. 2013. Epub 2013 May 20.
Béchade D, Roubaud G, Garbay D, Soubeyran I, Hé S, Cazeau AL, Desjardin M, Fonck M. Mediastinal sarcoidosis in an oncologic context: role of endoscopic ultrasound-guided fine needle aspiration. Rev Med Interne. 2013 Jun 4. Epub ahead of print.
Kurata A, Takayama N, Terado Y, Hirano K, Yokoyamda K, Fujioka Y. Sarcoidal granulomas in the spleen associated with multiple carcinomas. Sarcoidosis Vasc Diffuse Lung Dis. 2010 Jul;27(2):153–9.
Cornejo KM, Lum CA, Izumi AK. A cutaneous interstitial granulomatous dermatitis-like eruption arising in myelodysplasia with leukemic progression. Am J Dermatopathol. 2013 Apr;35(2):e26–9.
Davanageri RS, Bannur HB, Mastiholimath RD, Patil PV, Patil SY, Suranagi VV. Germ cell tumor of ovary with plenty of sarcoid like granulomas: a diagnosis on fine needle aspiration cytology. J Cytol. 2012 Jul;29(3):211–2.
Craun JB, Banks KP, Clemenshaw MN, Moren RW. Sarcoidlike reaction of neoplasia causing hypermetabolic thoracic adenopathy in setting of extrathoracic malignancy: report of two cases and a review of the differential diagnostic considerations. J Nucl Med Technol. 2012 Dec;40(4):231–5.
Gary-Rustom L, Declercq PL, Veresezan L, Muir JF, Cuvelier A. Mature mediastinal teratoma and sarcoid-like granulomatosis. Rev Mal Respir. 2012 Sep;29(7):898–902.
Ouellet S, Albadine R, Sabbagh R. Renal cell carcinoma associated with peritumoral sarcoid-like reaction without intratumoral granuloma. Diagn Pathol. 2012 Mar 18;7:28.
Kaikani W, Boyle H, Chatte G, de la Roche E, Errihani H, Droz JP, Fléchon A. Sarcoid-like granulomatosis and testicular germ cell tumor: the ‘Great Imitator’. Oncology. 2011;81(5–6):319–24.
Tao H, Yamamoto H, Matsuda E, Sano F, Okabe K, Sugi K. Severe bronchoconstriction due to sarcoid-like reaction to lung cancer. Asian Cardiovasc Thorac Ann. 2012 Apr;20(2):199–201.
Martella S, Lohsiriwat V, Barbalho DM, Della Vigna P, Bottiglieri L, Brambullo T, Gottardi A, Rietjens M, Petit JY. Sarcoid-like reaction in breast cancer: a long-term follow-up series of eight patients. Surg Today. 2012 Feb;42(3):259–63.
Stepień J, Domagała-Kulawik J, Chadzyński R, Kupis W, Chazan R. Sarcoidal reaction in lung adenocarcinoma in 50-years old man. Pneumonol Alergol Pol. 2010;78(4):302–5.
Tanizawa K, Tanaka E, Hashimoto S, Noma S, Kobashi Y, Okumura K, Shindo T, Taguchi Y. Paradoxical development of a sarcoid-like reaction during successful chemotherapy for seminoma. Intern Med. 2010;49(14):1423–6.
Nag S, Saraswathi TR, Sekhar G, Einstein A, Sivapathasundharam B. A rare case of sarcoid-like reaction of lymph nodes associated with squamous cell carcinoma of alveolar mucosa. Indian J Dent Res. 2009 Oct-Dec;20(4):503–5
Sharma OP, Peters RL, Ashcavai M, Balchum OJ. Australia (hepatitis) antigen in sarcoidosis. Lancet. 1970 Oct 31;2(7679):928.
Saboor SA, Johnson NM, McFadden J. Detection of mycobacterial DNA in sarcoidosis and tuberculosis with polymerase chain reaction. Lancet. 1992 Apr 25;339(8800):1012–5.
Graham DY, Markesich DC, Kalter DC, Moss MT, Hermon-Taylor J, el-Zaatari FA. Mycobacterial aetiology of sarcoidosis. Lancet. 1992 Jul 4;340(8810):52–3.
Ishige I, Usui Y, Takemura T, Eishi Y. Quantitative PCR of mycobacterial and propionibacterial DNA in lymph nodes of Japanese patients with sarcoidosis. Lancet. 1999 Jul 10;354(9173):120–3.
Di Alberti L, Piattelli A, Artese L, Favia G, Patel S, Saunders N, Porter SR, Scully CM, Ngui SL, Teo CG. Human herpesvirus 8 variants in sarcoid tissues. Lancet. 1997 Dec 6;350(9092):1655–61.
Mitchell DN, Rees RJ. A transmissible agent from sarcoid tissue. Lancet. 1969 Jul 12;2(7611):81–4.
Burke WM, Keogh A, Maloney PJ, Delprado W, Bryant DH, Spratt P. Transmission of sarcoidosis via cardiac transplantation. Lancet. 1990 Dec 22–29;336(8730):1579.
Richmond BW, Drake WP. Vitamin D, innate immunity, and sarcoidosis granulomatous inflammation: insights from mycobacterial research. Curr Opin Pulm Med. 2010 Sep;16(5):461–4.
Oswald-Richter KA, Drake WP. The etiologic role of infectious antigens in sarcoidosis pathogenesis. Semin Respir Crit Care Med. 2010 Aug;31(4):375–9.
Drake WP, Oswald-Richter K, Richmond BW, Isom J, Burke VE, Algood H, Braun N, Taylor T, Pandit KV, Aboud C, Yu C, Kaminski N, Boyd AS, King LE. Oral antimycobacterial therapy in chronic cutaneous sarcoidosis: a randomized, single-masked, placebo-controlled study. JAMA Dermatol. 2013 Jul 17. Epub ahead of print.
Alavi HA, Moscovic EA. Immunolocalization of cell-wall-deficient forms of Mycobacterium tuberculosis complex in sarcoidosis and in sinus histiocytosis of lymph nodes draining carcinoma. Histol Histopathol. 1996 Jul;11(3):683–94.
Berry MP, Graham CM, McNab FW, Xu Z, Bloch SA, Oni T, Wilkinson KA, Banchereau R, Skinner J, Wilkinson RJ, Quinn C, Blankenship D, Dhawan R, Cush JJ, Mejias A, Ramilo O, Kon OM, Pascual V, Banchereau J, Chaussabel D, O'Garra A. An interferon-inducible neutrophil-driven blood transcriptional signature in human tuberculosis. Nature. 2010;466:973–7.
Koth LL, Solberg OD, Peng JC, Bhakta NR, Nguyen CP, Woodruff PG. Sarcoidosis blood transcriptome reflects lung inflammation and overlaps with tuberculosis. Am J Respir Crit Care Med. 2011 Nov 15;184(10):1153–63.
Kandemir NO, Yurdakan G, Bektas S, Tekin NS. Classic Kaposi sarcoma with sarcoid-like granulomas: a case report and literature review. Exp Mol Pathol. 2009 Oct;87(2):89–93.
Zambrana F, Antúnez A, García-Mata J, Mellado JM, Villar JL. Sarcoidosis as a diagnostic pitfall of pancreatic cancer. Clin Transl Oncol. 2009 Jun;11(6):396–8.
Tchernev G, Wollina U. Sarcoidosis, cancer and molecular mimicry. Int J Immunopatol Phamacol. 2013;26(3):753–5.
Wormser GP, Dattwyler RJ, Shapiro ED, Halperin JJ, Steere AC, Klempner MS, Krause PJ, Bakken JS, Strle F, Stanek G, Bockenstedt L, Fish D, Dumler JS, Nadelman RB. The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006 Nov 1;43(9):1089–134.
Mazurek GH, Jereb J, Vernon A, LoBue P, Goldberg S, Castro K, IGRA Expert Committee, Centers for Disease Control and Prevention (CDC). Updated guidelines for using interferon gamma release assays to detect Mycobacterium tuberculosis infection—United States, 2010. MMWR Recomm Rep. 2010 Jun 25;59(RR-5):1–25.
Anderson H, Stryjewska B, Boyanton BL, Schwartz MR. Hansen disease in the United States in the 21st century: a review of the literature. Arch Pathol Lab Med. 2007 Jun;131(6):982–6.
Kubar J, Fragaki K. Recombinant DNA-derived leishmania proteins: from the laboratory to the field. Lancet Infect Dis. 2005 Feb;5(2):107–14.
Blair JE. Coccidioidal meningitis: update on epidemiology, clinical features, diagnosis, and management. Curr Infect Dis Rep. 2009 Jul;11(4):289–95.
Hofmann S, Franke A, Fischer A, Jacobs G, Nothnagel M, Gaede KI, Schürmann M, Müller-Quernheim J, Krawczak M, Rosenstiel P, Schreiber S. Genome-wide association study identifies ANXA11 as a new susceptibility locus for sarcoidosis. Nat Genet. 2008 Sep;40(9):1103–6.
Fischer A, Schmid B, Ellinghaus D, Nothnagel M, Gaede KI, Schürmann M, Lipinski S, Rosenstiel P, Zissel G, Höhne K, Petrek M, Kolek V, Pabst S, Grohé C, Grunewald J, Ronninger M, Eklund A, Padyukov L, Gieger C, Wichmann HE, Nebel A, Franke A, Müller-Quernheim J, Hofmann S, Schreiber S. A novel sarcoidosis risk locus for Europeans on chromosome 11q13.1. Am J Respir Crit Care Med. 2012 Nov 1;186(9):877–85. doi:10.1164/rccm.201204-0708OC.
Rybicki BA, Walewski JL, Maliarik MJ, Kian H, Iannuzzi MC. ACCESS research group ACCESS research group the BTNL2 gene and sarcoidosis susceptibility in African Americans and whites. Am J Hum Genet. 2005;773:491–499.
Hedfors E, Lindström F. HLA-B8/DR3 in sarcoidosis. Correlation to acute onset disease with arthritis. Tissue Antigens. 1983;223:200–20.
Voorter CE, Drent M, van den Berg-Loonen EM. Severe pulmonary sarcoidosis is strongly associated with the haplotype HLA-DQB1*0602-DRB1*150101. Hum Immunol. 2005;667:826–35.
Swider C, Schnittger L, Bogunia-Kubik K, Gerdes J, Flad H, Lange A, Seitzer U. TNF-alpha and HLA-DR genotyping as potential prognostic markers in pulmonary sarcoidosis. Eur Cytokine Netw. 1999 Jun;10(2):143–6.
Grutters JC, Sato H, Pantelidis P, Lagan AL, McGrath DS, Lammers JW, van den Bosch JM, Wells AU, du Bois RM, Welsh KI. Increased frequency of the uncommon tumor necrosis factor -857T allele in British and Dutch patients with sarcoidosis. Am J Respir Crit Care Med. 2002 Apr 15;165(8):1119–24.
Sharma S, Ghosh B, Sharma SK. Association of TNF polymorphisms with sarcoidosis, its prognosis and tumour necrosis factor (TNF)-alpha levels in Asian Indians. Clin Exp Immunol. 2008 Feb;151(2):251–9.
Hutyrová B, Pantelidis P, Drábek J, Zůrková M, Kolek V, Lenhart K, Welsh KI, Du Bois RM, Petrek M. Interleukin-1 gene cluster polymorphisms in sarcoidosis and idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2002 Jan 15;165(2):148–51.
Rothkrantz-Kos S, van Dieijen-Visser MP, Mulder PG, et al. Potential usefulness of inflammatory markers to monitor respiratory functional impairment in sarcoidosis. Clin Chem. 2003 Sep;49(9):1510–7.
Petereit HF, Reske D, Tumani H, Jarius S, Markus Leweke F, et al. Soluble CSF interleukin 2 receptor as indicator of neurosarcoidosis. J Neurol. 2010 Nov;257(11):1855–63.
Cui A, Anhenn O, Theegarten D, Ohshimo S, Bonella F, Sixt SU, Peters J, Sarria R, Guzman J, Costabel U. Angiogenic and angiostatic chemokines in idiopathic pulmonary fibrosis and granulomatous lung disease. Respiration. 2010;80(5):372–8.
Jonth AC, Silveira L, Fingerlin TE, et al. ACCESS group ACCESS group TGF-beta 1 variants in chronic beryllium disease and sarcoidosis. J Immunol. 2007;1796:4255–62.
Pabst S, Fränken T, Schönau J, Stier S, Nickenig G, Meyer R, Skowasch D, Grohé C. Transforming growth factor-{beta} gene polymorphisms in different phenotypes of sarcoidosis. Eur Respir J. 2011 Jul;38(1):169–75.
Spagnolo P, Sato H, Grunewald J, Brynedal B, Hillert J, Mañá J, Wells AU, Eklund A, Welsh KI, du Bois RM. A common haplotype of the C-C chemokine receptor 2 gene and HLA-DRB1*0301 are independent genetic risk factors for Löfgren’s syndrome. J Intern Med. 2008 Nov;264(5):433–41.
Niimi T, Tomita H, Sato S, Kawaguchi H, Akita K, Maeda H, Sugiura Y, Ueda R. Vitamin D receptor gene polymorphism in patients with sarcoidosis. Am J Respir Crit Care Med. 1999 Oct;160(4):1107–9.
Maliarik MJ, Rybicki BA, Malvitz E, Sheffer RG, Major M, Popovich J Jr, Iannuzzi MC. Angiotensin-converting enzyme gene polymorphism and risk of sarcoidosis. Am J Respir Crit Care Med. 1998 Nov;158(5 Pt 1):1566–70.
Tahir M, Sharma SK, Ashraf S, Mishra HK. Angiotensin converting enzyme genotype affects development and course of sarcoidosis in Asian Indians. Sarcoidosis Vasc Diffuse Lung Dis. 2007 Sep;24(2):106–12.
Schürmann M, Reichel P, Müller-Myhsok B, Dieringer T, Wurm K, Schlaak M, Müller-Quernheim J, Schwinger E. Angiotensin-converting enzyme (ACE) gene polymorphisms and familial occurrence of sarcoidosis. J Intern Med. 2001 Jan;249(1):77–83.
Lopez-Campos JL, Rodriguez-Rodriguez D, Rodriguez-Becerra E, Alfageme Michavila I, Guerra JF, Hernandez FJ, Casanova A, Fernández de Córdoba Gamero J, Romero-Ortiz A, Arellano-Orden E, Montes-Worboys A. Cyclooxygenase-2 polymorphisms confer susceptibility to sarcoidosis but are not related to prognosis. Respir Med. 2009 Mar;103(3):427–33.
Morbini P, Villa C, Campo I, Zorzetto M, Inghilleri S, Luisetti M. The receptor for advanced glycation end products and its ligands: a new inflammatory pathway in lung disease? Mod Pathol. 2006 Nov;19(11):1437–45.
Ho LP, Urban BC, Thickett DR, Davies RJ, McMichael AJ. Deficiency of a subset of T-cells with immunoregulatory properties in sarcoidosis. Lancet. 2005 Mar 19–25;365(9464):1062–72.
Varma M, Jasani B. Diagnostic utility of immunohistochemistry in morphologically difficult prostate cancer: review of current literature. Histopathology. 2005 Jul;47(1):1–16.
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, Hanna W, Jenkins RB, Mangu PB, Paik S, Perez EA, Press MF, Spears PA, Vance GH, Viale G, Hayes DF. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: american society of clinical oncology/college of american pathologists clinical practice guideline update. J Clin Oncol. 2013 Nov 1;31(31):3997–4013.
Rekhtman N, Ang DC, Sima CS, Travis WD, Moreira AL. Immunohistochemical algorithm for differentiation of lung adenocarcinoma and squamous cell carcinoma based on large series of whole-tissue sections with validation in small specimens. Mod Pathol. 2011 Oct;24(10):1348–59.
Taliano RJ, LeGolvan M, Resnick MB. Immunohistochemistry of colorectal carcinoma: current practice and evolving applications. Hum Pathol. 2013 Feb;44(2):151–63.
McCluggage WG, Young RH. Immunohistochemistry as a diagnostic aid in the evaluation of ovarian tumors. Semin Diagn Pathol. 2005 Feb;22(1):3–32.
Miettinen M. Immunohistochemistry of soft tissue tumors—review with emphasis on ten markers. Histopathology. 2013 Oct 1. doi:10.1111/his.12298.
Homma T, Kato A, Hashimoto N, Batchelor J, Yoshikawa M, Imai S, Wakiguchi H, Saito H, Matsumoto K. Corticosteroids and cytokines synergistically enhance toll-like receptor 2 expression in respiratory epithelial cells. Am J Respir Cell Mol Biol. 2004;31(4):463–9.
Veltkamp M, Wijnen PA, van Moorsel CH, Rijkers GT, Ruven HJ, Heron M, Bekers O, Claessen AM, Drent M, van den Bosch JM, Grutters JC. Linkage between Toll-like receptor (TLR) 2 promotor and intron polymorphisms: functional effects and relevance to sarcoidosis. Clin Exp Immunol. 2007;149(3):453–62.
Sato M, Kawagoe T, Meguro A, Ota M, Katsuyama Y, Ishihara M, Namba K, Kitaichi N, Morimoto S, Kaburaki T, Ando Y, Takenaka S, Ohno S, Inoko H, Mizuki N. Toll-like receptor 2 (TLR2) gene polymorphisms are not associated with sarcoidosis in the Japanese population. Mol Vis. 2011;17:731–6.
Chen ES, Song Z, Willett MH, Heine S, Yung RC, Liu MC, Groshong SD, Zhang Y, Tuder RM, Moller DR. Serum amyloid A regulates granulomatous inflammation in sarcoidosis through Toll-like receptor 2. Am J Respir Crit Care Med. 2010;181(4):360–73.
Wikén M, Idali F, Hayja MA, Grunewald J, Eklund A, Wahlström J. No evidence of altered alveolar macrophage polarization, but reduced expression of TLR2, in bronchoalveolar lavage cells in sarcoidosis. Respir Res. 2010;11:121.
Veltkamp M, van Moorsel CH, Rijkers GT, Ruven HJ, Grutters JC. Genetic variation in the Toll-like receptor gene cluster (TLR10-TLR1-TLR6) influences the disease course in sarcoidosis. Tissue Antigens. 2012;79(1):25–32.
Gazouli M, Koundourakis A, Ikonomopoulos J, Gialafos EJ, Rapti A, Gorgoulis VG, Kittas C. CARD15/NOD2, CD14, and toll-like receptor 4 gene polymorphism in Greek patients with sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2006;23(1):23–9.
Pabst S, Baumgarten G, Stremmel A, Lennarz M, Knüfermann P, Gillissen A, Vetter H, Grohé C. Toll-loke receptor (TLR) 4 polymorphisms are associated with a chronic course of sarcoidosis. Clin Exp Immunol. 2006;143(3):420–6.
Schürmann M, Kwiatkowski R, Albrecht M, Fischer A, Hampe J, Müller-Quernheim J, Schwinger E, Schreiber S. Study of Toll-like receptor gene loci in sarcoidosis. Clin Exp Immunol. 2008;152(3):423–31.
Veltkamp M, Grutters JC, van Moorsel CH, Ruven HJ, van den Bosch JM. Toll-like receptor (TLR) 4 polymorphism Asp299Gly is not associated with disease course in Dutch sarcoidosis patients. Clin Exp Immunol. 2006;145(2):215–8.
Iliadi A, Makrythanasis P, Tzetis M, Tsipi M, Traeger-Synodinos J, Ioannou PC, Rapti A, Kanavakis E, Christopoulos TK. Association of TLR4 single-nucleotide polymorphisms and sarcoidodis in Greek patients. Genet Test Mol Biomarkers. 2009;13(6):849–53.
Asukata Y, Ota M, Meguro A, Katsuyama Y, Ishihara M, Namba K, Kitaichi N, Morimoto S, Kaburaki T, Ando Y, Takenaka S, Inoko H, Ohno S, Mizuki N. Lack of association between toll-like receptor 4 gene polymorphisms and sarcoidosis-related uveitis in Japan. Mol Vis. 2009;15:2673–82.
Pabst S, Bradler O, Gillissen A, Nickenig G, Skowasch D, Grohe C. Toll-like receptor-9 polymorphisms in sarcoidosis and chronic obstructive pulmonary disease. Adv Exp Med Biol. 2013;756:239–45.
Veltkamp M, van Moorsel CH, Rijkers GT, Ruven HJ, van den Bosch JM, Grutters JC. Toll-like receptor (TLR)-9 genetics and function in sarcoidosis. Clin Exp Immunol. 2010;162(1):68–74.
Margaritopoulos GA, Antoniou KM, Karagiannis K, Samara KD, Lasithiotaki I, Vassalou E, Lymbouridou R, Koutala H, Siafakas NM. Investigation of Toll-like receptors in the pathogenesis of fibrotic and granulomatous disorders: a bronchoalveolar lavage study. Fibrogenesis Tissue Repair. 2010;3:20.
Tattoli I, Travassos LH, Carneiro LA, Magalhaes JG, Girardin SE. The Nodosome: Nod1 and Nod2 control bacterial infections and inflammation. Semin Immunpathol. 2007;29(3):289–301.
Wikén M, Grunewald J, Eklund A, Wahlström J. Higher monocyte expression of TLR2 and TLR4, and enhanced pro-inflammatory synergy of TLR2 with NOD2 stimulation in sarcoidosis. J Clin Immunol. 2009;29(1):78–89.
Rastogi R, Du W, Ju D, Pirockinaite G, Liu Y, Nunez G, Samavati L. Dysregulation of p38 and MKP-1 in response to NOD1/TLR4 stimulation in sarcoid bronchoalveolar cells. Am J Respir Crit Care Med. 2011;183(4):500–10.
Julian MW, Shao G, Schlesinger LS, Huang Q, Cosmar DG, Bhatt NY, Culver DA, Baughman RP, Wood KL, Crouser ED. Nicotine treatment improves Toll-like receptor 2 and Toll-like receptor 9 responsiveness in active pulmonary sarcoidosis. Chest. 2013;143(2):461–70.
Christoforidou A, Goudakos J, Bobos M, Lefkaditis E, Vital V, Markou K. Sarcoidosis-like granulomatosis of the hypopharynx as a complication of anti-TNF therapy. Am J Otolaryngol. 2013;34(3):268–72.
Yano S, Kobayashi K, Ikeda T, Kadowaki T, Wakabayashi K, Kimura M, Ishikawa S, Adachi Y, Araki K, Nagaoka S. Sarcoid-like reaction in Cryptococcus neoformans infection. BMJ Case Rep. 2012 Jul 27;2012. pii: bcr0720114528. doi:10.1136/bcr-07-2011-4528.
Guarneri F, Guarneri C. Molecular mimicry in cutaneous autoimmune diseases. World J Dermatol. 2013 Nov 2;2(4):36–43.
Conflict of interest
The authors declare that there are no actual or potential conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tchernev, G., Tana, C., Schiavone, C. et al. Sarcoidosis vs. Sarcoid-like reactions: The Two Sides of the same Coin?. Wien Med Wochenschr 164, 247–259 (2014). https://doi.org/10.1007/s10354-014-0269-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-014-0269-x