Abstract
Purpose
Postural orthostatic tachycardia syndrome (POTS) in adults is defined as symptoms of chronic orthostatic intolerance (COI) and autonomic dysfunction (AD) with heart rate (HR) increase of 30 beats per minute (bpm), or HR > 120 bpm, during prolonged upright position. However, in adolescents, POTS is defined as symptoms of OI and AD with HR increase of ≥ 40 bpm, based on tilt table data. We assessed frequency of COI symptoms in pediatric patients versus HR criteria on prolonged standing to evaluate using criteria of increased HR of 30–39 bpm versus ≥ 40 bpm in our POTS Program.
Methods
Patients with COI with symptoms for > 3 months plus HR increase of ≥ 30 bpm on 10 min stand aged ≤ 18 years at diagnosis were included. Patients were divided into two groups: those with HR increase of 30–39 bpm, and those with HR increase of ≥ 40 bpm or upright HR of > 120 bpm. A total of 28 symptoms described prior to diagnosis were evaluated using chi-square testing to assess for significant differences.
Results
Only insomnia was found to be significantly different between the two groups. The other 27 symptoms showed no significant difference as a function of HR.
Conclusion
There are minimal statistically significant differences and no clinical differences between patients as a function of HR increase during standing. Thus, a 40-bpm threshold for adolescents on standing test may be too high, or a specific HR criteria threshold is neither predictive nor definitive in diagnosing POTS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The clinical criteria used to define and diagnose postural tachycardia syndrome (POTS) include a history of chronic orthostatic intolerance (COI) and severely debilitating symptoms of orthostatic intolerance suggestive of autonomic dysfunction, as well as a significant tachycardic response to prolonged upright position, or an upright heart rate of at least 120 beats per minute (bpm). Earlier studies described this increase in heart rate to be at least 30 bpm [1, 2]. However, subsequent tilt table testing studies in adolescents determined that a cutoff of at least 40 bpm was more appropriate [3]. These data were subsequently used to create a consensus document in 2015 from the Heart Rhythm Society in which they utilized different heart rate criteria in adolescents aged 12–19, defined as an increase of at least 40 bpm [4], but maintained the 30-bpm criteria threshold for adult patients.
The POTS Program at the Children’s Hospital of Philadelphia (CHOP) opened in January 2014, although patients had been diagnosed and managed at CHOP by Dr. Boris since November 2007. The method of evaluation, including assessment of historical symptoms, involved a 10-min standing test based upon the previously published threshold of an increase of more than 30 bpm, or an upright heart rate of at least 120 bpm, for the diagnosis of POTS. Both the initial and subsequent onset of patient symptoms prior to diagnosis were recorded as discrete data within the health record. We sought to ascertain whether there was a difference in the presentation of patient symptoms in patients diagnosed with COI associated with a heart rate increase of 30–39 bpm, consistent with the prior diagnostic threshold, versus those with at least a 40-bpm increase or with an upright heart rate of at least 120 bpm, consistent with the newer diagnostic criteria. Our hypothesis was that the burden of symptomatology was unrelated to degree of tachycardic response to upright position.
Methods
The POTS Program at CHOP created a database in REDCap (Research Electronic Data Capture) that, in part, captured both demographic and discrete symptom data from the electronic health record [5]. Patients who were aged 18 years or under at the time of diagnosis of COI, and were evaluated between November 2007 and June 2016, met inclusion criteria for this retrospective evaluation. We utilized the accepted definition of POTS as daily symptoms of COI with sustained, excessive tachycardia in the absence of postural hypotension [6]. Initial patient evaluations and diagnoses were performed by only one of two physicians regularly caring for POTS patients in the Division of Cardiology. During initial intake a series of 28 symptoms [7,8,9] were reviewed with the patients and families to ascertain their presence or absence (Table 1). These symptoms spanned several somatic systems, including cardiovascular, gastrointestinal, orthopedic, and neurologic. Symptom history was also ascertained pertaining to qualitative worsening with upright position. Only those patients who had (1) multiple symptoms across more than one physiologic system, (2) symptoms for at least 3 months, (3) frequent recurrence of symptoms, and (4) interference in activities of daily living due to symptomatology were then evaluated by a 10-min standing test. For example, a patient with a complaint of lightheadedness, tachycardia, nausea, and visual changes (e.g., seeing spots or blurred vision) that was transient in nature, infrequent, or did not interfere with activities of daily living, would not undergo a standing test. However, a patient with lightheadedness, blurred vision, fatigue, cognitive dysfunction, insomnia, headache, nausea, and constipation that was persistent or frequently recurrent, and severe enough that it significantly disrupted routine activity would undergo testing. Patients included in this study were not taking medications that would affect the autonomic system at the time of evaluation, including volume expanding agents (e.g., fludrocortisone), vasoconstricting agents (e.g., midodrine), beta blockers, tricyclic antidepressants, or stimulants. ECGs were obtained on all patients. The protocol for the standing test required that the patient remain supine for 3 min. A resting heart rate was obtained. The patient was then asked to stand motionless for 10 min with minimal stimulation. Heart rate measurements were obtained once per minute, with the highest consistently achieved heart rate documented as diagnostic. If a patient achieved a 30-point increase in heart rate once during the 10-min stand, but otherwise maintained less than a 30-point increase, it was not recorded as the high heart rate, and the patient was not diagnosed with POTS. Conversely, if a patient had a heart rate increase of at least 30 bpm measured at least three times, the test was deemed positive. Blood pressure was measured at the 1-min and 3-min marks. Patients with a decrease in systolic blood pressure greater than 20 mmHg were not given a diagnosis of POTS. Serum and plasma catecholamine levels were not obtained as part of the evaluation. The patients then were divided into two groups of patients: those with a heart rate increase of 30–39 bpm, and those with at least a 40-bpm in heart rate on 10-min standing test, or an increase of over 120 bpm. Individual symptoms were then compared between the two groups for percentage frequency. Joint hypermobility was also diagnosed in the clinic by performing a Beighton score during physical examination, with a score of less than 6 consistent with joint hypermobility without Ehlers–Danlos syndrome. Patients with a Beighton score of 6 or greater plus appropriate other historical and clinical findings would be referred to the CHOP Connective Tissue Disorders clinic for further evaluation. If appropriate, a diagnosis of hypermobile Ehlers–Danlos syndrome was made through that clinic.
Statistical analysis was performed using R version 3.5.3, utilizing chi-square assessment to assess for differences between specific categorical variables, and Mann–Whitney U test to assess between two groups, at a significant value of 0.05. Since we tested for 28 variables, Bonferroni correction was used to adjust for multiple comparisons in order to control the false discovery rate. After adjustment, p value less than 0.002 was considered to be statistically significant. We performed a multiple logistic regression model using the group variable heart rate increase > 30–39 or > 40 bpm as the dependent variable and the 28 symptom variables as independent variables, and using variance inflation factor (VIF) to identify the variables that are highly correlated. To estimate the empirical density of the number of symptoms for each group, we used a kernel density estimation with a Gaussian kernel. We adopted the commonly used normal reference rule to select the bandwidth for the kernel estimation [10]. The method was implemented using R package “ggplot2”. In order to check the multicollinearity among the symptom variables, we calculated the pairwise Pearson correlations for the 28 symptom variables to evaluate the magnitude of association among the variables. Additionally, we conducted principal component analysis (PCA) to reduce the number of symptoms by extracting principal components. We specifically used the logistic PCA approach for dimensionality reduction of binary data proposed by Landgraf and Lee [11]. This approach is an extension of ordinary PCA by means of a matrix factorization, akin to the singular value decomposition, that maximizes the Bernoulli log-likelihood. We then built a classification tree based on Gini split to identify the variables that predicted the categories of HR (within 30–39 or ≥ 40) without the linearity assumption. We used all the 28 symptoms in the mode, and randomly split the data into training and testing sets in the ratio of 7:3. The training set was used to build the tree and the testing set was used to test the performance of the tree. The importance score measures of the variables are listed in Table 2, ranking from high to low. The importance score measures a variableʼs ability to predict the outcome in the built tree, where a higher score indicates that the variable is more useful for predicting the HR categories.
The data were obtained during the course of routine clinical care through the electronic health record and were subsequently de-identified. Thus, a waiver of consent was granted by the CHOP Institutional Review Board, as it would have been impractical to gain consent retroactively.
Results
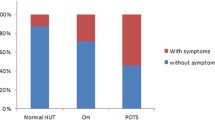
From November 2007 to June 2016, a total of 722 patients were evaluated and diagnosed with COI in our clinic. During the same time period, 548 patients were diagnosed with either dizziness or syncope, 2 patients were diagnosed with inappropriate sinus tachycardia, and 29 patients were diagnosed with autonomic dysfunction that was not consistent with COI. Only 708 of the 722 patients who were diagnosed with COI were aged 18 or under, and thus met initial criteria for study inclusion. However, only 640 of these patients had a complete assessment of their symptoms recorded, and thus were included in the study (Fig. 1). Demographic data for these patients are shown in Table 3. Symptoms and signs that specifically were reported to worsen with standing included blurred vision, dizziness, dyspnea with activity, exercise intolerance, fatigue, headache, palpitations, syncope, tachycardia, and venous pooling. All other symptoms were described either with standing or while seated or supine. Except for joint hypermobility, symptoms were noted to have started at, or after, the initial onset of symptoms. The median duration of symptoms was 2.0 years. All ECGs obtained were normal, without evidence of other arrhythmia, such as long QT or Wolff–Parkinson–White syndrome, or structural defects. The median heart rate increase on a 10-min standing test was 36.5 bpm for all patients, with a range of 30–120 bpm. There were no patients who demonstrated a significant drop in blood pressure that would preclude the diagnosis of POTS or COI. The number of patients in the two study groups was not statistically different, with 302 patients in the 30–39 group and 338 patients in the ≥ 40 group (p > 0.05). Four symptoms showed an initial significant difference between study groups: blurred vision, insomnia, nausea, and reported tachycardia (Table 4), although with Bonferroni correction, only insomnia reached statistical significance. None of the other 27 symptoms demonstrated a significant difference in occurrence between groups. The distribution of the total number of symptoms per patient was very similar between the two heart rate groups, as shown in Table 5 and Fig. 2. About 50% of patients experienced fewer than 16 of the 28 symptoms, with the range between 4 and 28 symptoms. Figure 3 demonstrates the magnitude and direction of the correlations. In the multiple logistic regression model, the VIF for both palpitations and tachycardia were very high, at > 4.6. The VIF for other variables were less than 1.4. We also found that both of these variables were highly correlated with the Pearson correlation at 0.85. After these diagnoses, we excluded “palpitations” and fit the multiple logistic regression model with the other 27 symptom variables to test if any of the symptoms were associated with the HR group. The results of the logistic regression model are shown in Table 6. We found that the symptoms cognitive dysfunction, chest pain, diaphoresis, and heat intolerance were significantly different between the two HR groups.
Pearson correlation between each pair of the 28 symptom variables. Positive correlations are displayed in blue and negative correlations in red color. Color intensity is proportional to the correlation coefficients. The color legend on the right side of the correlogram shows the correlation coefficients and the corresponding colors
Our PCA demonstrated minimal difference between the two groups. We extracted 17 principal components (PCs) which explained 91.9% of total deviance. The first two PCs explained 18.5% of total deviance. The PCs are visualized in Fig. 4 using a PCA score plot. However, as shown in the figure, we did not find a clear distinction between HR groups using the first two PCs. This is probably due to the concept that a linear sum of the binary variables may be a poor summary of the sources of variation between the groups. Our classification tree also demonstrated a diminished correlation. The area under the curve of the tree was 0.57 in the testing set, which indicated a low performance. After testing, we demonstrated the tree using the entire data sets as shown in Fig. 5. On the basis of the built tree, the top 10 variables that predicted the HR categories were chest pain, cold intolerance, diaphoresis, fatigue, heat intolerance, hyperacusis, insomnia, joint hypermobility, joint pain, and vomiting.
Discussion
The signs and symptoms that can be associated with COI are diverse, multisystemic, frequent, and highly variable in severity. Some can be directly related to COI, such as those that are dependent upon upright position to worsen them. Others are due to concurrent autonomic dysfunction, and some are due to downstream physiologic effects that accompany dysautonomia or coexisting deconditioning. In a previous study, we demonstrated that 66% of patients presented with at least 10 different symptoms, 50% of patients had at least 14 symptoms, and 30% of patients reported at least 26 symptoms associated with their POTS [9]. These symptoms varied widely and were of cardiovascular, neurologic, orthopedic, or gastrointestinal origin. The presence of these symptoms is an important element in suggesting a diagnosis of autonomic dysfunction. These were not patients with typical initial orthostatic intolerance, which can occur in up to 50% of adolescents [12, 13], nor were they patients with reflex syncope, occurring in up to 39% of adolescents [14], in which there is dizziness/lightheadedness, visual changes (blurring, tunnel vision, etc.), nausea, and headaches. An older Dutch study demonstrated that 43% of adolescents have a “near-fainting” event with tilt table testing, and demonstrate a mean increase in heart rate of 32 bpm [15]. These patients typically respond to modestly increased fluid and sodium intake, with resolution of symptoms; occasionally, they require the use of isometric muscular activities to abort episodes, and medication support to further suppress symptoms [16, 17]. In contrast, patients with COI are typically more severely debilitated, have more multisystem complaints, do not improve with modest supplementation of fluid and salt (routinely requiring greatly increased intake of fluid and sodium), and often require pharmacologic management to further support cardiovascular stability and/or suppress their symptoms [17]. Their symptoms are chronic and occur frequently, as often as daily. There is also suggestive evidence that further differentiates patients with POTS from those with neurally mediated syncope. Autoantibodies to adrenergic, cholinergic, and angiotensin receptors have been increasingly recognized in adult patients with POTS, while comparison groups with neurally mediated syncope do not [18,19,20]. Although this association has not been shown to be the etiology of POTS, this finding, if demonstrated to be a true cause, further sets COI and, specifically, POTS apart from other dysautonomias.
The utilization of a threshold heart rate increase of 40 or more bpm for adolescents is problematic [3, 4]. Although pediatric patients may have demonstrated a higher heart rate increase on tilt table testing as compared to adults, from a clinical standpoint it is apparent that the overlap between patients with simple orthostatic intolerance and patients with POTS is large [15, 21]. There are otherwise a large number of pediatric patients who do not technically meet specific heart rate criteria for POTS, but are nonetheless severely symptomatic compared to those with a more modest tachycardic response. This observation supports a theory that COI is only reflective of orthostatic tachycardic response and its associated cardiovascular symptomatology, while the other systemic symptoms are adjunctive in nature, and not truly a clinical manifestation of COI [22]. Despite this view, patients and families would suggest otherwise, as their symptomatology manifests as a variable and often changing collection of symptoms, with much of their symptom burden not existing prior to the onset of the symptoms. It is entirely possible that the diagnostic criterion for COI that relies on heart rate as an absolute threshold is insufficient. It is worth noting that the term postural tachycardia syndrome itself, or the use of previously published definitions of COI and POTS, may introduce cognitive bias and limit the interpretation of the patients’ history and presenting symptoms. This can result in assessments and diagnostic decision-making that are more restrictive and obstructive to a paradigm and clinical approach that might otherwise be required. Thus, the use of a 40-bpm heart rate threshold to absolutely define COI and POTS in otherwise severely symptomatic patients potentially isolates a group of patients and families from a diagnostic and medical management perspective. They are not diagnosed with POTS. They are not considered to have simple orthostatic intolerance. Thus, the reliance on absolute heart rate criteria can lead to possible underdiagnosis, undertreatment, and medical mismanagement with subsequent morbidity and delay in access to therapeutic strategies that could support clinical improvement. More simply stated, it is worth considering that utilizing a threshold heart rate as a diagnostic criterion for COI and POTS may be a red herring [23]. The constellation of symptoms and patient history along with the debilitating nature and chronicity of symptoms may be more important diagnostically than the absolute heart rate increase. A “relatively elevated” heart rate without a true absolute threshold may likely be a more appropriate adjunct finding in the diagnosis of COI and POTS. Previous data from the Mayo Clinic comparing adult patients with orthostatic intolerance (i.e., patients with a heart rate increase of less than 30 bpm on tilt table test) versus those with POTS have demonstrated that there is no difference in associated symptomatology between these two groups [24].
In our study, we conducted both univariate analysis and multiple logistic regression models to study the association between the variables and the HR categorization and to identify variables that predict the HR group. Both analyses have advantages and disadvantages. The estimated effects of univariate analyses are relatively easier to interpret, i.e., the marginal effects of a variable on the HR categories, but the univariate analyses could suffer from low power as multiple comparisons needed to be adjusted using Bonferroni correction. The multiple logistic regression model allowed us to incorporate all variables into one model, estimate the adjusted effect, and test the hypothesis simultaneously without adjusting for multiple comparisons. However, the regression coefficients from the multiple logistic regression model are difficult to interpret, as the estimated effects are adjusted by all other variables. Thus, the univariate analysis demonstrated insomnia as the only significantly different symptom between groups, while the multiple logistic regression model showed cognitive dysfunction, chest pain, diaphoresis, and heat intolerance as different between groups. Meanwhile, the PCA found no significant difference between groups. And, although the Gini classification tree suggested chest pain, cold intolerance, diaphoresis, fatigue, heat intolerance, hyperacusis, insomnia, joint hypermobility, joint pain, and vomiting as predictive of differentiation between the two groups, the tree’s performance was low, based on the area under the curve in the testing set. Thus, despite multiple statistical approaches to differentiation between the two groups, no symptoms emerged as clearly different between the two heart rate groups.
An important consideration is that we utilized a 10-min stand, not tilt table testing, to ascertain heart rate response to chronic upright position and subsequently make a diagnosis of OI (in conjunction with a preponderance of symptom burden). This approach has been previously utilized and accepted as reasonable for the diagnosis of POTS. A study in adult patients at Vanderbilt University Medical Center demonstrated that patients who underwent tilt table testing, and subsequently performed standing testing, had a 10-point greater increase in heart rate with tilt than with active standing [25]. This would be consistent with the use of a 10-min stand and utilizing a threshold of 30 bpm, or greater, for the diagnosis of OI. It is notable that tilt table testing, which utilizes passive upright position as its orthostatic challenge and not a physiologic state, tends to be more provocative. In previously asymptomatic adolescent control patients, 52% had either pre-syncope or syncope [26]. Furthermore, adult data suggest that tilt table testing does not correlate with implantable loop recorder findings during actual syncopal events [27], raising questions regarding the efficacy of tilt table testing as a diagnostic modality in this specific disease process.
When reviewing the results of the comparison of symptoms, only one of 28 symptoms (3.6%) demonstrated a statistically significant difference between the two groups. Insomnia occurred less frequently in those patients with a heart rate increase of 40 or more bpm. Although blurred vision, nausea, and tachycardia demonstrated a p value less than 0.05, it is curious that there seems to be a real difference in the incidence of insomnia; the reason for this is unclear, and may be unrelated to orthostatic intolerance and/or autonomic dysfunction. Regardless of these results and observations, these data do not suggest or support a significant clinical difference between the two groups of patients.
As the frequency of symptoms between the two heart rate groups is essentially equivalent, it suggests that in the comparison of a 10-min standing test that gives a 30–39 bpm increase in heart rate versus a test that gives a 40, or more, bpm increase, the artificial threshold of 40 bpm is not a clinically useful criterion. This does not address patients who may have similar symptoms, but have a heart rate increase of less than 30 bpm. Since this study was utilizing the older definition of POTS, with a heart rate increase of at least 30 bpm, only those patients with a 30, or more, bpm increase were entered into the database. Patients were identified and diagnosed in our clinic as early as 2007 utilizing these criteria. Updated diagnostic criteria were published in 2015. However, we were not performing tilt table testing and since tilt versus stand had already been shown to exhibit different results from the published 2013 data, we elected not to change our diagnostic criteria. Anecdotally, patients who had undergone tilt table testing at outside facilities consistently reported that tilt table testing routinely made them feel worse during the actual test, as well as for a prolonged period of time afterward, exacerbating their symptoms. While the standing test was often difficult for patients to tolerate, it typically did not flare their symptoms, and they were able to rapidly recover from their orthostatic intolerance upon sitting or lying down. Thus, a significant tachycardic response was achieved, which allowed for assessment and diagnosis while minimizing undue distress or provoking a prolonged flare of symptoms. In our clinic experience, there were very few patients who had a significantly elevated constellation of symptoms who did not also have at least a 30-point increase in heart rate. Of those who did, their heart rate increases were greater than 25 bpm.
This analysis presents some weaknesses. Because this is a retrospective review, it is predominantly reliant upon patient memory and recall for reporting symptoms. This is further complicated by a median duration of symptoms prior to diagnosis in our clinic of over 2 years [7], which may reduce the ability of the patients and families to accurately recall symptomatology. The greatest weakness in this study, however, is the use of a 10-min standing test to make the diagnosis of OI in lieu of a tilt table test. At this time, a standing test has not been validated. We have attempted to address the issues of comparison of stand versus tilt in the discussion above. As well, all patients meeting inclusion criteria were evaluated equally throughout the evaluation period, with assessment consistent across all patients. Finally, the Heart Rhythm Society consensus statement supports the use of just a 10-min stand, with the addition of tilt table testing, if indicated [4].
Our study demonstrates that the frequency of symptoms of COI in pediatric patients with a heart rate increase of 30–39 bpm on 10-min standing test was essentially equivalent to that of patients with a heart rate increase of at least 40 bpm or a heart rate greater than 120 bpm. These data may support reassessing the use of an absolute threshold criterion of at least 40 bpm for establishing a diagnosis of COI and POTS in adolescent patients. As well, the data may be used to support discussions regarding validating a standing test in comparison to a tilt table test. However, it also could be suggested that the use of an absolute heart rate threshold for the diagnosis of COI and POTS is of questionable validity, and that a relative tachycardia in conjunction with the panoply of severe debilitating symptoms might be better used to define this entity. Eventually, a biological marker, or set of markers, will be available to more consistently define and diagnose these patients. This may include a panel of autoantibodies or some other common, as yet undefined, biomarker. Doing so may facilitate the diagnosis of COI and POTS in the clinic without utilizing more complex equipment and procedures as well as reducing the overall sequelae for patients while undergoing evaluation and diagnosis for COI and POTS. It will also more completely identify these patients, and more quickly allow them to begin pharmacologic and non-pharmacologic treatment and management.
References
Raj SR, Black BK, Biaggioni I, Harris PA, Robertson D (2005) Acetylcholinesterase inhibition improves tachycardia in postural tachycardia syndrome. Circulation 111:2734–2740
Hoeldtke RD, Bryner KD, Hoeldtke ME, Hobbs G (2006) Treatment of postural tachycardia syndrome: a comparison of octreotide and midodrine. Clin Auton Res 16:390–395
Singer W, Sletten DM, Opfer-Gehrking TL, Brands CK, Fischer PR, Low PA (2012) Postural tachycardia in children and adolescents: what is abnormal? J Pediatr 160:222–226
Sheldon RS, Grubb BP 2nd, Olshansky B et al (2015) 2015 Heart Rhythm Society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm 12:e41–e63
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-drive methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Stewart JM, Boris JR, Chelimsky G et al (2018) Pediatric disorders of orthostatic intolerance. Pediatrics 141(1):e20171673. https://doi.org/10.1542/peds.2017-1673
Mathias CJ, Low DA, Iodice V, Owens AP, Kirbis M, Grahame R (2011) Postural tachycardia syndrome—current experience and concepts. Nat Rev Neurol 8:22–34
Jiawei L, Qingyou Z, Hongjun H, Hongfang J, Junbao D (2014) Clinical features and management of postural tachycardia syndrome in children: a single-center experience. Chin Med J127:3684–3689
Boris JR, Bernadzikowski T (2018) Demographics of a large paediatric postural orthostatic tachycardia syndrome program. Cardiol Young 28:668–674
Silverman BW (1986) Density estimation for statistics and data analysis. Chapman and Hall, London
Landgraf AJ, Lee Y (2015) Dimensionality reduction for binary data through the projection of natural parameters. arXiv:1510.06112
Stewart JM, Clarke D (2011) “He’s dizzy when he stands up”. An introduction to initial orthostatic hypotension. J Pediatr 158:499–504
Langhagen T, Albers L, Heinen F et al (2015) Period prevalence of dizziness and vertigo in adolescents. PLoS One 10:e0136512
Ganzeboom KS, Colman N, Reitsma JB, Shen WK, Wieling W (2003) Prevalence and triggers of syncope in medical students. Am J Cardiol 91:1006–1008
De Jong-deVos van Steenwijk CCE, Wieling W, Harms MPM, Wesseling KH (1997) Variability of near-fainting responses in healthy 6–16-year-old subjects. Clin Sci (Lond) 93:205–211
Freeman R (2003) Treatment of orthostatic hypotension. Semin Neurol 23:435–442
Frishman WH, Azer V, Sica D (2003) Drug treatment of orthostatic hypotension and vasovagal syncope. Heart Dis 5:49–64
Ruzieh M, Batizy L, Dasa O, Oostra C, Grubb B (2017) The role of autoantibodies in the syndromes of orthostatic intolerance: a systematic review. Scan Cardiovasc J 51:243–247
Watari M, Nakane S, Mukaino A et al (2018) Autoimmune postural orthostatic tachycardia syndrome. Ann Clin Transl Neurol 5:486–492
Yu X, Li H, Murphy TA et al (2018) Angiotensin II type 1 receptor autoantibodies in postural tachycardia syndrome. J Am Heart Assoc. https://doi.org/10.1161/JAHA.117.008351
Skinner JE, Driscoll SW, Porter CJ et al (2010) Orthostatic heart rate and blood pressure in adolescents: reference ranges. J Child Neurol 25:1210–1215
Chelimsky G, Kovacic K, Nugent M, Mueller A, Simpson P, Chelimsky TC (2015) Comorbid conditions do not differ in children and young adults with functional disorders with or without postural tachycardia syndrome. J Pediatr 167:120–124
Ives CT, Kimpinski K (2014) Higher heart rate increments on head-up tilt in control subjects are not associated with autonomic dysfunction. Clin Neurophysiol 125:2109–2114
Parsaik AJ, Singer W, Allison TG et al (2013) Orthostatic intolerance without postural tachycardia: how much dysautonomia? Clin Auton Res 23:181–188
Plash WB, Diedrich A, Biaggioni I et al (2013) Diagnosing postural tachycardia syndrome: comparison of tilt testing compared with standing haemodynamics. Clin Sci (Lond) 124:109–114
Berkowitz JB, Auld D, Hulse JE, Campbell RM (1995) Tilt table evaluation for control pediatric patients: comparison with symptomatic patients. Clin Cardiol 18:521–525
Brignole M, Sutton R, Menozzi C et al (2006) Lack of correlation between the responses to tilt testing and adenosine triphosphate test and the mechanism of spontaneous neurally mediated syncope. Eur Heart J 27:2232–2239
Acknowledgements
The authors would like to acknowledge the excellent assistance and review work of Andrew Glatz, MD, MSCE. As well, we would like to thank Andrea Kennedy, Arya Boris, Robert Rennie, and Elizabeth Schoenberg for the creation of and the updating within the CHOP POTS Database. Finally, we acknowledge the excellent support of the Cardiac Center Research Core at the Children’s Hospital of Philadelphia.
Funding
The creation of the CHOP POTS database was supported by the Cardiac Center of the Children’s Hospital of Philadelphia. Partial funding for personnel working on the database was provided by Dysautonomia International.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Boris, J.R., Huang, J. & Bernadzikowski, T. Orthostatic heart rate does not predict symptomatic burden in pediatric patients with chronic orthostatic intolerance. Clin Auton Res 30, 19–28 (2020). https://doi.org/10.1007/s10286-019-00622-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-019-00622-y