Abstract
We assessed the potency of octreotide and midodrine, and their combination, in the treatment of the postural tachycardia syndrome (POTS) and orthostatic intolerance (OI). Nine patients with POTS and six patients with OI stood for up to 1 hour while their HR and BP were monitored. Patients received on separate days, midodrine 10 mg 1 hour before testing, octreotide 0.9 µg/kg 8 minutes before testing or combination therapy. Standing time in the patients with POTS was 41.2 ± 8.4 minutes and not improved by midodrine or octreotide, but increased to 56.3 ± 2.7 (P < 0.01) minutes following combination therapy. The standing heart rate in POTS, 114 ± 0.7 bpm, was suppressed by midodrine 92.8 ± 0.7 (P < 0.001), octreotide 90.6 ± 0.78 (P < 0.001), and combination therapy 84.7 ± 0.7 (P < 0.001). Combination therapy was better than monotherapy (P < 0.001) but only for the first 10 minutes of standing.
Standing time of 36.3 ± 3.5 minutes in the patients with OI improved with midodrine, octreotide and combination therapy (55.5 ± 3.1, 56.5 ± 3.5, and 56.6 ± 3.3, respectively, P < 0.05 for each). Standing heart rate in OI was 100 ± .76 bpm; following midodrine it was 80.3 ± .69 (P < 0.05), following octreotide it was 84.8 ± .86, and following combination therapy it was 71.2 ± .9 (P < 0.01). The RR interval versus time area under the curve (The Orthostatic Index) was 21.1 ± 4 in patients with OI. After midodrine it was 41.4 ± 3.5 (P < 0.01), after octreotide 40.3 ± 3.8 (P < 0.01) and after the combination it was 47.3 ± 4.6 (P < 0.001).
Midodrine and octreotide suppressed tachycardia in POTS and improved standing times in OI. The two drugs had similar potencies; combination therapy was not significantly better than monotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many patients who experience dizziness upon shifting from the supine to the upright posture develop tachycardia upon standing, but have a stable blood pressure. This disorder, the postural tachycardia syndrome or POTS, can be diagnosed if the increment in heart rate associated with standing is at least 28 beats per minute [14]. Some patients with orthostatic dizziness, however, have less cardiac acceleration when upright but nevertheless develop hypotension, syncope, nausea, palpitations or headaches with prolonged standing [13]. We included these patients in the present study in the category Orthostatic Intolerance (OI). Although these are common disorders, few studies have focused on pharmacological therapy or compared treatments. Midodrine, a dihydroergotamine like alpha 1 agonist and vasoconstrictor is often used to treat these disorders and its efficacy in POTS has been documented [3]. Some patients cannot tolerate midodrine, however, or are dissatisfied with its therapeutic effect. Alternative therapies are needed and octreotide is theoretically attractive since it is a splanchnic vasoconstrictor and excessive splanchnic pooling has recently been documented in patients with orthostatic syncope [11] and POTS [12, 15]. The primary purpose of this study was to compare midodrine and octreotide with each other and to determine whether or not octreotide is a viable therapeutic option for patients who cannot tolerate midodrine. The second purpose of the study was to determine whether combination therapy was more effective than treatment with a single drug.
Methods
Subjects
Twenty-three patients with POTS or OI expressed interest in this study. We included one individual (Patient 1 in Table 1) in the POTS category who had a standing heart rate of 120 even though she did not have a 28 bpm increment with standing. Reversible causes of postural tachycardia and hypotension (Addison’s Disease, dehydration, and chronic infection) were excluded. Patients with diabetes or any uncontrolled systemic disease were excluded. Patients with a recent history of diarrhea or abdominal cramps were excluded. The protocol was approved by the Institutional Review Board of West Virginia University and informed consent obtained.
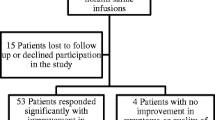
Patients who had never previously been treated with octreotide were first given a test dose (0.45 µg/kg) to determine whether they tolerated this agent. Seven patients had abdominal cramps or diarrhea and withdrew from the study. One patient developed headaches while treated with midodrine prior to the protocol and withdrew. The remaining 15 participants were all female (Table 1). Eleven of the patients had never received either midodrine or octreotide prior to their evaluation for this study. Their response to midodrine was not systematically assessed prior to the study. Chronic fatigue, orthostatic dizziness and palpitations were the most common symptoms (Table 1). Six patients had stopped working because of POTS or OI and were disabled [2].
Orthostatic testing and drug administration
Patients were studied in the morning before breakfast or in Endocrine Clinic or the Autonomic Function Laboratory at West Virginia University Medical Center. Caffeine was not allowed on the morning of the studies. Two patients took fludrocortisone prior to the study and this was discontinued one week prior to the experiments. Midodrine and octreotide were discontinued for at least 48 hours prior to the study. One patient was allowed to continue a constant dose of fluoxetine during the study. Patients rested in the supine posture for 10 minutes before duplicate measurements of the heart rate and blood pressure. The patients then were instructed to stand for 1 hour without moving their legs while their heart rate and blood pressure were measured at 1-minute intervals with a Accutorr III (Datascope, Paramus, New Jersey). A nurse or one of the investigators were always present to prevent injury at the time of syncope. Testing was terminated if the patients appeared presyncopal, complained of dizziness, nausea or headaches or became hypotensive (a systolic blood pressure of less than 75 mmHg).
Patients were first tested off all medicines and then received on separate days in a random sequence either midodrine 10 mg orally 1 hour before testing, octreotide 0.9 µg/kg subcutaneously 8 minutes before testing, or combination therapy given at the same time intervals as when the drugs were given individually. These time intervals were chosen since we have previously shown them to be optimal in patients with autonomic neuropathy [7].
Measurements
We measured standing time, heart rate, and blood pressure. To assess the therapeutic efficacy of the drugs we needed a mathematical formulation that would reflect both prolongation of standing time and suppression of tachycardia. The latter would necessarily result in an increase in the RR-interval. We therefore calculated the Orthostatic Index, the RR interval versus time area under the curve as follows: Orthostatic Index = RR interval (in seconds/beat) at minute 1 + RR interval at minute 2... + RR interval at minute n where n is standing time. The RR interval in seconds/beat = RR interval in minutes × 60/beat = 60/heart rate (beats per minute). For example a patient with a heart rate of 120 bpm for 4 minutes would have an orthostatic index of 0.5 second/beat × 4 = 2.0. A patient with a standing heart rate of 60 bpm for 60 minutes would have an orthostatic index of 1 second/beat times 60 = 60.
The effect of octreotide (0.9 µg/kg) on the orthostatic index is illustrated in Figure 1.
Statistical analyses
Standing time was treated as a time to event variable and assessed using a Weibull survival model [4].
Heart rate and blood pressure were compared for uniform standing times, which was the shortest standing time for each patient. For example, if a patient had a standing time of 20 minutes off therapy, but then longer standing times following treatment, we would only statistically compare the heart rate and blood pressure data for 20 minutes. The orthostatic index, however, took both the heart rate (RR interval) and standing time into account.
Data for the heart rate, blood pressure, and orthostatic index were first analyzed by a multivariate analysis of variance (MANOVA) [16]. Factors included in the MANOVA model were subjects, midodrine (yes/no), octreotide (yes/no), and the interaction of the last two. The primary contrast of interest was octreotide versus midodrine. Contrasts were formed to specifically compare each treatment to no treatment, and to compare combination therapy with monotherapy (the average of the mean heart rate following octreotide and the mean heart rate following midodrine). Misleading results from multiple comparisons were minimized by performing Bonferroni corrections on the final P values.
Results
Fifteen patients tolerated octreotide and were willing to participate. Ten had POTS and five had OI at the time of the initial evaluation. One of the individuals with POTS (patient 10 in Table 1) met the criteria for POTS at the initial evaluation but did not at the time of her testing off treatment in this protocol so the data gathered on her was included in the OI group. The mean age of the participants was 36.3 years.
Standing times
The mean standing time for the patients with POTS was 41.2 ± 8.4 minutes. Although neither midodrine nor octreotide led to a significant increase in standing time, after combination therapy standing time was 56.3 ± 2.7 minutes (different from no treatment, P = 0.001) (Table 2). Standing time for the patients with OI was 36.3 ± 3.5 minutes and increased by approximately 19 minutes following midodrine, octreotide, and combination therapy (P < 0.05 for all therapies) (Table 2).
Heart rates
Midodrine and octreotide suppressed heart rate equally in the patients with POTS (P < 0.001 for each treatment) (Table 2). Combination therapy was more effective than monotherapy (the mean of the heart rate following midodrine and the heart rate following octreotide) for the first 10 minutes of the test (P < 0.001) (Figure 2). Midodrine (P = 0.041) and combination therapy (P = 0.0024) led to significant suppression of heart rate in the subset with OI but octreotide did not (Table 2).
Blood pressures
The mean blood pressures were not affected by treatment in patients with POTS, OI or the pooled data (Figure 3, Table 2).
Orthostatic indices
The mean orthostatic index in the patients with POTS was 23.8 ± 4.7 and not significantly increased by either midodrine or octreotide (Table 2). Following combination therapy the orthostatic index was 40.6 ± 2.4 and the difference from no therapy approached significance (P = 0.062). The mean orthostatic index in the subset with OI was 21.1 ± 4.0 and approximately doubled by midodrine (P = 0.0063 versus no treatment), and octreotide (P = 0.0099) and increased to 47.3 ± 4.6 by combination therapy (P < 0.001).
Adverse effects
Octreotide and midodrine had adverse as well as beneficial effects. Octreotide caused nausea, vomiting, abdominal cramps or diarrhea in seven of the original 23 patients. The adverse effects following midodrine were less severe; nine patients developed scalp itching, chills, dysphoria or headaches following midodrine and six patients resisted chronic therapy because of these complaints. Two patients tolerated monotherapy with each drug but developed abdominal cramps and diarrhea when given the combination.
Discussion
The primary purpose of this study was to compare the effects of octreotide with those of midodrine. We observed that the two drugs suppressed tachycardia to a similar extent in patients with POTS (Table 2 and Figure 2) but neither drug improved standing time or significantly improved the orthostatic index in this subset of patients. Five of the nine patients with POTS were able to stand for the full 60 minutes off treatment, so there was no room for improvement in this parameter for most patients. Combination therapy suppressed tachycardia to a greater extent than did monotherapy but this was a transient benefit lasting only for the first 10 minutes of standing.
We observed that midodrine and octreotide improved standing times and the orthostatic indices to similar extents in patients with OI (Table 2). Midodrine suppressed the heart rate by approximately 20 beats per minute (P < 0.05) whereas octreotide suppression was only 15 beats per minute, which was not significant. Combination therapy suppressed the heart rate by 29 beats per minute (P < 0.0025). Assessment of the heart rate responses in the patients with OI was complicated, however, by variable standing times. How, for example, can one compare a standing time of 10 minutes and an average heart rate of 110 in one circumstance (following Drug A, for example) with a standing time of 20 minutes and an average heart rate of 120 on a separate day (following Drug B)? The tachycardia following Drug B may reflect the acceleration of heart rate between 10 minutes and 20 minutes, a time interval that was not even reached when the patient was tested following Drug A. To take both standing time and heart rate into consideration we propose the Orthostatic Index (RR interval versus time area under the curve) and reason that effective therapy would increase the RR interval, prolong the standing time and increase the area under the curve relating these parameters. Suppression of tachycardia is indicative of a corrective effect in patients with POTS where the tachycardia is the consequence of a maldistribution of blood and decreased cardiac filling [12]. Our data suggest that drug-induced suppression of heart rate is similarly a manifestation of a beneficial response in those with OI since lowering the heart rate was associated with increased standing times (Table 2). Patients with orthostatic syncope have gradually increasing heart rates prior to the onset of instability and collapse [8]. We observed this pattern repeatedly in both POTS and OI in the present study. These observations prompted us to consider the RR interval versus time area under the curve (Orthostatic Index) as a measure of orthostatic tolerance that could be used for both groups of patients. We believe this is appropriate since the two disorders share a common pathophysiology; orthostatic stress leads to excessive venous pooling in the lower extremities [14] and splanchnic veins [11, 12, 15] in both. It would be inappropriate, however, to use the Orthostatic Index to assess patients with dizziness or syncope that is unrelated to orthostatic stress.
The second purpose of this study was to compare combination therapy to monotherapy with each agent. This is of practical importance because neither of the drug was effective in all patients. We postulated that combination therapy would be better than monotherapy since midodrine and octreotide act on different vascular beds. Midodrine is a peripheral vasoconstrictor [9], whereas octreotide mainly affects the splanchnic circulation [6]. We thought that a vasoconstrictor effect on both vascular beds would translate into enhanced efficacy but the data did not demonstrate that. Although combination therapy suppressed heart rate more effectively than monotherapy during the first 10 minutes of standing for the patients with POTS (Figure 2) subsequently the heart rates following combination therapy were not different from the heart rates following monotherapy. The orthostatic index was slightly greater following combination versus monotherapy for both POTS and OI but this trend was not statistically significant.
We have previously performed a similar study of octreotide versus midodrine in autonomic neuropathy patients with postprandial hypotension and orthostatic hypotension and a comparison of the two studies is of interest [7]. Octreotide was more potent than midodrine in autonomic neuropathy patients particularly during the postprandial period. Combination therapy was frequently required to prevent orthostatic hypotension. In the present study, midodrine and octreotide showed similar potencies, and combination therapy was not significantly better than monotherapy.
Our data indicate that midodrine and octreotide were similarly effective at suppressing tachycardia in patients with POTS and improving orthostatic tolerance in patients with OI. Subsequent chronic therapy confirmed a previous report indicating that octreotide ameliorated chronic fatigue in patients with OI and POTS [13]. We nevertheless encountered prevalent patient dissatisfaction during this study. Patients with POTS and OI frequently have gastrointestinal complaints, especially abdominal cramps or nausea [1], which may be exacerbated by octreotide. Seven of the 23 original patients could not tolerate octreotide monotherapy and another two patients developed abdominal cramps when given combination therapy. Many patients, however, tolerate chronic octreotide remarkably well and, like patients with acromegaly, are essentially free of adverse effects despite the multiple known effects of the drug on gastrointestinal and endocrine function [10]. The major limitation of octreotide therapy is its expense, which may be prohibitive for those without insurance. A single injection of 50 µg per day is 400 dollars per month. Adverse effects were less severe following midodrine; nevertheless, six of the 23 patients refused chronic midodrine therapy because of scalp itching, chills, dysphoria or headaches. Patients complained that both drugs have short therapeutic effects (two and one-half to three hours). Four of the patients showed a good hemodynamic response to one or more of the treatments offered, but chronic therapy failed to relieve their symptoms. Some of the symptoms of POTS (dizziness, syncope, palpitations, fatigue) stem from hemodynamic instability, which is correctable; other symptoms (insomnia, depression, headaches) may be multi-factorial and difficult to treat.
The strength of this study is that we have compared the effects of octreotide and midodrine on a prolonged orthostatic challenge. Many studies of drug efficacy in patients with POTS and OI have involved only a brief orthostatic stress and failed to measure standing time as has been previously recommended [13]. The limitations to this study must also be acknowledged. First of all, we preselected patients who tolerated octreotide. Second, we did not give placebos since many patients given midodrine develop scalp itching or “gooseflesh” and therefore can distinguish this agent from placebo [7]. Thus it is difficult to blind patients to their therapy in trials involving midodrine. Nevertheless, placebo controlled trials in similar patients have been performed previously and shown efficacy for both midodrine [3] and octreotide [5]. Our purpose was to compare these two agents and to assess combination therapy.
In summary, octreotide and midodrine suppressed tachycardia to a similar extent in patients with POTS. The two drugs improved standing time and the orthostatic index similarly in patients with OI. Combination therapy was not significantly better than monotherapy.
References
Al-Shekhlee A, Lindenberg JR, Hachwi RN, Chelimsky TC (2005) The value of autonomic testing in postural tachycardia syndrome. Clin Auton Res 15:219–222
Benrud-Larson LM, Dewar MS, Sandroni P, Rummans TA, Haythornthwaite JA, Low PA (2002) Quality of life in patients with postural tachycardia syndrome. Mayo Clin Proc 77:531–537
Gordon VM, Opfer-Gehrking TL, Novak V, Low PA (2000) Hemodynamic and symptomatic effects of acute interventions on tilt in patients with postural tachycardia syndrome. Clin Auton Res 10:29–33
Harrell FE Jr (2001) Regression modeling strategies. Springer, New York, pp 413–432
Hoeldtke RD, Davis KM (1991) The orthostatic tachycardia syndrome: evaluation of autonomic function and treatment with octreotide and ergot alkaloids. J Clin Endocrinol Metab 73:132–139
Hoeldtke RD, Davis KM, Joseph J, Gonzales R, Panidis IP, Friedman AC (1991) Hemodynamic effects of octreotide in patients with autonomic neuropathy. Circulation 84:168–176
Hoeldtke RD, Horvath GG, Bryner KD, Hobbs GR (1998) Treatment of orthostatic hypotension with midodrine and octreotide. J Clin Endocrinol Metab 83:339–343
Julu PO, Cooer VL, Hansen S, Hainsworth R (2003) Cardiovascular regulation in the period preceding vasovagal syncope in conscious humans. J Physiol 549:299–311
Low PA, Gilden JL, Freeman R, Sheng K, McElligott MA (1997) Midodrine Study Group. Efficacy of midodrine vs. placebo in neurogenic orthostatic hypotension. JAMA 277:1046–1051
Razzore P, Colao A, Baldelli R, Gaia D, Marzullo P, Ferretti E (1999) Comparison of six months therapy with octreotide versus lanreotide in acromegalic patients: a retrospective study. Clin Endocrinol (Oxf) 51:159–164
Stewart JM, McLeod KJ, Sanyal S, Herzberg G, Montgomery LD (2004) Relation of postural vasovagal syncope to splanchnic hypervolemia in adolescents. Circulation 100:2575
Stewart JM, Medow MS, Glover JL, Montgomery L (2006) Persistent splanchnic hyperemia during upright tilt in postural tachycardia syndrome. Am J Physiol Heart Circ Physiol 290:H665–H673
Streeten DHP, Anderson GH (1992) Delayed orthostatic intolerance. Arch Intern Med 152:1066–1072
Streeten DHP, Anderson GH, Richardson R, Thomas FD (1988) Abnormal orthostatic changes in blood pressure and heart rate in subjects with intact sympathetic nervous function: evidence for excessive venous pooling. J Lab Clin Med 111:326–335
Tani H, Singer W, McPhee BR, Opfer-Gehrking TL, Haruma K, Kajiyama G et al. (2000) Splanchnic-mesenteric capacitance bed in the postural tachycardia syndrome (POTS). Auton Neurosci 86:107–113
Winer BJ (1979) Statistical principles and experimental design, 2nd edn. McGraw Hill, New York, pp 309–603
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hoeldtke, R.D., Bryner, K.D., Hoeldtke, M.E. et al. Treatment of postural tachycardia syndrome: a comparison of octreotide and midodrine. Clin Auton Res 16, 390–395 (2006). https://doi.org/10.1007/s10286-006-0373-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-006-0373-0