Abstract
Complement dysfunction results in impaired ability in clearing apoptotic cell debris that may stimulate autoantibody production in systemic lupus erythematosus (SLE). Herein, we provided a comprehensive search to find and meta-analyze any complement gene polymorphisms associated with SLE. The ITGAM, C1q, and MBL gene polymorphisms were included in this meta-analysis to reveal the exact association with SLE risk. Electronic databases, including Scopus, PubMed, and Google Scholar, were searched to find studies investigating the ITGAM, C1q, and MBL gene polymorphisms and SLE risk in different populations. The pooled odds ratio (OR) and its corresponding 95% confidence interval (CI) were used to analyze the association between ITGAM, C1q, and MBL gene polymorphisms and susceptibility to SLE. According to inclusion criteria, a total of 24 studies, comprising 4 studies for C1QA rs292001, 5 studies for C1QA rs172378, 9 studies for ITGAM rs1143679, 8 studies for MBL rs1800450, 3 studies for MBL2 rs1800451, and 3 studies for MBL2 rs5030737, were included in the final meta-analysis. A significant positive association was found between rs1143679 and SLE risk, while rs1800451 significantly associated with decreased SLE susceptibility. In summary, ITGAM gene rs1143679 SNP and MBL gene rs1800451 SNP were positively and negatively associated with SLE risk, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by autoantibodies production. These autoantibodies are against ubiquitous nuclear antigens and form immune complex deposits. Genetic is one of the crucial components in SLE etiology, as shown by the disease high-risk ratio between monozygotic twins over dizygotic twins [1,2,3]. Genetic deficiency in the complement system results in an increased risk of SLE development by reducing the ability in clearing apoptotic cells that may result in autoantibody production [4,5,6].
C1q is the first component of the classical pathway in complement activation. One of the important functions of C1q is the mediation of the clearance of apoptotic cells with binding to C1q/collectin receptors on phagocytes [7]. C1q is encoded by 3 genes, including C1QA, C1QB, and C1QC, that are harbored by chromosome 1p34.1–36.3 [8]. Mutations or single-nucleotide polymorphisms (SNPs) in C1q genes may result in C1q deficiency [9]. C1q deficiency results in impaired clearance of apoptotic cells and promotes autoreactivity and autoantibody production. Around 93% of individuals with C1q deficiency developed SLE or SLE-like symptoms [10,11,12]. The Integrin-α-M (ITGAM, also known as CD11B), which is located in chromosome 16p11.2, encodes CD11b. The CR3/Mac1/CD11b-CD18 modulates migration, leukocyte adhesion, and also has roles in phagocytosis of apoptotic cells that are coated by complement particles [13]. Variations, such as rs1143679 G/A polymorphism in the ITGAM gene, severely impair the phagocytosis of complement-coated particles [14]. Mannose-binding lectin 2 (MBL2) is located on chromosome 10q11.2–21, and it contains four exons [15]. MBL2 and C1q have similar structures and functions, and their deficiencies cause a higher risk of SLE [16]. There are three SNPs in the exon 1 of MBL2 gene that include codon 52 (allele D: rs5030737), codon 54 (allele B: rs1800450), codon 57 (allele C: rs1800451) [17]. Any of these variants change the functional structure of MBL and results in the absence of functional MBL protein and impairing complement-coated particle clearance [15, 18].
In this systematic review, we performed the first meta-analysis for C1QA SNPs (rs292001, rs172378), MBL2 SNPs (rs1800450, rs1800451, rs5030737) and also updated the last meta-analysis for ITGAM SNP (rs1143679) published in 2015 [19] to disclose an exact conclusion of the association between complement gene polymorphisms and SLE risk.
Methods
Searches and data sources
Herein, we searched the electronic databases, including PubMed, Scopus, and Google Scholar to include all eligible case–control studies between all complement gene polymorphisms and SLE risk up to June 2021. The following keywords were used to search the databases for finding many complement SNPs in SLE patients; (complement) AND (systemic lupus erythematosus OR SLE) AND (polymorphism OR variation OR single-nucleotide OR SNP OR mutation). Among all complement components, six SNPs had enough studies to include in the meta-analysis. The C1qA rs292001 (G > A) and rs172378 (A > G); ITGAM rs1143679 (G > A); MBL rs1800450 (G > A), rs1800451 (G > A) and rs5030737 (C > T) were selected to include in this study. The following keywords used to search each of these SNPs; (C1q OR Complement component 1q); (ITGAM OR Integrin Subunit Alpha M OR CD11b OR Component Receptor 3 OR CR3); (MBL OR Mannose Binding Lectin), AND (systemic lupus erythematosus OR SLE OR, in PubMed, "Lupus erythematosus, Systemic" [Mesh]) AND (polymorphism OR variation OR “single nucleotide” OR SNP OR mutation OR, in PubMed, "Polymorphism, Single Nucleotide" [Mesh]). In Google Scholar, the rs numbers were also used to limit the search results. Only English-language and human populations were included in this study. The protocol of the systematic review has been registered on the PROSPERO (ID: CRD42020170839).
Inclusion and exclusion criteria
The inclusion criteria for this meta-analysis were: (1) case–control studies that evaluate complement gene polymorphisms in SLE; (2) studies with available frequencies and numbers of each allele and different genotypes to calculate odds ratio (OR) and 95% confidence interval (CI); and (3) English-language research papers. The exclusion criteria were: (1) duplication or overlapping subjects and (2) article types of review, letter, and comment.
Data extraction and quality assessment
The following information was extracted: year of publication, first author’s last name, detection method, ethnicity of participants, number of cases and controls with minor A allele of rs292001, minor G allele of rs172378, minor A allele of rs1143679, minor A allele of rs1800450, minor A allele of rs1800451, minor T allele of rs5030737 and also the number of different genotypes for each SNPs in case and control subjects. The Newcastle–Ottawa Scale (NOS) was used for evaluation of methodological quality of included studies [20]. The quality of studies was scored by 0–3, 4–6, or 7–9 as low, moderate, or high quality, respectively.
Statistical methods
For evaluation of the mentioned complement gene polymorphisms and risk of SLE, we used pooled Odds Ratio (OR) as an effect size and its corresponding 95% CI for minor alleles in this meta-analysis. Hardy–Weinberg equilibrium was checked by Chi-squared test in the control group for each SNP. For assessing the heterogeneity and the variation in the pooled estimations, Cochran's Q test and I-squared index were used, respectively [21]. Meta-analysis was assessed with a random-effects model when heterogeneity existed between the individuals with a significant Cochran's Q test (P < 0.1), and the fixed-effects model was used if the heterogeneity was not detected. The Egger’s test and Begg’s test were used to checking the publication bias (P < 0.05) [22]. In addition, the influence of individual studies on the pooled OR (to assess the stability of the results) was calculated with re-estimating and plotting by omitting one of the studies each time (leave-one-out sensitivity analysis). Statistical software (STATA) (version 15.0; Stata Corporation, College Station, Texas 77845 USA) was used for data analysis.
Results
Characteristics of eligible studies
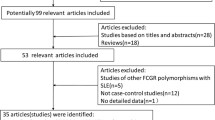
In the initial search, 257, 312, and 310 studies for C1q, ITGAM, and MBL complement SNPs were found, respectively. After removal of irrelevant papers, presentations, seminars, letters, case reports, reviews, non-English papers, duplications, and also with using mentioned criteria, 4 case–control studies comprising 571 cases and 793 healthy subjects for rs292001 [23,24,25,26], 5 case–control studies comprising 1145 cases and 1256 healthy subjects for rs172378 [23, 27,28,29,30], 9 case–control studies comprising 8260 cases and 8753 healthy subjects for rs1143679 [31,32,33,34,35,36,37,38], 8 case–control studies comprising 2006 cases and 2069 healthy subjects for rs1800450 [36, 39,40,41,42,43,44,45], 3 case–control studies comprising 726 cases and 834 healthy subjects for rs1800451 [42,43,44], and 3 case–control studies comprising 726 cases and 834 healthy subjects for rs5030737 [42,43,44] were included for meta-analysis. The papers were investigated in different nations of Asian, European, African, and American countries. The ranges of publication were between 2003 and 2019. The mean NOS score was 7.30 (range: 6–9) (Table 1, Fig. 1).
Main results, subgroup, and sensitivity analysis
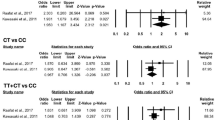
Significant associations were found between two SNPs, including ITGAM gene rs1143679 polymorphism and MBL2 gene rs1800451 polymorphism with SLE risk. The minor A allele of the ITGAM gene rs1143679 was significantly associated with an increased SLE risk (OR = 1.966, 95% CI = 1.757–2.20, P < 0.001). Moreover, the AA (OR = 3.608, 95% CI = 2.76–4.71, P < 0.001) and AG (OR = 1.923, 95% CI = 1.70–2.16, P < 0.001) genotypes significantly increased the disease risk. As such, the dominant (OR = 2.037, 95% C = 1.81–2.29, P < 0.001) and recessive (OR = 3.202, 95% CI = 2.45–4.18, P < 0.001) models of inheritance were significantly associated with increased susceptibility to SLE (Table 2, Fig. 2a). On the other side, the dominant genetic model of MBL2 gene rs1800451 SNP significantly decreased SLE proneness (OR = 0.641, 95% CI = 0.416–0.988, P = 0.044), but the allelic model of this SNP has a non-significant effect on SLE risk (Table 2, Fig. 2b).
Heterogeneity and publication bias
Cochran's Q test and I2 test were conducted for analyzing the heterogeneity of the studies. The (I2% > 50%, PHeterogeneity < 0.10) considered as significant heterogeneity between the studies.
Heterogeneity was observed in C1QA gene rs292001 SNP for the comparisons A versus G (I2% = 65.39%, PHeterogeneity = 0.02) and AA versus GG (I2% = 81.13%, PHeterogeneity = 0.001), GA versus GG (I2% = 54.3%, PHeterogeneity = 0.09), AA + GA versus GG (I2% = 66.2%, PHeterogeneity = 0.03), and AA versus GA + GG (I2% = 76.3%, PHeterogeneity = 0.005). Moreover, for C1QA gene rs172378 SNP, heterogeneity was detected for G versus A (I2% = 55.3%, PHeterogeneity = 0.04) and GG versus AA (I2% = 53.5%, PHeterogeneity = 0.07), GG + AG versus AA (I2% = 62.7%, PHeterogeneity = 0.03). The only comparison that had heterogeneity for ITGAM gene rs1143679 SNP was AG versus GG (I2% = 60.5%, PHeterogeneity = 0.007). On the other side, MBL2 gene rs1800450 SNP demonstrated heterogeneity for comparisons below: A versus G (I2% = 62%, PHeterogeneity = 0.01) and AA versus GG (I2% = 61%, PHeterogeneity = 0.01), AA versus AG + GG (I2% = 63.2%, PHeterogeneity = 0.008) (Table 2).
Assessing of publication bias was done by using a funnel plot, Egger’s and Begg’s tests. The shapes of the funnel plots did not reveal any evidence of an obvious significantly asymmetry in all comparison models. Also, nonsignificant publication bias was found in all analyses by the tests (Table 2, Fig. 3).
Sensitivity analysis
The stability of the meta-analysis was evaluated; as the results suggested, no individual study significantly affected the pooled ORs. The result of leave-one-out sensitivity analysis was shown for the allelic model of ITGAM gene rs1143679 SNP (Fig. 4a) and MBL2 gene rs1800451 SNP (Fig. 4b).
Discussion
SLE is a chronic autoimmune disease in which both genetic and environmental factors are contributed [46, 47]. A bulk of evidence has revealed that complement deficiencies result in a reduced ability in the clearance of apoptotic cells that increase the risk of autoantibody production and, therefore, SLE development in susceptible subjects. The complement system has an intricate role in SLE, and either complement deficiency or aberrant complement activation contributes to SLE risk [4,5,6].
The deficiency or malfunction of several complement proteins has been important in SLE pathogenesis. The C1q component that plays a significant role in the removal of apoptotic cells is associated with SLE. The lupus autoantigens that are located in apoptotic debris may stimulate an inappropriate immune response. C1q can also inhibit the interferon alpha (IFN-α) production via the inhibitory receptor leukocyte-associated immunoglobulin-like receptor 1 (LAIR-1, also called CD305) and, hence, is involved in SLE development [5, 48, 49]. Several studies reported an association between low serum levels of MBL and autoimmune disease development. In SLE patients, MBL deficiency may result in insufficient removal of apoptotic debris same as C1q deficiency. Genetic polymorphisms that are associated with decreased serum levels of MBL as well as the presence of anti-MBL autoantibodies which bind to MBL and decrease its serum level may increase the risk of SLE development [50,51,52,53,54,55]. ITGAM, a component of CR3 or Mac1, is expressed on most myeloid cells, such as macrophages and dendritic cells (DCs). CR3 binds to the complement protein iC3b and mediates the phagocytosis of iC3b-coated particles and, hence, has an important role in the removal of apoptotic cells. Some studies reported other essential roles for CR3 that are also associated with autoimmune responses in SLE patients. Mac1 could inhibit some immunological processes such as DC maturation and function, DC-induced T cell activation, Toll-like receptor (TLR) signaling, and macrophage activation. CR3 deficiency may result in impaired phagocytosis of apoptotic cells, activation of T cells, increased TLR signaling, and Th17 differentiation, which are contributing to the increased systemic inflammation and SLE development [56,57,58,59,60,61].
In the present study, we meta-analyzed the previously published data to attain conclusive outstanding of the genetic associations between the ITGAM (rs1143679), C1QA (rs292001 and rs172378), and MBL (rs1800450, rs1800451, and rs5030737) gene polymorphisms and susceptibility to SLE. The previous meta-analysis in 2015 [19] reported 1.77 pooled OR (95% CI = 1.65–1.90, P < 0.001) for the minor A allele of the ITGAM gene rs1143679 SNP which was also confirmed with our meta-analysis with 1.966 pooled OR (95% CI = 1.757–2.20, P < 0.001). The pooled OR of other genetic comparisons for ITGAM gene rs1143679 SNP reported in the previous meta-analysis was also included in the currently updated meta-analysis.
Some of the previous studies investigating the C1QA gene polymorphisms reported a significant association between these polymorphisms with SLE pathogenesis. Significant ORs that were reported include 1.80 for rs172378 [23] and 1.57 for rs292001 [24]. However, our meta-analysis resulted in no significant pooled ORs for the minor A allele of rs292001 and the minor G allele of rs172378. Some researchers reported significant associations between MBL gene polymorphisms (rs1800450, rs1800451, and rs5030737) with SLE risk [62]. However, others reported no significant association for these SNPs [44]. The current meta-analysis revealed non-significant associations between rs1800450 and rs5030737 SNPs with SLE risk, while a significant protective association was shown for rs1800451 (on the dominant genetic model). Other complement gene polymorphisms that were investigated had not enough data to be analyzed in this meta-analysis.
Conclusion
In summary, this meta-analysis study provides a comprehensive and up-to-date conclusion of the association between the complement SNPs and SLE risk until June 2021. The present meta-analysis revealed that the ITGAM gene rs1143679 SNP significantly increased the SLE risk. However, the dominant genetic model of MBL2 gene rs1800451 SNP was significantly associated with decreased SLE risk. Further studies of different ethnicities are still needed to attain a more comprehensive and conclusive understanding of the association between complement gene SNPs and SLE development.
Availability of data and material
Not applicable.
References
Kelly JA, Moser KL, Harley JB. The genetics of systemic lupus erythematosus: putting the pieces together. Genes Immun. 2002;3(Suppl 1):S71-85. https://doi.org/10.1038/sj.gene.6363885.
Rhodes B, Vyse TJ. The genetics of SLE: an update in the light of genome-wide association studies. Rheumatology (Oxford). 2008;47:1603–11. https://doi.org/10.1093/rheumatology/ken247.
Ebrahymian H, Rezaei R, Mostafaei S, et al. Association study between STAT4 polymorphisms and susceptibility to systemic lupus erythematosus disease: systematic review and meta-analysis. Meta Gene. 2018;16:241–7.
Leffler J, Bengtsson AA, Blom AM. The complement system in systemic lupus erythematosus: an update. Ann Rheum Dis. 2014;73:1601–6. https://doi.org/10.1136/annrheumdis-2014-205287.
Trouw LA, Pickering MC, Blom AM. The complement system as a potential therapeutic target in rheumatic disease. Nat Rev Rheumatol. 2017;13:538–47. https://doi.org/10.1038/nrrheum.2017.125.
Macedo AC, Isaac L. Systemic lupus erythematosus and deficiencies of early components of the complement classical pathway. Front Immunol. 2016;7:55. https://doi.org/10.3389/fimmu.2016.00055.
Eggleton P, Tenner AJ, Reid KB. C1q receptors. Clin Exp Immunol. 2000;120:406–12.
Sellar GC, Blake DJ, Reid KB. Characterization and organization of the genes encoding the A-, B- and C-chains of human complement subcomponent C1q. The complete derived amino acid sequence of human C1q. Biochem J. 1991;274(Pt 2):481–90.
Crispin JC, Liossis SN, Kis-Toth K, et al. Pathogenesis of human systemic lupus erythematosus: recent advances. Trends Mol Med. 2010;16:47–57. https://doi.org/10.1016/j.molmed.2009.12.005.
Walport MJ, Davies KA, Botto MJI. C1q and systemic lupus erythematosus. Immunobiology. 1998;199:265–85.
Pickering MC, Botto M, Taylor PR, Lachmann PJ, Walport MJ. Systemic lupus erythematosus, complement deficiency, and apoptosis. Adv Immunol. 2000;76:227–324.
Botto M, Dell’Agnola C, Bygrave AE, et al. Homozygous C1q deficiency causes glomerulonephritis associated with multiple apoptotic bodies. Nat Genet. 1998;19:56–9. https://doi.org/10.1038/ng0598-56.
Tan SM. The leucocyte beta2 (CD18) integrins: the structure, functional regulation and signalling properties. Biosci Rep. 2012;32:241–69. https://doi.org/10.1042/bsr20110101.
Rhodes B, Furnrohr BG, Roberts AL, et al. The rs1143679 (R77H) lupus associated variant of ITGAM (CD11b) impairs complement receptor 3 mediated functions in human monocytes. Ann Rheum Dis. 2012;71:2028–34. https://doi.org/10.1136/annrheumdis-2012-201390.
Madsen HO, Garred P, Kurtzhals JA, et al. A new frequent allele is the missing link in the structural polymorphism of the human mannan-binding protein. Immunogenetics. 1994;40:37–44.
Garcia-Laorden MI, Rua-Figueroa I, Perez-Aciego P, et al. Mannose binding lectin polymorphisms as a disease-modulating factor in women with systemic lupus erythematosus from Canary Islands. Spain J Rheumatol. 2003;30:740–6.
Jakab L, Laki J, Sallai K, et al. Association between early onset and organ manifestations of systemic lupus erythematosus (SLE) and a down-regulating promoter polymorphism in the MBL2 gene. Clin Immunol. 2007;125:230–6. https://doi.org/10.1016/j.clim.2007.08.020.
Garred P, Larsen F, Madsen HO, Koch C. Mannose-binding lectin deficiency–revisited. Mol Immunol. 2003;40:73–84.
Lee YH, Bae S-C. Association between the functional ITGAM rs1143679 G/A polymorphism and systemic lupus erythematosus/lupus nephritis or rheumatoid arthritis: an update meta-analysis. Rheumatol Int. 2015;35:815–23.
Zeng X, Zhang Y, Kwong JS, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8:2–10.
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11:193.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Radanova M, Vasilev V, Dimitrov T, et al. Association of rs172378 C1q gene cluster polymorphism with lupus nephritis in Bulgarian patients. Lupus. 2015;24:280–9. https://doi.org/10.1177/0961203314555173.
Mosaad YM, Hammad A, Fawzy Z, et al. C1q rs292001 polymorphism and C1q antibodies in juvenile lupus and their relation to lupus nephritis. Clin Exp Immunol. 2015;182:23–34. https://doi.org/10.1111/cei.12666.
Zervou MI, Vazgiourakis VM, Yilmaz N, et al. TRAF1/C5, eNOS, C1q, but not STAT4 and PTPN22 gene polymorphisms are associated with genetic susceptibility to systemic lupus erythematosus in Turkey. Hum Immunol. 2011;72:1210–3.
Yu Y, Zhu C, Zhou S, Chi S. Association between C1q, TRAIL, and Tim-1 gene polymorphisms and systemic lupus erythematosus. Genet Test Mol Biomark. 2018;22:546–53.
Cao C, Li P, Luan H, et al. Association study of C1qA polymorphisms with systemic lupus erythematosus in a Han population. Lupus. 2012;21:502–7.
Racila DM, Sontheimer CJ, Sheffield A, et al. Homozygous single nucleotide polymorphism of the complement C1QA gene is associated with decreased levels of C1q in patients with subacute cutaneous lupus erythematosus. Lupus. 2003;12:124–32. https://doi.org/10.1191/0961203303lu329oa.
Chew CH, Chua KH, Lian LH, Puah SM, Tan SY. PCR-RFLP genotyping of C1q mutations and single nucleotide polymorphisms in Malaysian patients with systemic lupus erythematosus. Hum Biol. 2008;80:83–93. https://doi.org/10.3378/1534-6617(2008)80[83:Pgocma]2.0.Co;2.
Irshaid FI, Birmingham DJ. Cq1 exon polymorphisms in Caucasian and African American systemic lupus erythematosus patients. Pak J Biol Sci. 2018;21:119–26.
Toller-Kawahisa JE, Vigato-Ferreira ICC, Pancoto JAT, et al. The variant of CD11b, rs1143679 within ITGAM, is associated with systemic lupus erythematosus and clinical manifestations in Brazilian patients. Hum Immunol. 2014;75:119–23. https://doi.org/10.1016/j.humimm.2013.11.013.
Skonieczna K, Czajkowski R, Kaszewski S, et al. Genetic similarities and differences between discoid and systemic lupus erythematosus patients within the Polish population. Postepy Dermatologii i Alergologii. 2017;34:228–32. https://doi.org/10.5114/pdia.2017.67479.
Han S, Kim-Howard X, Deshmukh H, et al. Evaluation of imputation-based association in and around the integrin-α-M (ITGAM) gene and replication of robust association between a non-synonymous functional variant within ITGAM and systemic lupus erythematosus (SLE). Hum Mol Genet. 2009;18:1171–80. https://doi.org/10.1093/hmg/ddp007.
Gupta V, Kumar S, Pratap A, et al. Association of ITGAM, TNFSF4, TNFAIP3 and STAT4 gene polymorphisms with risk of systemic lupus erythematosus in a North Indian population. Lupus. 2018;27:1973–9. https://doi.org/10.1177/0961203318786432.
Warchol T, Lianeri M, Lacki JK, Olesinska M, Jagodzinski PP. ITGAM Arg77His is associated with disease susceptibility, arthritis, and renal symptoms in systemic lupus erythematosus patients from a sample of the Polish population. DNA Cell Biol. 2011;30:33–8. https://doi.org/10.1089/dna.2010.1041.
Sanchez E, Webb RD, Rasmussen A, et al. Genetically determined Amerindian ancestry correlates with increased frequency of risk alleles for systemic lupus erythematosus. Arthritis Rheum. 2010;62:3722–9.
Nath SK, Han S, Kim-Howard X, et al. A nonsynonymous functional variant in integrin-α M (encoded by ITGAM) is associated with systemic lupus erythematosus. Nat Genet. 2008;40:152.
Li C, Tong F, Ma Y, et al. Association of the CD11b rs1143679 polymorphism with systemic lupus erythematosus in the Han Chinese population. J Int Med Res. 2018;46:1008–14.
Tsai YC, Yao TC, Kuo ML, Cheng TT, Huang JL. Lack of association of mannose-binding lectin gene polymorphisms with development and clinical manifestations of systemic lupus erythematosus in Chinese children. Lupus. 2009;18:372–6. https://doi.org/10.1177/0961203308099326.
Takahashi R, Tsutsumi A, Ohtani K, et al. Association of mannose binding lectin (MBL) gene polymorphism and serum MBL concentration with characteristics and progression of systemic lupus erythematosus. Ann Rheum Dis. 2005;64:311–4. https://doi.org/10.1136/ard.2003.020172.
Panda AK, Parida JR, Tripathy R, et al. Low producer MBL genotypes are associated with susceptibility to systemic lupus erythematosus in Odisha. India. 2013;74:114–9.
Negi VS, Devaraju P, Misra DP, et al. Mannose-binding lectin (MBL) codon 54 (rs1800450) polymorphism predisposes towards medium vessel vasculitis in patients with systemic lupus erythematosus. Clin Rheumatol. 2017;36:837–43.
Hristova M, Dourmishev L, Kamenarska Z, et al. MBL 2 polymorphisms–manifestations in Bulgarian patients with adult dermatomyositis and systemic lupus erythematosus. Int J Immunogenet. 2014;41:119–25.
Ho Lee Y, Witte T, Momot T, et al. The mannose-binding lectin gene polymorphisms and systemic lupus erythematosus: two case–control studies and a meta-analysis. Arthritis Rheum. 2005;52:3966–74.
Huang Y, Wang W, Han J, et al. Increased frequency of the mannose-binding lectin LX haplotype in Chinese systemic lupus erythematosus patients. Eur J Immunogenet. 2003;30:121–4.
Invernizzi P, Gershwin ME. The genetics of human autoimmune disease. J Autoimmun. 2009;33:290–9. https://doi.org/10.1016/j.jaut.2009.07.008.
Boscolo P, Youinou P, Theoharides TC, Cerulli G, Conti P. Environmental and occupational stress and autoimmunity. Autoimmun Rev. 2008;7:340–3. https://doi.org/10.1016/j.autrev.2007.12.003.
Son M, Diamond B. C1q-mediated repression of human monocytes is regulated by leukocyte-associated Ig-like receptor 1 (LAIR-1). Mol Med. 2015;20:559–68. https://doi.org/10.2119/molmed.2014.00185.
Fouët G, Bally I, Chouquet A, et al. Molecular basis of complement C1q collagen-like region interaction with the immunoglobulin-like receptor LAIR-1. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms22105125.
Monticielo OA, Mucenic T, Xavier RM, Brenol JC, Chies JA. The role of mannose-binding lectin in systemic lupus erythematosus. Clin Rheumatol. 2008;27:413–9. https://doi.org/10.1007/s10067-008-0838-8.
Seelen MA, Trouw LA, van der Hoorn JW, et al. Autoantibodies against mannose-binding lectin in systemic lupus erythematosus. Clin Exp Immunol. 2003;134:335–43. https://doi.org/10.1046/j.1365-2249.2003.02274.x.
Seelen MA, van der Bijl EA, Trouw LA, et al. A role for mannose-binding lectin dysfunction in generation of autoantibodies in systemic lupus erythematosus. Rheumatology (Oxford). 2005;44:111–9. https://doi.org/10.1093/rheumatology/keh417.
Garred P, Voss A, Madsen HO, Junker P. Association of mannose-binding lectin gene variation with disease severity and infections in a population-based cohort of systemic lupus erythematosus patients. Genes Immun. 2001;2:442–50. https://doi.org/10.1038/sj.gene.6363804.
Malhotra R, Wormald MR, Rudd PM, et al. Glycosylation changes of IgG associated with rheumatoid arthritis can activate complement via the mannose-binding protein. Nat Med. 1995;1:237–43. https://doi.org/10.1038/nm0395-237.
Tsutsumi A, Ikegami H, Takahashi R, et al. Mannose binding lectin gene polymorphism in patients with type I diabetes. Hum Immunol. 2003;64:621–4. https://doi.org/10.1016/s0198-8859(03)00054-5.
Fagerholm SC, MacPherson M, James MJ, Sevier-Guy C, Lau CS. The CD11b-integrin (ITGAM) and systemic lupus erythematosus. Lupus. 2013;22:657–63. https://doi.org/10.1177/0961203313491851.
Rhodes B, Fürnrohr BG, Roberts AL, et al. The rs1143679 (R77H) lupus associated variant of ITGAM (CD11b) impairs complement receptor 3 mediated functions in human monocytes. Ann Rheum Dis. 2012;71:2028–34. https://doi.org/10.1136/annrheumdis-2012-201390.
Wang L, Gordon RA, Huynh L, et al. Indirect inhibition of Toll-like receptor and type I interferon responses by ITAM-coupled receptors and integrins. Immunity. 2010;32:518–30. https://doi.org/10.1016/j.immuni.2010.03.014.
Varga G, Balkow S, Wild MK, et al. Active MAC-1 (CD11b/CD18) on DCs inhibits full T-cell activation. Blood. 2007;109:661–9. https://doi.org/10.1182/blood-2005-12-023044.
Ehirchiou D, Xiong Y, Xu G, et al. CD11b facilitates the development of peripheral tolerance by suppressing Th17 differentiation. J Exp Med. 2007;204:1519–24. https://doi.org/10.1084/jem.20062292.
Fagerholm SC, Varis M, Stefanidakis M, Hilden TJ, Gahmberg CG. alpha-Chain phosphorylation of the human leukocyte CD11b/CD18 (Mac-1) integrin is pivotal for integrin activation to bind ICAMs and leukocyte extravasation. Blood. 2006;108:3379–86. https://doi.org/10.1182/blood-2006-03-013557.
Monticielo O, Chies J, Mucenic T, et al. Mannose-binding lectin gene polymorphisms in Brazilian patients with systemic lupus erythematosus. Lupus. 2010;19:280–7.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
HE, and SA obtained the data, interpreted the data, drafted the article, and gave final approval to the article. EF and AJ conceived and designed the study, interpreted the data, revised the article critically, and gave final approval to the article. SM, STF, and MM conceived and designed the study, analyzed and interpreted the data, revised the article critically, and gave final approval to the article.
Corresponding authors
Ethics declarations
Conflict of interest
None.
Ethics approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ebrahimiyan, H., Mostafaei, S., Aslani, S. et al. Association between complement gene polymorphisms and systemic lupus erythematosus: a systematic review and meta-analysis. Clin Exp Med 22, 427–438 (2022). https://doi.org/10.1007/s10238-021-00758-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-021-00758-0