Abstract
Background
The incidence of surgical site infection (SSI) following stoma reversal can reach 40 %. A recent variation on primary linear closure (PLC) is purse-string approximation (PSA), where the skin is approximated via a purse-string suture but not closed. The optimal technique remains to be determined. The objective of this review was to compare outcomes with PLC versus PSA for skin closure following stoma reversal.
Methods
A literature search of Embase and Medline was performed to identify studies comparing PLC with PSA published between 1966 and 2012. Reviews of each study were conducted and data extracted. Random-effects methods were used to combine data, and between-study heterogeneity was assessed.
Results
Six out of 47 identified studies met the inclusion criteria: 2 randomized controlled trials and 4 case controlled series. For the primary outcome of SSI rate, 233 patients in the PLC and 170 patients in the PSA group were available for comparison. PSA resulted in a reduced rate of SSI (2.4 % PSA vs. 29.6 % PLC; OR 0.083, 95 % CI = 0.03–0.21, p < 0.001). No differences were noted in length of hospital stay. Three studies assessed self-reported cosmetic results at a minimum of 7 months post-operatively. Patients who underwent PSA reported greater satisfaction with the cosmetic outcome (Standard mean difference = 0.47 on ten-point scale, 95 % CI 0.15–0.79, p = 0.005).
Conclusions
Purse-string approximation of stoma wounds is associated with an 80 % reduction in SSI with no negative effect on length of hospital stay or long-term cosmetic outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of a temporary defunctioning stoma is common in colorectal surgery, predominantly following low anterior resection for rectal cancer. This strategy results in reduced rates of re-operation and a lower clinical leak rate [1]. A national audit of surgery for rectal cancer in Spain between 2006 and 2009 demonstrated the use of a temporary stoma in 36 % of cases [2]. However, the operations for reversal of temporary stomas are associated with substantial rates of morbidity, with major complication rates as high as 5 % [3, 4].
Primary wound closure following stoma reversal is associated with high rates of surgical site infection (SSI) with reported rates varying widely between 2 and 40 % [3–6]. A variety of methods have been employed in an attempt to reduce the SSI rate with most involving some form of partial closure. A number of single institution studies have reported low SSI rates with this approach [7–9].
Banerjee [10] described a refined technique of partial wound closure following stoma takedown. After fascial closure, the circular skin incision made around the stoma is drawn in using a purse-string suture placed in the dermal layer. This provides a route for drainage of wound contaminants but also provides a greater degree of wound apposition therefore expediting wound closure when compared to healing by secondary intention alone. The first prospective evaluation of this technique reported no SSIs in a consecutive series of 51 patients [11]. A number of studies have directly compared outcomes of purse-string approximation (PSA) to primary linear closure (PLC) for skin closure following stoma reversal. We performed a review of all studies comparing PLC with PSA. Our primary aim was to assess differences in SSI rates between the two wound closure techniques.
Materials and methods
Identification of studies
MEDLINE and EMBASE were searched between January 1966 and August 2012 for all studies comparing PLC and PSA by entering the following in the search algorithm: purse OR purse-string AND stoma OR ileostomy OR colostomy. The abstracts of the American Society of Colon and Rectal Surgeons, the Association of Coloproctology of Great Britain and Ireland, the European Society of Coloproctology and the Tripartite meetings from 2000 to 2012 were screened for relevant, unpublished studies. Finally, the search included the Current Controlled Trials Register (http://www.controlled-trials.com) and the Cochrane Database of Controlled Trials. The latest search was done on 29 August 2012. Two authors (DMC and JB) independently examined the title and abstract of citations, and the full texts of potentially eligible trials were obtained. Disagreements were resolved by discussion. The reference list of retrieved papers was further screened for additional publications. When data were unclear or incomplete, the corresponding author was contacted to clarify data extraction.
Eligibility criteria
Only studies that compared PLC and PSA for wound closure in adult patients were eligible for inclusion. The primary endpoint of this meta-analysis was the rate of SSI following wound closure. The secondary endpoints examined were length of post-operative hospital stay and patient reported cosmetic outcome.
Data extraction and outcomes
The following information regarding each eligible trial was recorded: authors’ names, journal, year of publication and study design. The following information was recorded from both arms of each eligible trial: the number of patients assigned to each wound closure technique, and the number analysed per arm, mean age, duration of follow-up, SSI rate as well as data on the secondary outcomes mentioned.
Statistical analysis
Data from eligible trials were entered into a computerized spreadsheet for analysis. Analyses were conducted using Statsdirect version 2.5.6 (StatsDirect Ltd, Chesire, UK) and Comprehensive Meta-analysis version 2 (Biostat Inc, NJ, USA). All pooled outcome measures were determined using a random-effects model as described by DerSimonian and Laird [12]. The odds ratio (OR) was estimated with its variance and 95 % confidence interval (CI). The random-effects analysis weighted the natural logarithm of each study’s OR by the inverse of its variance plus an estimate of the between-study variance in the presence of between-study heterogeneity. Standard mean difference was calculated for the effect size of PSA on the continuous variables of length of hospital stay and cosmetic outcome. Heterogeneity between relative risks for the same outcome between different studies was assessed by use of the I 2 inconsistency test and chi-square-based Cochran’s Q statistic [13] test in which p < 0.05 is taken to indicate the presence of significant heterogeneity. The quality of included studies was assessed by using the Newcastle-Ottawa Scale [14]. Quality was evaluated by examining 3 items: patient selection, comparability of the 2 study groups and assessment of exposure (maximum score 9).
Results
Eligible studies
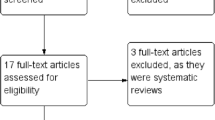
The literature search identified 4 published articles that directly compared PLC and PSA for wound closure following elective stoma reversal [6, 15–17]. Two additional unpublished studies were identified in abstract form from conference proceedings [18, 19]. Figure 1 shows the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart for the literature search. Forty-one papers were excluded from the review including one that exclusively studied a paediatric population [20]. Table 1 demonstrates the demographic data from each trial, which was similar between groups. The trials were well matched for age, sex and body mass index (BMI). There was one published randomised control trial identified as relevant (Jadad score 3 points) [15]. One of the studies identified through the search of conference proceedings and only published in abstract format to date was also a randomised control trial (Jadad score 3 points) [19]. Five of the studies examined procedures for ileostomy reversal only [6, 15, 17–19]. In the study by Marquez et al. [16], 27 % of procedures involved a midline laparotomy with 10 of the 78 reversal procedures performed for colostomy reversal.
All studies used intravenous antibiotics at induction of anaesthesia. Table 2 records aspects of the peri-operative management in the included studies. While the type and post-operative duration of antibiotic regimens differed between the various studies, apart from one patient in the study by Marquez et al. who did not receive antibiotics, the antibiotic use in the two arms of each trial was the same. A variety of suture materials, both absorbable and non absorbable, were used in both the PLC and PSA groups in the different studies. All subjects were enroled between 2002 and 2010, and all papers used the Centres for Disease Control (CDC) definition of SSI [21].
Primary outcome: SSI
The total number of patients assigned to treatment in the 6 studies was 403, 233 in the PLC and 170 in the PSA groups. On random-effects analysis, there was a marked reduction in SSI in patients who underwent PSA wound closure (2.4 % PSA vs. 29.6 % PLC; OR 0.083, 95 % CI = 0.03 to 0.21, p < 0.001) (Fig. 2). There was no evidence of statistical heterogeneity (Cochran Q = 2.80; p = 0.73, I 2 = 0 %).
Meta-analyses for surgical site infection (SSI) after stoma reversal. Each study is shown by the point estimate of the odds ratio (OR; square proportional to the weight of each study) and 95 % confidence interval (CI) for the OR (extending lines); the combined ORs and 95 % CIs by random-effects calculations are shown by a diamond. The arrows indicate that the 95 % CI extends beyond the depicted range. n = 403, Cochran Q: 2.8 (df: 5) p = 0.73, I 2: 0.0 %. PLC primary linear closure, PSA purse-string approximation
Secondary outcomes
Five studies examined length of hospital stay and did not identify a significant difference between the two wound closure techniques (SMD = 0.016 days shorter stay with PSA; 95 % CI = −0.52 to 0.49, p = 0.95) (Fig. 3). However, there was evidence of significant heterogeneity amongst the included studies: Cochran Q: 17.1, p = 0.002, I 2: 76.6 %.
Three studies examined patient self-reported assessment of cosmetic outcome using a visual analogue scale from 1 to 10, at a minimum of 7 months following the reversal procedure (range 7–25 months), comparing 73 patients in the PLC group to 78 patients in the PSA group (Fig. 4). Patients who had undergone skin closure with PSA reported a higher satisfaction with cosmetic outcome at long-term follow-up (SMD = 0.469, 95 % CI 0.15–0.79, p = 0.005). There was no evidence of statistical heterogeneity (Cochran Q: 0.7, p = 0.70, I 2: 0.0 %).
Discussion
This analysis of 6 trials comparing wound closure techniques following stoma reversal represents a summation of the available evidence to date and is the first of its kind. SSI following stoma reversal was markedly reduced when purse-string approximation was used for wound closure with no differences noted in length of hospital stay and, in the long term, an improved self-reported cosmetic outcome.
A previous systematic review of 6107 defunctioning ileostomy reversal procedures by Chow et al. [3] reported a SSI rate of 5.0 %; however, multiple variations in wound closure were employed. Primary closure of these wounds has been associated with SSI rates of up to 40 % [6]. Over recent years, numerous efforts have been made to reduce SSI following stoma reversal. A number of studies have shown reduced SSI when the wound is left open to heal by secondary intention, yet these do not assess the overall time for wound healing and any resultant negative impact on patient quality of life during the period required for wound closure [7, 22, 23]. Other novel techniques have fared little better with randomised controlled trials showing no improvement in SSI rate with the subcutaneous implantation of a gentamicin sponge [24] and, counter intuitively, an increased SSI rate with delayed primary closure [25].
Partial wound closure represents a refinement of healing by secondary intention. It allows partial wound edge apposition to expedite healing time but with an acceptably low SSI rate [7, 26]. The technique described by Banerjee [10] recommends placement of the purse-string suture into the dermis and is easily learned. Circumferential placement of the suture allows uniform tension throughout the wound edges. Skin from the entire diameter of the wound is recruited without the need to excise healthy skin that may be required to make the wound elliptical to facilitate primary closure [27].
The three studies that assessed cosmesis did so at a minimum of 7 months following surgery and while the results suggest an improved satisfaction with the final scar with PSA. This arm of the analysis only included 73 patients in the PLC group and 78 patients in the PSA group. Due to these small numbers, adoption of the PSA technique solely in the hope that it offers a better cosmetic outcome cannot be recommended, but these pooled results suggest the technique is not associated with an inferior cosmetic outcome. Previous studies of patients with circular incisions closed this way suggest that while the initial circular scar may be disconcerting [28], maturation overtime occurs along natural skin tension lines producing a cosmetically acceptable scar [28, 29].
Critics of a partial closure technique such as purse-string approximation will point to the time required to achieve a healed wound. Reid et al. [15] found the meantime to healing in the PSA group was 21 days, yet this was still marginally shorter than the meantime in the PLC group (25 days) due to the effect of the large proportion of PLC patients that developed SSI. The paper by Sutton et al. [11] concurs with the short period of wound healing reported by Reid et al. [15]. If reproduced in other trials, this is of an acceptably short duration. In this pooled analysis of 233 patients in the PLC group, 70 % of patients did not develop any wound sepsis and thus had no requirement for prolonged wound dressing. Therefore, the quality of life-related effects that an open wound has on patients should be one area considered for further investigation.
Despite the conclusive findings with regard to SSI, this review is limited by the quality of the data available. Only two studies were randomised, and all of the included studies were single centre. While antibiotic regimens and choice of suture material differed between the trials, they did not differ between the arms in each individual trial, so this is unlikely to be a significant confounding factor. There are no trials comparing PSA to other methods of partial closure which is a potential area of further study. However, a major benefit of the purse-string technique when compared to other forms of partial closure is that the technique is standardised and easily reproducible.
Conclusions
Further studies, ideally randomised controlled and multi-centre, should address issues regarding quality of life during the time required for post-operative dressings as well as time required for healing before the PSA technique can confidently be recommended as the standard of care. Despite these limitations, it can be concluded from this review that PSA is superior to primary linear skin closure following stoma reversal due to low rates of SSI with no negative impact on long-term cosmetic outcome.
References
Tan WS, Tang CL, Shi L, Eu KW (2009) Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg 96:462–472
Biondo S, Kreisler E, Fraccalvieri D et al (2012) Risk factors for surgical site infection after elective resection for rectal cancer. A multivariate analysis on 2131 patients. Colorectal Dis 14:e95–e102
Chow A, Tilney HS, Paraskeva P, Jevarajah S, Zacharakis E, Purkavastha S (2009) The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis 24:711–723
Luglio G, Pendlimari R, Holubar SD, Cima RR, Nelson H (2011) Loop ileostomy reversal after colon and rectal surgery: a single institutional 5-year experience in 944 patients. Arch Surg 146:1191–1196
Khoo RE, Cohen MM, Chapman GM, Jenken DA, Langevin JM (1994) Loop ileostomy for temporary fecal diversion. Am J Surg 167:519–522
Milanchi S, Nasseri Y, Kidner T, Fleshner P (2009) Wound infection after ileostomy closure can be eliminated by circumferential subcuticular wound approximation. Dis Colon Rectum 52:469–474
Wong KS, Remzi FH, Gorgun E et al (2005) Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patients. Dis Colon Rectum 48:243–250
Phang PT, Hain JM, Perez-Ramirez JJ, Madoff RD, Gemlo BT (1999) Techniques and complications of ileostomy takedown. Am J Surg 177:463–466
van de Pavoordt HD, Fazio VW, Jagelman DG, Lavery IC, Weakley FL (1987) The outcome of loop ileostomy closure in 293 cases. Int J Colorectal Dis 2:214–217
Banerjee A (1997) Purse string skin closure after stoma reversal. Dis Colon Rectum 40:993–994
Sutton CD, Williams N, Marshall LJ, Lloyd G, Thomas WM (2002) A technique for wound closure that minimizes sepsis after stoma closure. ANZ J Surg 72:766–767
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Lau J, Ioannidis JP, Schmid CH (1997) Quantitative synthesis in systematic reviews. Ann Intern Med 127:820–826
Mahid SS, Hornung CA, Minor KS, Turina M, Galadiuk S (2006) Systematic reviews and meta-analysis for the surgeon scientist. Br J Surg 93:1315–1324
Reid K, Pockney P, Pollitt T, Draganic B, Smith SR (2010) Randomized clinical trial of short-term outcomes following purse-string versus conventional closure of ileostomy wounds. Br J Surg 97:1511–1517
Marquez TT, Christoforidis D, Abraham A, Madoff RD, Rothenberger DA (2010) Wound infection following stoma takedown: primary skin closure versus subcuticular purse-string suture. World J Surg 34:2877–2882
Lee JR, Kim YW, Sung JJ et al (2011) Conventional linear versus purse-string skin closure after loop ileostomy reversal: comparison of wound infection rates and operative outcomes. J Korean Soc Coloproctol 27:58–63
Younis J, Chowdhury Y, Scott HJ (2011) Purse-string closure versus conventional primary linear closure of ileostomy wounds. Colorectal Dis 13(Supp 5):87
Camacho-Mauries D, Rodriguez J, Salgado-Nesme N, Vergara O, Gonzalez Q (2012) Randomized clinical trial that demonstrates the elimination of wound infection following pursestring versus conventional closure of ostomy wounds. (ASCRS Annual Meeting 2012). Dis Colon Rectum 55:e114
Ortqvist L, Almström M, Ojmyr-Joelsson M, Wigander H, Währner A, Wester T (2011) Cosmetic and functional outcome after stoma site skin closure in children. Pediatr Surg Int 27:1123–1126
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for prevention of surgical-site infection, 1999. Infect Control Hosp Epidemiol 20:250–278
Hackam DJ, Rotstein OD (1995) Stoma closure and wound infection: an evaluation of risk factors. Can J Surg 38:144–148
Vermulst N, Vermeulen J, Hazebroek EJ, Coene PP, van der Harst E (2006) Primary closure of the skin after stoma closure. Management of wound infections is easy without (long-term) complications. Dig Surg 23:255–258
Haase O, Raue W, Böhm B, Neuss H, Scharfenberg M, Schwenk W (2005) Subcutaneous gentamycin implant to reduce wound infections after loop-ileostomy closure: a randomized, double-blind, placebo-controlled trial. Dis Colon Rectum 48:2025–2031
Lahat G, Tulchinsky H, Goldman G, Klauzner JM, Rabau M (2005) Wound infection after ileostomy closure: a prospective randomized study comparing primary closure vs. delayed primary closure techniques. Tech Coloproctol 9:206–208
Mirbagheri N, Dark J, Skinner S (2012) Factors predicting stomal wound closure infection rates. Tech Coloproctol PMID: 23076288. doi:10.1007/s10151-012-0908-4
Patel KK, Telfer MR, Southee R (2003) A “round block” purse-string suture in facial reconstruction after operations for skin cancer surgery. Br J Oral Maxillofac Surg 41:151–156
Cohen PR, Martinelli PT, Schulze KE, Nelson BR (2007) The purse-string suture revisited: a useful technique for the closure of cutaneous surgical wounds. Int J Dermatol 46:341–347
Tremolada C, Blandini D, Beretta M, Mascetti M (1997) The “round block” purse-string suture: a simple method to close skin defects with minimal scarring. Plast Reconstr Surg 100:126–131
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McCartan, D.P., Burke, J.P., Walsh, S.R. et al. Purse-string approximation is superior to primary skin closure following stoma reversal: a systematic review and meta-analysis. Tech Coloproctol 17, 345–351 (2013). https://doi.org/10.1007/s10151-012-0970-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-012-0970-y