Abstract
Background
Circulating tumor cells (CTCs) have been shown to be associated with the response to neoadjuvant chemotherapy (NCT) and the prognosis of locally advanced breast cancer (LABC) patients. Our study aimed to investigate whether the change of CTC status during NCT could serve as a supplement to the Response Evaluation Criteria in Solid Tumors (RECIST) in the treatment and evaluation of LABC patients.
Methods
6 ml of blood samples were collected before NCT, after the first cycle of NCT and after the completion of NCT, respectively. According to the change of CTC number during NCT, the patients were divided into “CTC low-response (low-R)” group and “CTC high-response (high-R)” group. Survival data of each group of patients were obtained through long-term follow-up.
Results
A total of 35 patients diagnosed with LABC were enrolled. The median follow-up for distant metastasis was 27 months (range 7–36 months). There was no significant difference in distant metastasis-free survival (DMFS) between PR/CR group and PD/SD group (P = 0.0914), while CTC low-R group had a worse DMFS than CTC high-R group (P = 0.0199). In PR/CR subgroup, patients with CTC low-R showed a lower DMFS compared with those with CTC high-R (P = 0.0159). However, in PD/SD subgroup, there was no significant difference in DMFS between CTC low-R and CTC high-R group (P = 0.7521). In terms of assessing response to NCT, CTC change or RECIST classification alone had an AUC of 0.533 (95% CI 0.277–0.790) and 0.700 (95% CI 0.611–0.789), respectively. When combining the two, the AUC slightly increased to 0.713 (95% CI 0.532–0.895).
Conclusion
The change of CTC number during NCT has a potential to serve as a supplement to RECIST in the assessment of NCT efficacy and the prognosis of LABC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Locally advanced breast cancer (LABC) includes primary tumors larger than 5 cm, fused or fixed axillary lymph nodes, ipsilateral infraclavicular, supraclavicular or internal mammary lymph-node metastasis, or tumor invasion of chest wall or skin, which, however, has not been clinically demonstrated presenting distant metastasis [1]. LABC often has a poor prognosis due to the incidence of distant metastasis, although active therapeutic measures are applied [1]. Despite different therapeutic methods have been used in clinical studies for LABC, neoadjuvant chemotherapy (NCT) is still the standard treatment for LABC to obtain the chance to receive operation and better survival [2,3,4,5]. Nevertheless, complete pathologic response (pCR) was achieved in only a few patients with NCT because of multiple factors, such as heterogeneity of tumors [5, 6]. Although results from the NeoSphere trial showed that patients who achieved pCR after NCT had better progression-free survival than patients who did not (85% vs. 76%), it is worth noting that 15% of pCR patients still developed progresses within 5 years, which is not very satisfactory [7]. Therefore, it can be assumed that in addition to pCR, there are some other factors that affect the prognosis of breast cancer patients.
The Response Evaluation Criteria in Solid Tumors (RECIST), which is published in 2000 and revised in 2009, has been widely applied in the assessment of therapeutic response based on tumor shrinkage visible on imageological examination [8,9,10]. RECIST can help evaluate the efficacy of NCT and prognosis for multiple tumors, such as osteosarcoma, rectal cancer, and LABC [11,12,13,14]. However, RECIST still has relatively limited application value in assessing the response to NCT and predicting OS and RFS among LABC patients [15]. This assessment method sometimes underestimates or overestimates the residual neoplasm after NCT [16]. In addition, the evaluation value of RECIST for the efficacy of neoadjuvant chemotherapy varies among different molecular subtypes of breast cancer [14]. Therefore, the efficacy of RECIST alone in evaluating chemotherapy responses of breast cancer may not be reliable enough.
Circulating tumor cells (CTCs), one of the materials used in “liquid biopsy”, have been considered as the “seeds” of distant metastasis and an important predictor of prognosis of breast cancer [17]. In patients with large operable or LABC, detection of CTCs before or after NCT was an independent predictive factor for early metastatic relapse [18]. Furthermore, detection of one or more CTCs per 7.5 ml of blood was related to worse overall survival (OS) and distant metastasis-free survival (DMFS) in nonmetastatic breast cancer patients [19]. Another study showed that five or more CTCs detected after NCT indicated a lower relapse-free survival (RFS) and OS than less CTCs detected after NCT in triple-negative breast cancer (TNBC) patients who have not achieved pCR [20]. However, whether the change in CTCs before and after NCT can accurately predict the response to NCT and the prognosis of breast cancer is still controversial. A Meta-analysis in 2014 showed that there was no significant correlation between change in the number of CTCs during NCT and pCR rate [21]. In a recent study, the relationship between CTC status before and after NCT was found to be associated with objective response rate (ORR) but not pCR rate in early invasive breast cancer patients, indicating a potential association between CTC status and chemotherapy efficacy [22].
For patients with LABC, preoperative evaluation of the efficacy of NCT is extremely important in clinical practice. Therefore, it is necessary to seek an effective and accurate method for clinical evaluation of NCT response and prognosis of LABC. Since RECIST as an assessment method may not be reliable enough, this retrospective study aimed to apply the change of CTC number during NCT as a supplement to RECIST to compensate for the deficiency of evaluation via imaging methods alone.
Patients and methods
Patients
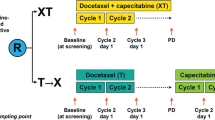
We selected patients who were diagnosed with LABC and underwent NCT. Those without available data about RECIST or Miller–Payne (M–P) grade and distant metastasis were excluded. All patients agreed to be enrolled in this study and written informed consents were obtained. This study has been approved by Institutional Review Boards of the First Affiliated Hospital with Nanjing Medical University. A total of 35 patients who were diagnosed with LABC at the First Affiliated Hospital of Nanjing Medical University from October 2016 to November 2017 were enrolled. All patients were diagnosed with breast cancer by needle biopsies and were staged as LABC. Prior to surgery, these patients were given an EC-T chemotherapy regimen (epirubicin 90 mg/m2 ivd d1, cyclophosphamide 600 mg/m2 ivd d1 on a 21 days cycle for four cycles, and then docetaxel 80 mg/m2 ivd d1, on a 21 days cycle for subsequent four cycles). For human epidermal growth factor receptor-2 (HER-2) positive patients, trastuzumab was used in the last four cycles of chemotherapy. After a total of eight cycles of NCT, all patients underwent surgery. Pathologic and immunohistochemical results (including histological type, ER status, PgR status, HER-2 status, Ki-67 before NCT, Ki-67 after NCT, lymph-node metastasis, histological grade and Miller–Payne grade) were determined by the Pathology Department of the First Affiliated Hospital with Nanjing Medical University. Patients underwent breast magnetic resonance (MR) examination before the first cycle of after the last cycle of neoadjuvant chemotherapy to obtain RECIST grades.
Detection method of CTC
6 ml of blood samples were collected before NCT, after the first cycle of NCT and after the completion of NCT (before operation) for CTC detection, respectively. The detection of CTC was realized using the subtraction enrichment (SE) and immunostaining-FISH, i•FISH® platform, which has been reported previously [23]. We completed all the experiments strictly following the operating instructions (Cytelligen, San Diego, CA, USA). Detailed experimental methods and procedures were reported in our previous studies [24].
Patient grouping
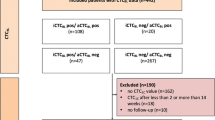
According to RECIST, all enrolled patients were divided into progressive disease (PD)/stable disease (SD) group and partial response (PR)/complete response (CR) group. High response of CTC number to NCT (“CTC high-R”) was defined as the number of CTC after completion of NCT decreased ≥ 33.33% compared with that before NCT or ≥ 66.67% compared with that after the first cycle of NCT. The remaining cases were defined as low response of CTC number to NCT (“CTC low-R”). According to this criterion, the patients were divided into CTC low-R group and CTC high-R group. Based on the combination of the above two grouping criteria, we further divided the patients into four groups: PD/SD + CTC low-R, PD/SD + CTC high-R, PR/CR + CTC low-R and PR/CR + CTC high-R. The M–P grading system after the surgery was used to assess the response to NCT. According to this grading system, patients were divided into M–P 1–3 group and M–P 4–5 group, which suggested that the response to NCT was poor and good respectively.
Statistical analysis
Fisher’s exact test was applied to analyze the relationship between clinical characteristics and the response of CTC number to NCT or RECIST classification. Continuous variables were represented by median, range and interquartile range (IQR). Kruskal–Wallis test was used to compare differences in continuous variables. Survival curves were drawn via the Kaplan–Meier method and differences in survival curves between groups were analyzed by log-rank test. Hazard ratio (HR) and 95% confidence interval (CI) were calculated using Cox proportional hazard model. The receiver-operating characteristic (ROC) curve and area under curve (AUC) were acquired using MedCalc version 19.5.6. Except for ROC and AUC, the rest of statistical analysis was implemented through Stata version 16.0 and GraphPad Prism version 8.3.0. The level of significance was set at 0.05 and a P value < 0.05 was considered to be statistically significant.
Results
Clinical characteristics of enrolled patients
From October 2016 to November 2017, a total of 35 LABC patients receiving NCT were enrolled in this retrospective study. The clinical characteristics of patients according to the response of CTC number to NCT and RECIST classification are summarized in Table 1. The median age of enrolled patients is 50 years (IQR 41–58 years). The mean number of CTCs before NCT for all enrolled patients was 7.2. 19 patients (54.3%) showed high response of CTC number to NCT, while the other 16 (45.7%) showed low response. 23 patients (65.7%) achieved imaging remission (PR or CR) according to RECIST, while the rest (34.3%) did not (SD or PD). As shown in Table 1, the response of CTC number to NCT and RECIST classification were not significantly related to age, ER status, PgR status, HER-2 status, Ki-67 level before NCT, Ki-67 level after NCT, lymph-node metastasis, histological grade and Miller–Payne grade.
The changing trend of CTC number in the enrolled patients from before NCT, after the first cycle of NCT to after completion of NCT
Figure 1 shows the overall trend of CTC number from before NCT, after the first cycle of NCT, to after the completion of NCT in the enrolled patients. The number of CTCs after the first cycle of NCT was significantly higher than that before NCT (Kruskal–Wallis test, P = 0.0001). Although the number of CTCs after completion of NCT showed a downward trend compared with that after the first cycle of NCT, the difference was not statistically significant (Kruskal–Wallis test, P = 0.0752). In addition, CTC number after completion of NCT was significantly higher than before NCT (Kruskal–Wallis test, P = 0.0042) in the general population.
The overall trend of CTC number from before NCT, after the first cycle of NCT, to after the completion of NCT in the enrolled patients. The number of CTCs showed a trend of increasing first and then decreasing at these three time points. CTC number after the first cycle and completion of NCT was both significantly higher than that before NCT (P < 0.05)
Effect of RECIST classification and CTC response to NCT on DMFS in the general population
The median follow-up for distant metastasis was 27 months (range 7–36 months). The results of log-rank test showed that there was no significant difference in DMFS between PR/CR group and PD/SD group (log-rank P = 0.0914; PR/CR vs. PD/SD HR: 0.39, 95% CI 0.13–1.22) (Fig. 2a). However, CTC low-R group had a worse DMFS than CTC high-R group (log-rank P = 0.0199; CTC high-R vs. CTC low-R HR: 0.24, 95% CI 0.07–0.90) (Fig. 2b). Therefore, CTC response to NCT, rather than whether achieving imaging remission, was related to the prognosis of LABC patients in the general population. In addition, based on the median number of CTCs after completion of NCT, we divided all cases into "< 17" group and "≥ 17" group. There was no significant difference in DMFS between the two groups (log-rank P = 0.1681; ≥ 17 group vs. < 17 group HR: 2.26, 95% CI 0.68–7.52; figure not shown).
Survival analysis according to different grouping criteria. a There was no significant difference in DMFS between PR/CR group and PD/SD group (P = 0.0914). b CTC low-R group showed a worse DMFS than CTC high-R group (P = 0.0199). c In PR/CR subgroup, patients with CTC low-R showed a significantly lower DMFS compared with those with CTC high-R (P = 0.0159). d In PD/SD subgroup, no significant difference was found in DMFS between CTC low-R and CTC high-R group (P = 0.7521). e, f There was no significant difference in DMFS between CTC high-R and CTC low-R group in both luminal or non-luminal subgroups (luminal subgroup: P = 0.1320; non-luminal subgroup: P = 0.0782)
The CTC response to NCT was still valuable in predicting the prognosis even when PR/CR was already achieved after NCT
In PR/CR subgroup, patients with CTC low-R showed a lower DMFS compared with those with CTC high-R (log-rank P = 0.0159; CTC high-R vs. CTC low-R HR: 0.11, 95% CI 0.01–0.96) (Fig. 2c). Nevertheless, in PD/SD subgroup, no significant difference was found in DMFS between CTC low-R and CTC high-R group (log-rank P = 0.7521; CTC high-R vs. CTC low-R HR: 0.73, 95% CI 0.12–4.39) (Fig. 2c). Therefore, even when PR/CR was already achieved through imaging evaluation after NCT, the CTC response to NCT is still valuable in predicting the prognosis in this population. In Fig. 3, we took a case for example. Although this case achieved PR after NCT, she developed distant metastasis at 12 months of follow-up and died at 15 months. Retrospectively analyzing the CTC levels of this case, the number of CTCs increased successively at these three time points. In this case, additionally, the routine pathological report after surgery suggested an M–P grade of 2.
Magnetic resonance (MR) imaging and trend of the number of CTCs in one case. In this case whose was aged 40 when diagnosed with LABC, PR was achieved after NCT according to MR (a). However, the number of CTCs increased successively at these three time points (b). The M–P grade of this case is 2 and she developed distant metastasis at 12 months of follow-up and died at 15 months
Subgroup analysis of DMFS according to ER and PgR expression
According to the expression of ER and PgR, the enrolled patients were divided into luminal subgroup and non-luminal subgroup. Results showed that there was no significant difference in DMFS between CTC high-R and CTC low-R group in both subgroups (luminal subgroup: log-rank P = 0.1320, CTC high-R vs. CTC low-R HR: 0.32, 95% CI 0.06–1.59; non-luminal subgroup: log-rank P = 0.0782, CTC high-R vs. CTC low-R HR: 0.16, 95% CI 0.02–1.61) (Fig. 2e, f).
Univariate and multivariate analyses of DMFS
In univariate analysis, none of the included factors was significantly associated with DMFS. However, in multivariate analysis, DMFS were significantly improved in CTC high-R group compared with CTC low-R group (HR: 0.16, 95% CI 0.03–0.87; P = 0.03) (Table 2).
Efficiency of combination of response of CTC number to NCT and RECIST classification in predicting the treatment response to NCT
We set the M–P classification as the reference standard for assessing response to NCT. ROC curve analyses showed that CTC response to NCT or RECIST classification alone had an AUC of 0.533 (95% CI 0.277–0.790) and 0.700 (95% CI 0.611–0.789), respectively (Fig. 4). When combining the two indexes above, that is, grouping patients according to RECIST classification combined with CTC response to NCT as mentioned above, the AUC slightly increased to 0.713 (95% CI 0.532–0.895), suggesting that this method may potentially further improve the accuracy of prediction of NCT response (Fig. 4).
The ROC curves and AUC of response of CTC number, RECIST classification and the combination in predicting the treatment response to NCT. The CTC response to NCT or RECIST classification alone had an AUC of 0.533 (95% CI 0.277–0.790) and 0.700 (95% CI 0.611–0.789), respectively. When combining the two indexes, the AUC slightly increased to 0.713 (95% CI 0.532–0.895)
Discussion
With the update of medical technology, the application of liquid biopsy for breast cancer has been developed, which makes up for the deficiency of traditional tissue biopsy. Subjects of fluid biopsy include multiple components of the tumor, such as CTCs, cell-free DNA (cfDNA) and exosomes [25, 26]. Liquid biopsy can be used to detect minimal residual disease (MRD) which cannot be demonstrated by clinical examination and imaging features [27]. CTCs, one of the components analyzed in liquid biopsy, are detached from the primary tumor into the circulation [28]. In addition, CTCs have been thought to be an intermediate process of distant metastasis [29]. At present, there are still many controversies about the role of CTCs in predicting the response of LABC patients to NCT and the prognosis of the disease.
The NSABP Protocol B-27 clinical trial divided the enrolled patients who received AC (doxorubicin + cyclophosphamide, 4 cycles) regimen NCT into three groups based on whether T (docetaxel, 4 cycles) was added to AC and the timing of T and surgery. Although there were significant differences in pCR rates between AC and AC-T as NCT regimen, no significant difference in OS, disease-free survival (DFS) and RFS was found between them [30]. Furthermore, a trial-based meta-regression analysis showed that pCR affected by NCT could only explain less than 9% of the influence on long-term prognosis among breast cancer patients and pCR might not be an appropriate surrogate end-point in the assessment of prognosis [31]. Therefore, even whether pCR was achieved after NCT could not completely predict the prognosis of breast cancer. In other words, a subset of patients who achieved pCR after NCT did not have a satisfactory prognosis. On the other side, in terms of clinical response rate, although some studies [32,33,34] have suggested that it was associated with prognosis, this evaluation method may sometimes be incomplete for LABC patients receiving NCT. In addition, a retrospective study showed that discontinuation of trastuzumab predicted a worse prognosis than continuous use in metastatic breast cancer, regardless of response to treatment according to RECIST [35]. Besides, the results from Neo-ALTTO trial in HER-2-positive breast cancer patients who received neoadjuvant targeted therapy showed that there was no significant correlation between the event-free survival (EFS) of responders and non-responders defined by RECIST, using mammography and/or ultrasound [36]. These findings suggested that both pathological remission and image reduction are limited predictors of prognosis, because they are only assessment of local tumor. Instead, the CTC status can reflect the minimal residual disease in the whole body of breast cancer patients and its prognostic value has been established [37].
A phase II randomized trial concluded that CTC-positive (at least one CTC detected per 7.5 mL of blood) pre- and/or post- NCT was related to a higher early metastatic relapse rate in patients with large operable breast cancer or LABC whether using univariate analysis or multivariate Cox regression model [18]. Another prospective study which enrolled 115 nonmetastatic patients showed that the number of CTCs detected ≥ 1 before, after or before/after NCT all indicated lower OS and DFS. However, CTC number after NCT was not significantly associated with OS or DFS in multivariate analysis [19]. A study in HER-2-positive metastatic breast cancer patients found that patients with at least one CTCs detected in 10 ml blood had a worse PFS than those with no CTC detected (P = 0.0125) [38]. Another study enrolled 286 patients with TNBC and CTC numbers were obtained before, 3 days and 7 days after surgery. The results showed that patients with CTC number > 5 per 7.5 ml blood whether detected before, 3 days or 7 days after surgery had a shorter 3-year OS and PFS than those with ≤ 5 [39]. In addition, a recent prospective study showed that ≥ 5 CTCs detected after NCT portended a worse RFS than < 5 CTCs after NCT in TNBC patients who did not achieve pCR after NCT [20]. This result also demonstrated that the number of CTCs after NCT still had an important influence on the prognosis among TNBC patients who did not achieve pCR after NCT. However, it should be noted that the indexes used in these studies were the absolute numbers of CTCs, rather than the relative proportion of change. To confirm the inferiority of the latter’s effect on prognosis, we divided the enrolled cases into “ < 17” group and “ ≥ 17” group based on the median number of CTCs after the end of NCT. The results showed that there was no significant difference in DMFS between the two groups. This phenomenon might be attributed to the differences of multiple factors in patients, such as local/regional tumor burden before NCT, baseline levels of CTCs and resistance to chemotherapy drugs. Moreover, only 4 of the 35 patients (11.4%) achieved pCR of primary tumor after NCT, indicating that most patients had residual tumors, although some patients achieved radiographic remissions. These factors might attenuate the effect of absolute numbers of CTCs on prognosis. Besides, different cut-off values of CTC levels were selected as the basis for grouping in above-mentioned studies, which resulted in inter-study heterogeneity.
In our study, LABC patients were divided into “CTC high-R” and “CTC low-R” group according to the variation amplitude of CTC number at the three time points of NCT, which reflected the response of CTC number to NCT. The results of survival analysis showed that CTC low-R group had a worse DMFS than CTC high-R group (P = 0.0199) and this was consistent with previous studies in which only the absolute number of CTCs was analyzed. However, there was no significant difference in DMFS between PR/CR group and PD/SD group (P = 0.0914), which indicated that the tumor shrinkage in clinical imaging could not accurately predict the prognosis. In addition, we conducted a stratified analysis according to RECIST classification. No significant difference was found in DMFS between CTC low-R and CTC high-R group in patients who achieved PD/SD after NCT (P = 0.7521), while patients with CTC low-R showed a lower DMFS compared with those with CTC high-R in PR/CR subgroup (P = 0.0159). In multivariate analysis, only change of CTC number was significantly associated with DMFS (P = 0.03). These results indicated that the response of CTC count to NCT was still valuable in prognostic judgment in patients who have achieved remission based on images. However, it is still impractical to use CTC alone to assess prognosis in current clinical practice. Therefore, we believe that the combination of CTC change and RECIST can better help clinicians to evaluate prognosis and guide systemic and individualized treatment, so as to improve prognosis.
Whether the CTC status was related to the treatment response of NCT remains controversial. A meta-analysis published in 2014 in which 4 studies were included concluded that the change (decrease or increase) of CTC number before and after NCT was not significantly associated with pCR in LABC patients (P = 0.877) [18, 21, 40,41,42]. However, a recent study showed that patients of whom CTC status was positive before NCT and turned negative after NCT had a significant higher ORR (P = 0.013) but an insignificant higher pCR rate (P = 0.0608) [22]. In our study, when setting the M–P classification as the reference standard, the response of CTC number during NCT had a comparatively low AUC (0.533) for assessing response to NCT, which was consistent with previous research results to a certain extent. A retrospective cohort analysis established a modified RECIST criteria which combined conventional RECIST criteria and pathologic verification. The results showed that the modified RECIST classification had no significant correlation with local recurrence rate [33]. Our results suggested that the combination of RECIST classification and CTC response to NCT showed a slightly improved AUC compared with RECIST classification alone (0.713 vs. 0.700). Despite the lack of significant difference, the result suggested that the RECIST classification combined with response of CTC to NCT might provide a more accurate assessment of the efficacy of NCT compared to RECIST classification alone, but a larger clinical sample size is needed to further confirm this conclusion.
This study has some drawbacks. First, due to the limited sample size, the relationship between the changing trend of CTC number and imaging remission could not be clearly defined. With the further increase of the sample size, more reliable conclusions will be drawn. Second, together with the small number of death events during the follow-up period, the correlation between the response of CTC number to NCT and OS could not be obtained. Third, in this study, the relationship between CTCs of different molecular subtypes and the response and prognosis of LABC patients receiving NCT was not analyzed, which should be further explored in future studies.
In conclusion, the change of CTC number during NCT has a potential to become a supplement to RECIST in the assessment of NCT efficacy and the prognosis of LABC patients. With the further development of related research and the increase of sample size, this synthetic assessment method has the potential to be widely used in clinical practice.
References
Tryfonidis K, Senkus E, Cardoso MJ et al (2015) Management of locally advanced breast cancer-perspectives and future directions. Nat Rev Clin Oncol 12:147–162
Kammerer E, Guevelou JL, Chaikh A et al (2018) Proton therapy for locally advanced breast cancer: a systematic review of the literature. Cancer Treat Rev 63:19–27
Brackstone M, Palma D, Tuck AB et al (2017) Concurrent neoadjuvant chemotherapy and radiation therapy in locally advanced breast cancer. Int J Radiat Oncol Biol Phys 99:769–776
Zagar TM, Oleson JR, Vujaskovic Z et al (2010) Hyperthermia for locally advanced breast cancer. Int J Hyperthermia 26:618–624
Specht J, Gralow JR (2009) Neoadjuvant chemotherapy for locally advanced breast cancer. Semin Radiat Oncol 19:222–228
Mathew J, Asgeirsson KS, Cheung KL et al (2009) Neoadjuvant chemotherapy for locally advanced breast cancer: a review of the literature and future directions. Eur J Surg Oncol 35:113–122
Gianni L, Pienkowski T, Im YH et al (2016) 5-year analysis of neoadjuvant pertuzumab and trastuzumab in patients with locally advanced, inflammatory, or early-stage HER2-positive breast cancer (NeoSphere): a multicentre, open-label, phase 2 randomised trial. Lancet Oncol 17:791–800
Schwartz LH, Litiere S, De Vries E et al (2016) RECIST 1.1-update and clarification: from the RECIST committee. Eur J Cancer 62:132–137
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Therasse P, Arbuck SG, Eisenhauer EA et al (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Guenther LM, Rowe RG, Acharya PT et al (2018) Response Evaluation Criteria in Solid Tumors (RECIST) following neoadjuvant chemotherapy in osteosarcoma. Pediatr Blood Cancer 65:e26896
Patel UB, Brown G, Machado I et al (2017) MRI assessment and outcomes in patients receiving neoadjuvant chemotherapy only for primary rectal cancer: long-term results from the GEMCAD 0801 trial. Ann Oncol 28:344–353
Litiere S, Collette S, De Vries EG et al (2017) RECIST—learning from the past to build the future. Nat Rev Clin Oncol 14:187–192
Chen S, Liu Y, Ouyang QW et al (2015) Clinical and pathological response to neoadjuvant chemotherapy based on primary tumor reduction is correlated to survival in hormone receptor-positive but not hormone receptor-negative locally advanced breast cancer. Ann Surg Oncol 22:32–39
Romero A, Garcia-Saenz JA, Fuentes-Ferrer M et al (2013) Correlation between response to neoadjuvant chemotherapy and survival in locally advanced breast cancer patients. Ann Oncol 24:655–661
Yeh E, Slanetz P, Kopans DB et al (2005) Prospective comparison of mammography, sonography, and MRI in patients undergoing neoadjuvant chemotherapy for palpable breast cancer. AJR Am J Roentgenol 184:868–877
Bidard FC, Proudhon C, Pierga JY (2016) Circulating tumor cells in breast cancer. Mol Oncol 10:418–430
Pierga JY, Bidard FC, Mathiot C et al (2008) Circulating tumor cell detection predicts early metastatic relapse after neoadjuvant chemotherapy in large operable and locally advanced breast cancer in a phase II randomized trial. Clin Cancer Res 14:7004–7010
Bidard FC, Mathiot C, Delaloge S et al (2010) Single circulating tumor cell detection and overall survival in nonmetastatic breast cancer. Ann Oncol 21:729–733
Gwark S, Kim J, Kwon NJ et al (2020) Analysis of the serial circulating tumor cell count during neoadjuvant chemotherapy in breast cancer patients. Sci Rep 10:17466
Fei F, Du Y, Di G et al (2014) Are changes in circulating tumor cell (CTC) count associated with the response to neoadjuvant chemotherapy in local advanced breast cancer? A meta-analysis. Oncol Res Treat 37:250–254
Ni C, Shen Y, Fang Q et al (2020) Prospective study of the relevance of circulating tumor cell status and neoadjuvant chemotherapy effectiveness in early breast cancer. Cancer Med 9:2290–2298
Lin PP (2015) Integrated EpCAM-independent subtraction enrichment and iFISH strategies to detect and classify disseminated and circulating tumors cells. Clin Transl Med 4:38
Ma G, Jiang Y, Liang M et al (2020) Dynamic monitoring of CD45-/CD31+/DAPI+ circulating endothelial cells aneuploid for chromosome 8 during neoadjuvant chemotherapy in locally advanced breast cancer. Ther Adv Med Oncol 12:1758835920918470
Ma G, Wang J, Huang H et al (2020) Identification of the plasma total cfDNA level before and after chemotherapy as an indicator of the neoadjuvant chemotherapy response in locally advanced breast cancer. Cancer Med 9:2271–2282
Alimirzaie S, Bagherzadeh M, Akbari MR (2019) Liquid biopsy in breast cancer: a comprehensive review. Clin Genet 95:643–660
Pantel K, Alix-Panabieres C (2019) Liquid biopsy and minimal residual disease—latest advances and implications for cure. Nat Rev Clin Oncol 16:409–424
Aceto N, Bardia A, Miyamoto DT et al (2014) Circulating tumor cell clusters are oligoclonal precursors of breast cancer metastasis. Cell 158:1110–1122
Micalizzi DS, Maheswaran S, Haber DA (2017) A conduit to metastasis: circulating tumor cell biology. Genes Dev 31:1827–1840
Bear HD, Anderson S, Smith RE et al (2006) Sequential preoperative or postoperative docetaxel added to preoperative doxorubicin plus cyclophosphamide for operable breast cancer: National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol 24:2019–2027
Berruti A, Amoroso V, Gallo F et al (2014) Pathologic complete response as a potential surrogate for the clinical outcome in patients with breast cancer after neoadjuvant therapy: a meta-regression of 29 randomized prospective studies. J Clin Oncol 32:3883–3891
Ma F, Ouyang Q, Li W et al (2019) Pyrotinib or lapatinib combined with capecitabine in HER2-positive metastatic breast cancer with prior taxanes, anthracyclines, and/or trastuzumab: a randomized, phase II study. J Clin Oncol 37:2610–2619
Klein J, Tran W, Watkins E et al (2019) Locally advanced breast cancer treated with neoadjuvant chemotherapy and adjuvant radiotherapy: a retrospective cohort analysis. BMC Cancer 19:306
Carrara GF, Scapulatempo-Neto C, Abrahao-Machado LF et al (2017) Breast-conserving surgery in locally advanced breast cancer submitted to neoadjuvant chemotherapy. Safety and effectiveness based on ipsilateral breast tumor recurrence and long-term follow-up. Clinics (Sao Paulo) 72:134–142
Campiglio M, Bufalino R, Sandri M et al (2011) Increased overall survival independent of RECIST response in metastatic breast cancer patients continuing trastuzumab treatment: evidence from a retrospective study. Breast Cancer Res Treat 128:147–154
Di Cosimo S, Campbell C, Azim HA Jr et al (2018) The use of breast imaging for predicting response to neoadjuvant lapatinib, trastuzumab and their combination in HER2-positive breast cancer: results from Neo-ALTTO. Eur J Cancer 89:42–48
Banys-Paluchowski M, Krawczyk N, Meier-Stiegen F et al (2016) Circulating tumor cells in breast cancer–current status and perspectives. Crit Rev Oncol Hematol 97:22–29
Liu Y, Liu Q, Wang T et al (2013) Circulating tumor cells in HER2-positive metastatic breast cancer patients: a valuable prognostic and predictive biomarker. BMC Cancer 13:202
Zhang Y, Lv Y, Niu Y et al (2017) Role of circulating tumor cell (CTC) monitoring in evaluating prognosis of triple-negative breast cancer patients in China. Med Sci Monit 23:3071–3079
Riethdorf S, Muller V, Zhang L et al (2010) Detection and HER2 expression of circulating tumor cells: prospective monitoring in breast cancer patients treated in the neoadjuvant GeparQuattro trial. Clin Cancer Res 16:2634–2645
Garcia-Saenz JA, Martin M, Maestro ML et al (2009) Circulating tumour cells in locally advanced breast cancer. Clin Transl Oncol 11:544–547
Camara O, Rengsberger M, Egbe A et al (2007) The relevance of circulating epithelial tumor cells (CETC) for therapy monitoring during neoadjuvant (primary systemic) chemotherapy in breast cancer. Ann Oncol 18:1484–1492
Acknowledgements
We thank all co-workers for their cooperation in this study. More importantly, we also thank all patients enrolled in our study for their agreeing to participate.
Funding
This study was funded by the Natural Science Foundation of China (81572607, 81572602 and 8210112767).
Author information
Authors and Affiliations
Contributions
SW and TX contributed to the study conception and design. XW, RC and ML were involved in data acquisition. Data processing and analysis were performed by GM and JW. The first draft of the manuscript was written by JW and XW. SW, TX and ML commented on previous versions of the manuscript. All authors read and approved the final manuscript. All named authors have met the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this article, take responsibility for the integrity of the whole work, and have given their approval for this version to be published.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the institutional ethics committee of the First Affiliated Hospital with Nanjing Medical University.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Wang, J., Wang, X., Chen, R. et al. Circulating tumor cells may serve as a supplement to RECIST in neoadjuvant chemotherapy of patients with locally advanced breast cancer. Int J Clin Oncol 27, 889–898 (2022). https://doi.org/10.1007/s10147-022-02125-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-022-02125-9