Abstract
Background
Nedaplatin (NDP)-related hypersensitivity reactions (HSRs) trigger adverse clinical events. Prediction and prevention of NDP-HSRs are thus essential to minimize the risk and maximize the benefit of NDP therapy. However, the incidence of NDP-HSRs and the associated risk factors remain unclear.
Methods
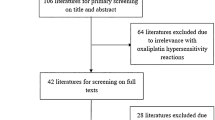
We retrospectively examined patients who received NDP monotherapy between April 2011 and July 2015 in Nagoya University Hospital. HSRs severity was defined according to the Common Terminology Criteria for Adverse Events version 4 (CTCAE ver.4). Risk factors for NDP-HSRs were determined using multivariate logistic regression.
Results
Of 111 patients who received NDP monotherapy, 90 (81%) were female; median age was 59 years (range, 29–78 years). Eighty-eight patients had gynecological cancer and 20 suffered from head and neck cancer. Eight of 111 patients (7.2%) experienced NDP-HSRs, six of which developed in the second NDP cycle. However, all patients with NDP-HSRs were treated with carboplatin (CBDCA) for more than three cycles. Grade 3 and 4 HSRs developed in 2 patients. NDP-HSRs were significantly associated with a history of CBDCA-HSRs (odds ratio 37.5, 95% confidence interval 5.38–262, p < 0.001) and with the interval between NDP administration and the previous platinum treatment (odds ratio 13.9, 95% confidence interval 1.23–158, p = 0.034).
Conclusion
The risk of NDP-HSRs increases in patients with a history of CBDCA-HSRs and in those administered NDP for more than 6 months after previous platinum treatment. Such individuals must be closely monitored if given NDP, even if they are expected to benefit from the treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypersensitivity reactions (HSRs), which are acute adverse events in chemotherapy, have prompted significant research efforts into the quantification of incidence and the identification of HSR risk factors. Commonly used platinum agents, such as carboplatin (CBDCA) and oxaliplatin (L-OHP), are known risk factors for HSRs [1].
CBDCA is one of the most frequently used platinum agents for the treatment of several malignancies (e.g., head and neck, lung, breast, cervical, ovarian, testicular cancer, and malignant lymphoma). The overall incidence of CBDCA-HSRs can range between 1% and 44%, with less than 1% occurring within five CBDCA cycles, 6.5% in six cycles, 27% in seven or more cycles, and 44% in third-line retreatment [1]. L-OHP, a drug commonly used to treat metastatic colorectal cancer, is generally combined with the genotoxic agent fluorouracil or its analogues. The incidence of L-OHP-related HSRs ranges from 10% to 18.9%, and the HSR usually develops following six or more cycles of treatment. Furthermore, the risk of HSRs driven by common platinum agents increases in patients who undergo repeated treatment [2,3,4,5].
NDP (cis-diammine-glycolatoplatinum) is a cisplatin (CDDP) analogue that has been approved for the treatment of various solid tumors; the drug elicits lesser gastrointestinal and renal toxicities when compared with CDDP [6, 7]. Thus, NDP may become the ‘drug of choice’ and substitute for both CDDP and CBDCA in the treatment of solid cancers. In support of this, several phase II studies have demonstrated the efficacy of NDP combination therapy in cervical cancer [8,9,10] and in head and neck cancer [11,12,13]. A recent phase III study indicated that NDP plus docetaxel was superior to CDDP plus docetaxel with regard to overall survival in advanced or relapsed squamous cell lung cancer patients [14]. Based on this evidence, NDP is currently the third most commonly used platinum agent, with only CDDP and CBDCA being used more frequently in the clinic.
NDP-HSRs can be associated with severe adverse clinical symptoms, although the risk factors that precipitate such events are still unclear. To minimize the risk and maximize the benefit of NDP therapy, it is therefore essential to identify factors associated with NDP-driven HSRs. In many cases, NDP is used to treat patients with gynecological cancer who have previously experienced CBDCA-HSRs. However, whether CBDCA treatment history has an impact on the risk of developing NDP-HSRs has not been formally tested. In this retrospective study, we investigated the incidence of NDP-HSRs, searched for associated risk factors, and evaluated the relationship between CBDCA- and NDP-triggered HSRs.
Patients and methods
Study design
This study was a single-center, retrospective cohort study. The study protocol was approved by the ethics board of Nagoya University School of Medicine.
Patients
We identified Japanese patients aged ≥20 years who had received NDP monotherapy at Nagoya University Hospital from April 2011 to July 2015. Exclusion criteria included prior treatment history with an NDP-containing regimen.
Treatment
In the monotherapy regimen approved by our institution, NDP at 80–100 mg/m2 was administrated intravenously for 60 min following pretreatment with 13.2 mg dexamethasone (DEX) and 5-HT3 antagonist every 4 weeks. Dose and type of 5-HT3 antagonist were optional. NDP and DEX dose reduction was allowed depending on each patient’s condition.
Hypersensitivity reactions
Considering their delayed onset, we defined HSRs caused by either NDP or CBDCA as allergy-like reactions (including itching, rash, flush, chest tightness, respiratory discomfort, emesis, blood pressure changes, and facial swelling) that occurred within the first 48 h of treatment. We excluded cases that could have been caused by other drugs administered concomitantly with platinum reagents. The severity of NDP and CBDCA-HSRs was graded according to the Common Terminology Criteria for Adverse Events version 4.0 (CTCAE ver.4.0).
Data collection
Clinical data collected from the medical records were as follows: age, type of cancer, history of allergy, incidence and severity of NDP- and CBDCA-HSRs, symptoms of NDP-HSRs, and NDP exposure during the study period (total number of courses, doses, and cumulative dose). We also recorded treatment line number, the number of prior CBDCA administrations, and the interval between NDP treatment and any previous platinum treatment (defined as the number of months from the last platinum treatment to the first NDP administration).
Statistical analysis
Univariate analyses were performed by Mann–Whitney U test and Fisher’s exact test. A multivariate logistic regression analysis was used to estimate adjusted odds ratios. All statistical analyses were performed with the Statistics Program for Social Science version 23 (SPSS; IBM, Armonk, NY, USA). Variables were considered significant when the p value was less than 0.05.
Results
Patient characteristics
One patient who had been previously treated with a regimen including NDP was excluded. A total of 111 patients treated with NDP were included. Because gynecological cancer patients were in the majority, 90 of 111 patients (81%) were women (Table 1). Median age was 59 years (range, 29–78 years). Eighty-eight of 111 patients (79%) were first treated with CDDP or CBDCA and given NDP as a third or higher line treatment.
Situations with developing NDP-HSRs
In the study population, eight patients experienced HSRs following NDP treatment, representing an incidence of 7.2% of all treated patients. Five of eight NDP-HSRs (63%) were observed within 10 min, and the most frequently observed symptoms were flush (six patients) and respiratory discomfort (four patients), which were typical reactions and also observed in CBDCA-HSRs (Table 2) [1, 2]. Two patients needed hospitalization (grade 3) and another two were transferred to an intensive care unit for treatment of HSRs (grade 4). Six of eight patients (75%) developed HSRs during the second NDP cycle (Fig. 1). All patients with NDP-HSRs had already been exposed to more than three cycles of CBDCA treatment (Table 3). There was no association between HSR grade and the number of platinum cycles. Five of eight patients (63%) had a history of CBDCA-HSRs.
Risk factors for NDP-HSRs
Univariate analysis revealed three parameters as potential risk factors for NDP-HSRs (Table 3). First, the number of prior CBDCA treatments was significantly higher in patients with NDP-HSRs compared to patients without NDP-HSRs (median, 9.5 vs. 5; p = 0.009). Second, the overall incidence of CBDCA-HSRs was higher in patients with NDP-HSRs relative to patients without NDP-HSRs (63% vs. 6%; p < 0.001). Finally, the proportion of patients who received NDP 6 months or more after the previous platinum treatment was higher in patients with NDP-HSRs than patients without NDP-HSRs (88% vs. 43%; p = 0.023). The effects of DEX reduction, age, and the number of NDP cycles had no statistically significant impact on NDP-HSRs.
Using multivariate analysis, NDP-HSRs were significantly associated with two factors: history of CBDCA-HSRs (odds ratio 37.5, 95% CI 5.38–262, p < 0.001), and the length of the interval between NDP and the previous platinum treatment (odds ratio 13.9, 95% CI 1.23–158, p = 0.034) (Table 4).
Association of NDP-HSRs with CBDCA-HSRs
In patients who experienced CBDCA-HSRs, 5 of 11 individuals (45%) developed NDP-HSRs. The interval between the first NDP treatment and previous CBDCA-HSRs was significantly longer in this group than in patients without NDP-HSRs (median months, 30 vs. 1; p = 0.025) (Table 5). Additionally, 72 of 111 patients in the study population had a history of CBDCA treatment (Table 1). The incidence of NDP-HSRs was significantly higher in these 72 patients compared to those without CBDCA-HSRs (45% vs. 4.9%; p > 0.001) (Table 6).
Discussion
In our study, most NDP-HSRs occurred during an early cycle of treatment, in contrast with the risk of common platinum-HSRs, which increased in patients who undergo repeated treatment. NDP is commonly used as the third platinum agent. It is predicted that prior repeated platinum exposure influences early onset of NDP-HSRs.
Additionally, we found that a history of CBDCA-HSRs was the most significant risk factor for NDP-HSRs.
Various mechanisms have been proposed to explain platinum-dependent HSRs. First, there is a correlation between severe CBDCA-HSRs and IgE-dependent-HSRs. Patients with CBDCA-HSRs had significantly higher expression of the Fc fragment of IgE receptor-I (FcεRI) on basophils, and a higher level of FcεRI mRNA in peripheral blood, compared to patients without CBDCA-HSRs. Accordingly, it was suggested that monitoring the pharmacodynamic changes of FcεRI expression on basophils was essential for prevention of CBDCA-HSRs in high-risk patients [15].
Second, specific IgE (sIgE) was observed in several patients with CBDCA- or L-OHP-induced HSRs; this finding has led to the proposal that sIgE may recognize different epitopes in CBDCA and L-OHP. CBDCA sIgE may be directed against primary amine groups that are present on both CBDCA and CDDP but absent on L-OHP [16]. Similar to CBDCA, NDP also contains a primary amine group and may therefore be recognized by autoantibodies. Together, these observations suggest that platinum-driven HSRs develop because of activation of a type I allergy mechanism, and that NDP possibly cross-reacts with CBDCA as to HSRs.
Although our multivariate analysis indicated that a history of CBDCA-HSRs was a risk factor for NDP-HSRs, substituting CBDCA with NDP in women with gynecological cancers who experienced CBDCA-HSRs is an effective treatment strategy. Indeed, two groups have reported approximately 30–35% response rates, including five cases of complete response [17, 18]. Accordingly, NDP treatment in patients who had experienced CBDCA-HSRs should generally be avoided, except when significant benefits are expected.
A long interval between NDP treatment and any previous platinum regimen was also detected as a risk factor for NDP-HSRs. This finding is consistent with a previous report that a 12-month platinum-free interval is a risk factor for CBDCA-HSRs in gynecological cancer patients [3, 19]. Similarly, L-OHP salvage therapy is a risk factor for HSRs in colon cancer patients [20]. In addition, two previous studies have reported the incidence of NDP-HSRs and interval to re-challenge after CBDCA-HSRs. Michikami et al., Arimoto et al., and we ourselves have reported that incidence of NDP-HSRs after CBDCA-HSRs was 7.9% in patients who subsequently switched to NDP, 27% in patients with a 1.4-month interval to re-challenge, and 45% in patients with a 9-month interval (Table 5) [17, 18]. The incidence of NDP-HSRs after CBDCA-HSRs was increased associated with a long interval to re-challenge. These reports suggest that the development of immune sensitization to platinum agents, including NDP, requires a relatively long period before it manifests in the form of clinical symptoms. Our current results suggest that a long time interval may be required to develop cross-immune sensitization to NDP in patients with CBDCA-HSRs. Thus we infer that, when deemed necessary, NDP treatment should be initiated relatively soon after CBDCA treatment in those patients who experienced CBDCA-HSRs. Conversely, if a long period (>6 months) has elapsed since the last episode of CBDCA-HSRs, NDP should only be administered with especially careful monitoring. However, further studies are required to validate this approach, because many mechanistic aspects of platinum immune sensitization remain unclear.
Management for platinum-HSRs including premedication, desensitization, and substitution of platinum agents has been investigated [1, 21,22,23,24]. However, preventive effects are still limited, and specific prophylaxis for NDP-HSRs has rarely been reported. Subsequent substitution of NDP for CBDCA may be an effective management for CBDCA-HSRs, but further study is also needed to demonstrate this hypothesis.
Several limitations of this study should be noted. As it was retrospective, this study was not able to address the outcome of novel changes to treatment strategies when HSRs were encountered. Also, the number of study subjects was relatively small and the data presented should therefore be interpreted with caution. Additionally, we only focused on prediction of NDP-HSR development, so we did not evaluate the efficacy of therapy and HSR prophylaxis.
In conclusion, a history of CBDCA-HSRs and an interval of 6 months or greater between NDP and the previous platinum treatment are risk factors for NDP-HSRs. Thus, NDP mo notherapy in patients who have experienced CBDCA-HSRs should be implemented with great care. When a benefit of the NDP monotherapy is expected for patients in whom the interval between different platinum treatments is long, its administration should be carefully monitored.
References
Makrilia N, Syrigou E, Kaklamanos I et al (2010) Hypersensitivity reactions associated with platinum antineoplastic agents: a systematic review. Met Based Drugs. doi:10.1155/2010/207084
Markman M (2002) Hypersensitivity reactions to carboplatin. Gynecol Oncol 84:353–354
Navo M, Kunthur A, Badell ML et al (2006) Evaluation of the incidence of carboplatin hypersensitivity reactions in cancer patients. Gynecol Oncol 103:608–613
Schwartz JR, Bandera C, Bradley A et al (2007) Does the platinum-free interval predict the incidence or severity of hypersensitivity reactions to carboplatin? The experience from Women and Infants’ Hospital. Gynecol Oncol 105:81–83
Okayama T, Ishikawa T, Sugatani K et al (2015) Hypersensitivity reactions to oxaliplatin: identifying the risk factors and judging the efficacy of a desensitization protocol. Clin Ther 37:1259–1269
Liu Y, Yu S, Liu S et al (2015) Comparison of nedaplatin-based versus cisplatin-based chemotherapy for advanced non-small cell lung cancer among East Asian populations: a meta-analysis. Sci Rep 5:10516
Shan J, Xiong Y, Wang D et al (2015) Nedaplatin- versus cisplatin-based chemotherapy in the survival time of patients with non-small cell lung cancer. Mol Clin Oncol 3:543–549
Yokoyama Y, Takano T, Nakahara K et al (2008) A phase II multicenter trial of concurrent chemoradiotherapy with weekly nedaplatin in advanced uterine cervical carcinoma. Tohoku Gynecologic Cancer Unit Study. Oncol Rep 19:1551–1556
Yamaguchi S, Nishimura R, Yaegashi N et al (2012) Phase II study of neoadjuvant chemotherapy with irinotecan hydrochloride and nedaplatin followed by radical hysterectomy for bulky stage Ib2 to IIb, cervical squamous cell carcinoma. Japanese Gynecologic Oncology Group study (JGOG1065). Oncol Rep 28:487–493
Takekuma M, Hirashima Y, Ito K et al (2012) Phase II trial of paclitaxel and nedaplatin in patients with advanced/recurrent uterine cervical cancer: a Kansai Clinical Oncology Group study. Gynecol Oncol 126:341–345
Kurita H, Yamamoto E, Nozaki S et al (2010) Multicenter phase 2 study of induction chemotherapy with docetaxel and nedaplatin for oral squamous cell carcinoma. Cancer Chemother Pharmacol 65:503–508
Ohashi T, Ohnishi M, Tanahashi S et al (2011) Efficacy and toxicity of concurrent chemoradiotherapy with nedaplatin and S-1 for head and neck cancer. Jpn J Clin Oncol 41:348–352
Hoshikawa H, Kishino T, Mori T et al (2015) Clinical outcomes of nedaplatin and S-1 treatment with concurrent radiotherapy in advanced head and neck cancer. Acta Otolaryngol 135:103–108
Shukuya T, Yamanaka T, Seto T et al (2015) Nedaplatin plus docetaxel versus cisplatin plus docetaxel for advanced or relapsed squamous cell carcinoma of the lung (WJOG5208L): a randomised, open-label, phase 3 trial. Lancet Oncol 16:1630–1638
Iwamoto T, Hirai H, Yamaguchi N et al (2014) Carboplatin-induced severe hypersensitivity reaction: role of IgE-dependent basophil activation and FcεRI. Cancer Sci 105:1472–1479
Caiado J, Venemalm L, Pereira-Santos MC et al (2013) Carboplatin-, oxaliplatin-, and cisplatin-specific IgE: cross-reactivity and value in the diagnosis of carboplatin and oxaliplatin allergy. J Allergy Clin Immunol Pract 1:494–500
Arimoto T, Oda K, Nakagawa S et al (2013) Retreatment with nedaplatin in patients with recurrent gynecological cancer after the development of hypersensitivity reaction to carboplatin. J Obstet Gynaecol Res 39:336–340
Michikami H, Minaguchi T, Ochi H et al (2013) Safety and efficacy of substituting nedaplatin after carboplatin hypersensitivity reactions in gynecologic malignancies. J Obstet Gynaecol Res 39:330–335
Sugimoto H, Iwamoto T, Murashima Y et al (2011) Risk factors contributing to the development of carboplatin-related delayed hypersensitivity reactions in Japanese patients with gynecologic cancers. Cancer Chemother Pharmacol 67:415–419
Kim BH, Bradley T, Tai J et al (2009) Hypersensitivity to oxaliplatin: an investigation of incidence and risk factors, and literature review. Oncology 76:231–238
Dizon DS, Sabbatini PJ, Aghajanian C et al (2002) Analysis of patients with epithelial ovarian cancer or fallopian tube carcinoma retreated with cisplatin after the development of a carboplatin allergy. Gynecol Oncol 84:378–382
Ottaiano A, Tambaro R, Greggi S et al (2003) Safety of cisplatin after severe hypersensitivity reactions to carboplatin in patients with recurrent ovarian carcinoma. Anticancer Res 23:3465–3468
O’Cearbhaill R, Zhou Q, Iasonos A et al (2010) The prophylactic conversion to an extended infusion schedule and use of premedication to prevent hypersensitivity reactions in ovarian cancer patients during carboplatin retreatment. Gynecol Oncol 116:326–331
Miyamoto S, Okada R, Ando K (2015) Platinum hypersensitivity and desensitization. Jpn J Clin Oncol 45:795–804
Acknowledgments
We thank Prof. Yuichi Ando (Department of Clinical Oncology and Chemotherapy, Nagoya University Hospital, Nagoya, Japan) for critical review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Kawarada, Y., Miyazaki, M., Itoh, A. et al. Incidence of and risk factors associated with nedaplatin-related hypersensitivity reactions. Int J Clin Oncol 22, 593–599 (2017). https://doi.org/10.1007/s10147-017-1091-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-017-1091-4