Abstract
There are many satisfactory long-term outcomes after posterolateral fusion (PLF) for degenerative lumbar spondylolisthesis (DLS); nonunion cases have also achieved good clinical outcomes. Facet fusion (FF), a minimally invasive evolution of PLF, also resulted in good clinical outcomes. We aimed to assess the course of nonunion cases after FF and determine whether the nonunion cases achieved good clinical outcomes. We retrospectively reviewed the records of 136 patients who underwent FF for DLS. Range of motion (ROM) at the fused level was measured using a flexion-extension lateral radiograph preoperatively and 1 year postoperatively. Patients were classified into the Fusion or Unconfirmed Fusion group by computed tomography (CT) 1 year postoperatively. Furthermore, patients in the Unconfirmed Fusion group were classified into the Delayed Union or Nonunion group depending on the confirmation status of FF upon the following CT. The average preoperative ROM and clinical outcomes were compared between the three groups. The Fusion, Delayed Union, and Nonunion groups had 109, 14, and 13 patients, respectively. In the Nonunion group, the average ROM significantly decreased from 13.0° preoperatively to 4.9° postoperatively. There was a significant difference in the average preoperative ROM between the groups. The larger the preoperative ROM, the fewer facets fused. There was no significant difference in clinical outcomes between the groups. Five patients (3.7%) required revision surgery for adjacent segment disease 1–5.5 years after FF. Even nonunion cases after FF achieved good clinical outcomes, likely because the unstable spondylolisthesis was stabilized. FF did not require revision surgery for nonunion itself.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Interbody fusion is generally performed for degenerative lumbar spondylolisthesis (DLS) [18, 28]. However, there are many satisfactory long-term outcomes after posterolateral fusion (PLF) [2, 14, 16, 32]. Some authors have reported no significant differences in clinical outcomes and fusion rates between PLF and interbody fusion, thereby questioning the need for anterior support in short lumbar fusions [6, 13, 15, 20]. Furthermore, even nonunion cases after PLF achieved good clinical outcomes [8, 25, 31]. Miyashita et al. found that facet fusion (FF) using a percutaneous pedicle screw (PS) system, as a minimally invasive evolution of PLF, also resulted in good clinical outcomes [22]. In this study, we assessed the clinical outcomes and course of nonunion cases after FF and determined whether the nonunion cases achieved good clinical outcomes as well as those after PLF.
Methods
Patient population
This was a retrospective study using prospectively collected data. We reviewed 136 out of 143 consecutive patients (77 women, 59 men; average age, 68.3 years; age range, 41–91 years) who underwent FF for single-level DLS between June 2009 and September 2015, after at least 1 year of follow-up. Seven patients were excluded; two were lost to follow-up, and five were not assessed using computed tomography (CT) up to 1 year postoperatively until adequate fusion was confirmed. The average postoperative follow-up period was 72.8 months (16–120 months). The slipped vertebra occurred at L4 in 126 patients and L3 in 10 patients. All included patients presented with intractable radiculopathy (either bilateral or unilateral) and intermittent claudication caused by spinal stenosis after several months of conservative treatment. Patients were excluded if they had low back pain (LBP) alone, foraminal stenosis, and spondylolytic spondylolisthesis. There were two indications for lumbar fusion: (1) sagittal translation of ≥ 8% on a flexion-extension lateral radiograph or (2) anterior wedging of ≥ 5° on a flexion radiograph and a disc range of motion (ROM) of ≥ 10°. The indication for fusion was not done according to lateral disc space height. When lumbar fusion was indicated, we did not use other approaches, such as interbody fusion or slippage reduction, and all DLS patients were treated with FF regardless of the spondylolisthesis grade (translation degree of all patients was grade I or II).
Operative technique
The FF procedure was performed according to Miyashita’s method [22]. Thus, the central canal and lateral recess were decompressed using laminar fenestration and bilateral undercutting of the medial part of the facet joints. Bone chips harvested from the spinous process and laminae were pushed into the thoroughly decorticated facet joint spaces (Fig. 1a). Percutaneous PSs were then inserted through the fascia.
Postoperative protocol
Patients were allowed to sit on bed with a soft brace on the first postoperative day and were mobilized with physiotherapy after the removal of the drain and urine catheter on the second postoperative day. The soft brace was worn for 3 months postoperatively. If a patient had osteoporosis, a hard brace was used for the first 3 months, and a soft brace was used for another 3 months.
Radiological assessment
ROM at the fused level was measured on a flexion-extension lateral radiograph preoperatively and 1 year postoperatively. Jiang et al. reported a mean difference of 1.9° in the Cobb angle between readings on midsagittal CT images of thoracolumbar burst fractures, with intra- and inter-observer reliability using intraclass correlation coefficients (ICCs) of 0.969–0.986 and 0.941–0.953, respectively [12]. Accordingly, ROM of less than 2° was defined as no motion taking measurement error into consideration. CT scans were performed repeatedly until adequate fusion was confirmed at 3, 6, and 12 months postoperatively and once a few years thereafter. Fusion was assessed according to Miyashita’s grading system for FF [22]. Complete (Grade I) or partial (Grade II) bony continuity on the facet joint was considered adequate fusion (Fig. 1b), and nonunion was determined when bony continuity could not be confirmed at any portion of the facet joint (grade III) (Fig. 1c) or when there was obvious FF nonunion (grade IV). Three experienced spine surgeons assessed three to five axial CT planes through the center of the facet. Bony continuity on at least one of the planes was judged as fusion. The planes were blindly evaluated on two separate occasions. When judgment differed between observers, discussions were conducted to reach a consensus. Based on the findings of 1-year postoperative CT scans, patients were classified into Fusion or Unconfirmed Fusion group. Furthermore, Unconfirmed Fusion group patients were classified into Delayed Union or Nonunion group depending on whether FF was confirmed on the following CT examination (Fig. 2). For the Nonunion group, the joint space proportion in the bilateral facets was output using image software (Ziostation2, Ziosoft, Inc., Minato-ku, Tokyo, Japan) on the axial CT plane through the center of the facet pre- and postoperatively. We evaluated lateral areas to a line through the anterior edge of the inferior articular process and vertical to a line through the anterior edges of the bilateral facets (Fig. 3).
Clinical outcome measures
The therapeutic effectiveness of FF was assessed as a clinical outcome using the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) [9], the Roland-Morris Disability Questionnaire (RMDQ), the visual analogue scale (VAS) of LBP (LBP-VAS), and VAS of buttock and lower limb pain (BLP-VAS), with all tests being done both preoperatively and 1 year postoperatively. According to previous reports, a minimal clinically important difference was defined as a 20-point increase in each category score of the JOABPEQ [9], a 5-point decrease in the RMDQ [24], a 21-point decrease in the LBP-VAS, and a 28-point decrease in the BLP-VAS [27]. Clinical outcomes were compared between the Fusion, Delayed Union, and Nonunion groups. In addition, surgical complications and revision surgeries were reviewed.
Statistical analysis
ICC was calculated to determine both intra- and inter-observer reliability for judgments of fusion using R (The R Foundation for Statistical Computing, Vienna, Austria). The Kruskal-Wallis test was used to determine significant differences in the average preoperative ROM between the three groups. The nonparametric Mann-Whitney U test was used to detect differences in ROM between each pair within the three groups and between the Fusion plus Delayed Union groups and the Nonunion group. The Wilcoxon signed-rank test was used to test differences between pre- and postoperative ROM and joint space proportion in the facets in the Nonunion group and between the pre- and postoperative RMDQ and VAS values in each of the three groups. Fisher’s exact probability test was employed to assess differences in therapeutic effectiveness between the three groups, between the Fusion and Nonunion groups, and between the Fusion plus Delayed Union and Nonunion groups. The level of significance was set at P < 0.05.
Institutional ethics committee approval
This study was approved by the Medical Ethics Committee of our hospital.
Results
Radiological results
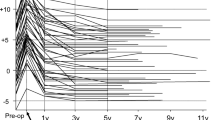
The reproducibility of the fusion judgments for each observer was quite high, and the ICC for intra-observer reliability was 0.833 for observer 1, 0.883 for observer 2, and 0.904 for observer 3. The ICC for inter-observer reliability was 0.763, which was above the statistically acceptable threshold of > 0.7. The fusion rate at the 1-year follow-up was 80.1% (109/136 cases) for unilateral facets and 76.5% (104/136 cases) for bilateral facets. The fusion rate at the final follow-up was 90.4% (123/136 cases) for unilateral facets and 86.8% (118/136 cases) for bilateral facets. That is, of the 136 patients, the Fusion group consisted of 109 cases; Delayed Union group, 14; and Nonunion group, 13 (Fig. 2) (Table 1). There was no patient for whom a judgment regarding fusion was changed during the follow-up period. We excluded seven patients from the ROM analysis because their bending radiographs were not taken from the precise lateral direction parallel to the disc space of the fusion segment. All Fusion group patients had ROM less than 2°, and no motion was recognized with the naked eye at the fused level on bending radiographs. In 14 delayed union patients, two had motion of 3.1° and 3.3° respectively at the fused level with slight PS loosening, and the others had no motion 1 year postoperatively. The average fusion period was 25.8 months (18–57 months) in nine of the 14 patients followed up with regular CT scans. Fusion was confirmed only at the final follow-up in the other five patients who did not have regular CT scans. In 13 nonunion patients, the average ROM significantly decreased from 13.0° preoperatively to 4.9° postoperatively (P < 0.01), with screw halos (range, slight to 4 mm). There was no significant change in the proportion of the facet joint space pre- and postoperatively.
The average preoperative ROM of the Fusion, Delayed Union, and Nonunion groups was 9.8°, 10.3°, and 13.0°, respectively, and there was a significant difference between the three groups (P < 0.01). There were also significant differences between the Fusion and Nonunion groups (P < 0.01), Delayed Union and Nonunion groups (P < 0.05), and Fusion plus Delayed Union and Nonunion groups (P < 0.01). That is, the larger the preoperative ROM, the fewer facets fused.
Clinical outcomes
JOABPEQ category scores demonstrated therapeutic effectiveness in 78.2% of the Fusion group, 72.7% of the Delayed Union group, and 90.9% of the Nonunion group for low back pain; 43.4%, 54.5%, and 10.0% of the respective groups for lumbar function; 88.4%, 100%, and 90.9% of the respective groups for walking ability; 64.2%, 63.6%, and 45.5% of the respective groups for Social life function; and 43.2%, 45.5%, and 9.1% of the respective groups for mental health (Fig. 4). There was no significant difference in therapeutic effectiveness between the three groups for any category. Moreover, there was no significant difference between the Fusion and Nonunion groups and between the Fusion plus Delayed Union and Nonunion groups for any category, with the exception of lumbar function (P < 0.05) and mental health (P < 0.05).
Therapeutic effectiveness of facet fusion with the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire category scores. There is no significant difference in therapeutic effectiveness between the three groups for any category. The asterisks indicate significant differences between the Fusion and Nonunion groups and between the Fusion plus Delayed Union and Nonunion groups (P < 0.05). N.S. not significant
The average RMDQ value significantly decreased from 11.3 preoperatively to 4.1 postoperatively in the Fusion group (P < 0.001), from 14.0 preoperatively to 5.5 postoperatively in the Delayed Union group (P < 0.01), and from 9.8 preoperatively to 4.7 postoperatively in the Nonunion group (P < 0.01). Therapeutic effectiveness was 67.4% in the Fusion group, 90.9% in the Delayed Union group, and 50.0% in the Nonunion group. There was no significant difference between the three groups in RMDQ value changes before and after surgery and in therapeutic effectiveness (Fig. 5a).
The average LBP-VAS value significantly decreased from 52.9 preoperatively to 17.1 postoperatively in the Fusion group (P < 0.001), from 52.5 preoperatively to 22.5 postoperatively in the Delayed Union group (P < 0.01), and from 53.9 preoperatively to 30.1 postoperatively in the Nonunion group (P < 0.01). Therapeutic effectiveness was 71.7% in the Fusion group, 60.0% in the Delayed Union group, and 63.6% in the Nonunion group. There was no significant difference between the three groups in LBP-VAS value changes before and after surgery and in therapeutic effectiveness (Fig. 5b).
The average BLP-VAS value significantly decreased from 68.6 preoperatively to 20.4 postoperatively in the Fusion group (P < 0.001), from 62.9 preoperatively to 26.2 postoperatively in the Delayed Union group (P < 0.05), and from 65.1 preoperatively to 23.5 postoperatively in the Nonunion group (P < 0.01). Therapeutic effectiveness was 78.2% in the Fusion group, 70.0% in the Delayed Union group, and 63.6% in the Nonunion group. There was no significant difference between the three groups in BLP-VAS value changes before and after surgery and in therapeutic effectiveness (Fig. 5c).
Complications and revision surgeries
There were no major complications such as implant failure, neural or vascular injury, or deep wound infection. Revision surgery for complications or poor clinical outcomes immediately after surgery was not required. Five patients required revision surgery for adjacent segment disease (ASD) between 1 and 5.5 years after the first surgery (revision surgery rate, 3.7%). Of these five patients, two were in the Fusion group, two in the Delayed Union group, and one in the Nonunion group.
Discussion
This study clearly demonstrated that nonunion cases after FF achieved good clinical outcomes, likely due to the significantly decreased postoperative ROM, indicating unstable spondylolisthesis stabilization. The fusion rate at the 1-year follow-up was 80%, and 10% of the patients achieved fusion thereafter. The larger the preoperative ROM, the fewer facets fused.
Radiographic assessment and fusion rate
The reported interbody fusion rates ranged from 77 to 100% [5]. However, definitive criteria for diagnosing a successful fusion are controversial, and CT is currently recommended as the most reliable assessment method [29]. Authors who reported high fusion rates used flexion-extension radiographs with a 5° angular motion cutoff [4, 13, 19, 23]. Santos et al. reported a fusion rate of 96% with a 5° cutoff using flexion-extension radiographs and 65% using CT [29]. Furthermore, they indicated that none of the nonunions seen on a thin-section helical CT scan was detected when the 5° cutoff was used. They also indicated that most of the levels assessed as having nonunion demonstrated movement of 2°, with 4° as the highest amount of movement measured. FF was assessed by CT, and a fusion rate of 90.4% was thought to be comparable with or higher than other fusion techniques assessed by CT.
Delayed union cases
In this study, 14 cases (10.3%) achieved fusion after the first postoperative year. Of these 14 cases, 12 had no motion at the fused level, and the other two had motion of 3.1° and 3.3° at the 1-year follow-up. Fay et al. reported that FF eventually occurred in 75.6% of patients after Dynesys dynamic stabilization for DLS [7]. Furthermore, Hoppe et al. reported an FF rate of 74.4% after the stabilization [11]. Among the delayed union cases, some without motion at the fused level just needed longer time for bony continuity to be confirmed on CT, and the others, with no fusion but “stabilized,” eventually achieved fusion as these reports.
Nonunion and preoperative intervertebral instability
This study indicated that preoperative intervertebral instability could result in nonunion. There are few reports regarding nonunion and preoperative intervertebral instability [1, 14]. Kornblum et al. reported, in their PLF study, that preoperative average angulation of 10.1° in the pseudarthrosis group was significantly larger than that of 6.6° in the fusion group [14]. They considered pseudarthrosis to be present if there was no continuity in the fusion mass between the transverse processes on the anteroposterior radiographs or if lateral flexion-extension radiographs demonstrated > 2° of angular motion or > 2 mm of sagittal motion at the spondylolisthesis level. In contrast, Agabegi et al. concluded that the translation degree, angular motion, and lateral disc space height could not predict fusion or development of pseudarthrosis [1]. However, they determined fusion if continuous bone bridging was present between the transverse processes, an angulation of ≤ 5°, and a translational movement of ≤ 3 mm on flexion-extension radiographs. In our study, all cases of fusion that were confirmed by CT displayed no motion at the fused level on a flexion-extension radiograph. Agabegi’s lenient fusion criteria may have included pseudarthroses as fusions.
Postoperative stabilization in the nonunion cases
Even if FF failed, unstable spondylolisthesis was stabilized postoperatively with the average ROM significantly decreasing from 13.0° to 4.9°. Postoperative stabilization was thought to be due to facet joint space change, restabilization, scar contracture, and impact of PS, even if it was loosened. Although facet joint orientation was reported to be significantly correlated to DLS [17], orientation-determining lines drawn through the two midpoints of the most anterior and posterior facet joint spaces did not change before and after FF, and we evaluated the joint space proportion. Although there was no significant change in proportion, we found obvious changes in joint space shape, which were thought to contribute to the stability (Fig. 6). Restabilization was occasionally observed in the natural course of DLS, and disc height loss, osteophyte formation, vertebral endplate sclerosis, and ligament ossification have been implicated in the process [30]. Minamide et al. reported that 34.9% of patients with preoperative instability had disc space collapse and restabilization during the 3-year follow-up period even after minimally invasive microendoscopic laminotomy [21].
Clinical outcomes and revision surgery rate of the nonunion cases
Good clinical outcomes were noted even in nonunion cases after FF, likely due to the significantly decreased postoperative ROM, indicating unstable spondylolisthesis stabilization. Fay et al. reported that all patients experienced significant improvement in clinical evaluations after Dynesys dynamic stabilization regardless of whether FF occurred, and that there were no significant differences between patients with and without FF [7]. Ohtori et al. also reported that there were no significant differences between the union and nonunion groups 2 years after PLF [25]. Although the effect of fusion status on clinical outcomes has been controversial, poor outcomes of nonunion cases, even shortly after interbody fusion, have been reported [19, 23]. The poor outcomes may have been due to cage migration or cage-related pain. Although the therapeutic effectiveness of FF with JOABPEQ was low for lumbar function and mental health in the Nonunion group, the other clinical outcomes were as good as the Fusion and Delayed Union groups, and revision surgery for nonunion itself was not required. The revision surgery rate of FF was 3.7% for an average follow-up period of more than 6 years, and ASD was the cause for all revisions. The insertion of cages can result in complications, such as cage migration or cage-related pain, thereby increasing the revision surgery rate of the interbody fusion, which has been reported to be 12.1% [26] and 12.9% [10] at 5 years postoperatively.
Fusion indication for DLS
We found that nonunion cases achieved good clinical results, as well as fusion cases. This poses a clinical question regarding the indication of fusion for DLS. Blumenthal et al. reported that reoperation was performed in 15 (37.5%) of the 40 patients after laminectomy for grade I DLS, despite excluding patients with gross motion of more than 3 mm on flexion-extension radiographs [3]. Minamide et al. reported that19 (7.8%) of 242 patients underwent reoperation due to insufficient decompression and recurrent stenosis caused by disc bulging or instability, even after minimally invasive microendoscopic laminotomy for DLS [21]. We believe that fusion is necessary for unstable DLS to avoid reoperation.
Limitations
This study has several limitations. Firstly, it is not clear whether the 1-year postoperative period was appropriate to assess fusion and to classify groups. Secondly, bone quality was not assessed, which could have implications for fusion rates. Thirdly, the study evaluated mid-term clinical outcomes; further studies are required to clarify long-term outcomes after FF.
Conclusions
This study demonstrated that even nonunion cases after FF achieved good clinical outcomes as well as those after PLF. This is likely due to the significantly decreased postoperative ROM of the slip segment, indicating unstable spondylolisthesis stabilization. FF did not require revision surgery for nonunion itself, and the revision surgery rate of 3.7% was quite low for an average follow-up period of > 6 years. Therefore, FF is useful for DLS management.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Agabegi SS, Majid K, Fischgrund JS, Vaccaro AR, Patel T (2011) Can preoperative radiographic parameters be used to predict fusion in non-instrumented posterolateral fusion for degenerative spondylolisthesis? Spine (Phila Pa 1976) 36(26):E1709–E1714. https://doi.org/10.1097/BRS.0b013e31821d289f
Andersen T, Videbæk TS, Hansen ES, Bünger C, Christensen FB (2008) The positive effect of posterolateral lumbar spinal fusion is preserved at long-term follow-up: a RCT with 11–13 year follow-up. Eur Spine J 17(2):272–280 Epub 2007 Sep 12
Blumenthal C, Curran J, Benzel EC, Potter R, Magge SN, Harrington JF Jr, Coumans JV, Ghogawala Z (2013) Radiographic predictors of delayed instability following decompression without fusion for degenerative grade I lumbar spondylolisthesis. J Neurosurg Spine 18(4):340–346. https://doi.org/10.3171/2013.1.SPINE12537
Challier V, Boissiere L, Obeid I, Vital JM, Castelain JE, Bénard A, Ong N, Ghailane S, Pointillart V, Mazas S, Mariey R, Gille O (2017) One-level lumbar degenerative spondylolisthesis and posterior approach: Is transforaminal lateral interbody fusion mandatory?: a randomized controlled trial with 2-year follow-up. Spine (Phila Pa 1976) 42(8):531–539. https://doi.org/10.1097/BRS.0000000000001857
Chrastil J, Patel AA (2012) Complications associated with posterior and transforaminal lumbar interbody fusion. J Am Acad Orthop Surg 20(5):283–291. https://doi.org/10.5435/JAAOS-20-05-283
Colman MW, Baronne LM 2nd, Brodke DS, Woodbury AM, Annis P, Lawrence BD (2019) Perioperative effects associated with the surgical treatment of degenerative spondylolisthesis: interbody versus no interbody. Clin Spine Surg 32(2):E71–E77. https://doi.org/10.1097/BSD.0000000000000729
Fay LY, Huang WC, Chang CC, Chang HK, Tsai TY, Tu TH, Wu CL, Cheng H, Wu JC (2018) Unintended facet fusions after Dynesys dynamic stabilization in patients with spondylolisthesis. J Neurosurg Spine 30(3):353–361
Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT (1997) Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine (Phila Pa 1976) 22(24):2807–2812
Fukui M, Chiba K, Kawakami M, Kikuchi S, Konno S, Miyamoto M, Seichi A, Shimamura T, Shirado O, Taguchi T, Takahashi K, Takeshita K, Tani T, Toyama Y, Yonenobu K, Wada E, Tanaka T, Hirota Y, Subcommittee of the Clinical Outcome Committee of the Japanese Orthopaedic Association on Low Back Pain and Cervical Myelopathy Evaluation (2009) JOA Back Pain Evaluation Questionnaire (JOABPEQ)/JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ). The report on the development of revised versions April 16, 2007. The Subcommittee of the Clinical Outcome Committee of the Japanese Orthopaedic Association on Low Back Pain and Cervical Myelopathy Evaluation. J Orthop Sci 14(3):348–365. https://doi.org/10.1007/s00776-009-1337-8
Greiner-Perth R, Boehm H, Allam Y, Elsaghir H, Franke J (2004) Reoperation rate after instrumented posterior lumbar interbody fusion: a report on 1680 cases. Spine (Phila Pa 1976) 29(22):2516–2520
Hoppe S, Schwarzenbach O, Aghayev E, Bonel H, Berlemann U (2016) Long-term outcome after monosegmental L4/5 stabilization for degenerative spondylolisthesis with the Dynesys device. Clin Spine Surg 29(2):72–77
Jiang SD, Wu QZ, Lan SH, Dai LY (2012) Reliability of the measurement of thoracolumbar burst fracture kyphosis with Cobb angle, Gardner angle, and sagittal index. Arch Orthop Trauma Surg 132(2):221–225. https://doi.org/10.1007/s00402-011-1394-2 Epub 2011 Sep 13
Kim KT, Lee SH, Lee YH, Bae SC, Suk KS (2006) Clinical outcomes of 3 fusion methods through the posterior approach in the lumbar spine. Spine (Phila Pa 1976) 31(12):1351–1357 discussion 1358
Kornblum MB, Fischgrund JS, Herkowitz HN, Abraham DA, Berkower DL, Ditkoff JS (2004) Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine 29(7):726–733 discussion 733-734
Kuraishi S, Takahashi J, Mukaiyama K, Shimizu M, Ikegami S, Futatsugi T, Hirabayashi H, Ogihara N, Hashidate H, Tateiwa Y, Kinoshita H, Kato H (2016) Comparison of clinical and radiological results of posterolateral fusion and posterior lumbar interbody fusion in the treatment of L4 degenerative lumbar spondylolisthesis. Asian Spine J 10(1):143–152
Kuroki H, Tajima N, Kubo S (2002) Clinical results of posterolateral fusion for degenerative lumbar spinal diseases: a follow-up study of more than 10 years. J Orthop Sci 7(3):317–324
Liu Z, Duan Y, Rong X, Wang B, Chen H, Liu H (2017) Variation of facet joint orientation and tropism in lumbar degenerative spondylolisthesis and disc herniation at L4-L5: a systematic review and meta-analysis. Clin Neurol Neurosurg 161:41–47. https://doi.org/10.1016/j.clineuro.2017.08.005
Lowe TG, Tahernia AD, O'Brien MF, Smith DA (2002) Unilateral transforaminal posterior lumbar interbody fusion (TLIF): indications, technique, and 2-year results. J Spinal Disord Tech 15(1):31–38
Makino T, Kaito T, Fujiwara H, Ishii T, Iwasaki M, Yoshikawa H, Yonenobu K (2014) Does fusion status after posterior lumbar interbody fusion affect patient-based QOL outcomes? An evaluation performed using a patient-based outcome measure. J Orthop Sci 19(5):707–712. https://doi.org/10.1007/s00776-014-0591-6
McAnany SJ, Baird EO, Qureshi SA, Hecht AC, Heller JG, Anderson PA (2016) Posterolateral fusion versus interbody fusion for degenerative spondylolisthesis: a systematic review and meta-analysis. Spine (Phila Pa 1976) 41(23):E1408–E1414
Minamide A, Yoshida M, Simpson AK, Nakagawa Y, Iwasaki H, Tsutsui S, Takami M, Hashizume H, Yukawa Y, Yamada H (2018) Minimally invasive spinal decompression for degenerative lumbar spondylolisthesis and stenosis maintains stability and may avoid the need for fusion. Bone Joint J 100-B(4):499–506. https://doi.org/10.1302/0301-620X.100B4.BJJ-2017-0917.R1
Miyashita T, Ataka H, Kato K, Tanno T (2015) Good clinical outcomes and fusion rate of facet fusion with a percutaneous pedicle screw system for degenerative lumbar spondylolisthesis: minimally invasive evolution of posterolateral fusion. Spine (Phila Pa 1976) 40(9):E552–E557. https://doi.org/10.1097/BRS.0000000000000842
Noshchenko A, Lindley EM, Burger EL, Cain CM, Patel VV (2016) What is the clinical relevance of radiographic nonunion after single-level lumbar interbody arthrodesis in degenerative disc disease?: a meta-analysis of the YODA project database. Spine (Phila Pa 1976) 41(1):9–17. https://doi.org/10.1097/BRS.0000000000001113
Ogura Y, Ogura K, Kobayashi Y, Kitagawa T, Yonezawa Y, Takahashi Y, Yoshida K, Yasuda A, Shinozaki Y, Ogawa J (2020) Minimum clinically important difference of major patient-reported outcome measures in patients undergoing decompression surgery for lumbar spinal stenosis. Clin Neurol Neurosurg 196:105966. https://doi.org/10.1016/j.clineuro.2020.105966
Ohtori S, Suzuki M, Koshi T, Takaso M, Yamashita M, Yamauchi K, Inoue G, Suzuki M, Orita S, Eguchi Y, Ochiai N, Kishida S, Kuniyoshi K, Nakamura J, Aoki Y, Ishikawa T, Arai G, Miyagi M, Kamoda H, Toyone T, Takahashi K (2011) Single-level instrumented posterolateral fusion of the lumbar spine with a local bone graft versus an iliac crest bone graft: a prospective, randomized study with a 2-year follow-up. Eur Spine J 20(4):635–639. https://doi.org/10.1007/s00586-010-1656-7
Park Y, Ha JW, Lee YT, Sung NY (2014) Minimally invasive transforaminal lumbar interbody fusion for spondylolisthesis and degenerative spondylosis: 5-year results. Clin Orthop Relat Res 472(6):1813–1823. https://doi.org/10.1007/s11999-013-3241-y
Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson O, Cheng JS, McGirt MJ (2011) Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 14(5):598–604. https://doi.org/10.3171/2010.12.SPINE10472
Potter BK, Freedman BA, Verwiebe EG, Hall JM, Polly DW Jr, Kuklo TR (2005) Transforaminal lumbar interbody fusion: clinical and radiographic results and complications in 100 consecutive patients. J Spinal Disord Tech 18(4):337–346
Santos ER, Goss DG, Morcom RK, Fraser RD (2003) Radiologic assessment of interbody fusion using carbon fiber cages. Spine (Phila Pa 1976) 28(10):997–1001
Simmonds AM, Rampersaud YR, Dvorak MF, Dea N, Melnyk AD, Fisher CG (2015) Defining the inherent stability of degenerative spondylolisthesis: a systematic review. J Neurosurg Spine 23(2):178–189. https://doi.org/10.3171/2014.11.SPINE1426 Epub 2015 May 15
Tokuhashi Y, Ajiro Y, Umezawa N (2008) Follow-up of patients with delayed union after posterior fusion with pedicle screw fixation. Spine (Phila Pa 1976) 33(7):786–791. https://doi.org/10.1097/BRS.0b013e31816956f7
Turunen V, Nyyssönen T, Miettinen H, Airaksinen O, Aalto T, Hakumäki J, Kröger H (2012) Lumbar instrumented posterolateral fusion in spondylolisthetic and failed back patients: a long-term follow-up study spanning 11–13 years. Eur Spine J 21(11):2140–2148. https://doi.org/10.1007/s00586-012-2320-1
Acknowledgments
The authors wish to thank Dr. Takeo Ishii for advice on statistics.
Author information
Authors and Affiliations
Contributions
TM and TT contributed to the study conception and design. Data collection was performed by all the authors. TM conducted the analysis and interpretation of data. The first draft of the manuscript was written by TM, and all the authors commented on previous versions of the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declare that they have no conflicts of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Medical Ethics Committee of our hospital (#25-13).
Informed consent
For this type of study formal consent is not required.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Informed consent for publication was obtained.
Code availability
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miyashita, T., Ataka, H., Kato, K. et al. Good clinical outcomes in nonunion cases after facet fusion with a percutaneous pedicle screw system for degenerative lumbar spondylolisthesis. Neurosurg Rev 44, 2847–2855 (2021). https://doi.org/10.1007/s10143-021-01479-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-021-01479-4