Abstract
The iliac crest bone grafting (ICBG) technique for lumbar posterolateral fusion surgery is widely used; however, donor site problems such as pain and sensory disturbance have been reported. Local bone is available for fusion surgery, but its reliability as a graft has not been fully reported. In the current study, we examined single-level instrumented posterolateral fusion with a local bone graft versus an ICBG in a prospective randomized study. Eighty-two patients diagnosed with L4 degenerated spondylolisthesis were divided into two groups at random. Forty-two patients underwent instrumented posterolateral fusion with a local bone graft (L4–L5 level), and 40 patients underwent instrumented posterolateral fusion with an ICBG (L4–L5 level). Rate and duration of bone union, visual analog scale (VAS) score, Japanese orthopedic association score (JOAS), Oswestry Disability Index (ODI), and complications were evaluated before and 2 years after therapy. VAS score, JOAS, and ODI were not significantly different between the two groups before and after surgery (P > 0.05). Rate and average duration of bone union were 90% and 8.5 months in the local bone graft group, and 85% and 7.7 months in the ICBG group, but without significant difference (P > 0.05). Prolonged surgical time and complications such as donor site pain (8 patients) and sensory disturbance (6 patients) were observed in the ICBG group. If single-level posterolateral fusion was performed, local bone graft technique has the same bone union rate compared with ICBG, requires less surgical time, and has fewer complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Degenerative lumbar spondylolisthesis accompanied by low back pain and leg pain is sometimes treated with surgery when conservative treatment fails. Instrumentation surgery such as posterolateral fusion combined with a bone graft has been widely used for degenerated lumbar spondylolisthesis.
Autologous iliac crest bone grafting (ICBG) is considered the gold standard in lumbar spinal fusion. However, the outcome of autograft use in lumbar spine fusion is associated with donor-site morbidity, such as risk of infection, hematoma, fracture, wound healing problems, and donor-site pain [1, 4, 5, 8, 11]. These complications caused by the bone graft harvesting can result in disability and thus increase the recovery time and patient care costs.
To avoid donor-site problems, there have been several reports of the use of local bone in lumbar fusion. Successful fusion has been reported using local bone alone for long posterolateral fusion in adolescent idiopathic scoliosis [10]. Local in situ autografts in instrumented posterolateral fusion of the lower lumbar or lumbosacral spine for treating degenerative spondylolisthesis have been evaluated [6]. Successful fusion mass was radiographically confirmed in 93% of patients at the arthrodesis level [6]. Clinical and radiologic outcome of instrumented posterolateral lumbar fusion using local bone versus autogenous ICBG have been evaluated retrospectively [9]. There was no significant difference in single-level fusion rate and overall clinical outcome between the two groups [9]. The investigators concluded that local bone graft alone achieved a similar clinical outcome, but with less morbidity irrespective of number of fusion levels [9]. However, there has been no study using a prospective randomized method.
The purpose of the current study was to examine the difference in bone union and clinical results after single-level posterolateral fusion surgery using a local bone graft versus an ICBG, in a prospective randomized study.
Methods
The ethics committee of our institution approved the protocol for the human procedures used in this study.
Patients
Patients had low back and leg pain, continuing for at least 12 months. Patients were diagnosed with lumbar degenerated spondylolisthesis at the L4 level with spinal stenosis between L4 and L5 level. X-ray examination, myelography, computed tomography (CT) after myelography, and magnetic resonance imaging (MRI) were performed in all patients for diagnosis.
Patients who had previously undergone spinal surgery were excluded. We also excluded spinal tumor, infection, and trauma.
Diagnosis of L4 spondylolisthesis and inclusion criteria for fusion surgery were (1) >5% slip of L4 vertebra in a neutral position; or (2) >3 mm translation between flexion and extension positions on radiographic evaluation.
The patients were randomized according to the minimization method for surgery using local bone graft or surgery using ICBG [7]. We employed sex and age as stratification factors. Details of the patients’ backgrounds are shown in Table 1.
All patients underwent decompression (L4–L5 laminotomy) and posterolateral fusion surgery at a single level between L4 and L5. Posterolateral fusion was performed using pedicle screws and a bone graft. Local bone consisted of spinal processes of both L4 and L5 and lamina between L4 and L5. Only local bone was transplanted in the local bone graft group. ICBG was harvested from the left iliac bone using a separate skin incision. Cortex and cancellous bone were obtained from the outer side of the iliac crest (length 40 mm, depth 30 mm). For the ICBG group, both ICBG and local bone obtained at decompression were transplanted. To evaluate the efficacy of each method we determined the amount of local bone graft in each patient. We measured the entire volume and then averaged this over the number of segments (2 segments).
We evaluated the change in low back and leg pain before and after surgery. To evaluate the pain score, the visual analog scale (VAS) score (0 no pain, 10 worst pain), Japanese orthopedic association score (JOAS: 0 worst pain, 3 no pain), and Oswestry Disability Index (ODI) were recorded before and 24 months after surgery and compared.
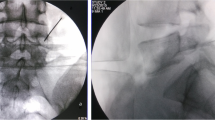
Radiography was used for evaluation of bone union. Profile views of X-ray images at flexion and extension positions before and 3, 6, 9, 12, 18, and 24 months after surgery were evaluated. We defined bone union of <1.5° as instability between the flexion and extension positions.
Computed tomography was performed to evaluate bone union at 6, 12, 18, and 24 months after surgery. We defined bone union as bridging bone formation across the transverse process between adjacent vertebrae.
Evaluation of bone union was blinded and performed by three observers. If at least two of the observers concurred, bone union was used to define the period of bone union.
Statistical analysis
Data were compared using a Mann–Whitney U test. P < 0.05 was considered statistically significant.
Results
Table 1 shows demographic characteristics in patients before surgery. There was no significant difference in patients’ background, low back pain score, and leg pain score between the local bone graft and ICBG groups (P > 0.05).
Intraoperative measurements are shown in Table 2. Surgical time in the local bone graft group was significantly shorter than that of the ICBG group (P = 0.045). However, there was no significant difference in blood loss between the two groups (P > 0.05). The total volume of local bone and the volume of graft bone used for one segment were 14.0 ± 3.0 and 7.0 ± 2.1 g, respectively. Total volume of ICGB and the volume of graft bone used for one segment were 22.0 ± 4.5 and 10.0 ± 2.9 g, respectively.
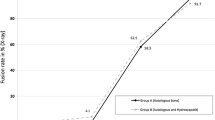
Evaluation of bone fusion is shown in Table 3. Most patients show bone union at final follow-up (24 months after surgery). The ratio of bone union was 83% (evaluation by X-ray examination) and 90% (CT) in the local bone graft group, and 85 and 85% in the ICBG group, respectively. There was no significant difference in the ratio of bone fusion evaluated by X-ray examination and CT between the two groups (P > 0.05). The average period of bone union was 7.5 months (evaluation by X-ray examination) and 8.5 months (CT) after surgery in the local bone graft group. The average period of bone union was 8.0 months (evaluation by X-ray examination) and 7.7 months (CT) after surgery in the ICBG group. There was no significant difference in average period for bone union between the two surgical groups (P > 0.05). Four patients in the local bone graft group did not show bony union, nor did six patients in ICBG group at final follow-up using CT evaluation. We observed loosening of pedicle screws in all patients; however, we did not observe breakage of screws or rods.
Pain score
VAS score, JOAS, and ODI were not significantly different between the two groups before surgery (P > 0.05) (Table 1). In both groups, VAS score, JOAS, and ODI significantly improved after surgery compared with before surgery (P < 0.01). VAS score, JOAS, and ODI at final follow-up (24 months) after surgery were not significantly different between the two groups (P > 0.05). There was no significant difference in VAS score, JOAS, and ODI at final follow-up (24 months) after surgery among bone union in the local bone graft group, bone non-union in the local bone graft group, bone union in the ICBG group, and bone non-union in the ICBG group (P > 0.05) (Table 4).
Complications at final follow-up
Table 5 shows complications at final follow-up. There was a deep infection (surgical site infection) in the local bone graft group. There was no other complication in the local bone graft group. However, sensory disturbance around the iliac crest in eight patients and donor site pain in six patients were found in the ICBG group.
Discussion
In the current study, bone union, clinical results, and complications were examined after single-level posterolateral fusion surgery using a local bone graft versus an ICBG in a prospective randomized study. Rate and average duration of bone union were not significantly different in the local bone and ICBG groups. However, prolonged surgical time and complications such as donor site pain were observed in the ICBG group.
Some authors have reported complications from harvesting ICBG [1, 4, 5, 8, 11]. A consecutive series of 261 patients, whose bone graft harvest was conducted by one surgeon, was studied [5]. Major complications such as hematoma, wound infection, reoperation, and chronic severe pain occurred in 10% of patients [5]. Minor complications such as dysesthesia and superficial infection occurred in 39% of patients [5]. In the current study, sensory disturbance around the iliac crest in eight patients (20%) and donor site pain in six patients (15%) were seen in the ICBG group 2 years after surgery.
Some authors have reported the efficacy of instrumented posterolateral fusion using ICBG for degenerated spondylolisthesis when compared with decompression only or non-instrumented posterolateral fusion [2, 12]. Prospective studies evaluating fusion rate using instrumented posterolateral fusion with ICBG showed results from 82 to 95% [2, 12]. There has been one report comparing the clinical and radiologic outcome of instrumented posterolateral lumbar fusion using local bone versus an autogenous ICBG using a retrospective comparative study [9]. Overall fusion rate was higher in the ICBG group (75%) compared with the local bone graft group (65%), but not significantly different [9]. In the current prospective randomized study, fusion rate using local bone graft and ICBG was consistent with the previous studies.
Clinical results after surgery were not significantly different between the local bone graft and ICBG groups in the current study. However, surgical time was significantly shorter for the local bone graft group compared with the ICBG group. As seen in the retrospective comparison between the two groups [9], there was no significant difference in overall clinical outcome between the two groups. However, blood loss and hospital stay were significantly less for the local graft bone group compared with the ICBG group. In this regard, the current and previous studies demonstrated that the local bone graft technique may be less invasive for patients during and after surgery.
It is interesting that there was no significant difference in VAS score, JOAS, and ODI at final follow-up among bone union in the local bone graft group, bone non-union in the local bone graft group, bone union in the ICBG group, and bone nonunion in the ICBG group in the current study. Some authors have reported a discrepancy between bone union and clinical results [2, 3]. Fischgrund et al. [2] reported that successful arthrodesis occurred in 83% of the instrumented posterolateral fusion surgery. However, successful fusion was not predictive of successful patient outcome [2]. Fifty patients who had spinal stenosis associated with degenerative lumbar spondylolisthesis were prospectively studied clinically and radiographically to determine if concomitant intertransverse-process arthrodesis provided better results than decompressive laminectomy alone [3]. Pseudoarthrosis of the fusion mass was seen in 36% of patients; however, the clinical results were excellent. They concluded that the development of a fibrous union appeared to provide sufficient structural support to prevent progressive olisthesis [3].
The current study has some limitations. It is a small-sized randomized trial and the number of patients was restricted. Second, only the VAS score, JOAS, and ODI were used to evaluate LBP and leg pain; more scores from other evaluative methods would strengthen our findings. Third, because the bone quality of each patient is an important issue, we did not measure bone mineral density. Fourth, we evaluated bone union by functional X-ray imaging and CT. We defined bone union of <1.5° as instability between the flexion and extension positions; however, this method has not been standardized. Fifth, in the current study, we performed massive decompression and harvested local bone consisting of spinal processes of both L4 and L5 and lamina between L4 and L5 (laminotomy). There is a possibility that this procedure may promote adjacent syndrome. If decompression is small, local bone may be insufficient for bony union. Further study is required to clarify these points.
In conclusion, the current prospective randomized study demonstrated that clinical pain scores, rate and average duration of bone union were not significantly different after single-level posterolateral fusion surgery between using local bone or ICBG. However, prolonged surgical time and complications such as donor site pain and sensory disturbance were observed in the ICBG group. The authors recommend local bone grafts for instrumented posterolateral fusion surgery in single-level cases.
References
Fernyhough JC, Schimandle JJ, Weigel MC, Edwards CC, Levine AM (1992) Chronic donor site pain complicating bone graft harvesting from the posterior iliac crest for spinal fusion. Spine 17:1474–1480
Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT (1997) Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine 22:2807–2812
Herkowitz HN, Kurz LT (1991) Degenerative lumbar spondylolisthesis with spinal stenosis. J Bone Joint Surg Am 73:802–807
Hu R, Hearn T, Yang J (1995) Bone graft harvest site as a determinant of iliac crest strength. Clin Orthop 310:252–256
Kurz LT, Garfin SR, Booth RE Jr (1989) Harvesting autogenous iliac bone grafts: a review of complications and techniques. Spine 14:1324–1331
Lee S-C, Chen J-F, Wu C-T, Lee ST (2009) In situ local autograft for instrumented lower lumbar or lumbosacral posterolateral fusion. J Clin Neurosci 16:37–43
Pocock SJ, Simon R (1975) Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics 31:103–115
Sasso RC, LeHuec JC, Shaffrey C, Spine Interbody Research Group (2005) Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: a prospective patient satisfaction outcome assessment. J Spinal Disord Tech 18:S77–S81
Sengupta DK, Truumees E, Patel CK, Kazmierczak C, Hughes B, Elders G, Herkowitz HN (2006) Outcome of local bone versus autogenous iliac crest bone graft in the instrumented posterolateral fusion of the lumbar spine. Spine 31:985–991
Violas P, Chapuis M, Bracq H (2004) Local autograft bone in the surgical management of adolescent idiopathic scoliosis. Spine 29:189–192
Younger EM, Chapman MW (1989) Morbidity at bone graft donor sites. J Orthop Trauma 3:192–195
Zdeblick TA (1993) A prospective, randomized study of lumbar fusion. Spine 18:983–991
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ohtori, S., Suzuki, M., Koshi, T. et al. Single-level instrumented posterolateral fusion of the lumbar spine with a local bone graft versus an iliac crest bone graft: a prospective, randomized study with a 2-year follow-up. Eur Spine J 20, 635–639 (2011). https://doi.org/10.1007/s00586-010-1656-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-010-1656-7