Abstract
Non-accidental trauma is a significant source of morbidity and mortality in the pediatric population. Given the vulnerable state of the child, the radiologist can often provide valuable diagnostic information in the setting of suspected abuse. This review focuses on common findings of abusive trauma and serves as a guide to aid in clinical decision-making for providers of emergency medicine and pediatrics. Amid this discussion is an assessment of modern controversies regarding reported mimicking pathologies, recapitulation of the current state of evidence with respect to radiologic findings of abuse, and examination of the contribution that spine imaging may add to the diagnosis of possible abusive head trauma in the acutely injured child. Recommendations for avoiding pitfalls regarding the dating of intracranial injuries are discussed, and illustrated depictions of perpetrator-induced pathology are provided to aid in the understanding of these injuries. Through the use of the appropriate approach to imaging and evidence-based guidelines regarding radiologic findings, the role of radiology is to provide fundamental clues to diagnose and prevent recurrence of abusive injury in patients who cannot speak for themselves.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Child maltreatment is frequently encountered in the emergency setting and resulted in 3.6 million child abuse referrals submitted to Child Protection Services nationally in 2014 with 1546 reported deaths, 70.7 % of which were ascribed to children under the age of 3 years [1]. Medical imaging is often crucial in identifying non-accidental trauma (NAT), as physical signs of abuse are not always present in the abused child. This review focuses on the radiologic approach to diagnosing NAT from the initial stages of exam selection to the accepted evidence basis for abuse-related trauma. Modern controversies and mimicking pathologies are also addressed.
Approach to imaging
The radiograph serves as the initial imaging approach to the suspected victim of abusive trauma, as osseous injuries are second only to skin wounds as signs of child maltreatment [2]. Healing fractures indicative of non-accidental injury may be identified as incidental lesions raising suspicion for NAT. In the initial work-up of alleged abuse, the American College of Radiology (ACR) and the Society for Pediatric Radiology (SPR) Skeletal Survey Practice Parameter [3] specifies the expected radiographic views inherent to the work-up for children under the age of 2 years (Table 1). Additional dedicated radiographs may be warranted due to skeletal survey findings, and as such, many radiology departments require validation of the skeletal survey as complete by the radiologist before the patient is released. The most recent addition to the parameter was the inclusion of bilateral oblique rib radiographs which was supported by the findings of Marine et al. in 2014 [4]. Adherence to this full radiographic series is recommended, and separation from the primary caregiver may be necessary to perform a complete series.
Non-contrast-enhanced computed tomography (CT) of the head is often indicated in the emergency setting when head trauma is suspected, even despite a lack of focal neurologic symptoms [5], as intracranial pathology can exist in the setting of a normal physical exam or lack of retinal hemorrhage [6]. CT improves sensitivity for skull fractures, especially when volumetric and multiplanar reconstructions are employed. CT also allows for assessment of intracranial injury. When available, iterative reconstruction and other age-appropriate dose reduction techniques should be instituted to reduce radiation exposure to the child [7]. Further evaluation with MRI may be helpful in the setting of an abnormal CT exam.
Nuclear medicine bone scan (skeletal scintigraphy) has been described as an adjunct to radiography in the work-up of non-accidental trauma [8]. Scintigraphy may improve evaluation for fracture by 25–50 %, especially in the posterior ribs, spine, and acromion [9]. The time-intensive nature of this technique may require sedation, and this modality is now less commonly used, especially in the emergent setting.
CT of the abdomen and pelvis may be appropriate as necessary per the same clinical parameters as utilized in general trauma, particularly if there is suspicion for solid organ or visceral injury. Intravenous contrast material is necessary for the evaluation of solid organ injury [5]. There are no specific radiologic findings of abusive trauma in the abdomen or pelvis; however, unexplained serologic evidence of solid organ insult may prompt imaging. In these cases, careful attention to the osseous structures may reveal evidence of a healing fracture which would strengthen the likelihood of repetitive injury (Fig. 1).
Non-accidental fracture patterns
Non-accidental osseous injuries have been classically described [10] as either high, moderate, or low specificity (Table 2). The likelihood of non-accidental injury increases when injuries are discordant with the caregiver’s history, when reported mechanisms are unexpected for the child’s developmental status, or when fractures of different ages are uncovered.
The classic metaphyseal lesion (CML) is a highly specific fracture for abusive trauma in a child less than 1 year of age. Descriptors such as “bucket handle fracture” and “corner fracture” have been used synonymously with the CML, though the pathophysiology of the fracture mechanics does not differ between these two radiologic presentations. The difference in appearance is due to variable radiographic projections [11]. A CML occurs when a shearing force is applied to long bone resulting in avulsion of the metaphysis and a characteristic fracture appearance (Figs. 2 and 3). Although the CML has been postulated to be associated with birth-related trauma [12], this lesion is not typically associated with falls [13]. It has been hypothesized that histologic and radiographic findings of the CML are similar to healing rickets in an infant [14] which continues to stir controversy among experts; however, the Society for Pediatric Radiology Child Abuse Committee reaffirmed the association of the CML with abusive trauma in 2014 [15]. Additionally, a 2016 retrospective review of child abuse investigations showed strong association with traumatic injury [16]. A consensus statement by the Board of Directors of the Society for Pediatric Radiology in 2016 outlined the role of vitamin D in bone health in a multidisciplinary review of childhood fracture epidemiology which compared lesions associated with metabolic disease to traumatic findings [17].
Classic metaphyseal lesions. The white arrows show the radiographic correlate to the distal femoral metaphyseal separation depicted in Fig. 2. The black arrow designates the “bucket handle” radiographic appearance in the proximal tibia
Along with the classic metaphyseal lesion, posterior and lateral rib fractures have a high association with non-accidental trauma [18, 19] in children less than 1 year of age. Posterior and lateral rib fractures occur with squeezing of the child (Figs. 4 and 5) and are more likely to manifest in the rib head and neck given the proximity to the transverse processes of the spine. Cardiopulmonary resuscitation (CPR), when performed on the infant in the supine position with support of the back, had previously been shown to be associated with anterior rib fractures in rare instances [20]. Though there is conflicting evidence as to whether or not the more commonly employed “two-thumbs” technique has resulted in increases in acute posterior rib fractures in resuscitated children [21, 22], the presence of healing fractures in a child without recent CPR remains highly suggestive for non-accidental injury.
Long bone and clavicular shaft fractures are commonly encountered in the pediatric emergency setting; however, specificity for abusive trauma declines as patients become able to walk on their own. Although oblique tibia fractures in ambulatory children are termed “toddler fractures” to connote an accidental mechanism, stress and compression fractures of the fibula, metatarsals, and tarsals are similarly common findings of accidental trauma in this age group [23].
Abusive head trauma
Abusive head trauma (AHT) is the most common form of non-accidental injury leading to death in children less than 1 year of age [24–27]. The vast spectrum of abusive head injuries includes collision with a stationary object, direct blow to the cranium, and alternating acceleration and deceleration. Infants are particularly at risk for traumatic brain injury as a result of being shaken back and forth (Fig. 6) due to the relative weight of the head compared to the rest of the body and relative lack of strength of the infant neck musculature. Primary and contre coup intracranial manifestations are similar to accidental injuries.
Isolated linear skull fractures are lower in specificity for abusive head trauma, and the presence of a cranial fracture may or may not be associated with intracranial hemorrhage. The inability to date skull fractures without coexisting superficial soft tissue or intracranial pathology also mires the differential diagnosis in cases of suspected abuse. Nonetheless, an isolated skull fracture in a child without a substantiated accidental cause for the injury should prompt a skeletal survey [5] to rule out additional injury. When skull fractures are encountered, three-dimensional (3D) reformatting of the cranium is helpful to improve evaluation of the skull by aiding in the differentiation of accessory sutures and wormian bones from subtle fractures. Numerous wormian bones may suggest a primary bone disorder such as osteogenesis imperfecta. The presence of multiple fractures, bilateral fractures, and fractures crossing suture lines may indicate AHT [28].
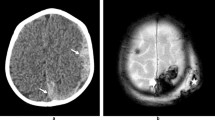
Extra-axial fluid collections (Fig. 7) are often encountered in abusive head trauma, and ordering clinicians would obviously benefit from information related to age of these fluid accumulations. Caution to the radiologist is advised in dating these collections by CT attenuation values, as hyperacute and acute hematomas may contain a mixture of cerebrospinal fluid (CSF) and blood products (hematohygroma) which limits specificity. While the presence of a high attenuation extra-axial fluid collection is concordant with acute hematoma, a homogeneously low attenuation collection may manifest acutely in the setting of arachnoid shearing. Because of these confounding variables, the use of CT to date extra-axial fluid collections must often be reserved for instances in which previous imaging is available.
Though access to MRI in the pediatric emergency setting is variable and often dependent on local resources (magnet availability, anesthesiology services, etc.), follow-up MRI is often indicated when an initial CT demonstrates a previously undocumented intracranial injury [29]. When employed, the use of MRI to evaluate for the presence of suspected bridging vein thrombosis (Fig. 8) in patients with subdural hematoma can increase specificity for a traumatic cause for the injury [30, 31]. It should be emphasized that the signal changes of subdural hemorrhage evolve at a much slower rate than intraparenchymal hemorrhage on both CT and MRI [32] which makes exact dating impossible. Chronic subdural hematomas may be suggested by the presence of membranes within the collection and may not have evidence of prior hemorrhage on SWI or GRE sequences [33]. While subdural hematomas (whether at the site of an externally visible injury or attributable to shearing forces of shaking) are the most common intracranial finding in non-accidental trauma, the nonspecific nature of this finding merits close correlation to clinical symptomology and patient history.
Susceptibility-weighted brain MRI demonstrating bridging vein thrombosis in a pattern referred to as the “tadpole sign” [30]
Parturitional subdural hemorrhages commonly occur regardless of the delivery method, and these fluid collections may occur in the same location as subdural hematomas due to head trauma. Birth-related subdural hemorrhages should resolve within 4 weeks and should not exhibit worsening clinical symptomatology [26]. Extra-axial blood products persisting beyond the first month of life merit additional consideration for non-accidental etiology.
Intra-axial injuries including intraparenchymal hematomas are nonspecific for abusive head trauma yet are regularly encountered in the abused child and correlate with poor neurologic outcome [34]. Both CT and MRI can provide prognostic information by demonstrating mass effect, cisternal effacement, and need for neurosurgical intervention.
Imaging of the spine has been advocated in cases of suspected non-accidental trauma due to the high incidence of ligamentous injury and visualization of extra-axial hemorrhage in the spine. Choudhary et al. reported that spinal canal subdural hematoma was significantly more common among children with abusive head trauma who had undergone thoracolumbar imaging [35] than accidental trauma, and a subsequent study demonstrated a significant correlation between nuchal, interspinous, and posterior occipital-atlantal-axial ligamentous injury and abusive head trauma [36]. Ensuing research has shown a positive association between ischemic changes observed on brain MRI and MRI-proven cervical spine injury in children with confirmed NAT [37]. Given these relationships, MRI of the spine is likely to emerge as a recommended initial imaging tool in the work-up of children with suspected abusive trauma.
Although isolated intracranial pathology is less specific for non-accidental injury than the higher specificity fracture patterns discussed above, even a low suspicion for abusive head trauma should warrant appropriate follow-up given the morbidity and mortality of trauma-related intracranial pathology. Additional physical exam findings such as retinal hemorrhage may raise suspicion for child abuse, but concordance of injury patterns with the history provided by the caregiver is often the salient element of prompting the appropriate inquiry.
Confounding pathologies
Patients with metabolic bone disease such as that seen in rickets (Fig. 9), Caffey disease, and osteogenesis imperfecta (Fig. 10) are more susceptible to fracture. To delineate non-accidental injury from fracture due to underlying bone disease, correlation can be made to prior radiography, the radiographic appearance of the bones, serologic testing, and physical exam. Herein lies the value of the skeletal survey, as metabolic disease should manifest in a predictable diffuse pattern, whereas injury due to trauma is more likely to be focal. Radiologists and emergency medicine providers would be well-served to review literature germane to the defense of the alleged perpetrator [14, 38] as well as the accepted conclusions of the Society of Pediatric Radiology [17] regarding metabolic bone disease and the 2015 study by Perez-Rossello et al. demonstrating the absence of rickets in infants with fatal abusive head trauma and classic metaphyseal lesions [39].
Benign enlarged subarachnoid spaces (BESS) are commonly encountered in children less than 1 year of age [40], and an association has been reported between subdural hemorrhage and BESS. Although much data regarding the linkage between BESS and subdural hematoma is based on case series reports of less than 20 children [41–44], an isolated subdural hematoma in the setting of known BESS may or may not be due to abusive head trauma. In cases of potential abusive head trauma, MRI can be helpful to determine if a subdural collection contains hemorrhagic products.
An additional confounding intracranial pathology is glutaric aciduria type 1 [27], a condition associated with brain atrophy and subdural fluid collections. This is a rare metabolic disorder occurring in 1 out of 30,000 births [45] and can be diagnosed through advanced serologic testing [46]. Menkes Syndrome, also a rare metabolic disorder involving copper storage identifiable through genetic studies and hair analysis, can generate findings that overlap with non-accidental trauma [47, 48].
Conclusion
When suspected non-accidental trauma is encountered in the emergency setting, selecting the appropriate radiographic study often provides a critical screening and diagnostic role in evaluation. Careful correlation between physical exam findings, radiologic testing, and the reported history must be taken into account in each case. Aided with proper evidence-based medicine, the clinician and radiologist can make appropriate recommendations while preventing future cases of child abuse.
References
U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau (2016) Child maltreatment 2014. Available at http://www.acf.hhs.gov/programs/cb/research-data-technology/statistics-research/child-maltreatment. Accessed October 1, 2016
Christian CW, Committee on Child Abuse and Neglect, American Academy of Pediatrics (2015) The evaluation of suspected child physical abuse. Pediatrics 135:e1337–e1354
ACR-SPR Practice Parameter for Performing Skeletal Surveys in Children. American College of Radiology; Amended 2016. Available at http://www.acr.org/~/media/9bdcdbee99b84e87baac2b1695bc07b6.pdf. Accessed October 1, 2016
Marine MB, Corea D, Steenburg SD, Wanner M, Eckert GJ, Jennings SG, Karmazyn B (2014) Is the new ACR-SPR practice guideline for addition of oblique views of the ribs to the skeletal survey for child abuse justified? Am J Roentgenol 202:872–879
ACR Appropriateness Criteria Suspected Physical Abuse—Child, 2016 Available at https://acsearch.acr.org/docs/69443/Narrative/. Accessed October 1
Rubin DM, Christian CW, Bilaniuk LT, Zazyczny KA, Durbin DR (2003) Occult head injury in high-risk abused children. Pediatrics 111:1382–1386
Zarella C, Didier R, Berquist C, Bardo DM, Selden NR, Kuang RR (2016) A reduction in radiation exposure during pediatric craniofacial computed tomography. J Craniofac Surg 27:331–333
Mandelstam SA, Cook D, Fitzgerald M, Ditchfield MR (2003) Complementary use of radiological skeletal survey and bone scintigraphy in detection of bony injuries in suspected child abuse. Arch Dis Child 88:387–390
Conway JJ, Collins M, Tanz RR, Radkowsi MA, Anandappa E, Hernandez R, Freeman EL (1993) The role of bone scintigraphy in detecting child abuse. Semin Nucl Med 23:321–333
Offiah A, van Rijn RR, Mercedes Perez-Rosello J, Kleinman PK (2009) Skeletal imaging of child abuse (non-accidental injury). Pediatr Radiol 39:461–470
Kleinman PK, Marks SC (1995) Relationship of the subperiosteal bone collar to metaphyseal lesions in abused infants. J Bone Joint Surg Am 77:1471–1476
Snedecor ST, Wilson HB (1949) Some obstetrical injuries to the long bones. J Bone Joint Surg Am 31A:378–384
Lyons TJ, Oates RK (1993) Falling out of bed: a relatively benign occurrence. Pediatrics 92:125–127
Ayoub DM, Hyman C, Cohen M, Miller M (2014) A critical review of the classic metaphyseal lesion: traumatic or metabolic? Am J Roentgenol 202:185–196
Brown SD, Serveas S, Hayes LL (2014) Child abuse committee response regarding classic metaphyseal lesion. Am J Roentgenol 203:W232
Thackeray JD, Wannemacher J, Adler BH, Lindberg DM (2016) The classic metaphyseal lesion and traumatic injury. Pediatr Radiol 46:1128–1133
Servaes S, Brown SD, Choudhary AK, Christian CW, Done SL, Hayes LL, Levine MA, Moreno JA, Palusci VJ, Shore RM, Slovis TL (2016) The etiology and significance of fractures in infants and young children: a multidisciplinary review. Pediatr Radiol 46:591–600
Barsness KA, Cha ES, Baensard DD, Calkins CM, Patrick DA, Karrer FM, Strain JD (2003) The positive predictive value of rib fractures as an indicator of nonaccidental trauma in children. J Trauma 54:1107–1110
Bulloch B, Schubert CJ, Brophy PD, Johnson N, Reed MH, Shapiro RA (2000) Cause and clinical characteristics of rib fractures in infants. Pediatrics 105:E48
Maguire S, Mann M, John N, Ellaway B, Sibert JR, Kemp AM (2006) Does cardiopulmonary resuscitation cause rib fractures in children? A systematic review. Child Abuse Negl 30:739–751
Franke I, Pingen A, Schiffmann H, Vogel M, Vlajnic D, Ganschow R, Born M (2014) Cardiopulmonary resuscitation (CPR)-related posterior rib fractures in neonates and infants following recommended changes in CPR techniques. Child Abuse Negl 38:1267–1274
Reyes JA, Somers GR, Taylor GP, Chiasson DA (2011) Increased incidence of CPR-related rib fractures in infants—is it related to changes in CPR technique? Resuscitation 82:545–548
John SD, Moorthy CS, Swischuk LE (1997) Expanding the concept of the toddler’s fracture. Radiographics 17:367–376
Bruce DA, Zimmerman RA (1989) Shaken impact syndrome. Pediatr Ann 18:482–492
Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH (2003) A population-based study of inflicted traumatic brain injury in young children. JAMA 290:621–626
Girard N, Brunel H, Dory-Lautrec P, Chabrol B (2016) Neuroimaging differential diagnoses to abusive head trauma. Pediatr Radiol 46:603–614
Fernando S, Obaldo RE, Walsh IR, Lowe LH (2008) Neuroimaging of nonaccidental head trauma: pitfalls and controversies. Pediatr Radiol 38:827–838
Meservy CJ, Towbin R, McLaurin RL, Myers PA, Ball W (1987) Radiographic characteristics of skull fractures resulting from child abuse. AJR Am J Roentgenol 149:173–175
Foerster BR, Petrou M, Lin D, Thurnher MM, Carlson MD, Strouse PJ, Sundgren PC (2009) Neuroimaging evaluation of non-accidental head trauma with correlation to clinical outcomes: a review of 57 cases. J Pediatr 154:573–577
Hahnemann ML, Kinner S, Schweiger B, Bajanowski T, Karger B, Pfeiffer H, Wittschieber D (2015) Imaging of bridging vein thrombosis in infants with abusive head trauma: the “Tadpole Sign”. Eur Radiol 25:299–305
Choudhary AK, Bradford R, Dias MS, Thamburaj K, Boal DK (2015) Venous injury in abusive head trauma. Pediatr Radiol 45:1803–1813
Vezina G (2009) Assessment of the nature and age of subdural collections in nonaccidental head injury with CT and MRI. Pediatr Radiol 39:586–590
Cramer JA, Rassner UA, Hedlund GL (2016) Limitations of T2*-gradient recalled-echo and susceptibility-weighted imaging in characterizing chronic subdural hemorrhage in infant survivors of abusive head trauma. AJNR Am J Neuroradiol 37:1752–1756
Colbert CA, Holshouser BA, Aaen GS, Sheridan C, Oyoyo U, Kido D, Ashwal S (2010) Value of cerebral microhemorrhages detected with susceptibility-weighted MR imaging for prediction of long-term outcome in children with nonaccidental trauma. Radiology 256:898–905
Choudhary AK, Bradford RK, Dias MS, Moore GJ, Boal DK (2012) Spinal subdural hemorrhage in abuse head trauma: a retrospective study. Radiology 262:216–223
Choudhary AK, Ishak R, Zacharia TT, Dias MS (2014) Imaging of spinal injury in abusive head trauma: a retrospective study. Pediatr Radiol 44:1130–1140
Jacob R, Cox M, Koral K, Greenwell C, Xi Y, Vinson L, Reeder K, Weprin B, Huang R, Booth TN (2016) MR imaging of the cervical spine in nonaccidental trauma: a tertiary institution experience. AJNR Am J Neuroradiol 37:1944–1950
Somers JM, Halliday KE, Chapman S (2014) Humeral fracture in non-ambulant infants—a possible accidental mechanism. Pediatr Radiol 44:1219–1223
Perez-Rossello JM, McDonald AG, Rosenberg AE, Tsai A, Kleinman PK (2015) Absence of rickets in infants with fatal abusive head trauma and classic metaphyseal lesions. Radiology 275:810–821
Hamza M, Bodensteiner JB, Noorani PA, Barnes PD (1987) Benign extracerebral fluid collections: a cause of macrocrania in infancy. Pediatr Neurol 2:218–221
Amodio J, Spektor V, Pramanik B, Rivera R, Pinkney L, Fefferman N (2005) Spontaneous development of bilateral subdural hematomas in an infant with benign infantile hydrocephalus: color Doppler assessment of vessels traversing extra-axial spaces. Pediatr Radiol 35:1113–1117
Ghosh PS, Ghosh D (2011) Subdural hematoma in infants without accidental injury: benign external hydrocephalus, a risk factor. Clin Pediatr 50:897–903
Ravid S, Maytal J (2003) External hydrocephalus: a probable cause for subdural hematoma in infancy. Pediatr Neurol 28:139–141
Pittman T (2003) Significance of a subdural hematoma in a child with external hydrocephalus. Pediatr Neurosurg 39:57–59
Kyllerman M, Steen G (1980) Glutaric aciduria. A “common” metabolic disorder. Arch Fr Pediatr 37:279
Kolker S, Christensen E, Leonard JV, Greenberg CR, Boneh A, Burlina AB, Burlina AP, Dixon M, Duran M, Carcia Cazorla A, Goodman SI, Koeller DM, Kyllerman M, Muhlhausen C, Muller E, Okun JG, Wilcken B, Hoffmann GF, Burgard P (2011) Diagnosis and management of glutaric aciduria type I—revised recommendations. J Inherit Metab Dis 34:677–694
Arita JH, Faria EC, Peruchi MM, Lin J, Rodrigues Masruha M, Vilanova LC (2009) Menkes disease as a differential diagnosis of child abuse. Arq Neuropsiquiatr 67:507–509
Bacopoulou F, Henderson L, Philip SG (2006) Menkes disease mimicking non-accidental injury. Arch Dis Child 91:919
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
No financial support was provided for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Pfeifer, C.M., Hammer, M.R., Mangona, K.L. et al. Non-accidental trauma: the role of radiology. Emerg Radiol 24, 207–213 (2017). https://doi.org/10.1007/s10140-016-1453-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-016-1453-7