Abstract
Objective
Coronary artery involvement in Takayasu arteritis (TAK) leads to poor prognosis and high mortality. Tocilizumab (TCZ) has been used to effectively treat large vessel vasculitis. However, the efficacy of TCZ in resolving coronary artery involvement in TAK is unclear. The aim of this retrospective study was to evaluate the efficacy of TCZ in the treatment of coronary artery involvement in TAK.
Methods
Clinical features and manifestations of coronary artery lesions in 11 TAK patients were evaluated before and after TCZ treatment, and the results were compared with those of 11 patients treated with traditional disease-modifying antirheumatic drugs (DMARDs).
Results
C-reactive protein (p = 0.006), erythrocyte sedimentation rate (ESR) (p = 0.011), and Kerr score (p = 0.007) were significantly decreased post-TCZ treatment for 6 months. The Indian Takayasu Clinical Activity Score (ITAS) 2010 (p = 0.019) and ITAS-A (p = 0.019) were significantly lower in patients treated with TCZ compared with those treated with traditional DMARDs. The glucocorticoid (GC) dose was tapered to 2.50 (0.00, 7.50) mg day−1 after TCZ treatment for 6 months, which was significantly lower than the GC dose after traditional DMARDs treatment [10.0 (5.00, 11.25) mg.day−1, (p = 0.033)]. After 6-month TCZ treatment, the total number of coronary artery lesions was reduced from 23 to 15 in 6 patients. Vascular wall thickening was remarkably improved in 2 lesions (in the ostia of the left main and right coronary arteries).
Conclusion
TCZ may decrease the disease activity and improve coronary artery lesion in patients with TAK.
Key Points • TCZ treatment significantly decreased the disease activity in TAK patients with coronary artery involvement. • TCZ treatment significantly reduces the dosage of GC. • TCZ treatment led to an improvement in imaging findings of TAK patients with coronary artery involvement. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
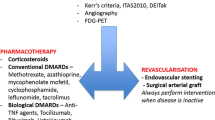
Takayasu arteritis (TAK) is a systemic large vessel vasculitis with an unknown etiology, mainly involving the aorta and its branches. Thickening of the vessel wall, stenosis, and even occlusion of the lumen may lead to tissue and organ ischemia or dysfunction, thereby endangering the lives of TAK patients [1]. Coronary artery involvement is a serious adverse factor associated with a poor prognosis and increased mortality in patients with TAK [2,3,4]. A study of cardiac involvement in Chinese patients with TAK found that the incidence rate of coronary artery involvement was 11.6% [5]. Another study found that the prevalence of coronary artery involvement was 44.4% among TAK patients with chest pain or shortness of breath [6]. Moreover, coronary arterial lesions were detected in 53.2% on computer tomography angiography (CTA) in TAK patients [7]. The revascularization of coronary arteries in patients with TAK, especially those with active TAK, is a challenge. The incidence of major adverse cardiac events (MACE) is significantly increased in patients with TAK who have undergone coronary artery revascularization during the active phase of the disease [8]. For the management of large vessel vasculitis, the European League against Rheumatism (EULAR) recommends that elective procedures only be performed while the disease is in remission [9].
Interleukin (IL)-6 plays an important role in promoting inflammation and fibrosis of the vascular wall in TAK. Serum IL-6 level in TAK patients is positively correlated with disease activity [10]. Moreover, vascular wall inflammation and disease activity in patients with TAK can be effectively improved by inhibiting IL-6 [11]. Therefore, IL-6 was considered as a potential target for the treatment of TAK [12]. The IL-6 receptor antagonist, tocilizumab (TCZ), is a human monoclonal antibody that blocks the effect of IL-6 by blocking the IL-6 receptor. Further, inhibiting the binding of IL-6 to the receptor has been successfully used in the treatment of giant cell arteritis (GCA) [13, 14]. In recent years, some small-sample clinical studies have found that TCZ is safe and effective in the treatment of TAK [15, 16]. Moreover, a two-center, double-blind, placebo-controlled trial demonstrated that administering a single dose of TCZ prior to coronary angiography attenuated the inflammatory response and primarily percutaneous coronary intervention (PCI)-related troponin T release in non-ST elevation myocardial infarction (NSTEMI) patients. Furthermore, no safety issues in the TCZ group were detected during the 6 months of follow-up [17]. Thus, the current study aimed to investigate the efficacy and safety of TCZ, and to compare the results to those of the traditional disease-modifying antirheumatic drug (DMARDs) in the treatment of coronary artery involvement in patients with TAK. Efficacy and safety were determined by evaluating the clinical parameters and imaging changes of the coronary artery.
Methods
Ethics
This retrospective study was conducted in accordance with the ethical principles of the Declaration of Helsinki and approved by the Ethics Committee of Beijing Anzhen Hospital, Capital Medical University (approval number: 2019012X).
Patients
We retrospectively studied the characteristics of 22 TAK patients with coronary artery involvement who were admitted to the Department of Rheumatology and Immunology, Beijing Anzhen Hospital, from October 2014 to October 2018. Inclusion criteria were determined according to the criteria for classification of TAK developed by the American College of Rheumatology in 1990 [18]. Disease activity was assessed using a modified version of Kerr’s criteria [19] and the Indian Takayasu Clinical Activity Score (ITAS2010 and ITAS-A) [20]. Patients with other autoimmune diseases, liver and kidney dysfunction, cancer, or infections were excluded from the study. Demographic and clinical features, as well as laboratory parameters were recorded and disease activity was evaluated before and after treatment. Follow-up coronary artery CTA was performed in 6 patients treated with TCZ after 6 months.
Treatment
All 22 patients selected for inclusion in the study were divided into two groups according to the treatment received. Eleven patients were treated with TCZ (TCZ group), and a second group of 11 patients were treated with traditional DMARDs (traditional DMARDs group). The TCZ group was treated with TCZ 8 mg kg−1 intravenously every 4 weeks. Among these patients, 6 underwent treatment combined with oral administration of methotrexate (MTX) 7.5–15 mg once a week. Another six patients received the prednisone at an initial median dosage of 7.5 mg d−1. In the group of 11 patients treated with traditional DMARDs, 3 patients were treated with cyclophosphamide (CTX), 1.0 g administered intravenously once every 4 weeks. Another 2 patients were administered oral CTX, 0.1 g once every other day. Another 2 patients were treated with mycophenolate mofetil, 1.0 g administered twice daily. Three patients in this group were treated with MTX 15 mg once a week. One patient in this group was treated with a combination of mycophenolate mofetil, 1.0 g administered twice daily, and oral MTX, 15 mg once weekly. Eight patients received GC with an initial median dose of prednisone of 30 mg d−1. All patients provided written informed consent to participate in the study. Therapeutic decisions for individuals were made jointly by the patient and his or her doctor.
Collection of clinical data
Data regarding age, sex, body mass index (BMI), disease duration, clinical manifestation, history of hypertension, type 2 diabetes mellitus (T2DM), hyperlipidemia, and smoking were recorded at baseline. Lesions were classified according to the angiographic classification of the 1994 International TAK Conference in Tokyo [21]. Laboratory data were obtained from laboratory examination reports of the participating hospital.
Imaging evaluation of coronary artery lesions
Coronary artery CTA was used to evaluate the location and nature of coronary artery lesions before and after treatment. Evaluation of the coronary artery was performed by two experienced imaging physicians. Heart rate was measured before examination in all patients, and the scanning mode was selected individually according to the heart rate to reduce the motion artifact of the heartbeat. Respiration training was performed to reduce the respiratory motion artifact. BMI was calculated to select the appropriate kilovoltage.
Statistical analysis
Values are expressed as the mean ± standard error. Differences between measured parameters in the two groups were assessed using an unpaired t test. The Mann–Whitney U test was used for variables that do not normally fall within a distribution and were represented by median values with interquartile ranges. Paired t test was used to analyze the change of parameters before and after treatment. P values < 0.05 indicated statistical significance. All statistical analyses were performed using SPSS 20.0 statistical software (SPSS Inc., Chicago, IL, USA).
Results
Comparison of the general data between the TCZ and traditional DMARDs groups at baseline
There was no difference in terms of sex, age of onset, and disease duration between the TCZ and traditional DMARDs group. The TCZ group had higher frequency of smoking history than that in traditional DMARDs group (36.4% vs 0.0%, p = 0.027).
In the TCZ group, 63.6% had chest pain (7/11) and 54.5% (6/11) had chest tightness, which were not significantly different from those of the traditional DMARDs group. In the traditional DMARD group, 5 patients had palpitation symptoms whereas no such symptoms were observed in the TCZ group (45.5% vs 0.00%, p = 0.011). Two patients in the traditional DMARDs group had back pain, whereas back pain was not found in the TCZ group (18.2% vs 0.00%. p = 0.138). Numano V type was the most common type in both the TCZ group and traditional DMARDs groups (45.5% vs 54.5%, p = 0.670). The imaging features of coronary involvement, treatment details, and history of revascularization were recorded and compared at baseline (Table 1).
Comparison of laboratory parameters and disease activities between the TCZ and the traditional DMARDs groups before and after treatment
Before treatment, serum tumor necrosis factor (TNF)-α levels in TCZ group was significantly higher than that in the traditional DMARDs group 49.60 (18.00, 234.50) pg/ml vs 13.80 (4.45, 24.30) pg/ml, (p = 0.009). There was no difference in IL-6, erythrocyte sedimentation rate (ESR), CRP, Kerr score, ITAS2010, and ITAS-A between the two groups.
CRP [3.18 (1.71, 14.51) mg/l vs 0.72 (0.25, 1.04) mg/l, p = 0.006], ESR [13.00 (5.00, 48.00) mm/1 h vs 2.00 (1.25, 6.50) mm/1 h, p = 0.011], and Kerr score [2.00 (2.00, 3.00) vs 0.00 (0.00, 0.00), p = 0.007] were significantly decreased after TCZ treatment than before the treatment. Serum high-density lipoprotein cholesterol (HDL-C) levels were significantly higher after the TCZ treatment than before the treatment [(1.02 ± 0.21 vs 1.25 ± 0.24) mmol/l, p = 0.041], C3 (1.14 ± 0.23 g/l vs 0.89 ± 0.18 g/l, p = 0.025). Complement 4 (C4) (0.21 ± 0.09 g/l vs 0.13 ± 0.05 g/l, p = 0.046) levels were also significantly lower after the treatment than before. In the traditional DMARDs group, levels of serum IL-6 decreased significantly after the treatment compared with baseline [8.20 (4.20, 101.45) pg/ml vs 2.20 (1.10, 8.25) pg/ml, p = 0.045]. The ITAS-A score decreased significantly [7.00 (4.50, 10.75) vs 4.00 (1.25, 9.00), p = 0.040] and HDL-C increased significantly after the treatment than before the treatment (1.13 ± 0.18 mmol/l vs 1.56 ± 0.24 mmol/l, p = 0.003).
After 6 months of treatment, the peripheral blood lymphocyte count was significantly lower in the traditional DMARDs group than in the TCZ group (2.39 ± 0.79 vs 1.40 ± 0.56)109/L, (p = 0.034). The ITAS2010 and ITAS-A scores of the TCZ treated group were both 1.00 (0.00, 1.00), which were significantly lower than those of the traditional DMARDs group [4.00 (1.25, 9.00), (p = 0.019)]. C4 level significantly decreased in the TCZ group than in the traditional DMARDs group (0.13 ± 0.05 g/l vs 0.23 ± 0.05 g/l, p = 0.016). After TCZ treatment, the GC dose was reduced from 7.5 mg day−1 to 2.50 (0.00, 7.50) mg day−1, which did not differ before and after TCZ treatment (P = 0.298). However, the dose of GC in TCZ group was significantly lower than that of the traditional DMARDs group after 6 months later [10.0 (5.00, 11.25) mg day−1, (p = 0.033)]. The reduction rate of GC was 72.92 ± 8.59% in TCZ group and 58.33 ± 39.67% in traditional DMARDs group with no significant difference between the groups (p = 0.444). The cumulative dose of GC from baseline to follow-up was 1.65 (1.62, 2.67) g in TCZ group, which was significantly lower than traditional DMARDs group [4.34 (2.06, 7.42) g] (p = 0.046) (Table 2).
Imaging features of the coronary artery lesions before and after TCZ treatment
Coronary artery CTA was re-performed in 6 patients after 6 months of TCZ treatment. Table 3 shows the general information, treatment details, and features of coronary lesions at baseline. A total of 23 lesions were found in 6 patients in the TCZ group at baseline with most lesions located in the ostia of the left main coronary artery (LM) (75%, 4/6) and the right coronary artery (RCA) (75%, 4/6). One lesion in one occlusion was found in the LM (16.7%). There were a total of 5 lesions with lumen narrowing of > 50%, of these, 33.3% (2/6) were located in the LM, 1 (16.7%) in the left anterior descending coronary (LAD), 1 (16.7%) in the left circumflex coronary (LCX), and 1(16.7%) in the RCA. After 6 months of TCZ treatment, the number of lesions reduced to 15. Vascular wall thickening significantly improved in 2 lesions (1 in the ostia of the LM and the other in the ostia of the RCA). There were 2 lesions with lumen stenosis of > 50%, which was reduced to < 50% (1 in the LM and 1 was in the LAD). Only one new atherosclerosis-related lesion at the proximal segment of the LAD was found in a 58-year-old female patient with disease duration of 20 years (Table 4).
Safety
Adverse reactions were noted in 3 patients of the TCZ group, including 1 case of slight platelet reduction and 2 cases of elevated transaminase levels. In the traditional DMARDs group, 4 patients had adverse reactions, including 1 case of slight platelet reduction, 2 cases of elevated transaminase levels, and 1 case of upper respiratory tract infection. There were no other serious adverse reactions.
Discussion
According to this study, TCZ treatment could significantly decrease the ESR, CRP, and Kerr scores as well as increase the HDL-C levels in TAK patients with coronary artery involvement. Compared with patients treated with the traditional DMARDs, the total number of peripheral blood lymphocytes was less affected in those treated with TCZ. Moreover, TCZ treatment could significantly reduce the dosage of GC. To our knowledge, this study is the first to show that TCZ treatment led to an improvement in imaging findings of TAK patients with coronary artery involvement.
Arterial reconstruction and bypass grafting may be necessary in approximately 70% of patients with TAK to reverse some features of the disease, and elective procedures should be performed when the disease is in remission [9]. Coronary artery involvement is a special but not rare manifestation of TAK. Although only 5–20% of patients with TAK present ischemic symptoms, coronary artery involvement is demonstrated in approximately 53% of patients with TAK on angiography [7, 22]. Coronary artery involvement is an important cause of mortality in these patients [22, 23]. For patients at the stable stage of TAK, PCI is comparable with coronary bypass graft surgery (CABG) in terms of improving the outcome, and coronary revascularization should be performed during the stable stage of TAK [8]. Therefore, rapid reduction of inflammatory indicators is very important to improve the prognosis associated with TAK.
GC has played a pivotal role in the treatment of systemic inflammatory diseases and remains the first-line treatment for systemic vasculitis. However, GC also incurs a significant risk of undesirable adverse events (AEs) including metabolic abnormalities such as diabetes and hypercholesterolemia, which may lead to life-threatening cerebrovascular and cardiovascular events [24,25,26]. Research has shown that reducing the dose of steroids has resulted in relapses, and prolonged GC therapy is frequently associated with various significant morbidities. In addition, conventional immunosuppressants such as methotrexate, leflunomide, and CTX have modest steroid-sparing effects, leaving an urgent unmet need [25]. A multicenter retrospective study showed that 6 months of TCZ treatment can result in remission in 80% of patients with DMARDs-refractory TAK, indicating that TCZ has a significant steroid-sparing effect and a relatively good safety profile [27]. In the current study, 5 patients in the TCZ group did not use GC. The median initial dose of GC was 7.5 mg, and the dose was reduced to 2.5 mg after 6 months of treatment, which was significantly lower than that in the traditional DMARDs group. However, TCZ treatment can significantly decrease ESR and CRP levels and Kerr score in TAK patients after 6 months, suggesting that TCZ may inhibit inflammation even with a low dose of GC.
A randomized, double-blind, placebo-controlled, phase 3 trial in Japan showed the effect of TCZ during the time interval to relapse on the pathogenesis of TAK is attributable to the inhibition of IL-6 signaling rather than solely the pharmacodynamic effects of TCZ on acute phase reactants. The trial results suggested superior outcomes of TCZ treatment compared with placebo and support further investigation of TCZ for the treatment of patients with refractory TAK [15]. A comparative study of TCZ and CTX suggested the potential effectiveness of TCZ in patients with refractory or severe TAK without serious side effects, but no significant improvement occurred in terms of vascular stenosis, thickness, and enhancement scores in both groups. However, significantly decreased ESR, CRP, and matrix-metalloprotease (MMP)-9 levels as well as increased MMP-2 levels were found in the TCZ group when compared with the CTX group [28]. In the current study, the decrease in ITAS and ITAS-A scores in the TCZ group was more significant than that in the traditional DMARDs group, which suggests the feasibility of treating TAK patients with vascularization.
After TCZ treatment, mural thickness of the common carotid artery and subclavian artery have been shown to reduce along with decreases in ESR and high sensitivity (hs)-CRP levels [16]. Yokokawa et al. described a case of an 18-year-old female with TAK who had severe stenosis in the ostium of both the LM and the LAD. She was treated with combined immunosuppressive treatment with corticosteroid and TCZ, and at 4 months after initiation of treatment, coronary angiography showed regression of the coronary ostial stenosis [29]. The results of our data showed that, after the treatment with TCZ for 6 months, the degree of lumen stenosis in most lesions was improved, and the number of lesions was significantly reduced. As shown in Fig. 1, a 39-year-old female had a history of 108 months with chest tightness and pain. Coronary artery CTA showed severe stenosis (> 75%) in the ostium of the LM (Fig. 1a, b), and after 6 months of TCZ treatment without GC, her coronary artery stenosis improved significantly (Fig. 1c, d).
Imaging of computer tomography angiography (CTA) of coronary artery in a TAK patient before and after TCZ treatment. A 39-year-old female patient with disease duration of 108 months, she has chest tightness and pain. Coronary artery CTA shows severe stenosis in the ostium of the left main coronary artery (LM) (a, b). After 6 month of TCZ treatment, her coronary artery stenosis improved significantly (c, d)
This study found that C3 level decreased significantly after TCZ treatment, which was consistent with previous studies. In patients with rheumatoid arthritis (RA) treated with TCZ for 12 months, 68.75% and 56.25% of patients had decreased C3 and C4 serum levels, respectively. Low C3 and C4 serum levels appeared to be the result of the anti-inflammatory effects mediated by TCZ [30]. Previous studies have shown that TAK has a proatherogenic lipid profile, and this profile is characterized by low HDL-C levels [31]. In one study, patients with active TAK had significantly lower levels of HDL-C than patients with inactive TAK [32]. TCZ treatment can significantly increase levels of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), HDL-C, and triglyceride (TG), yet does not change the lipid-related cardiovascular risk in RA patients [32]. The present study found that both TCZ and traditional DMARDs can increase serum HDL-C levels without elevating LDL-C, TC and TG levels, which may be related to the decreased TAK inflammation. A previous study found that HDL-C increased after one year of TCZ treatment compared to that at baseline in RA patients, and the magnitude of reduction in hs-CRP level was associated with increments of HDL-C efflux capacity of macrophages after TCZ treatment [33]. Moreover, compared with anti-TNF-α therapy, the application of TCZ not only can effectively control the activity of RA disease, but also can improve the endothelial function of the high-risk population [34]. A two-center, randomized, double-blind, placebo-controlled study confirmed that a single injection of TCZ (280 mg) in patients with non-ST elevation myocardial infarction helped to inhibit the inflammatory response and reduce PCI-associated troponin T release, and showed the safety of TCZ [17]. These results may indicate that TCZ administration can be a new perioperative treatment strategy for TAK patients with coronary artery involvement as it has cardiovascular benefits.
The main limitations of this study were the retrospective design and its relatively small sample size. High dose GC therapy (40–60 mg/day prednisone-equivalent) is recommended as initial treatment for the induction of remission in active GCA or TAK [35]. However, in this retrospective study, the initial dose of GC used was relatively low. Prospective studies with larger samples are necessary to further determine the effectiveness and safety of TCZ in the treatment of coronary artery involvement in TAK.
In conclusion, TCZ can decrease TAK activity as a whole, reduce the dosage of GC, and improve lumen stenosis caused by coronary artery wall inflammation. Thus, TCZ may also be used as a drug treatment for TAK patients with coronary artery involvement, and may be considered as a perioperative treatment strategy for vascularization treatment.
References
Vaideeswar P, Deshpande JR (2013) Pathology of Takayasu arteritis: a brief review. Ann Pediatr Cardiol 6(1):52–58
Park MC, Lee SW, Park YB, Chung NS, Lee SK (2005) Clinical characteristics and outcomes of Takayasu’s arteritis: analysis of 108 patients using standardized criteria for diagnosis, activity assessment, and angiographic classification. Scand J Rheumatol 34(4):284–292
Hlavaty L, Diaz F, Sung L (2015) Takayasu arteritis of the coronary arteries presenting as sudden death in a white teenager. Am J Forensic Med Pathol 36(3):221–223
Spagnolo EV, Cannavo G, Mondello C, Cardia L, Bartoloni G, Cardia G (2015) Unexpected death for Takayasu aortitis associated with coronary ostial stenosis: case report. Am J Forensic Med Pathol 36(2):88–90
Li J, Li H, Sun F, Chen Z, Yang Y, Zhao J, Li M, Tian X, Zeng X (2017) Clinical characteristics of heart involvement in Chinese patients with Takayasu arteritis. J Rheumatol 44:1867–1874
Soto ME, Melendez-Ramirez G, Kimura-Hayama E, Meave-Gonzalez A, Achenbach S, Herrera MC, Guering EL, Alexanderson-Rosas E, Reyes PA (2011) Coronary CT angiography in Takayasu arteritis. JACC Cardiovasc Imaging 4(9):958–966
Kang EJ, Kim SM, Choe YH, Lee GY, Lee KN, Kim DK (2014) Takayasu arteritis: assessment of coronary arterial abnormalities with 128-section dual-source CT angiography of the coronary arteries and aorta. Radiology 270(1):74–81
Wang X, Dang A, Lv N, Cheng N, Cheng X, Yang Y, Song Y (2017) Long-term outcomes of coronary artery bypass grafting versus percutaneous coronary intervention for Takayasu arteritis patients with coronary artery involvement. Semin Arthritis Rheum 47(2):247–252
Mukhtyar C, Guillevin L, Cid MC, Dasgupta B, de Groot K, Gross W, Hauser T, Hellmich B, Jayne D, Kallenberg CG, Merkel PA, Raspe H, Salvarani C, Scott DG, Stegeman C, Watts R, Westman K, Witter J, Yazici H, Luqmani R, European Vasculitis Study Group (2009) EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis 68(3):318–323
Park MC, Lee SW, Park YB, Lee SK (2006) Serum cytokine profiles and their correlations with disease activity in Takayasu’s arteritis. Rheumatology (Oxford) 45(5):545–548
Kong X, Sun Y, Ma L, Chen H, Wei L, Wu W, Ji Z, Zhang Z, Zhao Z, Hou J et al (2016) The critical role of IL-6 in the pathogenesis of Takayasu arteritis. Clin Exp Rheumatol 34(3 Suppl 97):S21–S27
Kong X, Ma L, Ji Z, Dong Z, Zhang Z, Hou J, Zhang S, Jiang L (2017) Pro-fibrotic effect of IL-6 via aortic adventitial fibroblasts indicates IL-6 as a treatment target in Takayasu arteritis. Clin Exp Rheumatol 36(1):62–72
Stone JH, Klearman M, Collinson N (2017) Trial of Tocilizumab in giant-cell arteritis. N Engl J Med 377(15):1494–1495
Villiger PM, Adler S, Kuchen S, Wermelinger F, Dan D, Fiege V, Butikofer L, Seitz M, Reichenbach S (2016) Tocilizumab for induction and maintenance of remission in giant cell arteritis: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet 387(10031):1921–1927
Nakaoka Y, Isobe M, Takei S, Tanaka Y, Ishii T, Yokota S, Nomura A, Yoshida S, Nishimoto N (2018) Efficacy and safety of tocilizumab in patients with refractory Takayasu arteritis: results from a randomised, double-blind, placebo-controlled, phase 3 trial in Japan (the TAKT study). Ann Rheum Dis 77(3):348–354
Zhou J, Chen Z, Li J, Yang Y, Zhao J, Chen H, Liu M, Sun F, Li M, Tian X et al (2017) The efficacy of tocilizumab for the treatment of Chinese Takayasu’s arteritis. Clin Exp Rheumatol 35 Suppl 103(1):171–175
Kleveland O, Kunszt G, Bratlie M, Ueland T, Broch K, Holte E, Michelsen AE, Bendz B, Amundsen BH, Espevik T, Aakhus S, Damås JK, Aukrust P, Wiseth R, Gullestad L (2016) Effect of a single dose of the interleukin-6 receptor antagonist tocilizumab on inflammation and troponin T release in patients with non-ST-elevation myocardial infarction: a double-blind, randomized, placebo-controlled phase 2 trial. Eur Heart J 37(30):2406–2413
Arend WP, Michel BA, Bloch DA, Hunder GG, Calabrese LH, Edworthy SM, Fauci AS, Leavitt RY, Lie JT, Lightfoot RW Jr et al (1990) The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum 33(8):1129–1134
Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M, Hoffman GS (1994) Takayasu arteritis. Ann Intern Med 120(11):919–929
Misra R, Danda D, Rajappa SM, Ghosh A, Gupta R, Mahendranath KM, Jeyaseelan L, Lawrence A, Bacon PA (2013) Development and initial validation of the Indian Takayasu clinical activity score (ITAS2010). Rheumatology (Oxford) 52(10):1795–1801
Hata A, Noda M, Moriwaki R, Numano F (1996) Angiographic findings of Takayasu arteritis: new classification. Int J Cardiol 54(Suppl):S155–S163
Miloslavsky E, Unizony S (2014) The heart in vasculitis. Rheum Dis Clin N Am 40(1):11–26
Rav-Acha M, Plot L, Peled N, Amital H (2007) Coronary involvement in Takayasu’s arteritis. Autoimmun Rev 6(8):566–571
van der Goes MC, Jacobs JW, Bijlsma JW (2014) The value of glucocorticoid co-therapy in different rheumatic diseases--positive and adverse effects. Arthritis Res Ther 16(Suppl 2):S2
Kondo T, Amano K (2018) Era of steroid sparing in the management of immune-mediated inflammatory diseases. Immunol Med 41(1):6–11
Banerjee S, Bagheri M, Sandfort V, Ahlman MA, Malayeri AA, Bluemke DA, Yao J, Grayson PC (2018) Vascular calcification in patients with large-vessel vasculitis compared to patients with hyperlipidemia. Semin Arthritis Rheum 48(6):1068–1073
Mekinian A, Resche-Rigon M, Comarmond C, Soriano A, Constans J, Alric L, Jego P, Busato F, Cabon M, Dhote R et al (2018) Efficacy of tocilizumab in Takayasu arteritis: multicenter retrospective study of 46 patients. J Autoimmun 91:55–60
Kong X, Zhang X, Lv P, Cui X, Ma L, Chen H, Liu H, Lin J, Jiang L (2018) Treatment of Takayasu arteritis with the IL-6R antibody tocilizumab vs. cyclophosphamide. Int J Cardiol 266:222–228
Yokokawa T, Kunii H, Kaneshiro T, Ichimura S, Yoshihisa A, Yashiro Furuya M, Asano T, Nakazato K, Ishida T, Migita K, Takeishi Y (2019) Regressed coronary ostial stenosis in a young female with Takayasu arteritis: a case report. BMC Cardiovasc Disord 19(1):79
Romano C, Del Mastro A, Sellitto A, Solaro E, Esposito S, Cuomo G (2018) Tocilizumab reduces complement C3 and C4 serum levels in rheumatoid arthritis patients. Clin Rheumatol 37(6):1695–1700
de Carvalho JF, Bonfa E, Bezerra MC, Pereira RM (2009) High frequency of lipoprotein risk levels for cardiovascular disease in Takayasu arteritis. Clin Rheumatol 28(7):801–805
Wang X, Chen B, Lv N, Liu Q, Dang A (2015) Association of abnormal lipid spectrum with the disease activity of Takayasu arteritis. Clin Rheumatol 34(7):1243–1248
Ferraz-Amaro I, Hernandez-Hernandez MV, Tejera-Segura B, Delgado-Frias E, Macia-Diaz M, Machado JD, Diaz-Gonzalez F (2019) Effect of IL-6 receptor blockade on proprotein convertase subtilisin/Kexin Type-9 and cholesterol efflux capacity in rheumatoid arthritis patients. Horm Metab Res 51(3):200–209
Bacchiega BC, Bacchiega AB, Usnayo MJ, Bedirian R, Singh G, Pinheiro GD (2017) Interleukin 6 inhibition and coronary artery disease in a high-risk population: a prospective community-based clinical study. J Am Heart Assoc 6(3). https://doi.org/10.1161/JAHA.116.005038
Hellmich B, Agueda A, Monti S, Buttgereit F, de Boysson H, Brouwer E, Cassie R, Cid MC, Dasgupta B, Dejaco C et al (2019) 2018 Update of the EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis 79(1):19–30
Funding
This project was supported by grant from the National Natural Science Foundation of China (91739111). The sponsors did not have a role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
LP conceived of the study and drafted the manuscript. JD, HL, JL, HH, and LY help to collected clinical data, XL help revised the manuscript, JL and XG evaluated the features of coronary CTA, Prof. Yujie Zhou guided the design of this study and modified the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosures
None.
Ethics approval and consent to participate
All subjects provided written informed consent. The study was conducted in accordance with the ethical principles of the Declaration of Helsinki and approved by the Clinical Research Ethics Board of Beijing Anzhen Hospital, Capital Medical University (approval number: 2019012X).
Consent for publication
The authors declare that there are no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pan, L., Du, J., Liu, J. et al. Tocilizumab treatment effectively improves coronary artery involvement in patients with Takayasu arteritis. Clin Rheumatol 39, 2369–2378 (2020). https://doi.org/10.1007/s10067-020-05005-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05005-7