Abstract
Objective
This cross-sectional study was designed to assess the clinical significance of the serum KL-6 in the diagnosis of interstitial lung disease (ILD) in patients with idiopathic inflammatory myopathy (IIM).
Methods
We measured serum KL-6 levels in 184 patients with IIM using a chemiluminescent enzyme immunoassay and compared KL-6 levels between patients with and without ILD, according to other clinical features.
Results
IIM patients with ILD had significantly higher serum KL-6 levels than those without ILD (776.5 [372.3–1378.8] vs. 297.5 [204.75–599.3] U/ml, P < 0.001). At a cut-off of 461.5 U/ml identified by ROC curve, serum KL-6 yielded a sensitivity of 70.2% and specificity of 73.9% for ILD in IIM patients. IIM patients with an elevated serum KL-6 were more likely to have clinical symptoms of mechanic’s hands (P = 0.002), anti-Jo-1 antibody positivity (P = 0.021), dysphagia (P = 0.039), hoarseness (P < 0.001), and polyarthritis/polyarthralgia (P < 0.001). Significant inverse correlations were found between serum KL-6 levels and pulmonary function tests (P < 0.01), including forced vital capacity (FVC, %Pred), total lung capacity (TLC, %Pred), and diffusing capacity for carbon monoxide (DLCO, %Pred).
Conclusions
Serum KL-6 offers high sensitivity and specificity for the diagnosis of IIM-associated ILD and is inversely correlated with pulmonary function deterioration. Serum KL-6 may represent a promising biomarker for monitoring ILD severity in IIM patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic inflammatory myopathies (IIMs), including polymyositis (PM) and dermatomyositis (DM), are considered systemic autoimmune diseases characterized by chronic progressive muscle weakness and inflammation of the striated muscles with unknown etiology and resulting in significant morbidity and mortality [1]. In addition, extramuscular complications, such as skin manifestations, interstitial lung disease (ILD), and cardiomyopathy, are very common and can be life-threatening [2].
ILD, which is characterized by diffuse pulmonary infiltrates and restrictive lung function impairment with decreased diffusing capacity of carbon monoxide (DLCO), is one of the most common complications, although the reported frequencies have varied widely, ranging from 20 to 78% in patients with IIM [3]. ILD negatively affects the survival of IIM patients and is consistently identified as one of the most important predictive factors for mortality in IIM patients. Early and accurate diagnosis of ILD in patients with IIM in clinical practice is critical to improve outcomes by preventing progression from initial inflammatory activity to end-stage disease with irreversible honeycombing and fibrosis [4]. At present, for early and accurate diagnosis of ILD in patients with IIM, high-resolution computed tomography of the chest (HRCT) scanning and invasive lung biopsy are used to screen and confirm the diagnosis.
In 1989, the serum level of Krebs von den Lungen-6 (KL-6) antigen was reported by Kohno et al. to be a useful indicator of disease activity in patients with ILD [5]. Several previous studies have shown that KL-6 is a marker of SSc-associated ILD, correlates with disease activity [6,7,8,9], and may provide valuable information in identifying patients with ILD who are at increased risk for subsequent mortality [9]. However, less research has been conducted in patients with IIM-associated ILD [10]. In the present study, we applied a chemiluminescent enzyme immunoassay (CLEIA) to detect KL-6 levels in serum samples of patients with IIM to explore whether the serum KL-6 concentration can serve as a specific marker complement to HRCT in identifying patients with ILD at the time of IIM diagnosis in Chinese patients.
Methods
Ethical approval
This study was approved by the Medical Ethics Committee of Peking Union Medical College Hospital (S-478). The methods were carried out in accordance with the principles stated in the Declaration of Helsinki, and informed consent was obtained from each patient.
Patients and samples
A total of 184 PM/DM patients (47.9 ± 13.8 years, 47 males, 137 females) enrolled in this study were from the Peking Union Medical College Hospital inflammatory myopathies (PUMCH-IM) registry database and were recruited from March 2012 to September 2016. Patients from outpatient clinic and inpatient ward, who were diagnosed with PM/DM and fulfilled the definite or probable diagnostic criteria of Bohan and Peter, were consecutively enrolled in the PUMCH-IM registry [11, 12]. Patients with other connective tissue diseases, malignancies, infectious diseases, or drug-induced myopathy as well as those aged younger than 14 years were excluded. Four-milliliter blood samples were collected when patients were registered using a BD vacutainer without anticoagulants and clotted at room temperature for up to 1 h, before being centrifuged at 4 °C for 5 min at 3000 rpm. The serum was then allocated and stored at − 80 °C. No sample was subjected to more than one freeze-thaw cycle before analysis.
Measurements of serum KL-6
Serum levels of KL-6 in patients with IIM were measured using a chemiluminescent enzyme immunoassay according to the manufacturer’s instructions (Fujirebio Inc., Japan).
Diagnosis of ILD
Pulmonary function tests (PFTs) based on lung volume, spirometry, and diffusing capacity were examined by the respiratory lab at PUMCH. Data collected from PFTs included forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), total lung capacity (TLC), and diffusing capacity for carbon monoxide (DLCO). The results were reported as percentages of predicted values for each patient’s age, gender, and height. Evidence of restriction (reduced FVC accompanied by abnormal or increased FEV1/FVC ratio) and impaired gas exchange (increased alveolar-arterial oxygen pressure gradient [PA-aO2], decreased arterial partial pressure of oxygen [PaO2], or decreased DLCO) were required for the diagnosis of ILD.
HRCT scans were reviewed by two independent radiologists (Drs. Hui Huang and Zuojun Xu) without the knowledge of patients’ clinical information. HRCT examinations were carried out using 2-mm-thick collimation at 1-cm intervals throughout both entire lungs during inspiration in the supine position. Ground-glass and bibasilar opacity represented alveolar involvement, while honeycombing represented the interstitial findings. Each radiologist provided a diagnosis based on HRCT characteristics. In cases of conflict regarding the HRCT diagnosis, the HRCTs were reread by both radiologists and a consensus on the diagnosis was reached if possible.
Statistical analysis
The normality of continuous variables was tested by distribution plots, and the data are expressed as mean ± standard deviation or as median plus inter quartile range (25th–75th percentiles) according to their normal or non-normal distribution. Dichotomous data are presented as frequencies and percentages. Differences in the serum KL-6 concentration between IIM patients with or without ILD were analyzed using the t test, and the performance of KL-6 in the diagnosis of IIM patients with ILD was assessed by receiver operating characteristic curve analysis. The associations between KL-6 and ILD as well as other clinical features of IIM were investigated using χ2 or Fisher’s exact test. The correlations between serum levels of KL-6 and PFT parameters were assessed using Spearman’s rank correlation coefficient. All statistical analyses were performed using the SPSS statistical software package for Windows (version 16.0; SPSS Inc., Chicago, IL, USA), and two-tailed P values < 0.05 were considered significant.
Results
Demographic data of IIM patients
The 184 IIM patients included in this study were divided into two groups according to a cut-off value for serum KL-6 of 500 U/ml, which was given as a cut-off value for high and low KL-6 levels by the manufacturer of the immunoassay used in this study. The mean age of patients in the group with serum KL-6 ≥ 500 U/ml was significantly higher than that of patients in the group with serum KL-6 < 500 U/ml (50.3 ± 12.2 vs. 45.8 ± 14.8 years, P = 0.025). Compared with patients with serum KL-6 < 500 U/ml, those with serum KL-6 ≥ 500 U/ml were more likely to have clinical symptoms of mechanic’s hands (40.5% vs. 20.0%, P = 0.002), positivity for anti-Jo-1 antibodies (16.67% vs. 6.00%, P = 0.021), dysphagia (47.9% vs. 35.0%, P = 0.0391), hoarseness (26.0% vs. 3.0%, P < 0.001), and polyarthritis/polyarthralgia (40.5% vs. 16.0%, P < 0.001). The characteristics of the IIM patients stratified according to the serum KL-6 cut-off value of 500 U/ml are presented in Table 1.
Performance of KL-6 in the diagnosis of ILD in patients with IIM
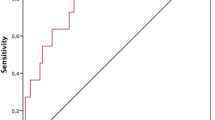
IIM patients with ILD had a significantly higher median serum KL-6 level than those without ILD (776.5 [372.3–1378.8] vs. 297.5 [204.75–599.3] U/ml, P < 0.001; Fig. 1). In order to assess the diagnostic value of serum KL-6 for ILD in IIM patients, the receiver operating characteristic curve analysis was performed and yielded a cut-off level of 461.5 U/ml. At this cut-off value, the serum KL-6 level had a sensitivity of 70.2% and specificity of 73.9% for the diagnosis of ILD in IIM patients (area under the curve [AUC] = 0.76, P = 0.000). The ROC curve is shown in Fig. 2.
Associations between serum levels of KL-6 and pulmonary function parameters in patients with IIM
A significant inverse correlation was found between serum levels of KL-6 and all included pulmonary function parameters: predicted TLC (%Pred) (r = − 0.440, P = 0.001), DLCO (%Pred) (r = − 0.492, P = 0.000), predicted FEV1 (%Pred) (r = − 0.372, P = 0.000), and FVC (%Pred) (r = − 0.396, P = 0.000) (Fig. 3).
In order to evaluate the relationship between KL-6 and lung function further, patients were divided into three groups according to diminished lung function: mildly decreased function (DLCO [%Pred] or FVC [%Pred] ≥ 80%), moderately decreased function (DLCO [%Pred] or FVC [%Pred] 50–80%), and severely decreased function (DLCO [%Pred] or FVC [%Pred] ≤ 50%). We found that the concentration of KL-6 was significantly lower in the group with moderately decreased function (846.6 ± 961.9 U/ml) than in the group with severely decreased function (1403.2 ± 1106.8 U/ml; P = 0.028), but this difference was not found between the groups with mildly and moderately decreased function, as shown in Fig. 4a. The frequency of patients with serum KL-6 ≥ 500 U/ml in the group with severely decreased function was significantly higher than that in the group with moderately decreased function. At the same time, the frequency of patients with serum KL-6 ≥ 500 U/ml in the group with moderately decreased function was also significantly higher than that in the group with mildly decreased function (P = 0.036), as shown in Fig. 4b.
The serum KL-6 levels with different degrees of change in lung function in patients with PM/DM. a Serum KL-6 levels with different degrees of change in DLCO (%Pred). b The frequency of patients with serum KL-6 ≥ 500 U/ml in the groups with differing degrees of change in DLCO (%Pred). c Serum KL-6 levels with different degrees of change in FVC (%Pred). d The frequency of patients with serum KL-6 ≥ 500 U/ml in the groups with differing degrees of change in FVC (%Pred)
With regard to FVC (%Pred), the concentration of KL-6 was significantly lower in the patients with FVC (%Pred) ≥ 80% (614.0 ± 646.0 U/ml) than that in those with FVC (%Pred) 50–80% (1176.1 ± 1173.4 U/ml; P = 0.005), but this difference was not found between patients with FVC (%Pred) 50–80% and patients with FVC (%Pred) ≤ 50% (777.4 ± 377.0 U/ml; P = 0.460), as shown in Fig. 4c. The frequency of patients with serum KL-6 ≥ 500 U/ml in the group with FVC (%Pred) 50–80% was significantly higher than that in the group with FVC (%Pred) ≥ 80% (P = 0.005), but this difference was not found between patients with FVC (%Pred) 50–80% and patients with FVC (%Pred) ≤ 50% (P = 0.992), as shown in Fig. 4d.
Discussion
Polymyositis and dermatomyositis are connective tissue diseases with characteristic of myositis and extramuscular complications, such as skin manifestations, ILD, and cardiomyopathy [1]. A number of risk factors have been identified to be associated with the presence of ILD in patients with IIM, which could benefit the early diagnosis of IIM patients and improve outcomes [13]. KL-6 is a mucin-like high molecular weight glycoprotein strongly expressed on type II alveolar pneumocytes and bronchiolar epithelial cells; it was discovered by Kohno et al. in 1985 and reported to be a serum marker of ILD in several studies [5, 14]. From then on, KL-6 was also reported as a marker of ILD in patients with scleroderma and rheumatoid arthritis, which can facilitate the diagnosis of ILD and play a role in predicting ILD progression and mortality [15,16,17].
In the present study, we applied a chemiluminescent enzyme immunoassay to detect serum KL-6 levels in a large cohort of patients with IIM. First, we found IIM patients with ILD had significantly higher serum KL-6 levels than those without ILD. Furthermore, we confirmed that the serum level of KL-6 reflected the severity of ILD in terms of pulmonary function deterioration. The KL-6 levels were significantly inversely correlated with the results of the included pulmonary function tests: TLC (%Pred), DLCO (%Pred), FEV1 (%Pred), and FVC (%Pred). Second, we identified the relationship that IIM patients with serum KL-6 ≥ 500 U/ml were more likely to have clinical symptoms of mechanic’s hands, positivity for anti-Jo-1 antibodies, dysphagia, hoarseness, and polyarthritis/polyarthralgia, which were consistent with the features of antisynthetase syndrome [1]. Among the clinical manifestations, ILD is the most frequent complication and present in 70–89% of antisynthetase syndrome patients. As ILD is often difficult to treat and can have a fatal clinical course, it has drawn much attention in the last few decades [18]. The ARS-Ab, including anti-Jo-1 antibodies, were reported to be associated with ILD, but those antibodies were present only in 7–20% of patients with IIM [19]. Moreover, the association between the concentrations of those antibodies and pulmonary function were not clear. In the present study, we have confirmed that 45.7% of Chinese IIM patients had a serum KL-6 level ≥ 500 U/ml, and the serum concentration of KL-6 was significantly higher in the PM/DM patients with ILD than in those without. At the cut-off value of 461.5 U/ml calculated by the receiver operating characteristic curve analysis, the serum KL-6 level had a sensitivity of 70.2% and a specificity of 73.9% for the diagnosis of ILD in PM/DM patients. Consistent with the results of Oguz et al. [20], the serum KL-6 level is a sensitive and specific diagnostic factor for ILD and may be used for the detection of ILD in patients with IIM. In patients with IIM, the lung is probably the most frequently involved extramuscular organ, and the presence of ILD in patients with IIM is associated with high morbidity and mortality [18]. As ILD encompasses a variety of lung parenchymal involvements, it may be overlooked and could be an underestimated problem in IIM, thereby with delayed treatment. The diagnosis of ILD has been based on the results of high-resolution CT or the invasive transbronchial lung biopsy, which could be influenced by numerous factors or bring great suffering for patients. Although it is known that the pulmonary function test is noninvasive, it is highly dependent on the cooperation of patients; instead of frequently repeated pulmonary function tests, radiographic examination, and invasive transbronchial lung biopsies, detection of serum KL-6 throughout the course of a patient’s disease is easier to perform. In our cohort, we observed an inverse correlation between changes in serum levels of KL-6 and pulmonary function test results. It is interesting that when the patients were divided into three subgroups according to the degree of change in lung function, DLCO (%Pred) (≥ 80%, 50–80%, and ≤ 50%) or FVC (%Pred) (≥ 80%, 50–80%, and ≤ 50%), the correlations between serum KL-6 levels and pulmonary function test results differed for different degrees of lung function decline. For the DLCO (%Pred), with a greater change in DLCO (%Pred), the change in the serum level of KL-6 was also greater. For the FVC (%Pred), the change in the serum KL-6 level was more sensitive for reflecting the change in FVC (%Pred) at the beginning, but the change in KL-6 did not reflect the changes in FVC (%Pred) when FVC (% Pred) was severely changed.
There are several limitations in our study. It has been reported in patients with systemic sclerosis-associated ILD that cyclophosphamide might affect the KL-6 serum level in spite of the spirometry parameters (FVC and DLCO) [9]. Given the remarkable disparity of treatment regimens when patients were registered, the effect of pharmacological treatments on serum level of KL-6 was not taken into account in our IIM patients. Furthermore, the relationship between serum KL-6 level and disease activity of myositis were not investigated in this study, because the disease activity of muscle, skin, and lung lesions in myositis patients are not always concordant, and the score system developed by International Myositis Outcome Assessment Collaborative Study (IMACS) is quite complicated and not available when these patients were registered. Instead, we compared the frequency of a number of typical myositis-related clinical features between groups with different KL-6 levels (Table 1). Obviously, detection of serum KL-6 serially may be useful in the follow-up of IIM patients with ILD and could possibly be a complement to repeat pulmonary function tests and chest radiography/HRCT for evaluating the response to therapy.
In conclusion, this is a comprehensive report on the significance of the serum KL-6 level in Chinese patients with IIM. IIM patients with ILD had significantly higher serum KL-6 concentrations than those without ILD. Also, there was a significant inverse correlation between serum KL-6 levels and the results of pulmonary function tests. From a clinical point of view, these data support the usefulness of serum KL-6 as an additional serological marker for the diagnosis of ILD in IIIM patients and as a predictive marker for some IIM-related manifestations. However, additional longitudinal studies are needed to validate the diagnostic and/or prognostic role of serum KL-6 in a larger cohort of patients with IIM.
References
Rider LG, Miller FW (2011) Deciphering the clinical presentations, pathogenesis, and treatment of the idiopathic inflammatory myopathies. JAMA 305:183–190
Dalakas MC, Hohlfeld R (2003) Polymyositis and dermatomyositis. Lancet 362:971–982
Hallowell RW, Ascherman DP, Danoff SK (2014) Pulmonary manifestations of polymyositis/dermatomyositis. Semin Respir Crit Care Med 35:239–248
Labirua A, Lundberg IE (2010) Interstitial lung disease and idiopathic inflammatory myopathies: progress and pitfalls. Curr Opin Rheumatol 22:633–638
Kohno N, Kyoizumi S, Awaya Y, Fukuhara H, Yamakido M, Akiyama M (1989) New serum indicator of interstitial pneumonitis activity. Sialylated carbohydrate antigen KL-6. Chest 96:68–73
Bonella F, Volpe A, Caramaschi P et al (2011) Surfactant protein D and KL-6 serum levels in systemic sclerosis: correlation with lung and systemic involvement. Sarcoidosis Vasc Diffuse Lung Dis 28:27–33
Yanaba K, Hasegawa M, Takehara K, Sato S (2004) Comparative study of serum surfactant protein-D and KL-6 concentrations in patients with systemic sclerosis as markers for monitoring the activity of pulmonary fibrosis. J Rheumatol 31:1112–1120
Vesely R, Vargova V, Ravelli A et al (2004) Serum level of KL-6 as a marker of interstitial lung disease in patients with juvenile systemic sclerosis. J Rheumatol 31:795–800
Kumanovics G, Gorbe E, Minier T, Simon D, Berki T, Czirjak L (2014) Follow-up of serum KL-6 lung fibrosis biomarker levels in 173 patients with systemic sclerosis. Clin Exp Rheumatol 32:S–138-144
Bandoh S, Fujita J, Ohtsuki Y, Ueda Y, Hojo S, Tokuda M, Dobashi H, Kurata N, Yoshinouchi T, Kohno N, Takahara J (2000) Sequential changes of KL-6 in sera of patients with interstitial pneumonia associated with polymyositis/dermatomyositis. Ann Rheum Dis 59:257–262
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (first of two parts). N Engl J Med 292:344–347
Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (second of two parts). N Engl J Med 292:403–407
Zhang L, Wu G, Gao D, Liu G, Pan L, Ni L, Li Z, Wang Q (2016) Factors associated with interstitial lung disease in patients with polymyositis and dermatomyositis: a systematic review and meta-analysis. PLoS One 11:e0155381
Fathi M, Barbasso Helmers S, Lundberg IE (2012) KL-6: a serological biomarker for interstitial lung disease in patients with polymyositis and dermatomyositis. J Intern Med 271:589–597
Wang Y, Chen S, Lin Z, du G, Lin J, Lin Q, Xiufeng H, Zhang G, Furst DE, Gargani L, Matucci-Cerinic M (2018) Imaging and serum biomarkers in connective tissue disease-associated interstitial lung diseases: correlation between lung ultrasound B-lines and KL-6 levels. Ann Rheum Dis:annrheumdis-2018-214098
Salazar GA, Kuwana M, Wu M, Estrada-Y-Martin RM, Ying J, Charles J, Mayes MD, Assassi S (2018) KL-6 but not CCL-18 is a predictor of early progression in systemic sclerosis-related interstitial lung disease. J Rheumatol 45:1153–1158
Benyamine A, Heim X, Resseguier N, Bertin D, Gomez C, Ebbo M, Harlé JR, Kaplanski G, Rossi P, Bardin N, Granel B (2018) Elevated serum Krebs von den Lungen-6 in systemic sclerosis: a marker of lung fibrosis and severity of the disease. Rheumatol Int 38:813–819
Hallowell RW, Danoff SK (2014) Interstitial lung disease associated with the idiopathic inflammatory myopathies and the antisynthetase syndrome: recent advances. Curr Opin Rheumatol 26:684–689
Marie I, Josse S, Decaux O, Dominique S, Diot E, Landron C, Roblot P, Jouneau S, Hatron PY, Tiev KP, Vittecoq O, Noel D, Mouthon L, Menard JF, Jouen F (2012) Comparison of long-term outcome between anti-Jo1- and anti-PL7/PL12 positive patients with antisynthetase syndrome. Autoimmun Rev 11:739–745
Oguz EO, Kucuksahin O, Turgay M, Yildizgoren MT, Ates A, Demir N, Kumbasar OO, Kinikli G, Duzgun N (2016) Association of serum KL-6 levels with interstitial lung disease in patients with connective tissue disease: a cross-sectional study. Clin Rheumatol 35:663–666
Funding
This study was supported by the National Natural Science Foundation of China (81771780, 81471615, 81102268, 81302610), the Outstanding Youth Fund of Peking Union Medical College Hospital (JQ201504), the CAMS Initiative for Innovative Medicine (2017-I2M-3-001), and the 2016 PUMCH Science Fund for Junior faculty (pumch-2016-1.5).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
This study was approved by the Medical Ethics Committee of Peking Union Medical College Hospital (S-478). The methods were carried out in accordance with the principles stated in the Declaration of Helsinki, and informed consent was obtained from each patient.
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hu, C., Wu, C., Yang, E. et al. Serum KL-6 is associated with the severity of interstitial lung disease in Chinese patients with polymyositis and dermatomyositis. Clin Rheumatol 38, 2181–2187 (2019). https://doi.org/10.1007/s10067-019-04501-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-019-04501-9