Abstract
It was aimed to evaluate KL-6 glycoprotein levels to determine if it may be a diagnostic marker for the connective tissue diseases (CTDs) predicting CTD-related interstitial lung diseases (ILDs) (CTD-ILD) development and to examine if there was a difference between patients and healthy controls. The study included 113 patients with CTD (45 CTD without lung involvement, 68 CTD-ILD) and 45 healthy control subjects. KL-6 glycoprotein levels were analyzed with ELISA in patients and the control group. The relationship between KL-6 glycoprotein levels and CTD-ILD was assessed. In the comparison of all the groups in the study, significantly higher levels of KL-6 were determined in the CTD-ILD group than in either the CTD without pulmonary involvement group or the healthy control group (p < 0.008 and p < 0.001, respectively). There was no statistically significant difference between the KL-6 levels in the healthy control group and the CTD without pulmonary involvement group (p = 0.289). The KL-6 levels did not differ significantly according to the connective tissue diseases in the diagnostic groups (systemic lupus erythematosus, Sjögren’s syndrome, rheumatoid arthritis, mixed connective tissue disease, scleroderma, polymyositis/ dermatomyositis). In the healthy control group, there was a statistically significant difference between KL-6 levels in smokers and non-smokers. Smokers had significantly higher serum KL-6 levels compared with non-smokers (p < 0.05). There was no statistically significant difference between smoking status (pack-year) and serum KL-6 levels. There was no statistically significant correlation between serum KL-6 levels and time since diagnosis of CTD and CTD-ILD. The level of KL-6 as a predictive factor could be used to identify the clinical development of ILD before it is detected on imaging modality. Further prospective clinical studies are needed to define whether levels of KL-6 might have prognostic value or might predict progressive ILD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), systemic sclerosis (SSc), Sjögren’s syndrome (SjS), polymyositis (PM)/dermatomyositis (DM), and mixed connective tissue disease (MCTD) are immune-mediated connective tissue diseases (CTDs), which may be complicated by the involvement of many organ systems. Pulmonary disease, typically manifested as interstitial lung disease (ILD), may be a part of this process and, when present, is usually associated with significant morbidity and even mortality. Prognosis and response to therapy together with presentation of pulmonary disease vary according to the underlying CTD and the specific pattern of ILD. CTD-related pulmonary disease is not confined to the interstitium. Alveoli, pleura, vascular and lymphatic structures, and airways of all diameters may all be involved in the disease-related immunopathological process.
ILDs are a group of diseases characterized by intersitital inflammation and fibrosis, and usually have no identifiable cause, so are defined as idiopathic. Those with identifiable causes are usually associated with environmental factors (pneumoconioses) or CTDs. CTD-related ILDs (CTD-ILD) are usually a consequence of the disease process and incidence varies according to the individual CTD. High-resolution computed tomography (HRCT) is able to detect early ILD [1, 2].
Krebs von den Lungen-6 (KL-6) is an important serum marker for ILD [3–5]. It is a high molecular weight, mucin-like glycoprotein classified as human MUC1 mucin secreted by type II alveolar pneumocytes and bronchial epithelial cells in response to cellular damage and regeneration in patients with ILD [4]. KL-6 has pro-fibrotic and anti-apoptotic effects on lung fibroblasts. Serum levels of KL-6 have been reported to be elevated in various ILD such as idiopathic pulmonary fibrosis, collagen vascular disease associated interstitial pneumonias, and other interstitial lung disorders [6–10].
The aim of the current study was to measure the serum levels of KL-6 in patients with CTD both with and without ILD and in a healthy control group to determine the association between serum KL-6 levels and CTD-ILD.
Materials and methods
Patients
The study included 45 patients with CTD without ILD, 68 patients with CTD-ILD and 45 healthy control subjects. Age, sex, diagnosis, medical and past history, duration of disease, type and duration of ILD (if present), smoking status, and the treatment regimen of patients were recorded. Patients with ILD were assessed for pulmonary symptoms such as cough, production of sputum, dyspnea, pleurisy, hemoptisis, and findings of direct radiographs, HRCT, respiratory function tests, and CO diffusion tests were recorded. Healthy subjects were assessed for smoking. The American College of Rheumatology criteria were used for diagnosis and classification of all patients. Inclusion criteria were any diagnosis of CTD (RA, SLE, SjS, SSc, PM/DM, MCTD) with or without ILD, and ≥18 years of age. Exclusion citeria were age <18 years and the presence of any active systemic disease such as malignancy, acute or chronic infections, and liver or kidney disease. Healthy volunteers with no known disease were used as control subjects. Informed consent was obtained from all the study participants. Approval for the study was granted by the Local Ethics Committee.
Laboratory analysis
8 mL of blood was drawn from each patient and control subject, into tubes with EDTA, then centrifuged immediately at 1000 cycle/min for 15 min. Separated serum samples were kept at −80 °C for quantification of KL-6. After dissolution and proper dilution of the samples, KL-6 levels were quantified using ELISA (Cusabio®, China) at room temperature according to the manufacturer’s instructions, and spectrophotometric absorbance values were converted to units per milliliter. The minimum detectable value was 3.9 U/mL.
Statistical analysis
Descriptive statistics were given as mean ± standard deviation (SD) for variables with normal distribution and as medians with minimum and maximum values for variables without normal distribution. Numbers with percentages (%) were used for nominal variables. Non-parametric tests were used for the data without normal distribution. ANOVA variance analysis and Kruskal Wallis tests were used to compare the mean and median values of groups, respectively. Spearman’s test was applied for comparison of continuous variables and the chi-square or Mann–Whitney U test for comparison of categorical variables according to the homogeneity of the distribution. All statistical analyses were applied using SPSS for Windows 15 statistical software. A value of p < 0.05 was accepted as statistically significant.
Results
CTD without ILD was determined in 45 (39.8 %) patients, CTD-ILD in 68 (60.2 %). The relative frequencies of specific CTDs in each group are shown in Table 1. Notably, all three patients with PM/DM in this study had ILD. The mean age was 50.8 ± 12.7 years in the CTD without ILD group, 54.1 ± 13.4 years in the CTD-ILD group, and 35.8 ± 8.5 years in the control group. In both the CTD without ILD and CTD-ILD groups, female dominance was determined (p < 0.05), whereas the control group comprised 22 (48.9 %) females and 23 (51.1 %) males.
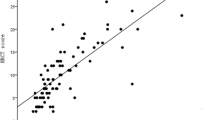
The median serum level of KL-6 was 3.9 U/mL (min 3.9; max 866.3 U/mL) in CTD without ILD, 33.75 U/mL (min 3.9; max 933.6 U/mL) in CTD-ILD, and 3.9 U/mL (min 3.9; max 132.3 U/mL) in the control group. The KL-6 levels were determined as higher in the CTD-ILD group than in the CTD without ILD (p < 0.001) and healthy control (p < 0.008) groups (Table 2). The difference was probably by chance (p = 0.28) between the CTD and the healthy control groups, so was not considered significant. As the age of the control group was younger than that of the patient groups, covariance analysis was performed according to age. A statistically significant difference in KL-6 serum levels was still present (p = 0.02) between the CTD-ILD and the other groups. No difference was determined in the KL-6 serum levels in specific disease subgroups (i.e., RA, SLE, SjS, SSc, PM/DM, and MCTD) of both the CTD without ILD or the CTD-ILD groups (p = 0.094, p = 0.585, respectively). In the CTD-ILD group, there was a positive association between the frequency of ILD and the duration of CTD (p < 0.05). No correlation was detected between the KL-6 level and the duration of either CTD or ILD (p = 0.627, p = 0.103, respectively). Of the conrol group, 30 (68.2 %) were smokers and the KL-6 serum level was higher in smokers than non-smokers (p = 0.048). No correlation was present between the number of cigarettes smoked (pack-years) and KL-6 serum level (p = 0.122). When the relationship between the duration of CTD and development of ILD was examined, it was determined that as the duration of CTD increased, so the incidence of ILD increased (p < 0.05). When the relationship between the duration of ILD and level of serum KL-6 was examined, a statistically significant relationship was determined between KL-6 level and the duration of pulmonary involvement (p = 0.103).
Discussion
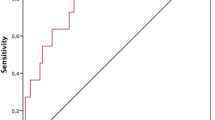
The most important result of this study was that, as expected, there was a positive association between ILD and serum levels of KL-6. As a sensitive, specific, and accurate diagnostic test for ILD, as shown by Ohnishi et al. [11], KL-6 serum level may be used for detection of ILD in patients with CTD. The results of the current study together with those of previous studies [8–10, 12, 13] have demonstrated that patients with CTD-ILD have higher serum KL-6 levels than those with CTD without ILD or a control group. Neither the duration nor the specific type of CTD affect KL-6 levels, making underlying disease-related false positive rates minimal if to be considered as a diagnostic tool for CTD-ILD. Although the current study was cross-sectional and lacked case by case longitudinal serum levels of KL-6, there was no association between the level and the duration of ILD. In a study by Kobayashi et al. [8], it was shown that serum KL-6 level was both predictive for interstitial pneumonia and correlated with the activity of pneumonitis in patients with sarcoidosis. Similar findings of a positive correlation with fibrotic activity in the lungs of patients with SSc were documented by Yanaba et al. [9]. Doishita et al. [10] reported positive correlations of KL-6 level and both the presence and activity of ILD in patients with other forms of CTDs. In addition, Hu et al. [4] showed that post-treatment serum levels of KL-6 were reduced in patients with improved ILDs and were increased in patients with advanced ILDs, thus making KL-6 level more important as a prognostic tool and enabling its use for monitoring of therapy.
Type II alveolar epithelial cells proliferate and participate in normal regenerative or pathological chronic processes in cases of inflammatory or non-inflammatory damage, either from the interstitium or airways, resulting in type II alveolar epithelial cell hyperplasia. These cells secrete several cytokines and proteins involved in local inflammatory response. One of these proteins is KL-6, a mucin-associated glycoprotein, which may be a trigger for TGF-β signaling and fibrosis [14]. Serum levels of this glycoprotein have been shown to be increased and well-correlated with the activity of pneumonitis in ILD and CTD-ILD, making it not only a marker of presence but also of activity, so there may be prognostic implications [7–10].
Smoking is known to be associated with higher serum levels of KL-6 [15] and this association was confirmed in the control group of the current study. Serum levels do not correlate with the amount smoked or duration of smoking. When there is a high serum KL-6 level in non-smokers, there should be consideration of malignant diseases of the lung and other sites, ILDs of unknown or known etiology (e.g., sarcoidosis, hypersensitivity pneumonitis, drug-induced pneumonitis, and pneumoconioses) other than CTD, radiation pneumonitis, tuberculosis, pneumocystis pneumonia, and bronchiolitis obliterans. KL-6 levels have also been shown to be associated with complications of interstitial pneumonia after bone marrow transplantation and may reflect the response to therapy but have no pre-transplantation predictive value [16].
There are some limitations to the current study. First, 68 patients with CTD-ILD and 45 with CTD without ILD were included, which although enough to document an association between serum KL-6 level and CTD-ILD, are relatively small numbers of patients, especially for detailed subgroup analyses. Second, the study was cross-sectional, with no further prognostic information of the patients. Longitudinal cohort studies are needed, especially for those with high levels of serum KL-6 with CTD but not ILD. Third, the control group was not age-matched, thus limiting the statistical power and requiring covariance analysis. Finally, there was no assessment of the activity of pneumonitis or the degree of pulmonary fibrosis, which prevented any correlations with KL-6 serum levels.
Conclusion
In conclusion, the level of KL-6 as a predictive factor could be used to identify the clinical development of ILD before it is detected on any imaging modality. Nevertheless, further prospective clinical studies are needed to define whether levels of KL-6 might have prognostic value or might predict progressive ILD.
References
Olson AL, Brown KK, Fischer A (2012) Connective tissue disease-associated lung disease. Immunol Allergy Clin North Am 32:513–536
Fischer A, Chartrand S (2015) Assessment and management of connective tissue disease-associated interstitial lung disease. Sarcoidosis Vasc Diffuse Lung Dis 22(32):2–21
Kohno N (1999) (1999) Serum marker KL-6/MUC1 for the diagnosis and management of interstitial pneumonitis. J Med Invest 46:151–158
Hu Y, Wang LS, Jin YP, et al. (2015) Serum Krebs von den Lungen-6 level as a diagnostic biomarker for interstitial lung disease in Chinese patients. Clin Respir J. doi: 10.1111/crj.12341. [Epub ahead of print]
Ishikawa N, Hattori N, Yokoyama A et al (2012) Utility of KL-6/MUC1 in the clinical management of interstitial lung diseases. Respir Inverstig 50:3–13
Bonella F, Costabel U (2014) Biomarkers in connective tissue disease-associated interstitial lung disease. Semin Respir Crit Care Med 35:181–200
Kobayashi J, Kitamura S (1995) KL-6: a serum marker for interstitial pneumonia. Chest 108:311–315
Kobayashi J, Kitamura S (1996) Serum KL-6 for the evaluation of active pneumonitis in pulmonary sarcoidosis. Chest 109:1276–82
Yanaba K, Hasegawa M, Hamaguchi Y et al (2003) Longitudinal analysis of serum KL-6 levels in patients with systemic sclerosis: association with the activity of pulmonary fibrosis. Clin Exp Rheumatol 21:429–436
Doishita S, Inokuma S, Asashima H et al (2011) Serum KL-6 level as an indicator of active or inactive interstitial pneumonitis associated with connective tissue diseases. Intern Med 50:2889–2892
Ohnishi H, Yokoyama A, Kondo K et al (2002) Comparative study of KL-6, surfactant protein-A, surfactant protein-D, and monocyte chemoattractant protein-1 as serum markers for interstitial lung diseases. Am J Respir Crit Care Med 165:378–381
Yamane K, Ihn H, Kubo M et al (2000) Serum levels of KL-6 as a useful marker for evaluating pulmonary fibrosis in patients with systemic sclerosis. J Rheumatol 27:930–934
Bonella F, Volpe A, Caramaschi P et al (2011) Surfactant protein D and KL-6 serum levels in systemic sclerosis: correlation with lung and systemic involvement. Sarcoidosis Vasc Diffuse Lung Dis 28:27–33
Ohshimo S, Yokoyama A, Hattori N et al (2005) KL-6, a human MUC1 mucin, promotes proliferation and survival of lung fibroblasts. Biochem Biophys Res Commun 338:1845–1852
Ishikawa N, Mazur W, Toljamo T et al (2011) Ageing and long term smoking affects KL-6 levels in the lung, induced sputum and plasma. BMC Pulm Med 11:22
Ashida T, Higashishiba M, Sumimoto Y et al (2001) Serum KL-6 levels in patients with pulmonary complications after allogeneic bone marrow transplantation. Int J Hematol 74:464–468
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Rights and permissions
About this article
Cite this article
Oguz, E.O., Kucuksahin, O., Turgay, M. et al. Association of serum KL-6 levels with interstitial lung disease in patients with connective tissue disease: a cross-sectional study. Clin Rheumatol 35, 663–666 (2016). https://doi.org/10.1007/s10067-015-3167-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-015-3167-8