Abstract
Objectives
This randomized, prospective, and split-mouth study aimed to evaluate flowable bulk-fill resin composites in class II restorations, comparing it with a conventional layering technique after 4-year follow-up.
Materials and methods
Fifty-three subjects received three class II restorations according to the restorative systems: conventional microhybrid composite resin (PA – Peak Universal + Amelogen Plus, Ultradent); flowable bulk-fill and nanoparticulate composite resins (ABF – Adper Single Bond 2 + Filtek Bulk Fill Flow + Filtek Z350XT, 3M/Espe); and flowable bulk-fill and microhybrid composite resins, (XST – XP Bond + SDR + TPH3, Dentsply). The clinical performance and interproximal contacts were evaluated. Statistical analyses were performed using the Kaplan-Meier, equality test of two proportions, Friedman, Wilcoxon, Kruskal-Wallis, Mann-Whitney, and Logistic regression analysis tests (alpha = 0.05).
Results
In total, 106 restorations were evaluated at 4 years. Both systems with bulk-fill composites presented higher marginal discoloration than PA. About surface texture, ABF restorative system showed superior bravo scores being statistically similar to XST. Better performance for wear and surface staining was found for XST restorative system. All restorative systems resulted in the decreased interproximal contacts, occurring early for XST.
Conclusions
The restorative systems that used flowable bulk-fill resin composites showed satisfactory clinical performance compared with conventional resin composite after 4 years. All restorative systems had decreased proximal contact after 4 years.
Clinical relevance
Initial marginal discoloration was observed in more than 50% of class II restorations performed with restorative systems that used flowable bulk-fill resin composite. All restorative systems had decreased proximal contact strength over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Composite resins became the most employed material for restoration of dental elements. The improvements in resin composite formulations and the increasing demand for esthetics have made composite resin restoration the optimal choice for restoring posterior. To improve the success of these restorations, factors related to the patient and operator are of primary importance [1].
However, the main challenge for the professional is the correct technique required by these materials. Another difficulty in direct composite resin restorations is the reconstruction of posterior large cavities, such as involving posterior proximal wall, to achieve the adequate proximal contacts [2]. The literature recommends inserting the composite resin on the inner proximal surface of the matrix band from gingival to occlusal to minimize the C-factor, the polymerization shrinkage, and the formation of marginal gaps [3, 4]. Another important factor is the amount of energy that must be supplied in the correct wavelengths to achieve a satisfactory degree of conversion of the resin material [4]. Besides, the use of 2-mm layering technique to achieve the success of conventional composite resin is also indispensable. However, the insertion of 2-mm increments and its correct light curing requires more clinical time and patient discomfort.
In this context, bulk-fill restorative resins required significantly less chair time to apply than the layering one, optimizing the clinical time and reducing the sensitivity to the technique by the professional [5, 6]. The bulk-fill composites have monomers with a high molecular weight to reduce the shrinkage stress [7]. The early bulk-fill resin-based composite (RBC) was composed with flowable consistency, being necessary a final increment with conventional composites [8, 9]. Currently, there are more three types of bulk fill RBC: bulk fill RBC (packable), sonic-activated bulk fill RBC, and dual-cure bulk fill RBC [9]. Bulk-fill packable RBC can be used alone; thus, they are more time-saving and simpler than flowable materials [9].
Some clinical studies and meta-analysis have demonstrated that bulk-fill composites have shown similar results to conventional resin composites mainly after short-term follow-up [7, 10,11,12,13,14,15,16,17,18,19]. Few randomized clinical trials (RCT) were conducted evaluating bulk-fill materials after long-term follow-up [20,21,22]. However, no randomized clinical trials (RCT) have yet compared two bulk fill restorative systems versus the incremental layering technique after 4 years. Additionally, more RCT with longer periods are necessary to evaluate the maintenance of interproximal contact of bulk fill restorative systems.
Thus, this RCT aimed to evaluate the clinical performance and interproximal contact after the placement of direct composite resin restorations in class II cavities, comparing restorative systems: one conventional 2-mm incremental resin composite with two using flowable bulk-fill covered with conventional composites. The null hypotheses tested were that there would be no difference among the three restorative systems for the clinical parameters, and that there would be no differences for the same restorative strategy over time.
Materials and methods
Study design
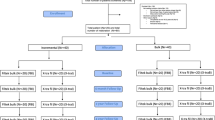
This clinical trial was a prospective, randomized, double-blind (volunteers and examiners), and split mouth model. It was executed after gaining approval from the local Ethics Committee (approval code: 1.235,100). This RCT was registered (#RBR-3gg3mg) and conducted according to CONSORT guidelines (Fig. 1). Three restorative systems were used: microhybrid conventional composite resin-considered control group (PA - Peak Universal + Amelogen Plus, Ultradent); flowable bulk-fill and nanoparticulate composite resins (ABF – Adper Single Bond 2 + Filtek Bulk Fill Flow + Filtek Z350XT, 3M/ESPE); and flowable bulk-fill and microhybrid composite resins, (XST – XP Bond + SDR + TPH3, Dentsply), and the two last restorative systems were considered test groups.
Patient selection
During March to June 2015, all patients attending the undergraduate clinic, at local faculty of dentistry who needed three class II restorations, were asked to participate in the study. The sample power for two proportions, when considering 95% success achieved for the control group and 80% for the test group, indicated that an experimental sample with 159 restorations had a high power of 98.3%.
The following inclusion criteria were used: patients presenting at least three unsatisfactory class II restorations that were at least 3 mm deep in a vital permanent premolar or molar of the maxilla or mandible with an adjacent tooth, patients with good periodontal health, and patients with no clinical history of allergies to dental products. The exclusion criteria were the following: pregnant or lactating women, patients receiving orthodontic treatment, tooth without an antagonist, and endodontically treated teeth.
In total, 53 subjects were selected and subjected to clinical and radiographic examination after signing the informed consent form.
Calibration and randomization
Two calibrated operators (residents), with clinical experiences of 19 years and 1 year, were trained by a faculty member specialized in restorative dentistry to perform the restorative procedures. For calibration, each operator performed two restorations for each group of patients that were not selected for the research. The operators were identified on the procedure sheets. The subjects then received oral hygiene instructions and initial photographs were taken.
All subjects received local anesthesia prior to restorative procedures. The randomization was performed by putting numbers in a sealed envelope and drawing which restorative procedure would be performed on each of the selected teeth. Each subject received three restorations, one from each group.
Restorative procedures
The complete restorative procedures have been described in our previous studies [23, 24]. The cavity preparations were performed using spherical diamond burs (#1015–1017; KG Sorensen, Barueri, SP Brazil), which were replaced after every three procedures. When carious tissue was found, smooth spherical carbide burs (#1/2–4, Dentsply-Maillefer, Ballaigues, Vaud, Switzerland) were also used in a slow speed handpiece. The operative field was isolated with a rubber dam.
Then, 35% phosphoric acid gel (Ultra-etch, Ultradent Products Inc., South Jordan, UT, USA) was used for 30 s on enamel and 15 s on dentin for all groups. Subsequently, adhesive systems and restorative materials were applied, following the recommendations of the respective manufacturers. Table 1 presents the specifications for each group.
To restore the shape of the proximal walls, wooden wedges, preformed metal matrices, and rings (Unimatrix sectional matrix system, TDV Dental Ltda. Pomerode, SC, Brazil) were used. Adhesives and composite resins were light-cured with a LED curing light (Valo, Ultradent Products Inc., South Jordan, UT, USA), in the standard application mode and an output of 1000 mW/cm2.
Finally, ultra-fine diamond burs (#1190F, 3118F, 1190FF, 3118FF; KG Sorensen, Cotia, SP, Brasil), and polishing points (Jiffy, Ultradent Products Inc., South Jordan, UT, USA) were used to finish all restorations.
Evaluation
Two independent and calibrated examiners, neither of which placed the restorations, were responsible for the clinical evaluations. The examiners were kept blind in the assessments. The clinical performance of restorations was assessed by visual and tactile inspection, using a flat dental mirror and a probe with both periodontal/explorer tips.
After 4-year follow-up, the restorations were evaluated using the modified US Public Health Service (USPHS) criteria, as described in Table 2. The tightness of the proximal contact was determined based on the resistance to dental floss (Sanifill, São Paulo, SP, Brazil) between the restored surface and the adjacent tooth. The following scores were used: 0 – no contact, 1 – minimum contact, 2 – ideal contact, 3 – tight contact, 4 – very tight contact [25]. In cases where more than one proximal surface was involved, the worst score of the two contacts was recorded.
Statistical methods
The Kappa index was used to measure the degree of agreement between the two evaluators. The annual failure rates were calculated. The Kaplan-Meier test was used to demonstrate the survival curve. The equality test of two proportions was used to evaluate clinical performance. The Friedman and Wilcoxon tests were used to evaluate interproximal contacts within each group, and the Kruskal-Wallis and Mann-Whitney tests were used within the same evaluation period. Dropout patients’ data were evaluated per protocol strategy used. No intention to be treated was used.
Logistic regression analysis was performed to predict the probability of total success (alpha score) of the clinical performance results at 4 years. Afterwards, the Hosmer-Lemeshow test was performed to evaluate the efficacy of the logistic regression model. All tests were performed at a 0.05% significance level. Statistical procedures were performed in the SPSS version 13.
Results
The mean age of the 53 subjects was 48.3 years (± 10.0). A total of 65 molars and 94 premolars were restored (159 restorations). The characteristics of the preparations and the restorative procedures are described in Table 3. In total, 38 subjects (71.7%) and 106 restorations were evaluated at 4-year follow-up.
There was an excellent concordance of Kappa (Baseline = 0.79, 6 months = 0.91, 1 year = 0.89, 3 years = 0.92, 4 years = 0.94). The Kaplan-Meier test showed no differences among groups regarding the survival curves when considering only charlie score or both bravo and charlie scores as failure (Fig. 2).
Table 4 shows data from the USPHS criteria. All failure data were accumulated even if the patient did not return at the evaluation, for example: PA group had 37 restorations evaluated for retention being 5 charlie scored at 4 years; however, 33 restorations were considered for marginal integrity because 1 had failed for this criterion at 3 years. Furthermore, in the first evaluation in which the restoration failed, all other criteria were evaluated if possible; however, only the criterion that failed was considered for next evaluations. Considering charlie scores, the annual failure rates at 4 years are 3.6%, 3.0%, and 2.3% for PA, ABF, and XST, respectively.
When the analysis among groups was executed, a statistically significant difference was observed for the following criteria: marginal discoloration, surface texture, wear, and superficial staining. Both systems with flowable bulk-fill composites presented higher initial marginal discoloration than PA. About surface texture, ABF restorative system showed superior bravo scores being statistically similar to XST. Better performance for wear and surface staining was found for XST when compared to other restorative systems.
When comparing the evaluation periods for each of the groups, no statistically significant difference was found for secondary caries, anatomical form, and gingival tissue for all groups. Considering retention, surface texture, and wear statistical differences were more evident from 3 years for all groups. However, the three groups presented statistical differences for marginal integrity, marginal discoloration, and surface staining from 1 year. Figure 3 represents some images of restored teeth from each group.
Evaluation of clinical performance according to USPHS criteria. A Second premolar of PA group, bravo score for the marginal integrity, and wear criteria and alpha for other criteria; B first molar representative of ABF group, charlie score for the retention criterion because a repair was performed in the buccal surface; C second premolar of XST group, alpha scores for all criteria; D second molar of the PA group, bravo scores for marginal integrity and surface staining, alpha scores for other criteria; E First molar of ABF group, bravo score for marginal integrity, marginal discoloration, wear and surface staining; alpha scores for other criteria; F second premolar of XST group, bravo scores for marginal discoloration and surface staining criteria, alpha score for other criteria; G second molar of PA group, bravo scores for marginal discoloration and wear criteria; alpha scores for other criteria; H First molar of ABF group, bravo scores for marginal integrity, marginal discoloration and surface staining, alpha scores for other criteria; I first molar of ABF group, marginal discoloration and surface staining, alpha scores for other criteria; J second premolar of PA group, charlie score for retention, bravo score for wear, and alpha scores for other criteria; (K) first molar of ABF group, charlie score for retention criterion and marginal integrity, bravo score for marginal discoloration alpha scores for other criteria; (L) second molar of XST group, bravo scores for marginal integrity and marginal discoloration, alpha scores for other criteria
Table 5 shows the interproximal contacts data. No significant difference among the groups was found. However, all restorative systems resulted in the decreased interproximal contacts, occurring from 1 year for XST.
The probability of success was influenced by the number of tooth faces involved in the restoration, previous condition, and time spent during the restorative procedures (Table 6).
Discussion
This study represents a prospective, randomized, double-blind, and split-mouth clinical trial, making possible to analyze the test and control groups under the same conditions, increasing the statistical efficiency and decreasing the number of patients required for the study [26]. Furthermore, the distribution of restorations (maximum of 3 pairs in the same patient) is in accordance to the American Dental Association guidelines when testing a new material [27]. According to van Dijken et al. [21], the theoretical sample size of 120 restorations is adequate to determine significant differences between groups treated with different materials in similar evaluations of intra-individual comparison design. The number of 53 restorations per group performed in this study was superior to that estimated by these authors [21]. Thereby, 159 restorations were considered a power of 98.3%. Also, 106 restorations were evaluated at 4-year follow-up, making the detection of statistical differences possible among the groups.
The method used for the performance of the restorations was USPHS, used in several clinical trials [11, 12, 21, 28, 29], although other criteria for the clinical evaluation of restorations can be found, such as those used by the World Dental Federation (FDI criteria) [13]. The FDI criteria better presented the restorations’ clinical success. However, in the case of failure, both criteria provided the same result [14]. The Kappa test revealed an increased and excellent agreement among the evaluators over time.
In this study, the annual failure rates were 3.6% for PA, 3.0% for ABF, and 2.3% for XST. In other study, the annual failure rate was 2.2% for flowable bulk-fill and 1.6% for conventional composite resin place in class II restorations, both over a 3-year period of comparison [29]. The causes of failure were mentioned dental fracture followed by fracture of the restorative material [29]. In a 5-year follow-up, flowable bulk-fill showed a satisfactory success rate, with an annual failure rate of 1.4% when observing only class II cavities [30]. Among the main causes of failure, a cusp fracture with 40% frequency was found, and the authors conclude that over the 5-year evaluation period; these materials present adequate results that support the indication in clinical practice [30]. In a systemic review, bulk-fill and conventional composites of class II restorations based on RCTs found annual failure rates of 1.1 (± 0.9) and 1.4 (± 1.4), respectively [31]. Although the curves from survival analysis showed no statistical differences among groups, possible changes may be detected in future evaluations considering both bravo and charlie scores.
Retention, marginal integrity and marginal discoloration are the main criteria that determine the longevity of restorations [32]. These parameters are directly related to the stress produced at the tooth/restoration interface, which may be influenced by the geometry of the cavity, adhesive systems, viscosity of the restorative materials, and placement technique [32].
When considering retention, no statistical difference of conventional composite resin, if compared to the bulk-fill resin composites, was found. However, XST group presented 2 charlie score after 1-year follow-up, and ABF group presented 3 bravo and 3 charlie scores at 3-year follow-up. In the case of bulk-fill resin composites, although they present similar percentage of filler particles (64.5% for ABF and 68% for XST), the monomers of Filtek Bulk Fill Flow present similar structure to conventional resins, while Surefil SDR has a patented monomer (SDR-UDMA) [33, 34]. A study comparing conventional resins to flowable and full-body bulk-fill composite resins, using tomography analysis, concluded that the flowable bulk-fill resins can promote an increased void in class II restorations, and it seems to be more related to voids present inside the syringe of the material than to the use of incremental or bulk-fill restorative techniques [35]. A clinical trial that evaluated the SDR bulk resin found one fractured restoration only after 5 years [21]. Furthermore, when partial retention occurs, both low and high-viscosity resin composites are amenable to successful repair using adhesives with functional monomers [36].
Regarding marginal integrity, no differences among the groups in all evaluations were found. Corroborating with this study, similarity in marginal adaptation among incremental and bulk-fill techniques after thermomechanical cycling was found using FDI criteria [37]. This fact maybe can be explained by the presence of enamel margins and the low modulus of elasticity of bulk materials, reducing the stresses generated by the polymerization contraction and, thereby, maintaining the marginal integrity [37, 38]. Another study comparing the same flowable bulk-fill composite resins used in our work showed similar polymerization shrinkage between them when performed analysis of microtomography in class II cavities [39]. Furthermore, a systematic review and meta-analysis of in vitro studies were observed that bulk fill composites had marginal integrity comparable to conventional resin composites with incremental techniques, corroborating with our study [40]. Clearly, the higher number of bravo scores begun at 1-year follow-up, since they kept statistically similar from 1 year until 4 years for PA and a statistical increase occurred for ABF and XST between 1 and 3 years, keeping similar to 4 years. In other study that compared conventional and bulk-fill composites in class II cavities, increased bravo scores were found only for conventional microhybrid composite at 2-years; however, the full-body Filtek Bulk Fill was used instead of the flowable version [11]. All restorative flowable bulk-fill systems also presented increased number of bravo scores after 2 years, but one of the flowable bulk-fill composite (ever X Posterior + G -aenial Posterior) had the double number of slight marginal unfitness than the other restorative system (SureFil SDR flow + Ceram.X mono) [12]. Durão et al. [14] indicated significant differences between all observation times for marginal adaptation (baseline, 12, and 36 months) when incremental and bulk-fill restorative systems were evaluated. One meta-analysis demonstrated that only marginal adaptation after 12 months showed statistically significant outcomes, in which conventional composites presented significantly better results than resin composites containing modified monomers [7].
In relation to marginal discoloration, the differences among the performances of the resin composites became more evident after 4-year follow-up, where bulk restorative systems presented greater marginal discoloration than conventional one. When the percentage of restorations with marginal gaps for same three resin composites after artificial aging was studied, the conventional composite resin was superior regarding marginal gap formation in enamel than flowable bulk-fill resin composites [41]. Flowable bulk-fill composites also had a higher imperfect margins than full-body bulk-fill [39, 42] and conventional microhybrid composites in class II restorations performed in an in vitro study [42]. The viscosity of the bulk-fill restorative material also influenced the proportion of gap-free marginal interface in dentin [42].
However, in other clinical trials evaluating posterior restorations, no marginal discoloration was found in 100% and 89.2% restorations with flowable bulk-fill resin composite (Surefil SDR) at 3- and 6-year follow-up, respectively [21]. Furthermore, superior discoloration and marginal adaptation were found for conventional nanofill (Filtek Ultimate) compared to full-body bulk-fill composite (Tetric EvoCeram Bulk Fill) at 3 and 6 years [22, 28]. A superiority of the etch-and-rise adhesive technique was seen compared to self-etch approach for marginal discoloration in vivo and adaptation in vitro, irrespective of the composite used [13, 43]. Although adhesive systems present different compositions, in our study, phosphoric acid gel was applied for all groups. Furthermore, two operators performed the restorations with different time of clinical experience, reflecting the actual clinical practice, in those clinical trials [21, 28]. Only an operator performed all restorations may improve the results [1]. Decreased alpha scores for marginal discoloration occurred over time for all groups, corroborating with other studies which evaluated bulk resins [11,12,13, 21, 28].
The next three criteria that will be discussed involve the resins used as top layer. With regard to surface texture, ABF showed the lowest number of alpha scores at 4-year follow-up, probably due to the presence of the TEGDMA monomer, which has an aliphatic chain, being more susceptible to the constant challenges of the oral cavity, such as water absorption and when exposed to acid environment [44, 45]. Furthermore, PA and ABF presented a high number of bravo scores for wear and surface staining, since only TPH resin has no TEGDMA monomer in its composition [46]. All restorative systems studied had statistical differences for surface texture and wear over time; however, the resins used as top layer, which contain TEGDMA, had initial surface staining from 6-month.
Clinical literature evaluating the intensity of the proximal contacts of posterior flowable bulk resin composite restorations in vivo is scarce. A recent study assessed the proximal contact of a full-body bulk-fill resin composite in class II restorations where all teeth restored with conventional and bulk resin had alpha score for this criterion after 2 years [11]. The current study also found no difference among the groups; however, all restorative system showed a decreased proximal contact over time, occurring early for XST. Manufacturers of both flowable bulk-fill composites studied recommend a 2-mm capping layer with a conventional composite resin; nonetheless, the bulk-fill composite may extend to reestablish the proximal contacts in a clinical situation. Algamaiah et al. [39] report that volumetric changes of flowable bulk-fill composites may compromise the precision of proximal contacts, leaving a space between adjacent teeth for food impaction. Van Ende et al. [47], in a review of the literature, suggested that a thicker consistency of bulk-fill composite might also help in obtaining a good contact point. Our findings showed that a mean of 1.9 was detected for all proximal contacts at baseline because the operators carefully observe if the contact was established after final curing.
According to the logistic regression analysis, some factors influenced the results, but the number of restored faces was the main factor because influenced three criteria: retention, marginal integrity and surface staining. Probably, higher volume of composite resins may promote an increase in the shrinkage stress, promoting greater chance of failure. This factor influenced the retention, marginal integrity, and surface staining. Polymerization shrinkage stress of resin-based materials has been related to several unwanted clinical consequences, such as marginal and internal gaps, and decreased bond strength [48].
Gingival floor of the proximal box and pulpal floor of the cavity had higher imperfect margin percentage than buccal and lingual walls of the proximal box [38]. In this study, radiographies were taken at all evaluation period to help in diagnosis when with only visual exam was not sufficient to define the scores. However, only standardized radiographies will be used in a future study, as well as clinical analysis with longer evaluation will be performed. New versions of a direct bulk fill resin composites should also be studied, such as short-fiber-reinforced resin composite which is indicated in large complex cavities [49] The limitations of this study included the inability to introduce blind operators and patient dropouts.
Conclusion
The restorative systems that used flowable bulk-fill resin composites showed satisfactory clinical performance compared with conventional resin composite after 4 years. However, the restorative systems with flowable bulk-fill resin composites presented initial marginal discoloration more evident than conventional one. All restorative systems had decreased proximal contact until 4-year of clinical service.
References
Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJ (2012) Longevity of posterior composite restorations: not only a matter of materials. Dent Mater 28:87–101. https://doi.org/10.1016/j.dental.2011.09.003
Alonso V, Caserio M, Darriba IL (2019) Use of transparent tips for obtaining tight proximal contacts in direct class II composite resin restorations. Oper Dent 44:446–451. https://doi.org/10.2341/17-112-T
El-Shamy H, Saber MH, Dörfer CE, El-Badrawy W, Loomans BAC (2012) Influence of volumetric shrinkage and curing light intensity on proximal contact tightness of class II resin composite restorations: in vitro study. Oper Dent 37:205–210. https://doi.org/10.2341/11-269-L
Ilie N, Stark K (2015) Effect of different curing protocols on the mechanical properties of low-viscosity bulk-fill composites. Clin Oral Investig 19:271–219. https://doi.org/10.1007/s00784-014-1262-x
Sabbagh J, McConnell RJ, McConnell MC (2017) Posterior composites: update on cavities and filling techniques. J Dent 57:86–90. https://doi.org/10.1016/j.jdent.2016.11.010
Torres CR, Jurema AL, Souza MY, Di Nicoló R, Borges AB (2021) Bulk-fill versus layering pure ormocer posterior restorations: a randomized split-mouth clinical trial. Am J Dent 34:143–149
Kruly PC, Giannini M, Pascotto RC, Tokubo LM, Suga USG, Marques ACR, Terada RSS (2018) Meta-analysis of the clinical behavior of posterior direct resin restorations: low polymerization shrinkage resin in comparison to methacrylate composite resin. PloS One 13:e0191942. https://doi.org/10.1371/journal.pone.0191942
Leprince JG, Palin WM, Vanacker J, Sabbagh J, Devaux J, Leloup G (2015) Physico-mechanical characteristics of commercially available bulk-fill composites. J Dent 42:993–1000. https://doi.org/10.1016/j.jdent.2014.05.009
Chesterman J, Jowett A, Gallacher A, Nixon P (2017) Bulk-fill resin-based composite restorative materials: a review. Br Dent 222:337–344. https://doi.org/10.1038/sj.bdj.2017.214
Veloso SRM, Lemos CAA, de Moraes SLD, do Egito Vasconcelos BC, Pellizzer EP, de Melo Monteiro GQ (2019) Clinical performance of bulk-fill and conventional resin composite restorations in posterior teeth: a systematic review and meta-analysis. Clin Oral Investig 23:221–233 https://doi.org/10.1007/s00784-018-2429-7
Balkaya H, Arslan S (2020) A two year clinical comparison of three different restorative materials in class II cavities. Oper Dent 45:E32–E42. https://doi.org/10.2341/19-078-C
Guney T, Yazici AR (2019) 24-month clinical evaluation of different bulk-fill restorative resins in class II restorations. Oper Dent 45:123–133. https://doi.org/10.2341/18-144-C
Loguercio AD, Rezende M, Gutierrez MF, Costa TF, Armas-Vega A, Reis A (2019) Randomized 36-month follow-up of posterior bulk filled resin composite restorations. J Dent 85:93–102. https://doi.org/10.1016/j.jdent.2019.05.018
Durão MA, Andrade AKM, Santos MDCMDS, Montes MAJR, Monteiro GQM (2021) Clinical performance of bulk-fill resin composite restorations using the united states public health service and federation dentaire internationale criteria: a 12-month randomized clinical trial. Eur J Dent 15:179–192. https://doi.org/10.1055/s-0040-1718639
Suneelkumar C, Harshala P, Madhusudhana K, Lavanya A, Subha A, Swapna S (2021) Clinical performance of class I cavities restored with bulk fill composite at a 1-year follow-up using the FDI criteria: a randomized clinical trial. Restor Dent Endod 46:e24. https://doi.org/10.5395/rde.2021.46.e24
Berti LS, Turssi CP, Amaral FL, Basting RT, Junqueira JLC, Panzarella FK, Reis AF, França FM (2020) Clinical and radiographic evaluation of high viscosity bulk-fill resin composite restorations. Am J Dent 33:213–217
Akman H, Tosun G (2020) Clinical evaluation of bulk-fill resins and glass ionomer restorative materials: a 1-year follow-up randomized clinical trial in children. Niger J Clin Pract 23:489–497. https://doi.org/10.4103/njcp.njcp_519_19
Balkaya H, Arslan S, Pala K (2019) A randomized, prospective clinical study evaluating effectiveness of a bulk-fill composite resin, a conventional composite resin and a reinforced glass ionomer in class II cavities: one-year results. J Appl Oral Sci 27:e20180678. https://doi.org/10.1590/1678-7757-2018-0678
Hoffmann L, Neuerer C, Heck K, Kunzelmann KH (2021) Bulk-fill composites compared to a nanohybrid composite in class-II cavities - a two-year follow-up study. J Adhes Dent 1(23):389–396. https://doi.org/10.3290/j.jad.b2000185
Heck K, Manhart J, Hickel R, Diegritz C (2018) Clinical evaluation of the bulk fill composite QuiXfil in molar class I and II cavities: 10-year results of a RCT. Dent Mater 34:e138–e147. https://doi.org/10.1016/j.dental.2018.03.023
van Dijken JWV, Pallesen U (2017) Bulk-filled posterior resin restorations based on stress-decreasing resin technology: a randomized, controlled 6-year evaluation. Eur J Oral Sci 125:303–309. https://doi.org/10.1111/eos.12351
Yazici AR, Kutuk ZB, Ergin E, Karahan S, Antonson AS (2021) Six-year clinical evaluation of bulk-fill and nanofill resin composite restorations. Clin Oral Investig 26:417–426. https://doi.org/10.1007/s00784-021-04015-2
Frascino S, Fagundes TC, Silva U, Rahal V, Barboza A, Santos PH, Briso A (2019) Randomized prospective clinical trial of class II restorations using low-shrinkage flowable resin composite. Oper Dent 45:19–29. https://doi.org/10.2341/18-230-C
Moda MD, Briso AF, Hoshino IAE, Frascino SMB, Santos PH, Gonçalves DM, Fagundes TC (2021) Three-year randomized prospective clinical trial of class II restorations using flowable bulk-fill resin composites. Oper Dent 14 Online ahead of print https://doi.org/10.2341/20-031-C
Teich ST, Joseph J, Sartori N, Heima M, Duarte S (2014) Dental floss selection and its impact on evaluation of interproximal contacts in licensure exams. J Dent Educ 78:921–926. https://doi.org/10.1002/j.0022-0337.2014.78.6.tb05746.x
Zhu H, Zhang S, Ahn C (2017) Sample size considerations for split-mouth design. Stat Methods Med Res 26:2543–2551. https://doi.org/10.1177/0962280215601137
Council on Scientific Affairs (2001) Resin based composites for posterior restorations: Acceptance Program Guidelines American Dental Association, Chicago https://doi.org/10.14219/jada.archive.2003.0204
Yazici AR, Antonson SA, Kutuk ZB, Ergin E (2017) Thirty-six-month clinical comparison of bulk fill and nanofill composite restorations. Oper Dent 42:478–485. https://doi.org/10.2341/16-220-C
van Dijken JW, Pallesen U (2015) Randomized 3-year clinical evaluation of class I and II posterior resin restorations placed with a bulk-fill resin composite and a one-step self- -etching adhesive. J Adhes Dent 17:81–88. https://doi.org/10.3290/j.jad.a33502
van Dijken JW, Pallesen U (2016) Posterior bulk-filled resin composite restorations. A 5-year randomized controlled clinical study. J Dent 51:29–35. https://doi.org/10.1016/j.jdent.2016.05.008
Splieth CH, Kanzow P, Wiegand A, Schmoeckel J, Jablonski-Momeni A (2020) How to intervene in the caries process: proximal caries in adolescents and adults-a systematic review and meta-analysis. Clin Oral Investig 24:1623–1636. https://doi.org/10.1007/s00784-020-03201-y
Correia A, Jurema A, Andrade MR, Borges A, Bresciani E, Caneppele T (2020) Clinical evaluation of noncarious cervical lesions of different extensions restored with bulk-fill or conventional resin composite: preliminary results of a randomized clinical trial. Oper Dent 45:e11–e20. https://doi.org/10.2341/18-256-C
Alshali RZ, Silikas N, Satterthwaite JD (2013) Degree of conversion of bulk-fill compared to conventional resin-composites at two time intervals. Dent Mater 29(9):e213–e217. https://doi.org/10.1016/j.dental.2013.05.011
Ilie N, Hickel R (2011) Investigations on a methacrylate-based flowable composite based on the SDR™ technology. Dent Mater 27:348–355. https://doi.org/10.1016/j.dental.2010.11.014
Pardo Díaz CA, Shimokawa C, Sampaio CS, Freitas AZ, Turbino ML (2019) Characterization and comparative analysis of voids in class II composite resin restorations by optical coherence tomography. Oper Dent 45:71–79. https://doi.org/10.2341/18-290-L
Lum IR, Martos R, Szalóki M, Lynch CD, Hegedűs C (2021) Effects of different surface treatments and adhesive self-etch functional monomers on the repair of bulk fill composites: a randomised controlled study. J Dent 108:103637. https://doi.org/10.1016/j.jdent.2021.103637
Al-Harbi F, Kaisarly D, Bader D, El Gezawi M (2016) Marginal integrity of bulk versus incremental fill class II composite restorations. Oper Dent 41:146–156. https://doi.org/10.2341/14-306-L
Campos EA, Ardu S, Lefever D, Jassé FF, Bortolotto T, Krejci I (2014) Marginal adaptation of class II cavities restored with bulk-fill composites. J Dent 42(5):575–581. https://doi.org/10.1016/j.jdent.2014.02.007
Algamaiah H, Sampaio CS, Rigo LC, Janal MN, Giannini M, Bonfante EA, Hirata R (2017) Microcomputed tomography evaluation of volumetric shrinkage of bulk-fill composites in class II cavities. J Esthet Restor Dent 29:118–127. https://doi.org/10.1111/jerd.12275
Gerula-Szymańska A, Kaczor K, Lewusz-Butkiewicz K, Nowicka A (2020) Marginal integrity of flowable and packable bulk fill materials used for class II restorations -a systematic review and meta-analysis of in vitro studies. Dent Mater J https://doi.org/10.4012/dmj.2018-180
Peutzfeldt A, Mühlebach S, Lussi A, Flury S (2018) Marginal gap formation in approximal “bulk fill” resin composite restorations after artificial ageing. Oper Dent 43(2):180–189. https://doi.org/10.2341/17-068-L
Han SH, Park SH (2017) Comparison of internal adaptation in class II bulk-fill composite restorations using micro-CT. Oper Dent 42:203–214. https://doi.org/10.2341/16-023-L
Haak R, Näke T, Park KJ, Ziebolz D, Krause F, Schneider H (2019) Internal and marginal adaptation of high-viscosity bulk-fill composites in class II cavities placed with different adhesive strategies. Odontology 107:374–382. https://doi.org/10.1007/s10266-018-0402-1
Gajewski V, Pfeifer CS, Fróes-Salgado NR, Boaro LC, Braga RR (2012) Monomers used in resin composites: degree of conversion, mechanical properties and water sorption/solubility. Braz Dent J. 23:508–514. https://doi.org/10.1590/s0103-64402012000500007
Rahim TN, Mohamad D, Md Akil H, Ab Rahman I (2012) Water sorption characteristics of restorative dental composites immersed in acidic drinks. Dent Mater 28:e63–e70. https://doi.org/10.1016/j.dental.2012.03.011
Ferracane JL (2006) Hygroscopic and hydrolytic effects in dental polymer networks. Dent Mater 22:211–222. https://doi.org/10.1016/j.dental.2005.05.005
van Ende A, De Munck J, Lise DP, Van Meerbeek B (2017) Bulk-fill composites: a review of the current literature. J Adhes Dent 19:95–109. https://doi.org/10.3290/j.jad.a38141
Soares CJ, Faria-E-Silva AL, Rodrigues MP, Vilela ABF, Pfeifer CS, Tantbirojn D, Versluis A (2017) Polymerization shrinkage stress of composite resins and resin cements - what do we need to know? Braz Oral Res 28(suppl 1):e62, . https://doi.org/10.1590/1807-3107
El Aziz RH, Mohammed MM, Gomaa HA (2020) Clinical performance of short-fiber-reinforced resin composite restorations vs resin composite onlay restorations in complex cavities of molars (Randomized Clinical Trial). J Contemp Dent Pract 1(21):296–303
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee (approval code: 1.235.100) and the study was registered (#RBR-3gg3mg) and conducted according to CONSORT guidelines.
Consent to participate
The authors affirm that research informed consent was obtained from all individual participants included in the study, with information on participation and publication of data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Endo Hoshino, I.A., Fraga Briso, A.L., Bueno Esteves, L.M. et al. Randomized prospective clinical trial of class II restorations using flowable bulk-fill resin composites: 4-year follow-up. Clin Oral Invest 26, 5697–5710 (2022). https://doi.org/10.1007/s00784-022-04526-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04526-6