Abstract
Objectives
This study compared the clinical performance of two bulk-fill (BF) and one conventional resin composite in a population with a high caries incidence.
Materials and methods
A total of 138 class I and II restorations were performed and randomly divided into three groups (n = 46) with equal allocation: Filtek BF (FBF; 3M ESPE), Tetric EvoCeram BF (TBF; Ivoclar Vivadent), and control Filtek Z250 (Z250; 3M ESPE). The evaluations were performed using the USPHS and FDI criteria at baseline and after 12 and 36 months by a previously calibrated evaluator. The Friedman and Wilcoxon tests for paired data were used for statistical analysis (α = 0.05).
Results
The DMFT index at baseline was 9.44, with 87% from the decayed component. After 36 months, 108 restorations (n = 36) were evaluated. Two failures were observed for TBF at marginal adaptation and recurrence of caries, resulting in a survival rate of 94.44% and an annual failure rate (AFR) of 1.26%. No equivalence was observed between the criteria for surface roughness, marginal adaptation, and discoloration.
Conclusions
The 36-month clinical performance of high-viscosity BF resin composites was comparable to conventional incremental-filled resin composites. The FDI criteria better presented the restorations’ clinical success. However, in the case of failure, both criteria provided the same result.
Clinical relevance
High-viscosity bulk-fill resin composites showed excellent performance after 36 months in a high caries incidence population. It can be considered a simplified alternative restoration method that reduces operating time and minimizes possible operator errors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Resin composites are the most used materials for the restoration of posterior teeth. Many modifications in the composition, restoration technique, and light-curing protocols have been proposed to increase the material’s clinical longevity [1, 2]. Simplified materials and techniques have become a trend in restorative dentistry to minimize technical sensitivity and optimize operating time [3]. Within this context, bulk-fill resin composites have emerged as alternatives to conventional, incrementally filled resin composites [4, 5]. The clinical performance of new restorative materials should ideally be based on clinical trials.
The first commercially available bulk-fill resin composites were of low viscosity (flowable) and required coverage by a conventional resin composite. Later, high-viscosity bulk-fill resin composites that could be sculpted (“full-body”) were marketed [3]. A more translucent resin matrix led to increased light penetration and depth of cure, enabling cavity filling in single increments of 4–5 mm [6, 7]. In addition to minimizing operating time, the use of single increments reduces the risk of incorporating voids and contamination between increments [8, 9].
Laboratory studies have reported similar results for conventional and bulk-fill resin composites. However, randomized clinical trials are needed to evaluate bulk-fill resin composites’ equivalence or superiority over conventional incremental-fill resin-based composites [10]. Searches performed in PubMed until January 2020 identified only three randomized clinical trials of sculptable bulk-fill resins with clinical follow-up longer than 24 months [11,12,13].
Different clinical parameters have been used for the evaluation of dental restorations. The United States Public Health Service (USPHS), also known as the Ryge criteria, is the most widely used criterion [14, 15]. Several modifications have been proposed to adapt the analyses to each type of study. Although allowing a more in-depth analysis, these modifications render data comparison across different studies a significant challenge. In 2007, the World Dental Federation (FDI) criteria were introduced to evaluate dental restoration’s clinical performance [16, 17]. The criteria are divided into three major groups that evaluate esthetic, functional, and biological properties by attributing a score that ranges from 1 to 5 [18,19,20].
The longevity of posterior resin composite restorations is influenced by clinical variables (type, size, and position of the restoration), operator quality and technique, socioeconomic factors (income and type of dental service), demographic factors (patient age), and behavioral variables (prevalence of caries) [21]. In the first year after restoration, the main reasons for failure are almost exclusively related to endodontic complications. The prevalence of endodontic complications decreases over time, and caries and fractures become the leading causes of failure. According to Opdam et al. (2014), failures due to caries were observed after 2 years, increasing over time. The patient’s caries risk has been shown to influence restorations’ longevity [22, 23].
Therefore, this study aimed to compare two high-viscosity bulk-fill resin composites’ clinical performance and one conventional incremental-fill resin composite in a high caries incidence population. Restorations in posterior teeth with class I and II cavities were observed over 36 months using the modified USPHS and FDI criteria. Two hypotheses were tested: (1) the clinical performance of the materials does not differ over the studied period; (2) there is no difference between the evaluation criteria for the corresponding categories.
Materials and methods
Ethical considerations
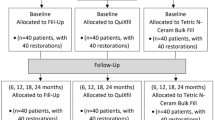
The study was approved by the Ethics Committee on Research Involving Humans of the University of Pernambuco, Brazil (Approval No. 944,518). The study was registered with the Brazilian Clinical Trials Registry (ReBEC; RBR-5v6dsj) and was conducted following the Consolidated Standards of Reporting Trials (CONSORT, Fig. 1) [24].
Flow diagram of the study (CONSORT 2010) [24]
Study design
This randomized, controlled, double-blind (patient and evaluator), split-mouth clinical study consisted of three groups with equal allocation. All restorations were performed between March and July 2015 in a University-based setting at the Postgraduate Clinic of the Dental School, University of Pernambuco, Brazil.
Sample size calculation
Considering that the study’s hypothesis was the restorative materials’ clinical performance, the annual failure rate (AFR) was considered the primary outcome. The sample size was calculated based on the AFR of 1.61% of a previous study that evaluated resin composite restorations in posterior teeth [1]. The Sealed Envelope software (www.sealedenvelope.com) was used for sample size calculation. The minimum required sample was 36 restorations per group to detect a 15% difference between groups, assuming a 5% significance level (alpha) and 80% power (beta) in a two-tailed test. Study designs that evaluated resin composite in posterior restorations with similar intraindividual comparisons found significant differences for this sample size [25]. The sample was increased to 46 restorations per group, given possible losses to follow-up.
Population and eligibility criteria
Adolescents from three public state schools located near the university campus were recruited. Criteria for inclusion were age between 12 and 18 years (mean of 14.82), presence of three vital teeth, either decayed or with unsatisfactory restorations (Black class I or II cavities); the presence of occlusal and proximal contacts; good general health; and no contraindication to dental treatment. Patients were excluded if they had advanced periodontal disease, non-carious cervical lesions in the teeth selected for the study, posterior teeth with pulpal alterations, teeth endodontically treated, or pulp exposure during the removal of carious tissue, and teeth with a history of pain. Smokers and individuals with potential behavioral problems that would not cooperate during interventions were also excluded from the study.
All participants filled out a small socioeconomic questionnaire. Information on whom the adolescent lived, the maternal education level, the monthly household income, and their access to health care was collected.
Participant adherence
All volunteers underwent complete dental treatment and periodical follow-up. For the assessments, the volunteers were contacted by telephone, WhatsApp® message, Facebook, or e-mail. Four attempts, including visits to the schools, were made to contact the volunteer before he/she was considered lost to follow-up.
Randomization, allocation sequence, and blinding
Each patient received three restorations, each with one of the studied materials (Table 1). All restoration procedures began in the most posterior tooth and followed the quadrants (upper right, upper left, lower left, and lower right). Three brown sealed envelopes were used for each participant, each containing one of the restorative groups assigned [1]. Before the restoration procedure, a draw was held by someone not involved in the study, indicating the restorative material to be used to ensure randomness. In this study, the patients and the evaluator were unaware of the restorative material used.
Clinical procedure
Before the examination, all patients received instructions about oral hygiene and diet, followed by dental prophylaxis. Intraoral photographs and interproximal radiographs were obtained. The sum of the number of decayed, missing due to caries, and filled permanent teeth at baseline was also registered (DMFT index). The teeth selected for the study were submitted to thermal pulp sensitivity testing using refrigerant spray (Endo-Frost, Wilcos do Brasil Ind. e Com., Ltda., Rio de Janeiro, Brazil).
After anesthesia, the cavities were prepared with round diamond tips (#1015-1017; KG Sorensen, Barueri, Brazil) at high rotation and round burs at low rotation under constant water cooling, limiting the procedure to the removal of carious tissue. The same operator with more than 25 years of clinical experience performed all 138 class I or II restorations. The final dimensions of all cavities were measured with a periodontal probe with a minimum depth (distance from the cavosurface angle to the pulpal floor) of 3 mm. Cavities between 3.0 and 3.9 mm deep were considered medium cavities, and cavities over 4 mm were considered deep cavities.
All cavities were isolated with a rubber dam. The dentin-pulp complex was protected according to cavity depth and the type of substrate. Selective enamel etching with 37% phosphoric acid was applied for 30 s before applying the self-etch bonding agent (Clearfil SE Bond - SEB, Kuraray, Tokyo, Japan). Dentine hardness was evaluated to define the need for resin-modified glass ionomer liner (Vitrebond, 3M ESPE, St. Paul, MN, USA) in deep cavities (> 4 mm). In the presence of harder reparative dentin, no lining was used [26]. The resin composites were placed and light-cured, as recommended by the manufacturer (Table 1). For all procedures, an LED light-curing unit (LCU) was used in the continuous mode at an intensity of 1200 mW/cm2 (Radii-cal, SDI, Victoria, Australia). According to manufacturer recommendation, after removing the matrix/wedge assembly (TDV, Pomerode, Santa Catarina, Brazil), the proximal regions were also light-cured on the lingual and buccal sides for 10 s.
At the end of each restoration, the occlusal contacts were adjusted with 12-blade carbide burs at high rotation using water/air spray. If necessary, flexible aluminum oxide sanding discs were used at low rotation (Sistema Sof-Lex, 3M ESPE, St. Paul, MN, USA). The proximal contact and cervical adaptation were verified with dental floss and adjusted with abrasive strips (3M ESPE, St. Paul, MN, USA). Finishing and polishing were performed 24 h with rubber points of decreasing grit (Astropol, Ivoclar Vivadent, Amherst, NY, USA) and a silicon carbide brush (Astrobrush, Ivoclar Vivadent) at low rotation using intermittent movements under water cooling. Abrasive strips were used in the proximal areas (3M ESPE, St. Paul, MN, USA).
Calibration, clinical evaluation, and data collection
The restorations were evaluated after 1 week (baseline) and after 12 and 36 months. The 36-month assessment was performed independently by an experienced and trained evaluator who was blind regarding treatment allocation and did not participate in the restoration procedures [16, 17]. Intraexaminer calibrations were performed for both evaluation methods (USPHS and FDI). At baseline, the agreement of 84% was obtained before the beginning of the assessments. The process at baseline was also supported by the online training and calibration tool e-Calib (www.e-calib.info), which was no longer available before the 36-month assessments. Calibration was done by clinically assessing 20 direct resin composite restorations from other volunteers who did not participate in the clinical trial and presented restorations with USPHS (A, B, C) and FDI (1–5) scores.
The restorations were evaluated using the modified USPHS (Table 2) and FDI criteria (Table 3). The modified USPHS criteria establish that Alpha and Bravo scores are classified as success and acceptable, respectively. Failure of the restoration is only defined when a Charlie score is attributed [1, 27, 28]. For the FDI criteria, scores 1, 2, and 3 are clinically excellent, good, and satisfactory. Score 4 is clinically unsatisfactory but reparable, while score 5 is attributed to clinically poor or failed restorations that need to be replaced [17]. With the aid of a mirror, patients observed the restored teeth and were asked whether they were satisfied with the restorations.
The modified USPHS and FDI criteria were compared in each group at the different observation times considering shared categories: marginal adaptation, color/color stability and translucency, marginal discoloration/(marginal) staining, anatomic form, surface roughness/gloss and roughness, postoperative sensitivity, and recurrence of caries. For this comparison, the scores obtained with the two evaluation methods were categorized as a success (Alpha; scores 1 and 2), clinically acceptable (Bravo; score 3), and failure (Charlie; scores 4 and 5) [16]. The formula (1-y)z = (1-x) was used to calculate the annual failure rate (AFR) of the restorations. The mean AFR is expressed by “y” and “x,” the total failure rate at “z” years [23].
Statistical analysis
Only the data from participants who were analyzed at the observation times were considered following per-protocol analysis. The Statistical Package for the Social Sciences v23 (SPSS) program was used for statistical analysis of each category/evaluation criteria.
Descriptive statistics were used to illustrate the distribution of the data. The homogeneity of the distribution of the sample’s clinical characteristics was evaluated using Fisher’s exact test and Pearson’s chi-square test. The Friedman test was applied to evaluate the resin composites’ differences at each observation time and differences between time points for each resin composite. In the case of a significant difference, multiple comparison tests of the Friedman test were used. If the number of events was too small, a Kaplan-Meier’s curve could not be used [29]. The results between the USPHS and FDI criteria were compared using the Wilcoxon test for paired data. A 5% error margin was established for the statistical tests, and intervals were obtained with 95% confidence.
Results
Twenty-two (47.8%) out of the 46 volunteers included in the study were male, and 24 (52.2%) were female. The baseline DMFT index was 9.44 and was influenced mainly by the decayed component (87%), followed by the missing (11%) and filled (2%) components. There was a cumulative loss of 10 volunteers in the 12- and 36-month assessments. Since this was a split-mouth study, this loss was not characterized as isolated losses of a group. Thirty-six volunteers were evaluated at 36 months, including 15 (41.7 %) males and 21 (58.3%) females.
In the present study, all adolescents were enrolled in public schools, and most of them lived only with their mother (45.6%). The most frequent maternal education level was an incomplete elementary school (48.4%), which corresponds to less than 8 years of schooling. Regarding monthly household income, 82.7% of the families of the volunteers received up to one minimum wage (approximately US$ 250/month at baseline). Also, there was the difficulty of access to health care.
Table 4 shows the clinical characteristics of the restored cavities. Apart from cavity depth at baseline (p = 0.029), all other variables (the type of restored tooth, width, depth, and the cavity classification (Black), and pulp protection used) were homogeneously distributed within the three groups (p > 0.05). A higher number of deep cavities was observed for the bulk-fill resin composites at baseline, but not at 36-month (p = 0.338). However, no differences between groups were observed within the pulp protection used. At 36 months, although without significant differences, 20.4% (n = 22) of the restorations were class II cavities, 73.1% (n = 79) had an isthmus width greater than 1/3 of the intercuspal distance, and 63.9% (n = 69) were deep cavities.
The results of clinical evaluation of the restorations according to the USPHS and FDI criteria (esthetic, functional, and biological properties) at the three observation times (baseline, 12, and 36 months) are shown in Tables 5, 6, 7, and 8, respectively. For the modified USPHS criteria, two failures were observed for TBF restoration (Table 5): at 12-month, for marginal adaptation and at 36-month, a failure regarding recurrent caries. A primary carious lesion was observed in the mesial side of a class I restoration that needed to be repaired.
Friedman’s test indicated significant differences between all observation times for marginal adaptation and surface roughness (p < 0.001). The marginal discoloration was observed for the Z250 (p = 0.007), and FBF (p = 0.018), remaining stable in the TBF group throughout the observation period. Differences within resin composites were only observed for the surface roughness at 12 and 36 months (p < 0.001). The TBF group showed a significantly higher percentage of Alpha scores at baseline, 12, and 36 months (95.7, 91.7, and 80.6%, respectively).
Table 6 shows the data regarding the esthetic properties of the restorations evaluated using the FDI criteria. No failures were observed. Friedman’s test indicated significant differences between observation times for gloss/roughness, surface and marginal staining, and anatomic form. However, differences within resin composites were only observed for gloss and anatomic form. TBF showed higher gloss and significant differences in anatomic form than the other two resin composites (p < 0.001).
No functional property failures were observed (Table 7). Significant differences were observed between observation times for marginal adaptation and the patient’s view (p < 0.001). One failure was attributed for the biological properties (Table 8) due to recurrent caries in one TBF restoration. However, no significant differences were found between resin composites or observation times. Postoperative sensitivity was self-reported after 24 h by two 16-year-old volunteers with Z250 restorations (tooth 47: 4-mm deep, GI lining/tooth 35: 3-mm, bonding), resulting in a 4.35% absolute risk. However, during clinical follow-up, both teeth exhibited normal response under clinical examination and cold vitality testing.
After 36 months of clinical follow-up, most restorations were classified as clinically acceptable, with the attribution of Alpha or Bravo scores (USPHS) or scores 1, 2, or 3 (FDI) for all categories analyzed. The survival rate of the restorations after 36 months was 94.44% for both evaluation methods. Two failures were observed in class I restorations with TBF, one at 12 months related to poor marginal adaptation (upper premolar) and the other at 36 months related to caries’ recurrence (upper molar). Thus, the annual failure rate of TBF restorations was 1.26%.
The USPHS and FDI criteria were compared using the Wilcoxon signed-rank test. Among all comparisons performed, differences were only found for surface roughness/gloss-surface roughness, marginal adaptation, and marginal staining/marginal discoloration (Tables 9, 10, and 11). The USPHS criteria scored most restorations as “acceptable” at 12 and 36 months, while the FDI criteria rated most restorations as “success.”
Discussion
The first hypothesis of this study that the materials’ clinical performance does not differ over the period studied was not rejected. No significant differences were found in the clinical performance of the materials tested. The result corroborates with the data from previous systematic reviews where bulk-fill resin composites have shown similar or superior performance than conventional resins in clinical trials [4, 28]. However, few clinical studies evaluating high-viscosity bulk-fill resin composites with a follow-up period longer than 24 months are available in the literature [11,12,13]. Studies with a follow-up period smaller than 3 years have been reported as of limited relevance, given that most materials do not fail within the first years. However, studies using a shorter observation period remain useful to exclude materials that result in early catastrophic failures [23].
Yazici et al. [11] compared the 36-month clinical performance of Tetric EvoCeram Bulk Fill to a conventional nanofiller resin composite (Filtek Ultimate, 3M ESPE). None of the 104 restorations performed was classified as a failure (Charlie). Loguercio et al. [12] also evaluated, for 36 months, 236 cavities restored with Tetric N-Ceram Bulk Fill placed by the incremental filling or bulk-fill technique using two bonding strategies (total acid etching and self-etching). Despite the observed minor fractures, marginal desadaptations, and color mismatch, all restorations were classified as clinically acceptable. The authors reported similar clinical performance of the studied groups. Heck et al. [13] evaluated restorations performed with QuiXfil (Dentsply) bulk-fill resin and conventional Tetric Ceram resin (Ivoclar Vivadent) in the most extensive clinical follow-up study of high-viscosity bulk-fill resin composites. After 10 years of clinical use, secondary caries and marginal discoloration were the main reasons for failures, followed by fractured teeth and restorations, postoperative sensitivity, and marginal integrity deterioration. The annual failure rate was stable over the years for the QuiXfil (2.5, 2.7, and 2.3% after 3, 4, and 10 years, respectively) and excellent Tetric Ceram (0.7, 0.6, and 1.3% after 3, 4, and 10 years, respectively).
Restorative failures can be classified as early, intermediate (6 to 24 months), and late failures (after 2 years or more of clinical use). Endodontic complications are the leading cause of intermediate failure [23]. Late failures are frequently caused by fracture of the tooth or restoration, secondary caries, or by wear or deterioration of the material [13]. Despite the higher number of deep cavities, no endodontic complications were observed in this study. The age of the studied population may have favored the maintenance of pulpal vitality. However, concerning postoperative sensitivity, the absolute risk for postoperative sensitivity observed in this study was 4.35% for incrementally filled restorations (Z250). Previous studies show a range of 3.85–18.6% absolute risk of postoperative sensitivity when bulk-fill resin composites were used in a self-etch adhesive strategy [30, 31]. The possibility of postoperative sensitivity occurring immediately after the restorative procedure is not exclusively related to the filling technique (incremental-fill or bulk-fill resin) or the bonding strategy [31]. Other factors that influence postoperative sensitivity risk must be considered, such as cavity size and complexity and the clinical setting in which the restorations are performed.
On the other hand, an early failure (before 24 months) was observed for marginal adaptation. At 36 months, many cases of minor marginal desadaptation were observed without compromising the clinical acceptability of the restorations [11]. A late failure (36-month) was observed regarding secondary caries. The recurrence of caries can be associated with patients neglecting oral hygiene and an increased caries risk [32, 33], or with defects at the restoration interface [34, 35]. The carious lesion in a restored tooth may also occur on a non-restored surface or even near the restoration margins [23]. In this study, caries’ failures were attributed whenever the carious lesion led to the restoration repair or replacement. Therefore, failure was attributed to one class I restoration with TBF repaired due to a primary proximal carious lesion that communicated with the restoration from underneath. On the other hand, failures resulting from new primary caries lesions are not necessarily related to the restoration’s quality [23]. For other authors, secondary caries should not be considered a failure of the material but rather to biological “failure” [36, 37].
Caries risk exerts a strong influence on the longevity of a restoration. A high/medium caries risk increases the chance of restoration failure by 2 to 3 times [38]. In a high caries risk population, the annual failure rate in 10 years was 4.6% versus 1.6% among low-risk patients [23]. Therefore, the “patient” factor is probably more critical for restorations’ longevity than factors related to the materials [23]. However, patients with a high incidence of caries and poor oral hygiene are excluded from most studies [4]. In some studies, teeth with secondary caries or those requiring replacement of existing restorations were also not included [11]. When individuals with these conditions were not excluded, failures resulting from secondary caries were associated with the patients’ high caries risk [32, 33].
Despite the differences in the caries risk assessment (CRA) method, the past caries experience is still the most powerful caries predictor in all age groups [34, 36, 37]. In this study, a high mean DMFT index was observed (9.44), with the decayed factor being the most significant component. This number is more than twice the national average (4.2) for the 15–19-year-old age group, obtained in the last national oral health census conducted in 2010 [39]. Moreover, social determinants are strongly associated with dental caries and influence restorations’ longevity [21]. The unfavorable socioeconomic status during life limits access to health services [40]. Restoration failures tend to be more prevalent among individuals who always belonged to poorer social classes of the population than those belonging to more privileged social classes [41].
Along with patient-related factors and socioeconomic characteristics, the restoration’s size also exerts a strong influence on its longevity. More extensive restorations with a larger amount of resin composite are more likely to fail. Each additional surface increases this risk by 30–40%. The risk of restoration failure is higher among molars than premolars [23]. In the present study, 70 of the 108 restorations evaluated over 36 months were molars. Despite the higher number of deep cavities at baseline observed for the bulk-fill resin composites, a small number of class II cavity restorations can be considered a limitation of this study (n = 22).
Other limitations can be related to the loss of follow-up. The low follow-up rate of long-term clinical studies is undoubtedly a significant limitation. Clinical trials take time to be completed, and volunteers may move during this process or often lose interest in returning for the reassessments [13]. This study was conducted in a university setting, and all volunteers received complete dental care according to their needs. We did not observe the previously described favorable scenario of more motivated volunteers with good oral health and low caries risk [12, 21, 42]. Even after complete dental care, oral health, and dental hygiene instructions, 34 new caries lesions were detected in 23 volunteers (63%) from 12-month to 36-month evaluation. The age of the studied population, consisting of young adolescents with low socioeconomic status, could have influenced this follow-up. Adolescents are a very vulnerable group as they no longer receive the care provided to children but, at the same time, have not yet reached the maturity of adults [43].
The university setting of this trial can also be considered a limitation. In universities, restorations are placed under ideal conditions to obtain the perfect outcomes possible. They are also performed by calibrated and experienced operators with in-depth knowledge of the techniques and materials and usually without time constraints for their completion. On the other hand, practice-based research better investigates the typical performance of a material [36].
The performance of the TBF resin in terms of gloss/surface roughness should be highlighted. The material provided a smooth and easily polishable restoration, with 80.6% of Alpha scores (USPHS). The inorganic composition of a material exerts a strong influence on finishing, smoothness, polishing quality, and gloss maintenance of the restorations [44, 45]. Filler particle analysis from SEM images showed that TBF had the smallest variation in-depth than other resin composites, including Z250 and FBF. TBF showed a subsurface layer of smaller fillers, with few agglomerates and larger particles [46].
Other differences in the composition of the materials should be considered to understand the clinical behavior of materials. Tetric EvoCeram Bulk Fill has, besides the tertiary camphorquinone-amine initiator, an additional germanium-based initiator called Ivocerin [47]. This photoinitiator absorbs light in the spectrum up to 455 nm, potentiating the depth of cure, degree of conversion, and, consequently, the material’s mechanical properties [6, 48]. Alternatively, the Filtek Bulk Fill contains a monomeric modification that allows its application in a single 5-mm increment [3, 44, 49, 50]. Its addition-fragmentation monomer (AFM) and aromatic urethane dimethacrylate (AUDMA) act as stress modulators, reducing polymerization stress and shrinkage [51]. Another added monomer is 1,12-dodecanodiol dimethacrylate (DDDMA), which confers low viscosity and hydrophobic properties, increasing molecular mobility and lowering stress polymerization [52]. The Filtek Z250 resin composite has the traditional Bis-GMA, UDMA, and Bis-EMA monomers that have shown good clinical results in longitudinal studies [27, 53].
A comparison of the evaluation criteria showed significant differences in three categories, rejecting the second hypothesis. Differences were found for marginal discoloration (USPHS)/marginal staining (FDI), marginal adaptation, and gloss-surface roughness (FDI)/surface roughness (USPHS). The FDI criteria obtained the most significant number of “success” responses, while the USPHS criteria received more responses classified as “acceptable.” The discrepancies observed between the evaluation criteria can be attributed to the differences in the criteria’s definition. While in the FDI criteria, score definitions change more “smoothly” due to the 5 score levels, in the USPHS, the differences between scores are more abrupt (3 score levels). The five score levels of the FDI criteria allow a more detailed evaluation of restorations in each category, better reflecting the restorations’ clinical success [54, 55]. However, most studies subcategorize the results into three (success/excellent, acceptable, and failure/unacceptable) or two levels (acceptable and unacceptable). Similarly, when assessing USPHS results, Alpha and Bravo scores are generally classified as clinically acceptable, and therefore, the restorations should be maintained without intervention [13]. Previous studies comparing the two evaluation methods in non-carious cervical lesions found differences for the staining [56] and marginal adaptation [56, 57] categories.
One of the FDI categories focuses on the patient (“patient’s view”), distinguishing this evaluation method from the USPHS criteria [55]. However, this category must be analyzed with caution because of its considerable subjectivity. When analyzing our results, we observed some lack of understanding by the participants, probably because of the studied population’s age. In the 12-month assessment, scores were distributed between scores 1 and 2 (50% each), whereas after 36 months, a 100% score 1 was obtained.
Clinical studies investigating complex cavities and potential patient-related risk factors such as high caries risk and bruxism should be conducted. Hence, there is a need for data that simulate situations observed in clinical practice to guide the decision-making process about the adoption or rejection of new material and techniques [40, 58]. Clinically, the incremental restoration technique leads to longer operative time and a higher risk of incorporating air bubbles between the increments. Less technically sensitive procedures and materials can reduce operator errors [59]. However, the shift from a widely used and reliable paradigm, such as the 2-mm incremental filling technique, to the use of single 4–5-mm increments still leaves clinicians feeling insecure [5].
Conclusions
The 36-month clinical performance of high-viscosity bulk-fill resin composites was comparable to that of the conventional incremental-fill resin composite in a high caries incidence population. For the corresponding categories between USPHS and FDI criteria, differences were found for surface roughness/gloss-surface roughness, marginal adaptation, and marginal staining/marginal discoloration. The FDI criteria obtained the most significant number of “success” responses and better presented the restorations’ clinical success. However, in the case of failure, both criteria provided the same results. Therefore, bulk-fill resin composites can be considered a simplified alternative restoration method.
References
De Andrade AKM, Duarte RM, Medeiros e Silva FDSC, et al (2014) Resin composite class I restorations: a 54-month randomized clinical trial. Oper Dent 39:588–594. https://doi.org/10.2341/14-067-C
Ferracane JL (2011) Resin composite - state of the art. Dent Mater 27:29–38. https://doi.org/10.1016/j.dental.2010.10.020
van Ende A, de Munck J, Lise DP, van Meerbeek B (2017) Bulk-fill composites: a review of the current literature. J Adhes Dent 19:95–109. https://doi.org/10.3290/j.jad.a38141
Veloso SRM, Lemos CAA, de Moraes SLD, do Egito Vasconcelos BC, Pellizzer EP, de Melo Monteiro GQ (2019) Clinical performance of bulk-fill and conventional resin composite restorations in posterior teeth: a systematic review and meta-analysis. Clin Oral Investig 23:221–233. https://doi.org/10.1007/s00784-018-2429-7
Boaro, Leticia Cristina Cidreira Lopes DP, de Souza ASC, Nakano EL, et al (2019) Clinical performance and chemical-physical properties of bulk fill composites resin —a systematic review and meta-analysis. Dent Mater 35:1–16. https://doi.org/10.1016/j.dental.2019.07.007
Ilie N (2019) Sufficiency of curing in high-viscosity bulk-fill resin composites with enhanced opacity. Clin Oral Investig 23:747–755. https://doi.org/10.1007/s00784-018-2482-2
Fronza BM, Ayres APA, Pacheco RR, Rueggeberg FA, Dias CTS, Giannini M (2017) Characterization of inorganic filler content, mechanical properties, and light transmission of bulk-fill resin composites. Oper Dent 42:445–455. https://doi.org/10.2341/16-024-L
Li X, Pongprueksa P, Van Meerbeek B, De Munck J (2015) Curing profile of bulk-fill resin-based composites. J Dent 43:664–672. https://doi.org/10.1016/j.jdent.2015.01.002
Chesterman J, Jowett A, Gallacher A, Nixon P (2017) Bulk-fill resin-based composite restorative materials: a review. Br Dent J 222:337–344. https://doi.org/10.1038/sj.bdj.2017.214
Rosa de Lacerda L, Bossardi M, Silveira Mitterhofer WJ, Galbiatti de Carvalho F, Carlo HL, Piva E, Münchow EA (2019) New generation bulk-fill resin composites: effects on mechanical strength and fracture reliability. J Mech Behav Biomed Mater 96:214–218. https://doi.org/10.1016/j.jmbbm.2019.04.046
Yazici AR, Antonson SA, Kutuk ZB, Ergin E (2017) Thirty-six-month clinical comparison of bulk fill and nanofill composite restorations. Oper Dent 42:478–485. https://doi.org/10.2341/16-220-C
Loguercio AD, Rezende M, Gutierrez MF, Costa TF, Armas-Vega A, Reis A (2019) Randomized 36-month follow-up of posterior bulk-filled resin composite restorations. J Dent 85:93–102. https://doi.org/10.1016/j.jdent.2019.05.018
Heck K, Manhart J, Hickel R, Diegritz C (2018) Clinical evaluation of the bulk fill composite QuiXfil in molar class I and II cavities: 10-year results of a RCT. Dent Mater 34:e138–e147. https://doi.org/10.1016/j.dental.2018.03.023
Ryge G (1980) Clinical criteria. Int Dent J 30:347–358
Cvar JF, Ryge G, Schmalz G (2005) Reprint of criteria for the clinical evaluation of dental restorative materials. Clin Oral Investig 9:7–24. https://doi.org/10.1007/s00784-005-0018-z
Hickel R, Roulet JF, Bayne S, Heintze SD, Mjör IA, Peters M, Rousson V, Randall R, Schmalz G, Tyas M, Vanherle G (2007) Recommendations for conducting controlled clinical studies of dental restorative materials. Clin Oral Investig 11:5–33. https://doi.org/10.1007/s00784-006-0095-7
Hickel R, Peschke A, Tyas M, Mjör I, Bayne S, Peters M, Hiller KA, Randall R, Vanherle G, Heintze SD (2010) FDI World Dental Federation: clinical criteria for the evaluation of direct and indirect restorations-update and clinical examples. Clin Oral Investig 14:349–366. https://doi.org/10.1007/s00784-010-0432-8
Da Rosa Rodolpho PA, Donassollo TA, Cenci MS et al (2011) 22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent Mater 27:955–963. https://doi.org/10.1016/j.dental.2011.06.001
Hafer M, Jentsch H, Haak R, Schneider H (2014) Clinical evaluation of a two-step etch-and-rinse adhesive and a one-step self-etch adhesive in non-carious cervical lesion. J Dent 46:58–61. https://doi.org/10.1016/j.jdent.2014.12.009
Coelho-De-Souza FH, Camargo JC, Beskow T et al (2012) A randomized double-blind clinical trial of posterior composite restorations with or without bevel: 1-year follow-up. J Appl Oral Sci 20:174–179. https://doi.org/10.1590/S1678-77572012000200009
Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJM (2012) Longevity of posterior composite restorations: not only a matter of materials. Dent Mater 28:87–101. https://doi.org/10.1016/j.dental.2011.09.003
Opdam NJM, Bronkhorst EM, Loomans BAC, Huysmans MCDNJM (2010) 12-year survival of composite vs. amalgam restorations. J Dent Res 89:1063–1067. https://doi.org/10.1177/0022034510376071
Opdam N, van de Sande F, Bronkhorst E et al (2014) Longevity of posterior composite restorations: a systematic review and meta-analysis. Artic J Dent Res 93:943–949. https://doi.org/10.1177/0022034514544217
Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG (2016) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Bmj 340:340–698. https://doi.org/10.1136/bmj.c869
Van Dijken JWV, Pallesen U (2014) A randomized controlled three year evaluation of bulk-filled posterior resin restorations based on stress decreasing resin technology. Dent Mater 30:e245–e251. https://doi.org/10.1016/j.dental.2014.05.028
de Durão MA, de Andrade AKM, do Carmo M, da Santos MS et al (2020) Clinical performance of bulk-fill resin composite restorations using the United States Public Health Service and Federation Dentaire Internationale Criteria: a 12-month randomized clinical trial. Eur J Dent. https://doi.org/10.1055/s-0040-1718639
De Andrade AKMI, Duarte RM, Medeiros E, Silva FDSC et al (2011) 30-Month randomised clinical trial to evaluate the clinical performance of a nanofill and a nanohybrid composite. J Dent 39:8–15. https://doi.org/10.1016/j.jdent.2010.09.005
Andrade A, Duarte R, Silva F, Batista AU, Lima KC, Pontual ML, Montes MA (2010) Efficacy of composites filled with nanoparticles in permanent molars: six-month results. Gen Dent 58:e190–e195
Borgia E, Baron R, Borgia JL (2019) Quality and survival of direct light-activated composite resin restorations in posterior teeth: a 5- to 20-year retrospective longitudinal study. J Prosthodont 28:e195–e203. https://doi.org/10.1111/jopr.12630
Costa T, Rezende M, Sakamoto A, Bittencourt B, Dalzochio P, Loguercio AD, Reis A (2017) Influence of adhesive type and placement technique on postoperative sensitivity in posterior composite restorations. Oper Dent 42:143–154. https://doi.org/10.2341/16-010-C
Tardem C, Albuquerque EG, De Souza LL et al (2019) Clinical time and postoperative sensitivity after use of bulk-fill (syringe and capsule) vs. incremental filling composites: a randomized clinical trial. Braz Oral Res 33:1–13. https://doi.org/10.1590/1807-3107BOR-2019.VOL33.0089
van Dijken JWV, Pallesen U (2016) Posterior bulk-filled resin composite restorations: a 5-year randomized controlled clinical study. J Dent 51:29–35. https://doi.org/10.1016/j.jdent.2016.05.008
van Dijken JWV, Pallesen U (2017) Bulk-filled posterior resin restorations based on stress-decreasing resin technology: a randomized, controlled 6-year evaluation. Eur J Oral Sci 125:303–309. https://doi.org/10.1111/eos.12351
Kim RJY, Kim YJ, Choi NS, Lee IB (2015) Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. J Dent 43:430–439. https://doi.org/10.1016/j.jdent.2015.02.002
Lynch CD, Opdam NJ, Hickel R, Brunton PA, Gurgan S, Kakaboura A, Shearer AC, Vanherle G, Wilson NH, Academy of Operative Dentistry European Section (2014) Guidance on posterior resin composites: Academy of Operative Dentistry - European Section. J Dent 42:377–383. https://doi.org/10.1016/j.jdent.2014.01.009
Reis A, Dourado Loguercio A, Schroeder M, Luque-Martinez I, Masterson D, Cople Maia L (2015) Does the adhesive strategy influence the post-operative sensitivity in adult patients with posterior resin composite restorations?: A systematic review and meta-analysis. Dent Mater 31:1052–1067. https://doi.org/10.1016/j.dental.2015.06.001
Nedeljkovic I, Teughels W, De Munck J et al (2015) Is secondary caries with composites a material-based problem? Dent Mater 31:e247–e277. https://doi.org/10.1016/j.dental.2015.09.001
Opdam NJM, Bronkhorst EM, Cenci MS, Huysmans MCDNJM, Wilson NHF (2011) Age of failed restorations: a deceptive longevity parameter. J Dent 39:225–230. https://doi.org/10.1016/j.jdent.2010.12.008
BRASIL (2010) SB Brasil 2010: Pesquisa Nacional de Saúde Bucal: resultados principais / Ministério da Saúde. Secretaria de Atenção à Saúde. Secretaria de Vigilância em Saúde. 116
Collares K, Opdam NJ, Peres KG, Peres MA, Horta BL, Demarco FF, Correa MB (2018) Higher experience of caries and lower income trajectory influence the quality of restorations: a multilevel analysis in a birth cohort. J Dent 68:79–84. https://doi.org/10.1016/j.jdent.2017.11.009
Correa MB, Peres MA, Peres KG, Horta BL, Barros AJ, Demarco FF (2013) Do socioeconomic determinants affect the quality of posterior dental restorations? A multilevel approach. J Dent 41:960–967. https://doi.org/10.1016/j.jdent.2013.02.010
Çolak H, Tokay U, Uzgur R et al (2017) A prospective, randomized, double-blind clinical trial of one nano-hybrid and one high-viscosity bulk-fill composite restorative systems in class II cavities: 12 months results. Niger J Clin Pract 20:822–831. https://doi.org/10.4103/1119-3077.212449
da Cumerlato CBF, Demarco FF, AJD B et al (2019) Reasons for direct restoration failure from childhood to adolescence: a birth cohort study. J Dent 89:103183. https://doi.org/10.1016/j.jdent.2019.103183
Flury S, Peutzfeldt A, Lussi A (2014) Influence of increment thickness on microhardness and dentin bond strength of bulk fill resin composites. Dent Mater 30:1104–1112. https://doi.org/10.1016/j.dental.2014.07.001
Kim K-H, Ong JL, Okuno O (2002) The effect of filler loading and morphology on the mechanical properties of contemporary composites. J Prosthet Dent 87:642–649. https://doi.org/10.1067/mpr.2002.125179
de Giovanna F, da Costa A, dos Santos Melo AM, de Assunção IV, BCD B (2019) Impact of additional polishing method on physical, micromorphological, and microtopographical properties of conventional composites and bulk fill. Microsc Res Tech 83:1–12. https://doi.org/10.1002/jemt.23404
Moszner N, Fischer UK, Ganster B, Liska R, Rheinberger V (2008) Benzoyl germanium derivatives as novel visible light photoinitiators for dental materials. Dent Mater 24:901–907. https://doi.org/10.1016/j.dental.2007.11.004
Flury S, Hayoz S, Peutzfeldt A, Hüsler J, Lussi A (2012) Depth of cure of resin composites: is the ISO 4049 method suitable for bulk fill materials? Dent Mater 28:521–528. https://doi.org/10.1016/j.dental.2012.02.002
Ilie N, Schöner C, Bücher K, Hickel R (2014) An in-vitro assessment of the shear bond strength of bulk-fill resin composites to permanent and deciduous teeth. J Dent 42:850–855. https://doi.org/10.1016/j.jdent.2014.03.013
Hirata R, Kabbach W, De Andrade OS et al (2015) Bulk fill composites: an anatomic sculpting technique. J Esthet Restor Dent 27:335–343. https://doi.org/10.1111/jerd.12159
3M (2014) Filtek Bulk Fill. 3M Espe 2–24. https://doi.org/10.1109/TPEL.2012.2189588
Kamalak H, Kamalak A (2018) Evaluation of polymerization shrinkage of dental composites by microcomputed tomography. Biomed Res 29:844–852
Lempel E, Tóth Á, Fábián T, Krajczár K, Szalma J (2015) Retrospective evaluation of posterior direct composite restorations: 10-year findings. Dent Mater 31:115–122. https://doi.org/10.1016/j.dental.2014.11.001
Göstemeyer G, Blunck U, Paris S, Schwendicke F (2016) Design and validity of randomized controlled dental restorative trials. Materials (Basel) 9:372. https://doi.org/10.3390/ma9050372
Marquillier T, Doméjean S, Le Clerc J et al (2018) The use of FDI criteria in clinical trials on direct dental restorations: a scoping review. J Dent 68:1–9. https://doi.org/10.1016/j.jdent.2017.10.007
Loguercio AD, De Paula EA, Hass V et al (2015) A new universal simplified adhesive: 36-month randomized double-blind clinical trial. J Dent 43:1083–1092. https://doi.org/10.1016/j.jdent.2015.07.005
Perdigão J, Kose C, Mena-Serrano AP, de Paula EA, Tay LY, Reis A, Loguercio AD (2014) A new universal simplified adhesive: 18-month clinical evaluation. Oper Dent 39:113–127. https://doi.org/10.2341/13-045-C
Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G (2002) Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res 81:459–463. https://doi.org/10.1177/154405910208100705
Demarco FF, Collares K, Correa MB et al (2017) CritiCal review dental materials/dentistry should my composite restorations last forever? Why are they failing? Braz Oral Res 31:92–99. https://doi.org/10.1590/1807-3107BOR-2017.vol31.0056
Funding
This work was carried out with the Higher Education Personnel Improvement Coordination support - Brazil (CAPES) - Financing Code 001, Pernambuco State Science and Technology Support Foundation (FACEPE).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Ethics Committee on Research Involving Humans of the University of Pernambuco, Brazil (Protocol No. 944.518).
Informed consent
All patients participated voluntarily, and the adolescents and their legal representatives signed the free, informed consent form.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Durão, M.d., de Andrade, A.K.M., do Prado, A.M. et al. Thirty-six-month clinical evaluation of posterior high-viscosity bulk-fill resin composite restorations in a high caries incidence population: interim results of a randomized clinical trial. Clin Oral Invest 25, 6219–6237 (2021). https://doi.org/10.1007/s00784-021-03921-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03921-9