Abstract
Objectives
This study aims to compare the performance of a bulk-fill and a nanofill resin composite in class II restorations after 6 years.
Materials and methods
Fifty patients having at least two class II carious lesions were recruited for the study. One lesion in each patient was randomly assigned to be restored using either the Tetric EvoCeram Bulk Fill (TB) or Filtek Ultimate (FU) resin composites with their respective adhesives. One hundred four restorations were placed by two calibrated operators. Restorations were evaluated at baseline and annually over the course of 6 years by two examiners using modified USPHS criteria. Data were statistically analyzed using the Chi-square and Cochran Q tests (p < 0.05).
Results
Sixty-six restorations in 33 patients were evaluated after 6 years. Only one restoration was lost from FU group at 5 years. At the end of 6 years, marginal discoloration was observed in three (9.1%) TB and eight (36.4%) FU restorations creating a significant difference between the groups (p < 0.05). The FU group showed a significant increase in marginal discoloration at 6 years from the baseline (p < 0.05). Marginal adaptation was rated as Bravo for 9.1% and 24.2% of TB and FU restorations, respectively (p > 0.05). Significant degradation was observed within each group in terms of marginal adaptation (p < 0.05). There were no statistically significant differences between the groups for the other criteria tested (p > 0.05).
Conclusions
Bulk-fill restorations performed better for marginal discoloration. The remaining clinical performance criteria of bulk-fill and nanofill resin composite restorations were similar after 6 years.
Clinical relevance
Bulk-fill resin might be a better alternative to incrementally placed restorative in terms of marginal discoloration under clinical conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tooth-colored restorative materials have become increasingly more desirable for posterior restorations. Despite the improvements in resin-based materials’ technology, the restoration of posterior teeth with direct methods still presents a challenge for clinicians. Therefore, the bulk-fill resin composites have attracted much attention as an alternative to incrementally placed composites, presenting several clinical benefits. First of all, the use of a bulk-fill resin composite requires shorter time to complete restorations in posterior teeth than conventional resins placed incrementally [1,2,3]. The risk for contamination between the increments and air bubble incorporation that results with void formation is also decreased [4, 5]. Furthermore, the translucency of some of the bulk-fill resins is higher as their filler loading was lowered while filler size was increased. This specification enables light penetration to deeper preparations and therefore facilitates improved depth of cure [3, 6]. Another important feature of some of the bulk-fill resin is their reduced polymerization shrinkage due to the addition of specific monomers, pre-polymerized fillers, and photoinitiators in their composition [7,8,9].
Current bulk-fill resin composites can be classified as high viscosity and low viscosity. While bulk-fill resins with higher viscosity are used as regular restorative materials, the low-viscosity bulk-fill resins are used in the proximal and internal part of the preparations as a base layer or a dentin replacement material. The low-viscosity bulk-fill resin composites require a capping layer made of a conventional resin composite due to their inferior physical and mechanical properties [10]. In a few short-term trials that compares the clinical behavior of high- and low-viscosity bulk-fill resin restorations, similar outcomes were reported [11, 12].
Clinical evaluations demonstrated that bulk-fill resin composites could also be a promising alternative to incrementally placed resin composites [11, 13,14,15,16,17,18]. However, this statement still needs to be validated as most of them are short-term clinical studies. To the extent of the authors’ knowledge, there are only few long-term clinical published data available regarding the longevity and performance of bulk-fill resins in the literature [19,20,21]. Additionally, because of the fact that many of the bulk-fill resin composites’ composition and the polymerization strategy is significantly different, it is impossible to make a generalized statement for their clinical performance.
Due to the limitation of the current evidence, it is difficult to speculate that bulk-fill resin composites are superior to traditional resin composites due to the insufficient and limited controlled studies. Our previous clinical trial was also one of the first studies that compared high-viscosity bulk-fill resin with a conventional layered resin in class II restorations up to 36 months [22]. As the performance of restorative materials might change over long periods under clinical circumstances related to the patients’ habits, diet, masticatory forces, and also deterioration of the restorative material itself, the aim of this extended clinical study was to compare the clinical performance of a high-viscosity bulk-fill resin composite with a nanofill resin composite for 6 years.
The null hypothesis was that there would be no difference between the clinical performance of the tested bulk-fill and incrementally placed resin composite restorations after 6 years of clinical service.
Materials and methods
This randomized controlled clinical trial was conducted following the CONSORT statement [23]. The study was approved by the Ethics in Human Research Committee of the University (#04KA-15004) and registered in ClinicalTrials.gov under protocol number NCT04320576.
All participants were informed about the purpose and nature of the study, and written consent forms were obtained prior to enrollment in the study.
Recruitment and eligibility
Fifty patients including 24 males and 26 females (mean age, 22; range, 24–55 years old) who had at least two similar-sized primary approximal lesions in their premolar/molar teeth and required class II restorations were included in this study.
Inclusion and exclusion criteria
Subjects had to be in good general and oral health without any deleterious habits. They had to present at least twenty teeth under occlusion. The remaining teeth had to be vital and sound without any caries or existing restoration. Subjects with a compromised medical history and poor oral hygiene/periodontal health were not included. Subjects with known allergies to the test materials, pregnant or lactating woman, and those potentially unable to attend recall visits were also excluded from participating.
Sample size calculation
A sample size calculation was performed with power analysis using an alpha of 0.05 and 80% power. Thus, the minimum sample size in this study was 40 restorations. However, the sample size was increased to compensate potential loss and drop-outs.
Study design
The randomization process was performed by a statistician from the Biostatistics Department of the Medical School who was not involved in the research protocol. The teeth were randomized for each of the two restorative treatments through a table of random numbers generated by the program “Research Randomized Program” (http://www.randomizer.org/form.htm). A randomization number was assigned to each patient. Then, restorative material was determined according to odd or even numbers in the table. If the number assigned was an even number, then the bulk-fill restorative material was used first or vice versa. Both restorative materials were placed in order by which the first assigned to restore the tooth with the lower tooth number (according to the FDI system), while the tooth with the next number received the other restorative material.
In accordance to allocation concealment, the randomization lists were kept in numbered sealed opaque envelopes. Corresponding envelopes were opened just before intervention. The operator performed a similar number of restorations for both groups. Each patient received at least two restorations, one from each of study groups. There was only one patient who had four lesions which were restored following the same randomization procedure. The operator was not blinded to group assignment when administering interventions. Neither the patients nor the examiners knew which type of resin composite was placed in each tooth, thus resulting in a double-blind study.
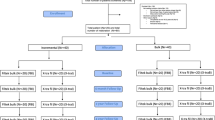
The flow chart of the study is displayed in Fig. 1.
Restorative procedures
Class II slot preparations were performed with a water-cooled high-speed handpiece using a flat end straight and round diamond burs (Diatech, Heerbrugg, Switzerland). The preparation was limited to that required for carious tissue access. Excessive removal of sound tooth tissue was avoided. All of the preparation margins were on sound enamel. Round steel burs in a slow-speed handpiece were used to excavate carious lesions. The caries extension guided the preparation size, and the tissue removal was ended when the dentin was hard on probing.
For each subject, at least two different restorative resin composites were placed in random, resulting in a total of 104 restorations. One of the two preparations was restored using the bulk-fill resin composite, Tetric EvoCeram Bulk Fill (TB, Ivoclar Vivadent, Schaan, Liechtenstein) (n = 52), and the other was restored with Filtek Ultimate (FU, 3 M ESPE, St Paul, MN, USA) (n = 52). The etch-and-rinse adhesive procedures were performed according to the manufacturers’ instructions for the respective resin composite as outlined in Table 1.
All restorations were placed under rubber dam (Optradam, Ivoclar Vivadent, Schaan, Lichtenstein) isolation. A sectional matrix system (Ivory #1, MEBA—Schwer GmbH & Co. KG, Denkingen, Germany) was used with wedging to create optimum adaptation. The restorative material Filtek Ultimate was inserted using an incremental layering technique not exceeding 2 mm in thickness. A minimum of two increments were placed, and each was cured with an LED (Starlight Mectron s.p.a., Carasco, Italy, output = 1400 mW/cm2) for 20 s. The intensity of the light was monitored regularly by a radiometer designed for LED (Demetron, Danbury, CT, USA). The bulk-fill restorative material, TB, was placed with a thickness of 4 mm and polymerized for 20 s with the same LED. Excess cured resin was removed, and the occlusion was adjusted using finishing diamond burs (Diatech, Heerbrugg, Switzerland).
Finishing and polishing were accomplished using aluminum oxide disks of decreasing abrasiveness (Sof-Lex, 3 M ESPE) and rubber tips (Kerr Corp, Orange, CA, USA) with slow-speed handpiece. A single experienced operator carried out all of the preparations and restorations.
Clinical evaluation
Restorations were evaluated by two previously calibrated and experienced dentists, who were unaware of which restorative material had been used. The overall kappa statistics with a value of 95% for each criterion showed excellent agreement between the evaluators. The evaluations were made at baseline, annually, and after 6 years in accordance with the modified USPHS criteria [24].
To assess the occurrence of postoperative sensitivity, 2 methods were used: (i) by applying compressed air for 3 s at a distance of 2–3 cm from the tooth surface and (ii) by moving the probe over the restored tooth surface. It was scored as present or absent according to the patients’ feedback. Clinical photographs at 1:1 magnification was taken pre- and postoperatively, at baseline, and each recall appointments. In case of any discrepancy during evaluation, a consensus was reached with the aid of photographic assessment. Bitewing radiographs were also taken annually.
Statistical analysis
The statistical analyses were carried out with the IBM SPSS version 22.0 software package (SPSS, Chicago, IL, USA). The comparison of two restorative materials for each category was analyzed using the Pearson Chi-square test. Cochran Q-test was used to compare the changes across the five time points (baseline, 3, 4, 5, and 6 years) (p < 0.05). The significance level was set at 5%.
Results
In total, 104 restorations were placed in 50 patients. At the end of 6 years, the recall rate was 66% with a total of 66 evaluated restorations. Most of the drop-outs were due to relocation to other cities or unavailability to reach them with the phone numbers that were provided.
From TB group, one restoration at 4-year recall and one in 5-year recall received crowns. While TB had 100% retention rate, one failure resulting from total retention loss occurred in FU group at 5-year recall. There was no significant difference among groups for retention (p > 0.05). Table 2 presents data for marginal discoloration, marginal adaptation, color match, and surface texture.
In terms of marginal discoloration, a significant difference was detected between the two groups at the end of 6 years (p = 0.009). Three restorations from TB and 12 from FU showed slight marginal discoloration at the enamel margins. Representative images of TB and FU restorations from the same patient at baseline, 3- and 6-year recalls are presented in Fig. 2. FU restoration shows an increase in marginal discoloration over time.
At the end of 6 years, localized marginal defects and minor discrepancies were observed in 9.1% and 24.2% of the TB and FU restorations, respectively, creating no statistically significant difference between the groups for marginal adaptation (p = 0.186).
Comparing the groups with respect to color match (p = 1.000) and surface texture (p = 0.613), no statistically significant difference was observed at 6-year recall.
The comparison of restoration performance with time (baseline vs 6-year data) in terms of marginal adaptation yielded a significant shift of alpha scores to bravo, indicating a deterioration of marginal adaptation for both TB (p = 0.008) and FU restorations (p = 0.000).
Significant differences in relation to marginal discoloration were detected between the baseline and 6 years for only FU group (p = 0.000). No significant difference was found within each group when baseline and 6-year data were compared in terms of color match (p > 0.05). At the end of 6 years, only 2 from TB and 3 from FU restorations showed slight mismatch. Representative images of both restorations from another patient at baseline, 3-, and 6-year recalls are presented in Fig. 3a–f. While TB restoration (#46) received alpha score in terms of color match at each time point (Fig. 3a–c), there was a trend toward increased mismatch in the FU restoration (#16) at 3- and 6-year recall (Fig. 3d–e).
None of the restored teeth showed caries recurrence, and the vitality was maintained throughout the study. The postoperative sensitivity was absent in all patients at 6-year recall.
For the surface texture, only 1 restoration from TB and 3 from FU showed slight roughness at the end of 6 years. Compared to baseline values, this change caused significant difference only in FU group (p < 0.05).
Discussion
The choice of an appropriate material is a crucial factor for the success of restorative treatment. In the present study, two different generations of resin composites were compared, and the results demonstrated that there was no difference between the two resin composites except for marginal discoloration. Therefore, the null hypothesis that there would be no difference in the clinical performance between bulk and incrementally placed resin composites was partially accepted.
Recently published clinical performance of bulk-fill resin composites reported annual failure rates between 1.0 and 2.3% for 6- and 10-year evaluations, respectively [20, 21]. Higher retention rates observed in both restorative resin groups in the current study might be attributed to the use of etch-and-rinse adhesive. Etch-and-rinse adhesives generally create clinically acceptable bond strengths that can withstand masticatory stress. It is difficult to speculate about a possible reason for the retention loss of only one restoration from FU group as the lesion characteristics and tooth distribution were similar for both groups. The reason could be attributed to patient’s parafunctional habits, even though this was not clinically diagnosed. However, patients with heavy bruxism were not included in the study. Nevertheless, this was a long follow-up clinical trial, and patients’ circumstances and behavior might have been changed. On the other hand, the reason for retention loss might not be attributed only to the occlusion, other systemic or behavioral components should also be taken into account. The similarity in retention rates of bulk and incrementally placed resin composites is also supported by the results of several clinical studies [19,20,21,22, 25].
Marginal discoloration was the only criteria that showed significant differences between the restorative groups at all evaluation periods after 24 months. The bond degradation and failures are generally reflected by marginal discoloration and marginal defects under clinical conditions. It is known that marginal discoloration is one of the deleterious effects of polymerization shrinkage of resin composites. The stress generated on resin/tooth interface might cause a failure on sealing of margins and gaps, thereby accumulation of food colorants, etc. The lack of staining at the margins of 90% of TB restorations at 6 years might be related with some modifications that has been adapted in the monomer phase of TB, which leads a reduction of polymerization shrinkage. This resin has a germanium-based photoinitiator called Ivocerin that has higher absorption coefficient than camphorquinone [26, 27]. Furthermore, the presence of pre-polymerized particles might have contributed to low polymerization shrinkage values. Polymerization stress reliever is another unique component of this material [27]. The absence of low-molecular-weight monomers like TEGDMA in the composition of TB, which is different from FU, might also lower shrinkage stress and contribute less marginal discoloration.
In a 24-month clinical study, three different types of bulk-fill resin composites were compared in class II preparations, Tetric EvoCeram Bulk Fill, SureFil SDR flow + Ceram.X Mono (n = 40), and everX Posterior + G-ænial Posterior. At the end of 2 years, none of the restorations in Tetric EvoCeram Bulk Fill group showed marginal discoloration, while slight discoloration was observed in the rest of the materials without causing any significant difference among them [12]. Likewise, in our previously published paper that shows 3-year results, no marginal discoloration was detected in any of the Tetric EvoCeram Bulk Fill restorations up to 24-month recall. Balkaya and Arslan [18] compared three restorative materials: a high-viscosity glass ionomer, a bulk-fill, and a microhybrid resin composites in class II restorations up to 24 months. They also found no difference between bulk or incrementally placed resin composite in terms of marginal discoloration and adaptation.
The tooth-resin interface integrity could be assumed as the most crucial factor determining the clinical success of restorations [28]. An important consequence of polymerization shrinkage is the potential of tooth-resin interface failure. The marginal gap formation occurs when bond strength between restoration and tooth structure cannot withstand the polymerization shrinkage forces. In most of the in vitro studies, the marginal adaptation of bulk-fill resin composites was found to be similar with incrementally placed resins [29,30,31,32]. In the present study, although incrementally placed resin composite, FU resulted in higher cases of marginal discrepancies (24.2%); the difference in marginal adaptation between the groups was not of statistically significance. The relatively better marginal adaptation of TB restorations (9.1 percent receiving Bravo) could be related with lower elastic modulus of TB, despite both restorative resins have similar number of fillers (78–82 wt%). TB contains pre-polymerized fillers that result in a reduced elastic modulus [33, 34]. It is known that resin composites that have pre-polymerized fillers in their composition usually demonstrate low elasticity modulus [34]. Tetric Bulk Fill and Filtek Ultimate have linear shrinkage values of 11.57 and 11.13, respectively [33]. There is only a minor difference between them. TB has some specific fillers functionalized with saline that act as a shrinkage stress reliever in its composition [27, 35]. However, many other variables could influence the marginal adaptation not solely polymerization shrinkage. Although not statistically different, TB revealed a higher percentage of alpha ratings in terms of marginal adaptation that could also be related with the used adhesive system. Although an etch-and-rinse adhesive system was used for both restoratives, the promising efficiency of Adper Single Bond 2 which was reflected by higher continuous margins might be another contributing factor for obtaining better results with TB restorations. This adhesive contains the polyalkenoic acid (Vitrebond copolymer) that has the ability to bond chemically with calcium in hydroxyapatite in dentin and might contribute better bond durability [36].
When we examined our previous published 36-month data, the difference in terms of marginal adaptation was found to be statistically significant showing superior results for TB. Clinical outcomes might change over time. Therefore, longer follow-up periods should be taken into consideration to determine a final conclusion. Marginal adaptation showed the most significant changes with time for both restorative materials, showing a statistically significant difference after 6 years when compared with the baseline data.
Two restorations from TB and 3 from FU group received bravo scores in terms of color match. The color mismatch of two restorations with the adjacent tooth structure from the same patient might have developed due to the patient nutrition and oral hygiene habits rather than the restorative material.
There was only 1 restoration from TB and 3 from FU group rated as bravo at the end of 6 years for surface texture. All of these restorations’ surfaces were slightly rough that can be repolished.
It has been stated that secondary caries is one of the primary reasons for the failure of the restorations [21, 37]. In most of the longer follow-up studies, secondary caries occurrence was observed after four to 6 years of clinical service in resin composites [21, 38, 39]. Despite this evidence, none of the restorations failed due to secondary caries in the present study, even after 6 years of clinical service. This could be related to the precise placement technique of the clinician, inclusion of patients with adequate oral hygiene, and also improvements in the adhesive systems and restorative materials. Only one failure was observed in this study, and this was the total retention loss of one restoration from FU group that was discussed previously.
In our study, none of the patients from either group suffered from postoperative sensitivity. It was not an unexpected result as most of the studies reported either no occurrence of postoperative sensitivity in restored teeth or no differences in postoperative sensitivity between bulk-fill and conventional resins [11, 18, 40, 41]. However, one study argued that the lack of postoperative sensitivity resulted from the placement of liners in deep and very deep cavities [11]. Another study observed postoperative sensitivity after 12 months in only one tooth of all those restored with bulk-fill with sonic activation, attributing this to the lack of calcium hydroxide liner in the deep cavity [40]. The depth and the extension of the cavity are factors that can influence postoperative sensitivity. That’s why in the present study, the depth of the lesions was quite similar. Moreover, as the cavity preparations were in middle dentin most of the time, no liners were placed to the preparations. Additionally, adequate depth of cure of the bulk-fill resin used in the present study might have contributed to the lack of difference with incrementally placed resin composite.
Heck et al. [21] compared the clinical performance of a bulk-fill resin, Quixfil, with that of a hybrid resin composite, Tetric Ceram, in class I and II preparations in molar teeth. At the end of 10 years, the overall success rate (76.9%) was found to be quite well with no significant difference between the materials. Previous clinical studies with shorter follow-up periods than this present study have also shown similar results confirming that no difference exists between these resin composites [11, 15, 18].
Our results are in line with a recent systematic review and meta-analysis that showed similar clinical performances of bulk-fill and conventional resin composites over a follow-up period of 12 to 72 months [42]. In another meta-analysis of clinical and laboratory studies comparing these restorative resins, the same results were obtained during 1 to 10 years of follow-ups [43].
Recently, Arbildo-Vega et al. [25] performed a systematic review and meta-analysis similar to reviews mentioned above. They came to the same conclusion that clinical effectiveness of bulk-fill resin and incrementally placed conventional resin composites were comparable.
The results of the present study cannot be generalized to other bulk-fill resins as only one type of resin composite was selected and tested. Further long-term studies should be carried out using different bulk-fill resin composites as well as in other types of cavities, to support these findings.
Conclusion
Within the limitations of this clinical study, bulk-fill (Tetric EvoCeram Bulk Fill) and incrementally placed (Filtek Ultimate) restorations presented similar clinical performance with the exception of marginal discoloration criteria where better results were observed with bulk-fill resin restorations after 6 years.
References
Bellinaso MD, Soares FZM, Rocha RO (2019) Do bulk-fill resins decrease the restorative time in posterior teeth? A systematic review and meta-analysis of in vitro studies. J Investig Clin Dent 10(4):e12463. https://doi.org/10.1111/jicd.12463
Vianna-de-Pinho MG, Rego GF, Vidal ML, Alonso RCB, Schneider LFJ, Cavalcante LM (2017) Clinical time required and internal adaptation in cavities restored with bulk-fill composites. J Contemp Dent Pract 18(12):1107–1111. https://doi.org/10.5005/jp-journals-10024-2184
Ilie N, Bucuta S, Draenert M (2013) Bulk-fill resin-based composites: an in vitro assessment of their mechanical performance. Oper Dent 38(6):618–625. https://doi.org/10.2341/12-395-L
Soares CJ, Rosatto C, Carvalho VF, Bicalho AA, Henriques J, Faria ESAL (2017) Radiopacity and porosity of bulk-fill and conventional composite posterior restorations-digital x-ray analysis. Oper Dent 42(6):616–625. https://doi.org/10.2341/16-146-L
Demirel G, Orhan AI, Irmak O, Aydin F, Buyuksungur A, Bilecenoğlu B, Orhan K (2020) Micro-computed tomographic evaluation of the effects of pre-heating and sonic delivery on the internal void formation of bulk-fill composites. Dent Mater J. https://doi.org/10.4012/dmj.2020-071
Van Ende A, De Munck J, Lise DP, Van Meerbeek B (2017) Bulk-fill composites: a review of the current literature. J Adhes Dent 19(2):95–109. https://doi.org/10.3290/j.jad.a38141
Fronza BM, Rueggeberg FA, Braga RR, Mogilevych B, Soares LE, Martin AA, Ambrosano G, Giannini M (2015) Monomer conversion, microhardness, internal marginal adaptation, and shrinkage stress of bulk-fill resin composites. Dent Mater 31(12):1542–1551. https://doi.org/10.1016/j.dental.2015.10.001
Martins LC, Oliveira LRS, Braga SSL, Soares CJ, Versluis A, Borges GA, Verissimo C (2020) Effect of composite resin and restorative technique on polymerization shrinkage stress, cuspal strain and fracture load of weakened premolars. J Adhes Dent 22(5):503–514. https://doi.org/10.3290/j.jad.a45180
Lins RBE, Aristilde S, Osorio JH, Cordeiro CMB, Yanikian CRF, Bicalho AA, Stape THS, Soares CJ, Martins LRM (2019) Biomechanical behaviour of bulk-fill resin composites in class II restorations. J Mech Behav Biomed Mater 98:255–261. https://doi.org/10.1016/j.jmbbm.2019.06.032
Fugolin APP, Pfeifer CS (2017) New resins for dental composites. J Dent Res 96(10):1085–1091. https://doi.org/10.1177/0022034517720658
Colak H, Tokay U, Uzgur R, Hamidi MM, Ercan E (2017) A prospective, randomized, double-blind clinical trial of one nano-hybrid and one high-viscosity bulk-fill composite restorative systems in class II cavities: 12 months results. Niger J Clin Pract 20(7):822–831. https://doi.org/10.4103/1119-3077.212449
Guney T, Yazici AR (2020) 24-month clinical evaluation of different bulk-fill restorative resins in class II restorations. Oper Dent 45(2):123–133. https://doi.org/10.2341/18-144-C
Oter B, Deniz K, Cehreli SB (2018) Preliminary data on clinical performance of bulk-fill restorations in primary molars. Niger J Clin Pract 21(11):1484–1491. https://doi.org/10.4103/njcp.njcp_151_18
Canali GD, Ignacio SA, Rached RN, Souza EM (2019) One-year clinical evaluation of bulk-fill flowable vs. regular nanofilled composite in non-carious cervical lesions. Clin Oral Investig 23(2):889–897. https://doi.org/10.1007/s00784-018-2509-8
Bayraktar Y, Ercan E, Hamidi MM, Colak H (2017) One-year clinical evaluation of different types of bulk-fill composites. J Investig Clin Dent 8(2). https://doi.org/10.1111/jicd.12210
Balkaya H, Arslan S, Pala K (2019) A randomized, prospective clinical study evaluating effectiveness of a bulk-fill composite resin, a conventional composite resin and a reinforced glass ionomer in class II cavities: one-year results. J Appl Oral Sci 27:e20180678. https://doi.org/10.1590/1678-7757-2018-0678
Berti LS, Turssi CP, Amaral FL, Basting RT, Junqueira JLC, Panzarella FK, Reis AF, Franca FM (2020) Clinical and radiographic evaluation of high viscosity bulk-fill resin composite restorations. Am J Dent 33(4):213–217
Balkaya H, Arslan S (2020) A two-year clinical comparison of three different restorative materials in class II cavities. Oper Dent 45(1):E32–E42. https://doi.org/10.2341/19-078-C
Manhart J, Chen HY, Hickel R (2010) Clinical evaluation of the posterior composite Quixfil in class I and II cavities: 4-year follow-up of a randomized controlled trial. J Adhes Dent 12(3):237–243. https://doi.org/10.3290/j.jad.a17551
van Dijken JWV, Pallesen U (2017) Bulk-filled posterior resin restorations based on stress-decreasing resin technology: a randomized, controlled 6-year evaluation. Eur J Oral Sci 125(4):303–309. https://doi.org/10.1111/eos.12351
Heck K, Manhart J, Hickel R, Diegritz C (2018) Clinical evaluation of the bulk fill composite QuiXfil in molar class I and II cavities: 10-year results of a RCT. Dent Mater 34(6):e138–e147. https://doi.org/10.1016/j.dental.2018.03.023
Yazici AR, Antonson SA, Kutuk ZB, Ergin E (2017) Thirty-six-month clinical comparison of bulk fill and nanofill composite restorations. Oper Dent 42(5):478–485. https://doi.org/10.2341/16-220-C
Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, Gotzsche PC, Lang T, Consort G (2001) The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 134(8):663–694. https://doi.org/10.7326/0003-4819-134-8-200104170-00012
Cvar JF (1971) Ryge G (2005) Reprint of criteria for the clinical evaluation of dental restorative materials. Clin Oral Investig 9(4):215–232. https://doi.org/10.1007/s00784-005-0018-z
Arbildo-Vega HI, Lapinska B, Panda S, Lamas-Lara C, Khan AS, Lukomska-Szymanska M (2020) Clinical effectiveness of bulk-fill and conventional resin composite restorations: systematic review and meta-analysis. Polymers (Basel) 12(8):1786. https://doi.org/10.3390/polym12081786
Moszner N, Fischer UK, Ganster B, Liska R, Rheinberger V (2008) Benzoyl germanium derivatives as novel visible light photoinitiators for dental materials. Dent Mater 24(7):901–907. https://doi.org/10.1016/j.dental.2007.11.004
Scientific documentation of Tetric EvoCeram Bulk Fill. Retrieved online March 04, 2016 from http://www.ivoclarvivadent.com
Haak R, Schmidt P, Park KJ, Hafer M, Krause F, Ziebolz D, Schneider H (2018) OCT for early quality evaluation of tooth-composite bond in clinical trials. J Dent 76:46–51. https://doi.org/10.1016/j.jdent.2018.06.007
Al-Harbi F, Kaisarly D, Bader D, El Gezawi M (2016) Marginal integrity of bulk versus incremental fill class ii composite restorations. Oper Dent 41(2):146–156. https://doi.org/10.2341/14-306-L
Campos EA, Ardu S, Lefever D, Jasse FF, Bortolotto T, Krejci I (2014) Marginal adaptation of class II cavities restored with bulk-fill composites. J Dent 42(5):575–581. https://doi.org/10.1016/j.jdent.2014.02.007
de Assis FS, Lima SN, Tonetto MR, Bhandi SH, Pinto SC, Malaquias P, Loguercio AD, Bandeca MC (2016) Evaluation of bond strength, marginal integrity, and fracture strength of bulk- vs incrementally-filled restorations. J Adhes Dent 18(4):317–323. https://doi.org/10.3290/j.jad.a36516
Furness A, Tadros MY, Looney SW, Rueggeberg FA (2014) Effect of bulk/incremental fill on internal gap formation of bulk-fill composites. J Dent 42(4):439–449. https://doi.org/10.1016/j.jdent.2014.01.005
Jang JH, Park SH, Hwang IN (2015) Polymerization shrinkage and depth of cure of bulk-fill resin composites and highly filled flowable resin. Oper Dent 40(2):172–180. https://doi.org/10.2341/13-307-L
Blackham JT, Vandewalle KS, Lien W (2009) Properties of hybrid resin composite systems containing prepolymerized filler particles. Oper Dent 34(6):697–702. https://doi.org/10.2341/08-118-L
Manhart J, Hickel R (2014) Bulk-fill-composites. Modern application technique of direct composites for posterior teeth. Swiss Dent J 124(1):19–37
Sezinando A, Perdigao J, Ceballos L (2017) Long-term in vitro adhesion of polyalkenoate-based adhesives to dentin. J Adhes Dent 19(4):305–316. https://doi.org/10.3290/j.jad.a38895
Demarco FF, Correa MB, Cenci MS, Moraes RR, Opdam NJ (2012) Longevity of posterior composite restorations: not only a matter of materials. Dent Mater 28(1):87–101. https://doi.org/10.1016/j.dental.2011.09.003
van Dijken JW, Lindberg A (2009) Clinical effectiveness of a low-shrinkage resin composite: a five-year evaluation. J Adhes Dent 11(2):143–148
Schmidt M, Dige I, Kirkevang LL, Vaeth M, Horsted-Bindslev P (2015) Five-year evaluation of a low-shrinkage Silorane resin composite material: a randomized clinical trial. Clin Oral Investig 19(2):245–251. https://doi.org/10.1007/s00784-014-1238-x
Atabek D, Aktas N, Sakaryali D, Bani M (2017) Two-year clinical performance of sonic-resin placement system in posterior restorations. Quintessence Int 48(9):743–751. https://doi.org/10.3290/j.qi.a38855
Tardem C, Albuquerque EG, Lopes LS, Marins SS, Calazans FS, Poubel LA et al (2019) Clinical time and postoperative sensitivity after use of bulk-fill (syringe and capsule) vs. incremental filling composites: a randomized clinical trial. Braz Oral Res 33(0):e089. https://doi.org/10.1590/1807-3107bor-2019.vol33.0089
Veloso SRM, Lemos CAA, de Moraes SLD, do Egito Vasconcelos BC, Pellizzer EP, de Melo Monteiro GQ (2019) Clinical performance of bulk-fill and conventional resin composite restorations in posterior teeth: a systematic review and meta-analysis. Clin Oral Investig 23(1):221–233. https://doi.org/10.1007/s00784-018-2429-7
Cidreira Boaro LC, Pereira Lopes D, de Souza ASC, Lie Nakano E, Ayala Perez MD, Pfeifer CS, Goncalves F (2019) Clinical performance and chemical-physical properties of bulk fill composites resin -a systematic review and meta-analysis. Dent Mater 35(10):e249–e264. https://doi.org/10.1016/j.dental.2019.07.007
Acknowledgements
The authors thank Ivoclar Vivadent and 3M ESPE for providing materials used in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This article contains human participants performed by the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
For this type of study, formal consent is required. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Disclaimer
Data analyses and drafting of the manuscript were implemented without any restrictions by the funding sponsor.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yazici, A.R., Kutuk, Z.B., Ergin, E. et al. Six-year clinical evaluation of bulk-fill and nanofill resin composite restorations. Clin Oral Invest 26, 417–426 (2022). https://doi.org/10.1007/s00784-021-04015-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04015-2