Abstract
Adult subjects with growth hormone (GH) deficiency (GHD) are known to have reduced life expectancy due to increased cardiovascular and cerebrovascular events. In adults, these events are associated with elevated circulating concentrations of asymmetric dimethylarginine (ADMA) which is an endogenous inhibitor of l-arginine (Arg)-derived nitric oxide (NO). Low circulating concentrations of homoarginine (hArg) emerged as a cardiovascular risk factor. In adults, hArg seems to antagonize ADMA. In the present work, we tested the hypothesis that children with short stature without or with GHD have altered Arg/NO pathway as compared to children with normal growth. We studied 66 short stature children (38 boys, 28 girls) aged 3.5–17.3 years, who underwent the routine l-Arginine Test to diagnose presence of GHD. GHD was confirmed in 47 children (GHD group; 30 boys, 17 girls) and was absent in the remaining 19 children (non-GHD group; 8 boys, 11 girls). In addition, we investigated 24 healthy age- and gender-matched children (10 boys, 14 girls) with normal growth. In EDTA plasma samples of all children, we determined by mass spectrometry-based methods the concentrations of Arg, hArg and ADMA, and calculated the Arg/ADMA and hArg/ADMA molar ratios. With respect to these biochemical parameters, we did not find statistically significant differences between the GHD and non-GHD groups. Comparing short with normal stature children, we found small differences regarding plasma hArg concentrations [mean ± SD; median (25th–75th percentile)]: 2.06 ± 0.52 µM; 2.12 (1.74–2.36) µM vs. 1.7 ± 0.5 µM; 1.6 (1.4–1.8) µM, P < 0.001. Compared to normal stature children, short stature children had considerably higher plasma concentrations of ADMA [0.77 ± 0.15 µM; 0.77 (0.66–0.85) µM vs. 0.57 ± 0.09 µM; 0.58 (0.50–0.63) µM, P < 0.001], but not of Arg [83.3 ± 19.2 µM; 82.2 (71.9–90.3) µM vs. 86.5 ± 17.8 µM; 84.8 (77.2–94.8) µM, P = 0.336], or the hArg/ADMA ratio [2.74 ± 0.76; 2.7 (2.2–3.1) vs. 3.1 ± 1.2; 2.85 (2.42–3.66), P = 0.161. hArg in the GHD group (r = 0.41, P = 0.004) and the hArg/ADMA ratio in both groups (r = 0.44, P = 0.002 in GHD; r = 0.55, P = 0.01 in non-GHD)], but not ADMA were positively correlated with insulin-like growth factor-1 (IGF-1). hArg and hArg/ADMA differed between girls and boys in the GHD and non-GHD groups but in the normal growth group. The hArg/ADMA ratio increased with age in all groups. Our study suggests that hArg and ADMA are involved in growth in the childhood, presumably in an antagonistic manner, with ADMA slowing and hArg accelerating growth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nitric oxide (NO) is generated from l-Arginine (l-Arg) by nitric oxide synthase (NOS) isoforms virtually in all types of cells. Homoarginine (hArg), an l-Arg homologue, may also serve as substrate for NOS (Hecker et al. 1991; Moali et al. 1998). NO possesses several biological activities and exerts multiple pathophysiological roles. Thus, NO is a potent vasodilatator, an inhibitor of platelets and leukocyte adhesion, an important neurotransmiter (Cines et al. 1998), and exerts anti-proliferative and anti-atherosclerotic actions (Cooke and Dzau 1997). Asymmetric dimethylarginine (ADMA) is an endogenous inhibitor of NOS activity and an established cardiovascular risk factor in adults (Leiper and Vallance 2006). Recently, low circulating hArg concentrations emerged as a risk factor for stroke in patients that undergo coronary angiography (Pilz et al. 2011a) and cardiovascular and hepatic morbidity and mortality (März et al. 2010; Drechsler et al. 2011; Pilz et al. 2011a, b, 2014, 2015a, b; Atzler et al. 2013). In patients with cardiovascular risk, elevated serum hArg concentration was found during normal pregnancy and they were related to flow-mediated vasodilatation (Valtonen et al. 2008; see also Khalil et al. 2013).
Unlike in adults, the l-Arg/NO pathway in children has been rarely investigated in the past. Increased ADMA levels have been reported in children with hypertension (Goonasekera et al. 1997), citrullinemia (Lücke et al. 2006), focal-segmental glomerulosclerosis (Lücke et al. 2008), familial hypercholesterolemia (Jehlicka et al. 2009), chronic kidney disease (Brooks et al. 2009), homocystinuria (Kanzelmeyer et al. 2011) and hypercholesterolemia type II (Chobanyan-Jürgens et al. 2012). ADMA plasma concentrations in young healthy children are much higher than in adults and decrease with advancing age to reach the levels prevailing in adulthood (Lücke et al. 2007). There is increasing evidence that the l-Arg/NO pathway is differently regulated in children and adults.
Adults with growth hormone (GH) deficiency (GHD) are known to have reduced life expectancy due to increased cardiovascular (Rosen and Bengtsson 1990) and cerebrovascular (Bulow et al. 1997) events. GHD determinates a premature atherosclerosis (Colao et al. 2004, 2006) and is associated with a reduced bioavailability of NO (Capaldo et al. 2001). In GHD patients, GH replacement contributes to decreased cardiovascular risk by reducing ADMA levels and improving the Arg/ADMA ratio and endothelial dysfunction (Setola et al. 2008). Supplementation of GH in children with GHD was associated with the redistribution of adipose tissue from an abdominal to a more peripheral area, which may lead to decrease in obesity-related diseases, such as hypertension, diabetes mellitus, stroke, and myocardial infarction (Rosenbaum et al. 1989).
Children with short stature have a length below the 3rd percentile in relation to gender, age and population. But only every fourth child with short stature is small due to a certain disease and needs therapy. GHD in children has a prevalence of 1:4000–1:30,000 and is about 100 times rarer than idiopathic or familiar short stature (Binder 2014). Formation and distribution of GH is decreased, with the cause being hereditary or acquired. The Muscatine Study linked childhood coronary risk factors to atherosclerosis in asymptomatic adults. One of the most predictive childhood risk factor was found to be increased body mass index (BMI) (Baars et al.1998; Davis et al. 2001; Dawson et al. 2009).
In GHD children, significantly higher plasma ADMA levels, total cholesterol and LDL-cholesterol indicate that pre-pubertal GHD children like adults manifest increased cardiovascular risk markers (De Marco et al. 2014). After a 12-month GH treatment, ADMA, total cholesterol and LDL-cholesterol significantly decreased in GHD children, reaching values comparable to those in controls (De Marco et al. 2014). In contrast, another study showed no significant differences in plasma ADMA levels between GHD children and healthy controls, and a significant increase in ADMA levels in patients receiving GH therapy compared to baseline (Önder et al. 2014).
The aim of the present study was to test the hypothesis that children with short stature have altered the l-Arg/NO pathway compared to children with normal growth. In consideration of the importance of ADMA and its potential antagonist hArg in the circulation (Kayacelebi et al. 2014a; Tsikas and Kayacelebi 2014), the focus of our study was on circulating ADMA, hArg and Arg.
Materials and methods
Subjects
Patients referred for suspected slow statural growth were included in the study and underwent the l-Arginine Test to diagnose GHD. All children were overnight fasting. Excluded were patients with other endocrinologic, organic, chromosomal, metabolic or psycho-social reasons for microsomia. All children were asked to abstain from fish consumption for the last 24 h. The clinical baseline characteristics of the patients and of the healthy control children with normal growth are summarized in Table 1. Control children were recruited from those who had been referred for endoscopic diagnostic as in- or outpatient without chronic disease.
Patients with short stature (38 males, 28 females) aged from 3.5 to 17.3 years were tested for GHD by means of the l-Arginine Test. Thus, the patients received infusion of an l-Arg·HCl solution in 190 mL 0.9 g % NaCl (0.5 g Arg/kg bodyweight) for 30 min. Positive GHD was based on failure to show serum GH concentration above 8 µg/L in two l-Arginine Tests. GHD was confirmed in 47 children (GHD group); in 19 children with short stature no GHD was detected (non-GHD group) (Table 1).
Venous blood samples (2.7 mL) from the children were collected in EDTA monovettes (Sarstedt, Germany). If the patients underwent the l-Arginine Test, blood sampling occurred before starting the infusion. EDTA plasma was stored at −80 °C until analysis.
The studies were approved by the Ethics Committees of the Bochum University. Written informed consent was obtained from the parents.
Biochemical analyses
ADMA in plasma samples was determined by gas chromatography-tandem mass spectrometry (GC–MS/MS) as described elsewhere (Tsikas et al. 2003; Tsikas 2009). Arg in plasma samples was analysed by gas chromatography–mass spectrometry (GC–MS) (Tsikas et al. 2003). hArg in plasma samples was quantitated by gas chromatography–mass spectrometry (GC–MS) as described elsewhere (Kayacelebi et al. 2014b, 2015a). Study samples were analyzed alongside quality control (QC) samples as described previously for each analyte and biological sample. ADMA, Arg and hArg were determined in the QC samples with accuracy (bias %) and imprecision (relative standard deviation %) of less than ±20 % and ≤20 %, respectively. These data indicate the validity of the analytical results in study samples. All other parameters were measured by standard Clinical Chemistry assays.
Statistical analysis
Data are expressed as mean ± SD and/or median [25th–75th percentile]. Differences between the two study groups in continuous variables were tested by unpaired t test for normally distributed variables or the Mann–Whitney test for non-normally distributed variables. P values <0.05 were considered statistically significant. Categorical analysis was tested by Chi-Quadrat. Statistical analysis was performed using SPSS program (Statistical Package for Social Science), version 21.0 software for Windows (SPSS, Chicago, IL, USA). Graphs were constructed by GraphPad Prism 5.04 (GraphPad Prism Software Inc. San Diego, California, USA).
Results
Clinical and biochemical characteristics of the children enrolled in the present study are summarized in Table 1. For comparison we used the baseline levels, i.e., those measured in blood samples taken before starting the l-Arginine test. GHD was diagnosed in patients failing a GH-response during the test (i.e., GH <8 µg/L). Before starting the l-Arginine Test, there was no statistically difference in GH in children with GHD short stature and non-GHD short stature. There were no statistically significant differences in TSH, IGF-1, IGFBP3 and GH as baseline between the GHD and non-GHD groups (Table 1). Yet, IGF-1 levels failed narrowly statistical significance (P = 0.055).
Plasma Arg, hArg and ADMA concentrations as well as the Arg/ADMA and hArg/ADMA molar ratios did not differ between GHD and non-GHD short stature children. Compared to healthy normal stature children, with short stature children had significantly higher plasma concentrations of ADMA [0.77 ± 0.15 µM; 0.77 (0.66–0.85) µM vs. 0.57 ± 0.09 µM; 0.58 (0.50–0.63) µM, P < 0.001] and hArg [2.06 ± 0.52 µM; 2.12 (1.74–2.36) µM vs. 1.70 ± 0.50 µM; 1.6 (1.4–1.8), P < 0.001], but not of Arg (83.8 ± 19.2 µM vs. 86.5 ± 17.8 µM, P = 0.336). In line with these findings, the Arg/ADMA molar ratio in plasma was higher in normal compared to short stature children (113 ± 33 µM vs. 155 ± 33, P < 0.001).
In short stature children without GHD, the hArg/ADMA ratio but not ADMA (r = −0.22, P = 0.38) or hArg (Fig. 1a) correlated positively with IGF-1. With respect to BMI, Arg, ADMA and Arg/ADMA there was no statistical difference between non-GHD short stature girls and boys (Table 2). Girls had significantly (P = 0.043) higher circulating hArg concentrations, whereas the difference regarding hArg/ADMA ratio was borderline (P = 0.137) (Table 2).
In short stature children with GHD, both hArg/ADMA and hArg (Fig. 1b) but not ADMA (r = −0.04, P = 0.80) were positively correlated with IGF-1. This correlation was stronger in females (r = 0.611, P = 0.009 for hArg; r = 0.516, P = 0.034 for hArg/ADMA; n = 17) than in males (r = 0.355, P = 0.059 for hArg; r = 0.475, P = 0.009 for hArg/ADMA; n = 29). With respect to BMI, Arg, ADMA and Arg/ADMA there were no statistical differences between short stature GHD girls and boys (Table 3). Girls had significantly (P = 0.021) higher hArg/ADMA ratios, whereas the difference regarding hArg was borderline (P = 0.095) (Table 3).
In healthy normal stature children, there were no differences between girls and boys with respect to BMI, Arg, ADMA, Arg/ADMA, hArg and hArg/ADMA (Table 4).
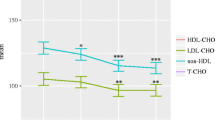
In a previous work, we found that the concentration of ADMA in plasma of healthy children decreases consistently until adulthood (Lücke et al. 2007). Compared to healthy elderly subjects (Tsikas and Kayacelebi 2014), the healthy normal stature children of the present study have considerably lower hArg concentrations in plasma. This may suggest that hArg synthesis increases with age. As a consequence of decreasing ADMA and concomitant increasing hArg concentration in the circulation, the hArg/ADMA molar ratio is expected to increase with age. Indeed, we observed a positive correlation between the plasma hArg/ADMA molar ratio and age in short stature children without GHD (r = 0.641, P = 0.003) and with GHD (r = 0.411, P = 0.004), whereas this correlation failed narrowly statistical significance in normal statute healthy children (r = 0.345, P = 0.097) (Fig. 2).
Discussion
l-Arginine belongs to the best investigated, semi-essential proteinogenic amino acids and plays multiple physiological roles (Wu et al. 2009). In the Arg/NO pathway, much less than 0.1 % of Arg is utilized in humans for the NOS-catalysed formation of NO. Nevertheless, the Arg/NO pathway plays a pivotal role in health and disease. In adults, high circulating ADMA (Leiper and Vallance 2006) and low circulating hArg concentrations (März et al. 2010; Drechsler et al. 2011; Pilz et al. 2011a, b, 2014, 2015a; Atzler et al. 2013) are potential risk factors for stroke and cardiovascular morbidity and mortality. GHD is another well-known cardiovascular risk factor in adults (Rosen and Bengtsson 1990). Yet, the importance of circulating ADMA and hArg and their potential relation to GHD in childhood are poorly understood. The aim of the present study was therefore to measure circulating concentrations of ADMA, hArg and Arg in short stature children without GHD or with GHD, as well as in normal stature healthy control children, in order to determine the status of the Arg/NO pathway and hArg in children in relation to GHD.
In the present study, we did not find differences in plasma Arg, hArg and ADMA concentrations between GHD and non-GHD short stature children. Short and normal stature children had very similar Arg plasma concentrations and little differing hArg plasma concentrations in our study. On the other hand, the ADMA plasma concentrations were remarkably higher in the short stature compared to normal stature children, i.e., by about 26 %. This difference cannot be attributed to differences in the demographic characteristics of the population studied in the present work (Lücke et al. 2007). The finding with respect to ADMA concentrations agrees with recently reported findings (De Marco et al. 2014), but disagrees with those reported almost in parallel by another study (Önder et al. 2014). Differences in the populations investigated and in the analytical methods used to determine circulating ADMA concentrations are likely to have contributed to the discrepancies observed by these two groups (De Marco et al. 2014; Önder et al. 2014).
It is still unknown why GHD and non-GHD children have similar circulating ADMA, Arg and hArg concentrations. One possible explanation may be that GH itself is not primarily associated with these amino acids under regular conditions such as normal circulating Arg concentrations. Also, GH supplementation may not be favourable with respect to the Arg/NO pathway, although GH replacement may improve cardiovascular outcome by altering lipid profiles (Foster et al. 2014), presumably independent of the Arg/NO pathway. At first glance, because circulating Arg and hArg concentrations are not very different in short stature and normal stature children, respectively, Arg and hArg appear unlikely to be associated with stature in childhood. Unlike circulating Arg, circulating ADMA is largely independent of nutritional or pharmaceutical Arg. Nevertheless, the considerably higher ADMA plasma concentrations measured in short stature children compared to those measured in healthy children with normal stature may decrease the relative bioavailability of NO (expressed as the Arg/ADMA ratio) and may attenuate the protective effect of hArg (expressed as the hArg/ADMA ratio) in the vasculature (Kayacelebi et al. 2014a; Tsikas and Kayacelebi 2014).
The difference in circulating ADMA concentrations between short and normal stature children observed in the present study is remarkable. Also, the positive correlation of IGF-1 with the hArg/ADMA molar ratio in the short stature children without GHD, and with hArg and hArg/ADMA molar ratio in short stature children with GHD is interesting. Given that short stature children have considerably higher plasma ADMA concentrations than normal stature children in our study may be of particular importance in the context of children’s growth. The results of the present study and a previous study indicating constantly decreasing ADMA synthesis until the adulthood (Lücke et al. 2007) suggest that ADMA may function as a regulator, presumably as repressor of growth in the childhood (Fig. 3a). In general, NO is regarded as an angiogenic factor, and ADMA, being an inhibitor of NOS activity, is generally assumed to inhibit angiogenesis (Cooke 2006). Whether ADMA may inhibit growth by NO-independent mechanisms is unclear and remains to be elucidated (Fig. 3b). Our study suggests that hArg may positively contribute to growth; however, the underlying mechanisms are unresolved. hArg, being a substrate of NOS, may elevate NO synthesis by two ways: by serving as a substrate for NOS and by attenuating the inhibitory action of ADMA on NOS activity. Whether hArg may enhance growth, for instance by stimulating IGF-1 synthesis, by NO-independent mechanisms is unclear and remains to be elucidated as well (Fig. 3b). In a previous work, we suggested that hArg and ADMA may act antagonistically in the circulation. We assume that the value of the Arg/ADMA molar ratio may reflect the resulting net effect of hArg and Arg in the vasculature (Kayacelebi et al. 2014a; Tsikas and Kayacelebi 2014). The present study suggests that the higher the hArg/ADMA ratio is, the higher is the IGF-1 and, consequently, growth.
Proposal of asymmetric dimethylarginine (ADMA) as a modulator of growth by mechanisms (a) depending on nitric oxide (NO) and (b) independent of NO, and of the antagonistic actions of l-homoarginine (hArg). In mechanism (a), ADMA inhibits the NOS-catalyzed synthesis of NO from l-arginine and thus the NO-dependent growth. hArg may attenuate this effect of ADMA by serving as substrate for NOS. In mechanism (b), ADMA itself or ADMA-containing proteins inhibit the production of GH/IGF-1, thus repressing growth. hArg may attenuate this effect of ADMA and/or ADMA-containing proteins
The idea of a growth-attenuating role of ADMA and a growth-promoting role of hArg is supported by several in vivo and in vitro findings. For example, in middle-aged healthy volunteers, administration of recombinant human GH decreased plasma ADMA concentration, without changing plasma and urinary concentrations of the NO metabolites nitrite and nitrate (Thum et al. 2007). Also, normalization of plasma testosterone concentration by transdermal testosterone administration to hypogonadal men decreased the plasma ADMA concentration (Leifke et al. 2008). In normal pregnancy, the hArg/ADMA ratio in maternal blood is higher than in non-pregnant women and increases in gestation to reach mean values around 10 (Valtonen et al. 2008; Khalil et al. 2013; Tsikas and Kayacelebi 2014). In vitro, ADMA externally added to cultured human umbilical vein endothelial cells accelerated their senescence (Scalera et al. 2004). In another in vitro study, GH was found to act directly on GH receptors in human aortic endothelial cells and on eNOS phosphorylation and activity as measured by the L-citrulline assay (Li et al. 2008). Yet, it is worth mentioning that ADMA is a very weak inhibitor (IC50 ≈ 12 µM) of eNOS activity (Kielstein et al. 2007). These observations argue for a much stronger negative effect of ADMA on growth by NO-independent mechanisms. For example, in Indian children with GHD, one-year GH therapy was found to have beneficial effects on body composition and cardio-metabolic risk (Khadilkar et al. 2014). Thus, GHD may be associated with an elevated cardiovascular risk via abnormal body composition, presumably independent of an NO-based mechanism.
Patients with primary hyperparathyroidism have elevated circulating concentrations of parathyroid hormone (PTH). Patients with primary hyperparathyroidism were found to have lower serum hArg levels compared with matched controls (Tomaschitz et al. 2015). Among a general older population, higher PTH concentrations are associated with higher all-cause mortality risk, mostly explained by fatal cardiovascular disease events (van Ballegooijen et al. 2013). In a random population sample of women but not of men, IGF-1 was found to correlate negatively with PTH (Landin-Wilhelmsen et al. 1994). In post-menopausal women with primary hyperparathyroidism, GH administration increased IGF-1 but decreased PTH concentration (Lombardi et al. 2010). There is increasing evidence from clinical studies of an interaction between GH/IGF-1 and PTH on bone in the adulthood. Arginine:glycine amidinotransferase (AGAT) is considered the main enzyme responsible for the synthesis of hArg (Davids et al. 2012; Kayacelebi et al. 2015b; Pilz et al. 2015a). As AGAT gene expression and subsequent AGAT-catalyzed hArg synthesis are regulated by GH, IGF-1 and PTH are likely to modulate the biosynthesis of hArg in the childhood as well. Yet, as circulating PTH levels are not available from the children of our study, a potential interplay between PTH and GH/IGF-1 remains to be investigated in forthcoming studies.
Conclusions
In short stature children without and with GHD and on the basis of the clinical l-Arginine test, ADMA but not Arg and hArg plasma concentrations are elevated compared to age- and sex-matched healthy children with normal stature. This may suggest that short stature children may have an increased cardiovascular risk independent of the GH status. The role of hArg and ADMA in the childhood is unrevealed. Our results suggest that ADMA and hArg may be involved in the regulation of growth in the childhood. Higher ADMA concentrations are likely to exert an inhibitory/slowing effect on growth, whereas higher hArg concentrations seem to promote/accelerate growth, presumably by NO-dependent and NO-independent mechanisms. The hArg/ADMA molar ratio in the circulation is a quantitative measure of the actions of the antagonistically acting amino acids hArg and ADMA. In short stature children, hArg seems not to outweigh sufficiently the inhibitory effect of ADMA on growth. We propose that in the childhood, that is a phase of life in which the child organism is growing, higher ADMA synthesis is required than in the adulthood in order to control growth and slowdown excess growth. Forthcoming experimental and clinical studies are warranted to address these issues. Such studies need to consider that boys and girls behave differently with respect to hArg biosynthesis (circulating hArg concentration) and its antagonistic action on ADMA (circulating hArg/ADMA molar ratio).
Abbreviations
- ADMA:
-
Asymmetric dimethylarginine
- AGAT:
-
Arginine:glycine amidinotransferase
- Arg:
-
l-Arginine
- BMI:
-
Body mass index
- GH:
-
Growth hormone
- GHD:
-
Growth hormone deficiency
- hArg:
-
l-Homoarginine
- IGF-1:
-
Insulin-like growth factor 1
- IGFBP:
-
Insulin-like growth factor binding protein
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- PTH:
-
Parathyroid hormone
- QC:
-
Quality control
- TSH:
-
Thyroid stimulating hormone
References
Atzler D, Rosenberg M, Andersso M, Choe CU, Lutz M, Zugck C, Böger RH, Frey N, Schwedhelm E (2013) Homoarginine—an independent marker of mortality in heart failure. Int J Cardiol 168:4907–4909
Baars J, Van den Broeck J, le Cessie S (1998) Body mass index in growth hormone deficient children before and during growth hormone treatment. Horm Res 49:39–45
Binder G (2014) Kleinwuchs und Therapie. Monatsschrift Kinderheilkunde 162:299–308
Brooks ER, Langmann CB, Wang S, Price HE, Hodges AL, Darling L, Yang AZ, Smith FA (2009) Methylated arginine derivates in children and adolescents with chronic kidney disease. Pediatr Nephrol 24:129–134
Bulow B, Hagmar L, Mikoczy Z, Nordström CH, Erfurth EM (1997) Increased cerebrovascular mortality in patients with hypopituitarism. Clin Endocrin 46:75–81
Capaldo B, Guardasole V, Pardo F, Matarazzo M, Di Rella F, Numis F, Merola B, Longobardi S, Sacca L (2001) Abnormal vascular reactivity in growth hormone deficiency. Circulation 103(4):520–524
Chobanyan-Jürgens K, Fuchs A-J, Tsikas D, Kanzelmeyer N, Das AM, Illsinger S, Vaske B, Jordan J, Lücke T (2012) Increased asymmetric dimethylarginine (ADMA) dimethylaminohydrolase (DDAH) activity in childhood hypercholesterinemia type II. Amino Acids 43(2):805–811
Cines DB, Pollak ES, Buck CA, Loscalzo J, Zimmerman GA, McEver RP, Pober JS, Wick TM, Konkle BA, Schwartz BS, Barnathan ES, McCrae KR, Hug BA, Schmidt AM, Stern DM (1998) Endothelial cells in physiology and in the pathophysiology of vascular disorders. Blood 91(10):3527–3561
Colao A, Di Somma C, Filippella M, Rota F, Piconello R, Orio F, Vitale G, Lombardi G (2004) Insulin-like growth factor-1 deficiency determines increased intima-media thickness at common carotid arteries in adult patients with growth hormone deficiency. Clin Endocrinol (Oxf) 61(3):360–366
Colao A, Di Somma C, Spiezia S, Rota F, Pivonello R, Savastano S, Lombardi G (2006) The natural history of partial growth hormone deficiency in adults: a prospective study on the cardiovascular risk and atherosclerosis. J Clin Endocrinol Metab 91(6):2191–2200
Cooke JP (2006) Asymmetric dimethylarginine (ADMA): an endogenous inhibitor of angiogenesis. Eur J Clin Pharmacol 62:115–121
Cooke JP, Dzau VJ (1997) Nitric oxide synthase: role in the genesis of vascular disease. Annu Rev Med 48:489–509
Davids M, Ndika JD, Salomons GS, Blom HJ, Teerlink T (2012) Promiscuous activity of arginine:glycine amidinotransferase is responsible for the synthesis of the novel cardiovascular risk factor homoarginine. FEBS Lett 586:3653–3657
Davis PH, Dawson JD, Riley WA, Lauer RM (2001) Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: the Muscatine Study. Circulation 104:2815–2819
Dawson JD, Sonka M, Blecha MB, Lin W, Davis PH (2009) Risk factors associated with aortic and carotid intima-media thickness in adolescents and young adults: the Muscatine Offspring Study. J Am Coll Cardiol 53(24):2273–2279
De Marco S, Marcovecchio ML, Caniglia D, De Leonibus C, Chiarelli F, Mohn A (2014) Circulating asymmetric dimethylarginine and lipid profile in pre-pubertal children with growth hormone deficiency: effect of 12-month growth hormone replacement therapy. Growth Horm IGF Res 5:216–220
Drechsler C, Meinitzer A, Pilz S, Krane V, Tomaschitz A, Ritz E, März W, Wanner C (2011) Homoarginine, heart failure, and sudden cardiac death in haemodialysis patients. Eur J Heart Fail 13:852–859
Foster C, Burton A, Scholl J, Scott ML, Gunter V, McCormick K (2014) Lipid patterns in treated growth hormone deficient children vs. short stature controls. J Pediatr Endocrinol Metab 27:909–914
Goonasekera CDA, Rees DD, Woolard P, Frend A, Shah V, Dillon MJ (1997) Nitric oxide synthase inhibition and hypertension in children and adolescents. J Hypertens 15:901–909
Hecker M, Walsh DT, Vane JR (1991) On the substrate specificity of nitric oxide synthase. FEBS Lett 294:221–224
Jehlicka P, Stozicky F, Mayer OJR, Varvarovska J, Racek J, Trefil L, Siala K (2009) Asymmetric dimethylarginine and the effect of folat substitution in children with familial hypercholesterolemia and diabetes mellitus type I. Physiol Res 58:179–184
Kanzelmeyer N, Tsikas D, Chobanyan-Jürgens K, Beckmann B, Vaske B, Illsinger S, Das AM, Lücke T (2011) Asymmetric dimethylarginine in children with homocystinuria or phenylketonuria. Amino Acids 42(5):1765–1772
Kayacelebi AA, Pham VV, Willers J, Hahn A, Stichtenoth DO, Jordan J, Tsikas D (2014a) Plasma homoarginine (hArg) and asymmetric dimethylarginine (ADMA) in patients with rheumatoid arthritis: is homoarginine a cardiovascular corrective in rheumatoid arthritis, an anti-ADMA? Int J Cardiol 176(3):1129–1131
Kayacelebi AA, Beckmann B, Gutzki FM, Jordan J, Tsikas D (2014b) GC-MS and GC- MS/MS measurement of the cardiovascular risk factor homoarginine in biological samples. Amino Acids 46:2205–2217
Kayacelebi AA, Knöfel AK, Beckmann B, Hanff E, Warnecke G, Tsikas D (2015a) Measurement of unlabeled and stable isotope-labeled homoarginine, arginine and their metabolites in biological samples by GC-MS and GC-MS/MS. Amino Acids. doi:10.1007/s00726-015-1984-3
Kayacelebi AA, Langen J, Weigt-Usinger K, Chobanyan-Jürgens K et al (2015b) Biosynthesis of homoarginine (hArg) and asymmetric dimethylarginine (ADMA) from acutely and chronically administered free l-arginine in humans. Amino Acids. doi:10.1007/s00726-015-2012-3
Khadilkar V, Ekbote V, Kajale N, Khadilkar A, Chiplonkar S, Kinare A (2014) Effect of one-year growth hormone therapy on body composition and cardio-metabolic risk in Indian children with growth hormone deficiency. Endocr Res 39(2):73–78
Khalil AA, Tsikas D, Akolekar R, Jordan J, Nicolaides KH (2013) Asymmetric dimethylarginine, arginine and homoarginine at 11-13 weeks’ gestation and preeclampsia: a case-control study. J Hum Hypertens 27:38–43
Kielstein A, Tsikas D, Galloway GP, Mendelson JE (2007) Asymmetric dimethylarginine (ADMA)—a modulator of nociception in opiate tolerance and addiction? Nitric Oxide 17:55–59
Landin-Wilhelmsen K, Wilhelmsen L, Lappas G, Rosén T, Lindstedt G, Lundberg PA, Bengtsson BA (1994) Serum insulin-like growth factor I in a random population sample of men and women: relation to age, sex, smoking habits, coffee consumption and physical activity, blood pressure and concentrations of plasma lipids, fibrinogen, parathyroid hormone and osteocalcin. Clin Endocrinol (Oxf) 41:351–357
Leifke E, Kinzel M, Tsikas D, Gooren L, Frölich JC, Brabant G (2008) Effects of normalization of plasma testosterone evels in hypogonadal men on plasma levels and urinary excretion of asymmetric dimethylarginine (ADMA). Horm Metab Res 40:56–59
Leiper M, Vallance P (2006) The synthesis and metabolism of asymmetric dimethylarginine (ADMA). Eur J Clin Pharmacol 62:33–38
Li G, Del Rincon JP, Jahn LA, Wu Y, Gaylinn B, Thorner MO, Liu Z (2008) Growth hormone exerts acute vascular effects independent of systemic or muscle insulin-like growth factor I. J Clin Endocrinol Metab 93:1379–1385
Lombardi G, Di Somma C, Vuolo L, Guerra E, Scarano E, Colao A (2010) Role of IGF-I on PTH effects on bone. J Endocrinol Invest 33(7 Suppl):22–26
Lücke T, Tsikas D, Kanzelmeyer N, Vaske B, Das AM (2006) Elevated plasma concentrations of the endogenous nitric oxide synthase inhibitor asymmetric dimethylarginine in citrullinemia. Metabolism 55:1599–1603
Lücke T, Kanzelmeyer N, Kemper MJ, Tsikas D, Das AM (2007) Developmental changes in the l-arginine/nitric oxide pathway from infancy to adulthood: plasma asymmetric dimethylarginine levels decrease with age. Clin Chem Lab Med 45:1525–1530
Lücke T, Kanzelmeyer N, Chobanyan K, Tsikas D, Franke D, Kemper MJ, Ehrich JHH, Das AM (2008) Elevated asymmetric dimethylarginine (ADMA) and inverse correlation between circulating ADMA and glomerular filtration rate in children with sporadic focal semental glomerulosclerosis (FSGS). Nephrol Dial Transplant 23:734–740
März W, Meinitzer A, Drechsler C, Pilz S, Krane V, Kleber ME, Fischer J, Winkelmann BR, Böhm BO, Ritz E, Wanner C (2010) Homoarginine, cardiovascular risk, and mortality. Circulation 122:967–975
Moali C, Boucher JL, Sari MA, Stuehr DJ, Mansuy D (1998) Substrate specificity of NO synthases: detailed comparison of l-arginine, homo-l-arginine, their N omega- hydroxy derivatives, and N omega-hydroxynor-l-arginine. Biochemistry 37:10453–10460
Önder A, Aycan Z, Koca C, Ergin M, Çetinkaya S, Ağladıoğlu SY, Peltek Kendirci HN, Baş VN (2014) Evaluation of asymmetric dimethylarginine (ADMA) levels in children with growth hormone deficiency. J Clin Res Pediatr Endocrinol 6(1):22–27
Pilz S, Tomaschitz A, Meinitzer A, Drechsler C, Ritz E, Krane V, Wanner C, Böhm BO, März W (2011a) Low serum homoarginine is a novel risk factor for fatal strokes in patients undergoing coronary angiography. Stroke 42:1132–1134
Pilz S, Meinitzer A, Tomaschitz A, Drechsler C, Ritz E, Krane V, Wanner C, Böhm BO, März W (2011b) Low homoarginine concentration is a novel risk factor for heart disease. Heart 97:1222–1227
Pilz S, Teerlink T, Scheffer PG, Meinitzer A, Rutters F, Tomaschitz A, Drechsler C, Kienreich K, Nijpels G, Stehouwer CD, März W, Dekker JM (2014) Homoarginine and mortality in an older population: the Hoorn study. Eur J Clin Invest 44:200–208
Pilz S, Meinitzer A, Gaksch M, Grübler M, Verheyen N, Drechsler C, Hartaigh BÓ, Lang F, Alesutan I, Voelkl J, März W, Tomaschitz A (2015a) Homoarginine in the renal and cardiovascular systems. Amino Acids. doi:10.1007/s00726-015-1993-2
Pilz S, Putz-Bankuti C, Meinitzer A, März W, Kienreich K, Stojakovic T, Pieber TR, Stauber RE (2015b) Association of homoarginine and methylarginines with liver dysfunction and mortality in chronic liver disease. Amino Acids. doi:10.1007/s00726-015-2000-7
Rosen T, Bengtsson BA (1990) Premature mortality due to cardiovascular disease in hypopituitarism. Lancet 336(8710):285–288
Rosenbaum M, Gernter JM, Leiber RL (1989) Effects of systemic growth hormone (GH) administration on regional adipose tissue distribution and metabolism in GH- deficient children. J Clin Endocrinol Metab 69:1274–1281
Scalera F, Borlak J, Beckmann B, Martens-Lobenhoffer J, Thum T, Täger M, Bode-Böger SM (2004) Endogenous nitric oxide synthesis inhibitor asymmetric dimethyl l-arginine accelerates endothelial cell senescence. Arterioscler Thromb Vasc Biol 24:1816–1822
Setola E, Monti LD, Lanzi R, Lucotti P, Losa M, Gatti E, Galluccio E, Oldani M, Fermo I, Giovannelli M, Bosi E, Piatti PM (2008) Effects of growth hormone treatment on arginine to asymmetric dimethylarginine ratio and endothelial function in patients with growth hormone deficiency. Metabolism 57:1685–1690
Thum T, Fleissner F, Klink I, Tsikas D, Jakob M, Bauersachs J, Stichtenoth DO (2007) Growth hormone treatment improves markers of systemic nitric oxide bioavailability via insulin-like growth factor-I. J Clin Endocrinol Metab 92:4172–4179
Tomaschitz A, Verheyen N, Gaksch M, Meinitzer A, Pieske B, Kraigher-Krainer E, Colantonio C, März W, Schmidt A, Belyavskiy E, Rus-Machan J, van Ballegooijen AJ, Stiegler C, Amrein K, Ritz E, Fahrleitner-Pammer A, Pilz S (2015) Homoarginine in patients with primary hyperparathyroidism. Am J Med Sci 349:306–311
Tsikas D (2009) De novo synthesis of trideuteromethyl esters of amino acids for use in GC-MS and GC-tandem MS exemplified for ADMA in human plasma and urine: standardization, validation, comparison and proof of evidence for their aptitude as internal standards. J Chromatogr B Analyt Technol Biomed Life Sci 877(23):2308–2320
Tsikas D, Kayacelebi AA (2014) Do homoarginine and asymmetric dimethylarginine act antagonistically in the cardiovascular system? Circ J 78(8):2094–2095
Tsikas D, Schubert B, Grutzki FM, Sandmann J, Frölich JC (2003) Quantitative determination of circulating and urinary asymmetric dimethylarginine (ADMA) in humans by gas chromatography-tandem mass spectometry as methyl ester tri(N- pentrafluoropropionyl) derivate. J Chromatogr B Analyt Technol Biomed Life Sci 798:87–99
Valtonen P, Laitinen T, Lyyra-Laitinen T, Raitakari OT, Juonala M, Viikari JS, Heiskanen N, Vanninen E, Punnonen K, Heinonen S (2008) Serum l-homoarginine concentration is elevated during normal pregnancy and is related to flow-mediated vasodilatation. Circ J 72:1879–1884
van Ballegooijen AJ, Reinders I, Visser M, Dekker JM, Nijpels G, Stehouwer CD, Pilz S, Brouwer IA (2013) Serum parathyroid hormone in relation to all-cause and cardiovascular mortality: the Hoorn study. J Clin Endocrinol Metab 98:E638–E645
Wu G, Bazer FW, Davis TA, Kim SW, Li P, Marc Rhoads J, Carey Satterfield M, Smith SB, Spencer TE, Yin Y (2009) Arginine metabolism and nutrition in growth, health and disease. Amino Acids 37:153–168
Conflict of interest
The authors declare that they have no conflict of interest.
Compliance with ethical standards
Accepted principles of ethical and professional conduct have been followed. The studies were approved by the Ethics Committees of the Bochum University. Informed consent of the parents of the children involved in the study was obtained.
Author information
Authors and Affiliations
Corresponding author
Additional information
D. Tsikas and T. Lücke are senior authors.
Rights and permissions
About this article
Cite this article
Langen, J., Kayacelebi, A.A., Beckmann, B. et al. Homoarginine (hArg) and asymmetric dimethylarginine (ADMA) in short stature children without and with growth hormone deficiency: hArg and ADMA are involved differently in growth in the childhood. Amino Acids 47, 1875–1883 (2015). https://doi.org/10.1007/s00726-015-2028-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-015-2028-8