Abstract
Numerous reports have indicated that the plasma concentration of endogenously produced inhibitors of nitric oxide synthase are elevated in human disease states. In this review we discuss recent advances in our understanding of the enzymes responsible for the synthesis and metabolism of these inhibitors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Endogenous inhibitors of nitric oxide synthase
Free guanidino-methylated (N G) arginine residues occur endogenously as a result of proteolysis of post-translationally methylated tissue proteins [1]. The arginine analogues identified to date include N G-monomethyl-L-arginine (L-NMMA), N G,N G-dimethyl-L-arginine (asymmetric dimethylarginine; ADMA) and N G,N′G-dimethyl-L-arginine (symmetric dimethylarginine; SDMA) (Fig. 1). The asymmetrically methylated arginine residues (L-NMMA and ADMA), but not the symmetrically methylated arginine (SDMA), are competitive inhibitors of the nitric oxide synthase (NOS) enzymes.
Structure of L-arginine and endogenously produced methylarginines. Only asymmetrically methylated arginines (L-NMMA and ADMA) are nitric oxide synthase inhibitors. L-NMMA N G-monomethyl-L-arginine, ADMA (asymmetric dimethylarginine) N G,N G-dimethyl-L-arginine, SDMA (symmetric dimethylarginine) N G,N′G-dimethyl-L-arginine
Initially L-NMMA was developed as a pharmacological tool and was not known to be a naturally occurring compound. The inhibition of NO formation by L-NMMA in cultured vascular endothelial cells was demonstrated by Palmer et al. [2]. These workers also showed that L-NMMA could elicit an endothelium-dependent increase in the tone of rabbit aortic rings and inhibit the endothelium-dependent relaxation induced by acetylcholine. These results were consistent with inhibition of vascular endothelial NOS (eNOS) under basal and stimulated conditions. In vivo, L-NMMA increased mean arterial blood pressure in rabbit [3], rat [4] and guinea-pig [5]. In humans, local infusion of L-NMMA in brachial arteries caused a fall in basal blood flow and attenuated the dilator response to acetylcholine [6]. NO was therefore identified as a major determinant of blood pressure and vascular tone. Subsequently, ADMA was shown to have similar effects to L-NMMA while SDMA was inactive [7]. In pre-contracted endothelium-intact rat aortic rings, ADMA caused dose-dependent increases in tone. ADMA was able to raise blood pressure in guinea-pigs and reduce resting forearm blood flow. Thus, it was postulated that ADMA, which was identified as circulating in human plasma at a concentration ten times greater than that of naturally occurring L-NMMA, might act as an important endogenous regulator of the L-arginine/NO pathway and/or arginine-handling enzymes in vivo [7].
Methylarginine synthesis
Protein methylation is a post-translational modification involving addition of a methyl group to a polypeptide chain by enzymes termed protein methyltransferases (reviewed in [8, 9]). These enzymes utilise S-adenosylmethionine as methyl donors and catalyse a large number of modifications that can be divided into two groups. The first group of reactions modifies carboxyl groups to generate methyl esters. These reactions are generally reversible by the actions of protein methylesterases. They function to regulate the activity of target proteins and can be seen as analogous to protein phosphorylation and dephosphorylation. These reactions will not be discussed further here. The second group of protein-methylation reactions results in generally irreversible methyl transfer to sulphur or nitrogen atoms of several amino acids. The function of these reactions is less clear but possibly it provides a way of creating proteins with new function without de novo protein synthesis. Methylation of the terminal nitrogen atom(s) of arginine belongs to this group and is catalysed by a family of enzymes termed protein-arginine methyltransferases (PRMTs).
PRMT activity was initially identified by Paik and Kim [10] and denoted protein methylase I activity. Two types of activity were thereafter discovered: myelin basic protein-specific and histone-specific [11]. Although the existence of protein-arginine methylation has been known for over 30 years, the genes encoding PRMTs have only been cloned in the last decade and their cellular functions are only beginning to be understood. PRMTs are now classified into two types according to substrate and reaction product specificity (Fig. 2). Six PRMT genes have been cloned to date and labelled PRMT1 to PRMT6. Methyltransferase activity has been demonstrated for all PRMT gene products except PRMT2. Type I and II enzymes both form L-NMMA (possibly as an intermediary species to the formation of the dimethylated species) but differ in that type I enzymes produce ADMA while type II enzymes produce SDMA. In vivo substrates for type I PRMTs include histones and RNA-binding proteins including heterogeneous nuclear ribonuclear protein (hnRNP) A1, fibrillarin, nucleolin. Methylation of RNA-binding proteins occurs in all cells. hnRNPs are a group of proteins that regulate mRNA maturation, stability and export to the cytoplasm and their activity is regulated by methylation. Approximately 65% of total cellular ADMA is contained in hnRNPs [12]. To date, the only known in vivo substrates for type II PRMTs are myelin basic protein (MBP) and spliceosomal D1 and D3 proteins [13]. Type I PRMTs have no activity towards MBP. MBP is a major component of the myelin sheath of nerve axons and a role for arginine methylation in the maintenance and functional integrity of the myelin sheath has been suggested [14].
Methylation of arginine residues in proteins by protein-arginine methyltransferases. Arginine residues in proteins that lie within appropriate consensus sequences can be post-translationally methylated by the action of Protein Arginine MethylTransferase enzymes (PRMT's). S-Adenosyl methionine (SAM) is the methyl donor in these reactions and S-adenosyl homocysteine (SAH) is produced. ADMA asymmetric dimethylarginine, SDMA symmetric dimethylarginine, L-NMMA N G-monomethyl-L-arginine
Although the overall physiological role of PRMTs is not clear, one of their functions appears to be regulation of mRNA processing and maturation by modulating the activity of RNA-binding proteins. These nuclear substrates of type I PRMTs are ubiquitous and highly abundant proteins that contain clusters of asymmetrically methylated arginine residues. There is no evidence to date to suggest that methylated arginine residues in proteins can be demethylated in an enzyme-catalysed reaction. Indeed, synthesis and degradation of methylated proteins has been shown to be closely coupled with protein synthesis and degradation [15]. Thus, it is assumed that upon proteolysis of these type I substrates, significant amounts of free ADMA are released into the cytoplasm. Intracellular ADMA levels may therefore be governed by PRMT activity and protein turnover.
Release of free methylarginine residues
An essential component of cell survival is protein degradation and this is a major source of intracellular and plasma arginine and methylarginines. In the adult liver, for example, constitutive proteins are turned over at a rate of 40% per day [16]. In such tissues with high turnover rates, levels of free methylarginines liberated upon protein degradation (which are not re-incorporated into proteins) might be sufficiently high to inhibit NOS. In contrast, endothelial cells turn over very slowly and have lifetimes of months or years. However, the proportion of proliferating endothelial cells is especially high at branch points in arteries, where it is presumed that turbulence stimulates cell turnover [17], and in these cells ADMA levels may be significantly higher than in non-dividing cells.
Several conditions are associated with enhanced protein catabolism. Muscular dystrophy is a disease characterized by muscular wasting and rapid degradation of all classes of muscle protein. In patients with this disease, increased urinary ADMA levels have been reported with no change in SDMA levels compared to healthy controls [18]. A primitive function of protein turnover is to secure cells an endogenous source of amino acids. An essential adaptation to stress, fasting or infection in mammals is the mobilization of amino acids from tissue proteins. Accelerated protein breakdown of skeletal muscle during fasting was first indicated by Millward [19]. Increased protein degradation has also been reported in ischaemic heart [20] and diabetes [21]. In these conditions, it is possible that free methylarginine levels are raised.
Transient changes in the rate of protein degradation may also occur. Exposure of cultured hepatoma cells to a 43°C heat shock transiently accelerates the degradation of the long-lived fraction of cellular proteins [22]. It is conceivable that under conditions of cellular stress, e.g. ischaemic or reperfusion injury, endotoxaemia, activity of this pathway may be upregulated to remove abnormal proteins. Cellular concentrations of free methylarginines may therefore rise in response to these insults.
Methylarginine handling in vivo: identification of dimethylarginine dimethylaminohydrolase (DDAH)
The isolation of appreciable quantities of ADMA and SDMA in human urine [1] led to the assumption that renal excretion was the only route for removal of free methylarginines. Indeed, on the assumption that neither re-incorporation nor catabolism occurred, ADMA and SDMA were used as markers of in vivo protein metabolism. However, investigation into the route of elimination of these amino acids showed that urinary excretion of SDMA was 30 times greater than that of either L-NMMA or ADMA in rabbits [23]. This observation led McDermott [24] to propose the existence of a catabolic pathway for L-NMMA and ADMA. A detailed study of the metabolic fates of 14C-labelled ADMA and SDMA in rats confirmed this early notion. The excretion of analogous metabolites of ADMA and SDMA indicated a common catabolic pathway for both dimethylarginines (catalysed by dimethylarginine: pyruvate aminotransferase). However, there appeared to be an additional pathway that specifically metabolised ADMA. This was demonstrated by the identification of metabolites, mainly citrulline, in the tissue samples and plasma of 14C-ADMA- but not 14C-SDMA-injected rats. The enzyme responsible for this specific pathway was subsequently purified from rat kidney and called N G,N G-dimethylarginine dimethylaminohydrolase (DDAH) [25]. Subsequent studies have shown that >90% of ADMA is metabolised by DDAH.
DDAH was shown to specifically hydrolyse ADMA and L-NMMA to yield citrulline and dimethylamine or monomethylamine, respectively. It had no activity towards SDMA. K M values of DDAH for ADMA and L-NMMA were 0.18 mmol/l and 0.36 mmol/l, respectively. Activity was found in kidney, pancreas, liver and brain, and this was consistent with high protein expression as revealed by immunoblotting analyses using a monoclonal antibody in rat tissues [26]. In addition, high concentrations were also found in aorta and immunoexpression clearly existed in neutrophils and macrophages. A study of DDAH expression in rat kidney also revealed co-localisation of DDAH with NOS at several anatomical sites [27]. Thus, the substrate specificity of DDAH and its distribution in NO-generating systems supported the idea that regulation of intracellular ADMA levels by DDAH might in turn regulate NOS activity (Fig. 3).
The functional role of DDAH
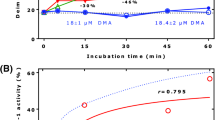
Pharmacological studies using a DDAH inhibitor S-2-amino-4(3-methylguanidino)butanoic acid (4124W; which had no effect on NOS), gave functional significance to this hypothesis [28]. It was shown that 4124W caused the accumulation of endogenously-generated ADMA (but not SDMA) in the supernatant of cultured human endothelial cells. This suggested that ADMA was continuously generated by these cells, and that DDAH acted to prevent its accumulation. In functional studies, 4124W caused endothelium-dependent contraction of rat aortic ring that was reversible by L-arginine. Bradykinin-induced relaxation of human saphenous vein (which is mediated by NO) was also reversed by DDAH inhibition. Further observations showed that 4124W only increased tone in vessels that contained both DDAH and NOS. The vascular effects of 4124W were, therefore, best explained by indirect inhibition of NOS by accumulation of endogenous ADMA, due to inhibition of DDAH.
Cloning of human DDAH isoforms
These observations suggested that DDAH activity was present to ensure that local concentrations of ADMA did not accumulate to inhibit NO generation. The significance of these findings led to the cDNA cloning of human DDAH [29, 30] following the cloning of rat DDAH cDNA [31]. The human cDNA clone contained an 855 bp open reading frame encoding a 285-amino acid protein. The derived amino acid sequence was 93% identical with that of rat [29]. However, prompted by the observation that DDAH activity and DDAH protein expression did not always correlate, we identified a novel human DDAH isoform, named DDAH II [30]. Recombinant expression of this protein confirmed that it was a functional homologue of DDAH (now DDAH I). The open reading frame of the cloned DDAH II cDNA was 63% identical to that of human DDAH I, and the derived amino acid sequence was 62% similar to that of human DDAH I. Recombinantly expressed DDAH II had a K M for L-NMMA of 0.51 mmol/l, comparable to the 0.36 mmol/l obtained for rat DDAH I by Ogawa et al. [25]. These apparently high K M values might suggest that higher intracellular concentrations of methylarginines than those reported (∼5 μmol/l) may be reached under certain conditions. However, these in vitro determinations may not reflect the true in vivo K M values of these enzymes.
Comparison of the mRNA distribution of the human DDAH isoforms with that of the constitutive NOS isoforms in eight adult tissues indicated that DDAH I was most highly expressed in brain and kidney. In these tissues, neuronal NOS (nNOS) expression was apparent in the brain but eNOS was only expressed at a very low level. DDAH II was found to be most highly expressed in heart, placenta and kidney. In heart and placenta, eNOS was also highly expressed while nNOS was not detected. These data raised the possibility of isoform-specific regulation of NOS via modulation of methylarginine concentration [30].
Elucidation of the crystal structure of Pseudomonas aeruginosa DDAH, previously identified by Santa Maria et al. [32], revealed structural similarity with arginine:glycine amidinotransferase [33]. Conservation of a Cys-His-Glu catalytic triad within these enzymes defined a superfamily of arginine-modifying enzymes. The presence of a reactive cysteine residue in the active site also suggested that DDAH activity might be regulated by S-nitrosation of this residue and this was found to be the case. DDAH activity was reversibly inhibited by S-nitrosation of Cys-249 of the enzyme catalytic triad by exogenous and inducible NOS (iNOS)-derived NO [34]. Thus, under conditions where NO production is increased, diminished DDAH activity would be expected to lead to accumulation of ADMA and inhibition of NOS, thus preventing further production of NO. The DDAH structure will also enable the design of selective inhibitors with which to probe the functions of DDAH in vivo. Furthermore, these inhibitors may be of potential clinical use in modulating NOS activity in certain conditions.
ADMA and cardiovascular disease
ADMA is eliminated from the body by a combination of renal excretion and metabolism by DDAH. An increase in plasma ADMA levels was first reported in patients with renal failure [7], a condition in which cardiovascular disease is a major cause of death. In this disease, methylarginine excretion is diminished, and both ADMA and SDMA accumulate in plasma. SDMA levels rise more than ADMA, probably because ADMA levels are reduced by DDAH activity. The rise in ADMA and subsequent inhibition of NO generation has been proposed to be the cause of the hypertension, enhanced atherogenesis and immune dysfunction associated with renal disease. Short-term studies using L-arginine to reverse the competitive inhibition exerted by ADMA on NOS have given conflicting results [35, 36]. However, Zoccali et al. [37] have placed plasma ADMA concentration second only to age as a predictor of mortality and cardiovascular events in patients with chronic renal failure. While impaired renal function may result in raised circulating ADMA levels in chronic renal disease, elevated concentrations of ADMA have been reported in various other cardiovascular and non-cardiovascular conditions [7, 18, 38–61]. In these conditions, dysfunctional metabolism of ADMA by DDAH may provide a mechanism for this accumulation.
In diseases where NO is overproduced, might reduced ADMA levels be the cause? ADMA concentrations have been reported to be significantly lower (by −48%) in patients with Alzheimer’s disease (AD) than in age-matched controls [62]. Increased NO production and elevated oxidative stress have been implicated in brain aging and the pathogenesis of AD. The decrease in ADMA levels observed in AD and with age may provide a mechanism for increased NO production in these processes.
Conclusion
It is becoming increasingly apparent that both the synthesis and metabolism of asymmetric methylarginine is highly regulated. Asymmetric methylarginines are endogenous inhibitors of all isoforms of NOS and are liberated upon proteolysis of proteins that have been methylated by PRMTs. Free methylarginine concentrations are determined in part by the enzymes that metabolise them, i.e. DDAH I and DDAH II, and regulation of NOS activity has been a central focus of DDAH studies. Given the pleiotropic effects of NO in multiple systems, DDAH has the potential to regulate all of these actions of NO through modulation of ADMA levels. Isoform-specific inhibitors and mouse knockouts will be required to conclusively elucidate the physiological and pathophysiological roles of DDAH.
References
Kakimoto Y, Akazawa S (1970) Isolation and identification of N G,N G and N G,N′G dimethyl-arginine, N-epsilon-mono-, di-, and trimethyllysine, and glucosylgalactosyl- and galactosyl-delta-hydroxylysine from human urine. J Biol Chem 245:5751–5758
Palmer RM, Ashton DS, Moncada S (1988) Vascular endothelial cells synthesize nitric oxide from L-arginine. Nature 333:664–666
Rees DD, Palmer RM, Hodson HF, Moncada S (1989) A specific inhibitor of nitric oxide formation from L-arginine attenuates endothelium-dependent relaxation. Br J Pharmacol 96:418–424
Whittle BJ, Lopez-Belmonte J, Rees DD (1989) Modulation of the vasodepressor actions of acetylcholine, bradykinin, substance P and endothelin in the rat by a specific inhibitor of nitric oxide formation. Br J Pharmacol 98:646–652
Aisaka K, Gross SS, Griffith OW, Levi R (1989) N G-methylarginine, an inhibitor of endothelium-derived nitric oxide synthesis, is a potent pressor agent in the guinea pig: does nitric oxide regulate blood pressure in vivo? Biochem Biophys Res Commun 160:881–886
Vallance P, Collier J, Moncada S (1989) Effects of endothelium-derived nitric oxide on peripheral arteriolar tone in man. Lancet 2:997–1000
Vallance P, Leone A, Calver A, Collier J, Moncada S (1992) Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet 339:572–575
Clarke S (1993) Protein methylation. Curr Opin Cell Biol 5:977–983
Aletta JM, Cimato TR, Ettinger MJ (1998) Protein methylation: a signal event in post-translational modification. Trends Biochem Sci 23:89–91
Paik WK, Kim S (1968) Protein methylase I. Purification and properties of the enzyme. J Biol Chem 243:2108–2114
Ghosh SK, Paik WK, Kim S (1988) Purification and molecular identification of two protein methylases I from calf brain. Myelin basic protein- and histone-specific enzyme. J Biol Chem 263:19024–19033
Boffa LC, Karn J, Vidali G, Allfray VG (1977) Distribution of N G,N G-dimethylarginine in nuclear protein fractions. Biochem Biophys Res Commun 74:969–976
Brahms H, Raymackers J, Union A, de Keyser F, Meheus L, Luhrmann R (2000) The C-terminal RG dipeptide repeats of the spliceosomal Sm proteins D1 and D3 contain symmetrical dimethylarginines, which form a major B-cell epitope for anti-Sm autoantibodies. J Biol Chem 275:17122–17129
Baldwin GS, Carnegie PR (1971) Isolation and partial characterization of methylated arginines from the encephalitogenic basic protein of myelin. Biochem J 123:69–74
Miyake M, Kakimoto Y (1976) Synthesis and degradation of methylated proteins of mouse organs: correlation with protein synthesis and degradation. Metabolism 25:885–896
Garlick PJ, Waterlow JC, Swick RW (1976) Measurement of protein turnover in rat liver. Analysis of the complex curve for decay of label in a mixture of proteins. Biochem J 156:657–663
Alberts B, Bray D, Lewis J, Raff M, Roberts K, Watson J (1994) Molecular biology of the cell, 3rd edn. Garland Publishing, New York
Inoue R, Miyake M, Kanazawa A, Sato M, Kakimoto Y (1979) Decrease of 3-methylhistidine and increase of N G,N G -dimethylarginine in the urine of patients with muscular dystrophy. Metabolism 28:801–804
Millward DJ (1970) Protein turnover in skeletal muscle. II. The effect of starvation and a protein-free diet on the synthesis and catabolism of skeletal muscle proteins in comparison to liver. Clin Sci 39:591–603
Goldberg AL, St John AC (1976) Intracellular protein degradation in mammalian and bacterial cells: part 2. Annu Rev Biochem 45:747–803
Dice JF, Walker CD (1979) Protein degradation in metabolic and nutritional disorders. Ciba Found Symp 75:331–350
Parag HA, Raboy B, Kulka RG (1987) Effect of heat shock on protein degradation in mammalian cells: involvement of the ubiquitin system. EMBO J 6:55–61
McDermott JR (1976) Studies on the catabolism of N G-methylarginine, N G,N G-dimethylarginine and N G,N′G-dimethylarginine in the rabbit. Biochem J 154:179–184
Ogawa T, Kimoto M, Watanabe H, Sasaoka K (1987) Metabolism of N G,N G-and N G,N′G -dimethylarginine in rats. Arch Biochem Biophys 252:526–537
Ogawa T, Kimoto M, Sasaoka K (1989) Purification and properties of a new enzyme, N G,N G-dimethylarginine dimethylaminohydrolase, from rat kidney. J Biol Chem 264:10205–10209
Kimoto M, Tsuji H, Ogawa T, Sasaoka K (1993) Detection of N G,N G-dimethylarginine dimethylaminohydrolase in the nitric oxide-generating systems of rats using monoclonal antibody. Arch Biochem Biophys 300:657–662
Tojo A, Welch WJ, Bremer V, Kimoto M, Kimura K, Omata M, Ogawa T, Vallance P, Wilcox C (1997) Colocalization of demethylating enzymes and NOS and functional effects of methylarginines in rat kidney. Kidney Int 52:1593–1601
MacAllister RJ, Parry H, Kimoto M, Ogawa T, Russell R, Hodson H, Whitley G, Vallance P (1996) Regulation of nitric oxide synthesis by dimethylarginine dimethylaminohydrolase. Br J Pharmacol 119:1533–1540
Kimoto M, Miyatake S, Sasagawa T, Yamashita H, Okita M, Oka T, Ogawa T, Tsuji H (1998) Purification, cDNA cloning and expression of human N G,N G-dimethylarginine dimethylaminohydrolase. Eur J Biochem 258:863–868
Leiper JM, Santa Maria J, Chubb A, MacAllister R, Charles I, Whitley G, Vallance P (1999) Identification of two human dimethylarginine dimethyl-aminohydrolases with distinct tissue distributions and homology with microbial arginine deiminases. Biochem J 343:209–214
Kimoto M, Sasakawa T, Tsuji H, Miyatake S, Oka T, Nio N, Ogawa T (1997) Cloning and sequencing of cDNA encoding N G,N G-dimethylarginine dimethylaminohydrolase from rat kidney. Biochim Biophys Acta 1337:6–10
Santa Maria J, Vallance P, Charles IG, Leiper J (1999) Identification of microbial dimethylarginine dimethylaminohydrolase enzymes. Mol Microbiol 33:1278–1279
Adak S, Aulak KS, Stuehr DJ (2002) Direct evidence for nitric oxide production by a nitric-oxide synthase-like protein from Bacillus subtilis. J Biol Chem 277:16167–16171
Murray-Rust J, Leiper J, McAlister M, Phelan J, Tilley S, Santa Maria J, Vallance P, McDonald N (2001) Structural insights into the hydrolysis of cellular nitric oxide synthase inhibitors by dimethylarginine dimethylaminohydrolase. Nat Struct Biol 8:679–683
Leiper J, Murray-Rust J, McDonald N, Vallance P (2002) S-nitrosylation of dimethylarginine dimethylaminohydrolase regulates enzyme activity: further interactions between nitric oxide synthase and dimethylarginine dimethylaminohydrolase. Proc Natl Acad Sci U S A 99:13527–13532
Hand MF, Haynes WG, Webb DJ (1998) Hemodialysis and L-arginine, but not D-arginine, correct renal failure-associated endothelial dysfunction. Kidney Int 53:1068–1077
Cross JM, Donald AE, Kharbanda R, Deanfield J, Woolfson R, MacAllister R (2001) Acute administration of L-arginine does not improve arterial endothelial function in chronic renal failure. Kidney Int 60:2318–2323
Zoccali C, Bode-Böger SM, Mallamaci F, Benedetto F, Tripepi G, Malatino L, Cataliotti A, Bellanuova I, Fermo I, Frölich JC, Böger RH (2001) Plasma concentrations of asymmetrical dimethylarginine and mortality in patients with end-stage renal disease: a prospective study. Lancet 358:2113–2117
Goonasekera CD, Rees DD, Woolard P, Frend A, Shah V, Dillon M (1997) Nitric oxide synthase inhibitors and hypertension in children and adolescents. J Hypertens 15:901–909
Chen BM, Xia LW, Zhao RQ (1997) Determination of N G,N G-dimethylarginine in human plasma by high-performance liquid chromatography. J Chromatogr B 692:467–471
Holden DP, Fickling SA, Whitley GS, Nussey S (1998) Plasma concentrations of asymmetric dimethylarginine, a natural inhibitor of nitric oxide synthase, in normal pregnancy and preeclampsia. Am J Obstet Gynecol 178:551–556
Matsuoka H, Itoh S, Kimoto M, Kohno K, Tamai O, Wada Y, Yasukawa H, Iwami G, Okuda S, Imaizumi T (1997) Asymmetrical dimethylarginine, an endogenous nitric oxide synthase inhibitor, in experimental hypertension. Hypertension 29(1 Pt 2):242–247
Gorenflo M, Zheng C, Werle E, Fiehn W, Ulmer H (2001) Plasma levels of asymmetrical dimethyl-L-arginine in patients with congenital heart disease and pulmonary hypertension. J Cardiovasc Pharmacol 37:489–492
Böger RH, Bode-Böger SM, Kienke S, Stan A, Nafe R, Frölich JC (1998) Dietary L-arginine decreases myointimal cell proliferation and vascular monocyte accumulation in cholesterol-fed rabbits. Atherosclerosis 136:67–77
Böger RH, Bode-Böger SM, Szuba A, Tsao P, Chan J, Tangphao O, Blaschke T, Cooke JP (1998) Asymmetric dimethylarginine (ADMA): a novel risk factor for endothelial dysfunction: its role in hypercholesterolemia. Circulation 98:1842–1847
Bode-Böger SM, Böger RH, Kienke S, Junker W, Frölich JC (1996) Elevated L-arginine/dimethylarginine ratio contributes to enhanced systemic NO production by dietary L-arginine in hypercholesterolemic rabbits. Biochem Biophys Res Commun 219:598–603
Herlitz H, Petersson A, Sigstrom L, Wennmalm A, Westberg G (1997) The arginine-nitric oxide pathway in thrombotic microangiopathy. Scand J Urol Nephrol 31:477–479
Azuma H, Sato J, Hamasaki H, Sugimoto A, Isotani E, Obayashi S (1995) Accumulation of endogenous inhibitors for nitric oxide synthesis and decreased content of L-arginine in regenerated endothelial cells. Br J Pharmacol 115:1001–1004
Usui M, Matsuoka H, Miyazaki H, Udea S, Okuda S, Imaizumi T (1998) Increased endogenous nitric oxide synthase inhibitor in patients with congestive heart failure. Life Sci 62:2425–2430
Feng Q, Lu X, Fortin AJ, Pettersson A, Hedner T, Kline R, Arnold J (1998) Elevation of an endogenous inhibitor of nitric oxide synthesis in experimental congestive heart failure. Cardiovasc Res 37:667–675
Piatti P, Fragasso G, Monti LD, Setola E, Lucotti P, Fermo I, Paroni R, Galluccio E, Pozza G, Chierchia S, Margonato A (2003) Acute intravenous L-arginine infusion decreases endothelin-1 levels and improves endothelial function in patients with angina pectoris and normal coronary arteriograms: correlation with asymmetric dimethylarginine levels. Circulation 107:429–436
Masuda H, Goto M, Tamaoki S, Azuma H (1999) Accelerated intimal hyperplasia and increased endogenous inhibitors for NO synthesis in rabbits with alloxan-induced hyperglycaemia. Br J Pharmacol 126:211–218
Abbasi F, Asagmi T, Cooke JP, Lamendola C, McLaughlin T, Teaven G, Stuehlinger M, Tsao P (2001) Plasma concentrations of asymmetric dimethylarginine are increased in patients with type 2 diabetes mellitus. Am J Cardiol 88:1201–1203
Böger RH, Bode-Böger SM, Sydow K, Heistad D, Lentz S (2000) Plasma concentration of asymmetric dimethylarginine, an endogenous inhibitor of nitric oxide synthase, is elevated in monkeys with hyperhomocyst(e)inemia or hypercholesterolemia. Arterioscler Thromb Vasc Biol 20:1557–1564
Böger RH, Lentz SR, Bode-Böger SM, Knapp H, Haynes W (2001) Elevation of asymmetrical dimethylarginine may mediate endothelial dysfunction during experimental hyperhomocyst(e)inaemia in humans. Clin Sci 100:161–167
Yoo JH, Lee SC (2001) Elevated levels of plasma homocyst(e)ine and asymmetric dimethylarginine in elderly patients with stroke. Atherosclerosis 158:425–430
Masuda H, Tsujii T, Okuno T, Kihara K, Goto M, Azuma H (2001) Involvement of accumulated endogenous NOS inhibitors and decreased NOS activity in the impaired neurogenic relaxation of the rabbit proximal urethra with ischaemia. Br J Pharmacol 133:97–106
Hermenegildo C, Medina P, Peiro M, Segarra G, Vila J, Ortega J, Lluch S (2002) Plasma concentration of asymmetric dimethylarginine, an endogenous inhibitor of nitric oxide synthase, is elevated in hyperthyroid patients. J Clin Endocrinol Metab 87:5636–5640
Das I, Khan NS, Puri BK, Hirsch S (1996) Elevated endogenous nitric oxide synthase inhibitor in schizophrenic plasma may reflect abnormalities in brain nitric oxide production. Neurosci Lett 215:209–211
Rawal N, Lee YJ, Whitaker JN, Park J, Paik W, Kim S (1995) Urinary excretion of N G-dimethylarginines in multiple sclerosis patients: preliminary observations. J Neurol Sci 129:186–191
Fandriks L, von Bothmer C, Johansson B, Holm M, Bolin I, Pettersson A (1997) Water extract of Helicobacter pylori inhibits duodenal mucosal alkaline secretion in anesthetized rats. Gastroenterology 113:1570–1575
Abe T, Tohgi H, Murata T, Isobe C, Sato C (2001) Reduction in asymmetrical dimethylarginine, an endogenous nitric oxide synthase inhibitor, in the cerebrospinal fluid during aging and in patients with Alzheimer’s disease. Neurosci Lett 312:177–179
Acknowledgements
This work was funded by British Heart Foundation Programme grant PG20007.
Note added in proof
Recently Wang et al. (Science 2004; 306:279–283) demonstrated that histone arginine methylation can be reversed by the action of human protein arginine deiminase 4.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leiper, J.M., Vallance, P. The synthesis and metabolism of asymmetric dimethylarginine (ADMA). Eur J Clin Pharmacol 62 (Suppl 1), 33–38 (2006). https://doi.org/10.1007/s00228-005-0013-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-005-0013-y