Abstract
The serological pattern, “anti-HBc alone”, characterized by the presence of antibodies against the core antigen of hepatitis B virus (anti-HBc) as the only marker of hepatitis B, is not rare in a diagnostic setting. Depending on the prevalence of HBV infection and the patient group investigated, 1–31% of positive anti-HBc results are isolated positive findings. Anti-HBc alone is frequently observed in intravenous drug addicts, HIV-infected individuals, patients who are coinfected with HBV and hepatitis C virus, and pregnant women. However, it is not clear how this profile should be interpreted. Several studies have shown that anti-HBc alone is not only compatible with acute and resolved HBV infection but also with chronic infection. The reasons for the lack of HBsAg and anti-HBs in anti-HBc-alone individuals are not clear, but several mechanisms and possibilities have been suggested that could explain this phenomenon, some of which are delineated in this article.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
HBcAg is the most immunogenic hepatitis B virus (HBV) component during infection [1]. It is the nucleocapsid of HBV, a 27-nm particle composed of multiple copies of a single polypeptide (P21) [2]. Despite the fact that HBcAg is an internal component of the virion, high titers of HBc antibody (anti-HBc) are produced in virtually all patients who have been exposed to HBV and usually persist, irrespective of ongoing liver disease or clearance of the virus [2, 3]. The high frequency of anti-HBc production is due, at least in part, to the fact that HBcAg can function as a cell-independent antigen [1]. Thus, during the acute phase of infection, anti-HBc of the IgM class predominates. As the infection evolves, anti-HBc IgM levels gradually decline and anti-HBc IgG can persist with slowly decreasing titers for many years [2, 3]. For this reason, antibodies to the core of hepatitis B virus are considered to be the most reliable serological marker of HBV infection [4] and are very cost-effective, especially if compared to molecular markers [5]. Anti-HBc antibodies are called ‘epidemiological markers’ and are widely employed in HBV screening [5]. Once detected, they will guide to additional tests in order to establish the patient’s clinical status [6]. Some anti-HBc-positive patients also carry the hepatitis B surface antigen (HBsAg), indicating ongoing infection, whereas others have the corresponding antibody (anti-HBs), indicating recovery and immunity [7, 8]. However, in a third group of anti-HBc carriers, neither HBsAg nor anti-HBs is detectable in the serum. Subjects that demonstrate this serological profile are said to be ‘anti-HBc alone’ [9]. Such a serological profile can be encountered in different population groups and may be explained by different mechanisms, as described in this article.
False positivity to anti-HBc
Depending on the anti-HBc test used and the HBV prevalence where the assay is employed, a certain proportion of individuals with ‘anti-HBc alone’ will be false positive [9]. This false reactivity has been attributed to nonspecific reactions associated with competitive anti-HBc enzyme immunoassays (EIAs), cross-reactivity with interfering serum substances or with IgA or IgM-related molecules produced from nonspecific HBV-activated B-lymphocytes [10]. To minimize nonspecific results, modifications have been made by using different HBcAg antibodies (human, mouse-monoclonal), different detection systems (enzymes, fluorescence, chemiluminescence), and changes in the reaction kinetics (incubation steps, temperature, and time). It has been demonstrated that samples that exhibit reactivity around the cutoff values are most likely to be false positives. Therefore, modifications in cutoff calculations or the use of a broader gray-zone have been proposed [11], but not accepted universally. Cross-reactivity can be diminished by treating samples with reducing agents (dithiothreitol [DTT] or potassium bisulfite [MBS]) [12] and by the employment of neutralization assays, which have been shown to significantly improve the specificity of anti-HBc determination [13].
In vivo studies have allowed the evaluation of the specificity of anti-HBc assays. Ural and Findik [14] observed that almost half of ‘anti-HBc alone’ patients developed primary immune response when challenged with the HBV vaccine. Another study in China also demonstrated that among anti-HBc-alone patients, 72.9% developed a primary anti-HBs response [15], suggesting false reactivity to anti-HBc.
Therefore, because false positive results are very frequently observed, it has been recommended that complementary tests should be employed to confirm anti-HBc reactivity. Such strategies involve the use of another EIA test format, the search for another serological marker (HBsAg, anti-HBs or anti-HBe) or the detection of HBV DNA by an amplification method [9, 11, 16].
Chronic carrier with low levels of HBV
It is generally accepted that the diagnosis of HBV infection is based on the detection of serum hepatitis B surface antigen (HBsAg) and that disappearance of this antigen indicates the clearance of HBV and resolution of infection. On the other hand, the persistence of HBsAg suggests a chronic-carrier status [17]. However, several studies have shown that HBV DNA has been frequently detected in patients with chronic liver disease who are negative for HBsAg and positive for antibodies to core antigen [17–19], suggesting that a large number of anti-HBc-positive healthy individuals are ‘latent’ carriers of HBV with ongoing viral replication in the liver tissue. Although little is known about the molecular mechanisms of viral persistence, this finding might reflect the difficulty in eliminating HBV covalently closed circular DNA (cccDNA) from the hepatocyte nucleus, and this defines the HBV chronic-carrier state [19, 20].
The persistence of HBV/DNA in the liver after HBsAg clearance has been demonstrated by molecular techniques (PCR and in situ hybridization), suggesting that viral DNA may exist in a complete form in the hepatocyte. In addition, the presence of extrachromossomal HBV DNA has been detected in some patients, suggesting that latent HBV infection may persist in hepatocytes without production of viral particles [21]. Analysis of liver histopathology by immunohistochemistry in anti-HBc-alone patients has revealed that the expression of HBsAg or HBcAg in liver tissue is comparable to that in chronic HBV carriers, except that the signals are lower. This finding could be due to lower expression levels of the viral proteins and/or to a weaker recognition by the immune system of the antigens produced [22]. Thus, some patients may have already had serological markers, but subsequently lost them, while expressing low levels of HBV replication associated with ongoing liver disease. In summary, some anti-HBc-alone individuals are characterized as HBV carriers when the ‘s’ antigen is not present in the bloodstream years after infection or its low levels limit detection by routinely available commercial assays. In this case, the chronic infection diagnosis must be established through HBV DNA detection by PCR or an alternative nucleic acid amplification procedure with detection limits of 10–100 genomes per ml [9]. The vaccination of these individuals against HBV could be worthwhile for their characterization, since they are unable to produce anti-HBs antibodies [15, 23].
Infection by HBV mutants
Several studies have suggested that point mutations, deletions, or rearrangements in some genes of the HBV genome that interfere with gene expression or lead to the production of antigenically modified ‘s’ proteins may be responsible for the lack of HBsAg detection in the bloodstream.
Infection by mutants of the a-determinant region of hepatitis B surface antigen
The “a” determinant of hepatitis B virus consists of a serologically defined region, located between amino acid residues 124 and 147 of the hepatitis B surface antigen (HBsAg), which induces a protective immune response common to all HBV subtypes [24]. Variations in its primary structure have been demonstrated to markedly alter the antigenic conformation and antigenicity of HBsAg [25]. Variant virus with an amino acid substitution at residue 145 from glycine to arginine (G145R) [26] or lysine to glutamic acid at residue 141 (L141E) [27], amongst others [28, 29], within the “a” determinant, have been identified and may escape protection from vaccine-induced anti-HBs–specific neutralizing antibodies. However, it has been demonstrated that variability in the common “a” determinant not only can favor viral escape from neutralizing antibodies but also reduces in vitro HBsAg detection in routine immunoassays, promoting mutant HBsAg diagnosis escape when HBsAg is established as the only infection marker for HBV infection [25, 30, 31]. These mutations may promote variations in the tertiary structure of HBsAg, hindering the correct formation of disulphide bonds among cysteine residues of the ‘a’ determinant, which alters protein immunological properties, leading to false negative results. Overall, it is also important to emphasize that failure in HBsAg variant detection is due to the antigenic exchanges described above and not because of low HBs Ag levels in the bloodstream, although exchanges may also affect the overlapping polymerase gene and, consequently, viral replication capacity [30].
Infection by mutants of the polymerase gene of hepatitis B virus
Mutations in the polymerase gene may produce changes in the overlapping ‘s’ gene. Similarly, mutations within the ‘s’ gene may produce changes in the overlapping polymerase gene [30]. Therapy with lamivudine (LMV) often results in exchanges in the viral polymerase catalytic center, some of which induce the selection of HBV mutants that are resistant to treatment with this nucleoside analogue, maintaining low levels of replication. These mutations produce exchanges in the overlapping s gene, which results in reduction in HBsAg antigenicity and expression. The most common amongst them affects the YMDD (tyrosine-methionine-aspartate-aspartate) motif, where the methionine (M) residue at amino acid 204 is replaced by isoleucine (rtM204I) or valine (rtM204V), accompanied by a compensatory leucine-to-methionine exchange at codon 180 (rtL180M/M204V) [32]. This mutation produces I195M and W196S exchanges in the HBsAg, which alter the structural integrity of the protein and affect the binding to anti-HBs antibodies present in EIA assays, and consequently its in vitro detection [33]. LMV-resistant mutants often show reduced replication capacity when compared to wild-type virus, and its emergence is associated with the reappearance of DNA/HBV in the serum. Recently, it was demonstrated that two overlapping s gene mutations (sP120T and sG145R) produce exchanges of rtT128N and rtW153Q in the polymerase protein, which were found to partially restore the replication in vitro of the LMV-resistant HBV phenotype, maintaining resistance to the antiviral agent. These exchanges produce a stop codon in the overlapping s gene, resulting in deficient secretion of HBsAg and virus [34]. Other mutations in the polymerase gene have been reported in individuals undergoing antiviral therapy. Such mutations can introduce a stop codon in the surface antigen and include rtM204I (sW194stop) [35, 36] and rt V207I (Sw199stop) [37].
New drugs, such as adefovir, entecavir and tenofovir, have shown efficacy in suppressing viral replication and therefore seem to be promising candidates for treatment of chronic hepatitis B [38]. However, their long-term efficacy in association with their potential to induce mutations has not been widely evaluated [38, 39]. The use of entecavir for LMV-resistant HBV in particular has been questionable, since both drugs may promote HBV mutations by similar mechanisms [40]. Hepatitis B virus resistance to adefovir and tenofovir has also been described. Mutations rtN236T [41] and rtA194T [42] are associated with adefovir and tenefovir resistance, respectively, but do not affect HBsAg expression. However, the mutation rtV191I, which was selected after 24 weeks of adefovir therapy, was shown to simultaneously create a stop codon in the surface antigen (sW182stop), reducing HBsAg levels in the serum [43]. Several HBV mutations associated with drug resistance have been detected and are well-elucidated [44]. There are many other drugs currently under clinical investigation, such as Emtricitabine, Clevudine and Telbivudine [45]. However, new mechanisms of drug resistance will certainly emerge, including those involving changes in the polymerase gene, which may impair secretion, production and/or detection of HBsAg [46, 47].
Infection by mutants of the s-promoter region of hepatitis B virus
Mutations in the HBV regulatory regions can also affect HBsAg secretion and synthesis and lead to the anti-HBc-alone serological profile. The HBV envelope gene is controlled by two different promoters: the pre-S and the S promoter, which regulate transcription of a 2.4- and a 2.1-kb mRNA, respectively. The pre-S promoter is located 5′ of the first in frame ATG of the large (pre-S1) envelope protein. The S-promoter is found in the pre-S gene coding region and is a TATA-less promoter. The two mRNAs transcribed from the S gene code for 3 S-proteins (small, middle, and large) sharing the 226 amino acids at the C-terminus [48]. Deletions in pre-s region can promote S-promoter removal, which blocks HBsAg transcription. This can result in reduction of HBsAg protein synthesis and secretion [49], or even intracellular viral retention, leading to a low concentration of extracellular S gene products in the bloodstream [50] despite active viral replication.
In addition, for appropriate HBV assembly and secretion, a specific ratio between the small and large surface protein is necessary, with the amount of small S-protein predominating [48]. Thus, the reduced synthesis of small surface antigen results in the accumulation of large surface protein in the endoplasmic reticulum, which can only be secreted if small S-protein is present in adequate proportions [51]. On the other hand, overexpression of the large S-protein may result in retention of small S-protein within cells, quantitative decrease of HBsAg in the serum and lack of viral secretion [52]. A single gene-defective HBV population may coexist with a wild-type population, helping in viral rescue. These alterations could be part of a dynamic process in which the existing mutants gradually may die out in order to be replaced by mutants originating from the wild type [48]. This phenomenon may be related with the control of viral replication and the evasion of immune surveillance, which account for occasional life-long persistence of HBV infection and the discrepancy between the presence of HBV DNA and HBsAg in serum [51]. These mutants have been isolated frequently from individuals with persistent viral infection, including those with cirrhosis and hepatocellular carcinoma.
Coinfection with other hepatoviruses
The suppression of HBV replication and its gene expression is known to occur during the late phases of chronic and acute infection and may eventually lead to disappearance of the HBsAg protein in the serum [21, 53]. In the case of HCV/HDV coinfection/superinfection, HBV replication may also be suppressed, leading to the ‘anti-HBc alone’ serostatus.
HBV and HCV are parenterally transmitted and share common routes of infection, and therefore, combined infection may occur, particularly in areas where both agents are endemic and among people or groups with high risk for parenteral infection [54, 55]. Several studies have shown that occult HBV infection can be found in patients with chronic HCV infection [54, 56, 57]. Occult HBV infection is characterized by persistent HBV viremia in HBsAg-negative patients with or without markers of previous infection (anti-HBc and/or anti-HBs) [58]. In spite of the limited knowledge about the mechanisms involved in the absence of circulating HBsAg protein, it has been demonstrated that there is a causal relationship between HCV infection and the absence of non-anti-HBc markers. This relationship is supported by the direct influence of HCV core protein on HBV, which reduces its replication capacity and HBsAg production dramatically and compromises its detection in the serum of co-infected individuals [59]. Consistent with this, Weber et al. [60], in a study involving 104 anti-HBc-alone-positive individuals from a population of high HCV seroprevalence (patients on maintenance dialysis, organ transplant patients, intravenous drug addicts, HIV-infected individuals and HCV-chronic individuals), demonstrated that the isolated anti-HBc reactivity could be due to HCV interference with HBsAg synthesis (65.4%), with consequent establishment of occult infection associated with a viral interference mechanism [61]. In addition, data from other studies have shown that in HBV/HCV coinfected patients, there is low DNA polymerase activity, low levels of HBV DNA in the serum and low levels of HBsAg in the bloodstream, which suggest suppression of HBV replication [62].
Formation of HBsAg-anti-HBs immune complexes
The detection of anti-HBs and anti-HBe antibodies in patients with chronic infection (or acute—in the ‘window phase’) has been difficult due to the presence of excess surface antigen (HBsAg), composed of preS/S and S proteins, and of the hepatitis B e antigen (HBeAg—a secreted form of the nucleoprotein) [63]. The anti-HBs and anti-HBe antibodies produced would be consumed by their corresponding antigens, forming immune complexes that could explain the isolated positivity to anti-HBc [23, 64]. These immune complexes (ICs) cannot be detected by the standardized commercial assays, which usually detect anti-HBs and anti-HBe antibodies only after the corresponding antigens have been cleared from the serum, since dissociation of these complexes is necessary for their detection. Joller-Jemelka et al. [64], in a study aiming to identify whether the dissociation of immune complexes in patients’ serum with ‘anti-HBc alone’ could lead to detection of additional serological markers, showed that 31% of the sera examined had HBsAg in the form of immune complexes and detectable HBV-DNA in plasma. Thus, in the early phase of acute hepatitis B, HBV exists in both forms, free and immunoglobulin-bound, but subsequently there is a shift to the immunoglobulin-bound form due to seroconversion from HBsAg to anti-HBs [65]. In another study, a series of 200 HBeAg-positive serum samples from chronically infected hepatitis B patients were analyzed using novel immunoassays designed to detect antibodies in the presence of excess circulating viral antigens. All patients were seronegative for antibodies directed to envelope antigens and to the secreted nucleoprotein antigen (HBeAg) when the standardized commercial assays were used. In contrast, virtually all chronically infected patients were found to have anti-HBe and anti-envelope antibodies in the form of immune complexes when sera were tested employing more sensitive immunoassays [63].
Low levels of anti-HBs despite immunity to HBV
This serological profile can be found in subjects who have lost their anti-HBs-producing capacity after a long period of infection—years, but most often decades—after resolution of infection, or who have never been able to produce it at a sufficient level for detection [66] despite evidence that T cells can produce a soluble factor that selectively suppresses the production of anti-HBs by B lymphocytes [67].
The occurrence of antibodies directed to the HBs antigen indicates viral clearance and the development of life-long immunity in patients who have recovered from HBV infection. For HBs antigen vaccine recipients, the presence of HBs antibodies signifies protective immunity. However, little is known about the kinetics and regulation of this HBs-specific antibody response in the clinical course of HBV infection and in vaccine recipients [68]. Likewise, the reasons for decreased levels of antibodies after a long period of infection or following vaccination are not very clear. Several immunological mechanisms that could explain a deficient anti-HBs production have been discussed in detail by Milich and Leroux-Roels [69]. One of them is associated with low HBsAg imunogenicity at the T-cell level. Being a strictly T-cell-dependent immunogen, HBsAg could not be able to induce a strong and long-lasting immune response [69, 70]. However, some studies have demonstrated that T cell memory to HBsAg can be detected by lymphocyte proliferation many years after HBV vaccination, even in the majority of individuals with serum anti-HBs < 10UI/L. This means that protective antibodies could reappear rapidly or that effector cytotoxic T cells could rapidly eliminate virus-infected hepatocytes after exposure to HBV [71]. Bocher et al. [72] observed that patients with acute self-limiting HBV infection had high levels of HBs-specific B cells, despite undetectable anti-HBs serum antibodies. In addition, Bauer and Jilg [73] have shown significant numbers of HBsAg-specific memory T and B cells in vaccine recipients, suggesting that these memory T cells are able to trigger anti-HBs production by B cells once they are activated by revaccination [73]. These findings suggest that despite undetectable anti-HBs serum antibodies, it is possible that the HBsAg-specific T cell immune response plays an important role in protecting against hepatitis B virus infection and that immunological memory persists beyond the time at which anti-HBs levels are no longer detectable and is able to protect against clinically relevant disease. In the case of HBV exposure, the immune memory rapidly leads to a vigorous anamnestic response, which often prevents acute infection and, most often, acute disease and prolonged viremia.
An additional explanation for the “anti-HBc alone” profile in the scenario of low titers of anti-HBs antibodies is that they can escape detection by the commercially available assays. The EIAs are not adjusted to detect such low levels, since any increase in sensitivity carries the risk of false positivity. Thus, results also depend on assay sensitivity, which is arbitrarily determined by different manufacturers. Greub et al. [74] demonstrated that samples from vaccinated individuals were anti-HBs negative when analyzed in a first assay, and subsequently showed positive results in, respectively, 25, 35 and 38% of the cases when a second, third and fourth assay were used. In this study, it was demonstrated that samples from individuals characterized as ‘non-responders’ and vaccinated individuals that had has lost anti-HBs showed significantly higher absorbances than those observed in the group that had not been vaccinated (control). Such findings suggest that subliminal levels of anti-HBs may be present in ‘non-responders’ and vaccinated individuals who have lost anti-HBs, and despite the non-detection by commercially available assays, such subjects may be protected [74, 75]. Regarding susceptibility to HBV re-infection, it is probable that individuals with “anti-HBc alone” as a sign of late immunity do not differ from those who also carry anti-HBs antibodies. Despite the lack of such antibodies, individuals seem to be protected against reinfection by cellular immune mechanisms and immunological memory.
Significance of “anti-HBc alone” in different geographical contexts
The significance of ‘anti-HBc alone’ varies markedly according to the prevalence of HBV infection in a given region. Hepatitis B virus is highly endemic in certain developing regions, such as South East Asia, China, sub-Saharan Africa and the Amazon Basin, where at least 8% of the population are HBV chronic carriers. In these areas, 70–95% of the population shows past or present serological evidence of HBV infection [76]. Most infections occur during infancy or childhood. Hepatitis B is moderately endemic in part of Eastern and Southern Europe, Japan and part of South America. Between 10 and 60% of the population show evidence of infection, and 2–7% are chronic carriers [76, 77]. The endemicity of HBV is low in most developed areas, such as North America, Northern and Western Europe and Australia. In these regions, HBV infects 5–7% of the population, and only 0.5–2.0% of the population are chronic carriers [76, 77]. In areas with low endemicity, such as most parts of Europe and United States, “anti-HBc alone” is found in 10–20% of all individuals with HBV markers. In about 10% of these individuals, HBV DNA is detected by PCR [9]. Lower prevalence, 0.08 and 1.5%, has been reported in the UK and Germany, respectively, with the percentage of samples containing HBV DNA ranging between 0 and 7.7% [78]. In areas with a higher prevalence of HBV infection, such as Greece (15.8%), China (70%) and Ghana (83.6%), the frequency of DNA-positive results in anti-HBc-alone patients tends to increase to 1.9, 2.7 and 12.7%, respectively [78, 79]. As in highly endemic countries, the majority of infections are contracted perinatally or in early childhood, a higher proportion of the infected adults have late chronic HBV with undetectable HBsAg [80], suggesting that the prevalence of ‘anti-HBc alone’ and the proportion of individuals with HBV DNA might be higher in areas with intermediate and high hepatitis B endemicity [9]. However, it should be noted that there has been a great disparity in reported rates among various studies carried out in these areas [81–86], and it has been difficult to elucidate such results for several reasons, such as differences in the epidemiology of the tested populations, sample selection criteria for PCR testing, and differences in sensitivity and specificity of NAT methods, which promote a great disparity in HBV DNA results [87]. Additionally, the analysis of ‘anti-HBc alone’ prevalence among reports is often difficult because of the low specificity associated with anti-HBc screening and of the algorithms applied to identify true reactivity [78].
Suggested algorithm for investigation of the “anti-HBc alone” pattern
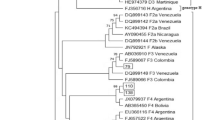
Once the anti-HBc-alone serologic profile is detected, false-positive reactivity should be ruled out by a second anti-HBc test. It is also suggested to test for anti-HBe antibodies. In one-third of the cases, anti-HBe antibodies are also present, representing a good confirming test for hepatitis B infection. Once the anti-HBc-alone profile is confirmed, anti-HBs should be tested after another 1–3 months. If positive, this suggests that the initial testing had been performed during the “window period”. If the anti-HBs test is negative, the presence of viral DNA should be investigated by highly sensitive amplification methods, such as PCR, and if viral DNA is detected, this points to a possible chronic HBV infection. If HBV DNA is negative, HBV vaccination is suggested to test for “late immunity”, which is characterized by the presence of serum anti-HBs antibodies within 1–2 weeks [88]. If these antibodies are not detected after vaccination, chronic hepatitis B infection should be suspected (Fig. 1).
(1) A different ELISA assay format is recommended. (2) It is also recommended that HCV coinfection should be investigated, especially in high-risk individuals such as haemodialysis patients, organ transplant recipients, intravenous drugs addicts, HIV-infected individuals, in whom HCV seroprevalence is also high. Concurrent HCV infection interferes with HBV replication, favoring the HBV chronic-carrier state with undetectable HBsAg. (3) An HBV DNA test with sensitivity of 10–100 genomes/ml should be employed. (4) Individuals should be tested for alanine aminotransferase activity (ALT). In the case of a clearly elevated ALT level, a biopsy seems appropriate to guide therapy. (5) Individuals with positive HBV DNA and normal ALT values should be assessed in yearly intervals. (6) This approach, named “Diagnostic HBV-Vaccine Booster”, attempts to stimulate immunological memory. (7) The presence of anti-HBs at high levels suggests a secondary response
The vaccination approach, named “Diagnostic HBV—Vaccine Booster” attempts to stimulate immunological memory. HBV-immune individuals with undetectable levels of anti-HBs antibodies will develop a strong secondary immune response after the first dose of hepatitis B vaccine. On the other hand, chronic low-level HBV carriers, when challenged by vaccination, are not able to produce anti-HBs antibodies after vaccine doses at 0, 1 and 6 months [15, 23, 89]. In subjects who develop a primary response to hepatitis B vaccine, the isolated anti-HBc positivity is presumably a false positive result [89].
Conclusion
Isolated reactivity to anti-HBc, is a frequent and common laboratory finding that is observed during serological blood donor screening and routine serological assays in the clinical laboratory. In the context of this serological profile, the detection of this marker can represent a false-positive result, but it can also be indicative of acute infection in the window phase. On the other hand, ‘anti-HBc alone’ can represent a resolved infection or even a chronic infection. Other possibilities are not easily distinguished by routine serological testing, but they can have clinical implications and important consequences, particularly in chronic infection with HBV mutants when HBsAg cannot be detected. HBV vaccination has been an efficient strategy for the diagnosis and management of patients with isolated reactivity to anti-HBc, separating low-level anti-HBs individuals with resolved infection from those chronically infected with undetectable HBV DNA.
The adoption of highly sensitive genome-amplification techniques for detection of viral nucleic acid and sequencing has allowed the identification of HBV chronic carriers and HBV mutants that can escape diagnosis by currently employed immunoassay methods. It is expected that with the advent of the next generation of immunoassays and molecular techniques of higher sensitivity and specificity, new serological and molecular patterns will be identified. These profiles may be able to characterize different infection phases and even revise the current clinical concepts of HBV infection.
References
Milich DR, McLachlan A (1986) The nucleocapsid of hepatitis B virus is both a T-cell-independent and a T-cell-dependent antigen. Science 234:1398–1401
Milich DR, Salberg M, Maruyama T (1995) The humoral immune response in acute and chronic hepatitis B virus infection. Springer Semin Immunopathol 17:140–166
Jung M-C, Pape GR (2002) Immunology of hepatitis B infection. Lancet 2(1):43–50
Laperche S, Guitton C, Smilovici W, Courouce AM (2001) Blood donors infected with the hepatitis B virus but persistently lacking antibodies to the hepatitis B core antigen. Vox Sang 80:90–94
Busch MP (2004) Should HBV DNA NAT replace HBsAg and/or anti-HBc screening of blood donors? Tranfus Clin Biol 11(1):26–32
Alhababi F, Sallam T, Tong C (2003) The significance of ‘anti-HBc alone’ in the clinical virology laboratory. J Clin Virol 27:162–169
Chan H (2002) Changing scene in hepatitis B serology interpretation. Hosp Med 63(1):16–19
Greub G, Frei PC (2001) Presence of low levels on anti-HBs antibody in so-called ‘anti-HBc alone’ subjects. Liver 21:380–383
Grob JP, Jilg W, Bornhak H, Gerken G, Gerlich W, Gunther S, Hess G, Hudig H, Kitchen A, Margolis H, Michel G, Trepo C, Will H, Zanetti A, Mushahwar I (2000) Serological pattern ‘anti-HBc Alone’: report on a workshop. J Med Virol 62:450–455
Weber B, Melchior W, Gehrke R, Doerr HW, Berger A, Rabenau H (2001) Hepatitis B virus markers in Anti-HBc only positive individuals. J Med Virol 64:312–319
Westh H, Hoffmann S, Christian E, Worm AM (1996) Hepatitis B core antibody screening in a high prevalence group: comparison of the three enzyme immunoassays using receiver operating characteristic analysis. J Virol Med 56(1):13–18
Weber B, Michl U, Muhlbacher A, Paggi G, Bossi V (1998) Evaluation of the new automated enzymun-test anti-HBc plus for the detection of hepatitis B virus core antibody. Intervirology 41(1):17–23
Weare JA, Robertson EF, Madsen G, Hu R, Decker RH (1991) Improvement in the specificity of assays for detection of antibody to hepatitis B core antigen. J Clin Microbiol 29(3):600–604
Ural O, Findik D (2001) The response of isolated anti-HBc positive subjects to recombinant hepatitis B vaccine. J Infect 43(3):187–190
Lai C-L, Johnson Y, Yeoh E-K, Chang W-K, Lin H-J (1992) Significance of Isolated Anti-HBc Seropositivity by ELISA: implications and the role of radioimmunoassay. J Med Virol 36:180–183
Rodriguez JC, García DG, Teruel AB, Lorenz NF, Espeja AG (2005) Significado de la reactividad aislada anti-HBc como único marcador de infeccíon de la hepatitis B. Enferm Infecc Microbiol Clin 23(1):80–85
Marusawa H, Uemoto S, Hijikata M, Ueda Y, Tanaka K, Shimotohno K, Chiba T (2000) Latent hepatitis B virus infection in healthy individuals with antibodies to hepatitis B core antigen. Hepatology 31(2):488–495
Noborg U, Anki G, Horal P, Magnus L (2000) Levels of viraemia in subjects with serological markers of past or chronic hepatitis B virus infection. Scand J Infect Dis 32:249–252
Bréchot C, Thiers V, Kremsdorf D, Nalpas B, Pol S, Bréchot P (2001) Persistent hepatitis B virus infection in subjects without hepatitis B surface antigen: clinically significant or purely “occult”? Hepatology 1(34):194–203
Zoulim F (2005) New insight on hepatitis B virus persistence from the study of intrahepatic viral cccDNA. J Hepatol 42:302–308
Loriot M-A, Marcellin P, Walker F, Boyer N, Degott C, Randrianatoavina I, Benhamou JP, Erlinger S (1997) Persistence of hepatitis B Virus DNA in serum and Liver from patients with chronic hepatitis B after Loss of HBsAg. J Hepatol 27:251–258
Chemin I, Zoulim F, Merle P, Arkhis A, Chevallier M, Kay A, Cova L, Chevalier P, Mandrand B, Trépo C (2001) High incidence of hepatitis B infections among chronic hepatitis cases of unknown aetiology. J Hepatol 34:447–454
Zuckerman AJ, Zuckerman JN (2000) Current topics in hepatitis B. J Infect 41:130–136
Weber B (2004) The diagnostic and clinical impact of the genetic variability of the s gene of hepatitis B virus. J Lab Med 28(1):56–69
Tonekaboni SS, Waters J, Jeffers S, Gehrke R, Ofenloch B, Horsch A, Hess G, Howard C, Karayiannis P (2000) Effect of variation in the common ‘a’ determinant on the antigenicity of hepatitis B surface antigen. J Med Virol 60:113–121
Carman WF, Zanetti AR, Karayiannis P, Waters J, Manzillop G, Tanzi E, Zuckerman AJ, Thomas HC (1990) Vaccine-induced escape mutant of hepatitis B virus. Lancet 336:325–329
Karthiguesu V, Allison L, Fortuin M, Mendy M, Whittle H, Howard C (1994) A novel hepatitis B virus in the sera of immunized children. J Gen Virol 75:443–448
Jongerius J, Cuypers H, Van Oostendorp W, Lelie PN, Van der Poel CL, Leeuwen EF (1998) New hepatitis B virus mutant form in a blood donor that in undetectable in several hepatitis B surface antigen screening assays. Transfusion 38:56–59
Grethe S, Monazahian M, Bohme I, Thomsen R (1998) Characterization of unusual escape variants of hepatitis B virus isolated from a hepatitis B surface antigen-negative subject. J Virol 9(72):7692–7696
Weinberger KM, Bauer T, Bohm S, Jilg W (2000) High genetic variability of the group-specific a-determinant of hepatitis B virus surface antigen (HBsAg) and the corresponding fragment of the viral polymerase in chronic virus carriers lacking detectable HBsAg in serum. J Gen Virol 81:1165–1174
Carman WF, Korula J, Wallace L, MacPhee R, Mimms L, Decker R (1995) Fulminant reactivation of hepatitis B virus due to envelope protein mutant that escaped detection by monoclonal HBsAg ELISA. Lancet 345:1406–1407
Stuyver L, Locarnini S, Lok A, Richman D, Carman W, Dienstag J (2001) Nomenclature for antiviral-resistant human hepatitis B virus mutations in the polymerase region. Hepatology 33:751–757
Torresi J (2002) The virological and clinical significance of mutations in the overlapping envelope and polymerase genes of hepatitis B virus. J Clin Virol 25(2):97–106
Torresi J, Erneste-Silveira L, Civitico G, Walters T, Lewin S, Fyfe J, Locarnini S, Manns M, Trautwein C, Bock T (2002) Restoration of replication phenotype of lamivudine-resistant Hepatitis B mutants by compensatory changes in the fingers subdomain of the viral polymerase selected as a consequence of mutations in the overlapping S gene. Virology 299(1):88–99
Wakil SM, Kazim SN, Khan LA (2002) Prevalence and profile of mutations associated with lamivudine therapy in Indian patients with chronic hepatitis B in the surface and polymerase genes of hepatitis B virus. J Med Virol 68:311–318
Pichoud C, Seigneres B, Wang Z, Trepo C, Zoulim F (1999) Transient selection of a hepatitis B virus polymerase gene mutant associated with a decreased replication capacity and famciclovir resistance. Hepatology 29:230–237
Xiong X, Yang H, Westland CE, Zou R, Gibbs CS (2000) In vitro evaluation of hepatitis B virus polymerase mutations associated with famciclovir resistance. Hepatology 31:219–224
Krastev AZ (2006) The “return” of hepatitis B. W J Gastroenterol 12(44):7081–7086
Pastor R, Habersetzer F, Fafi-Kremer S, Doffoel M, Baumert Tf, Gut J-P, Stoll-Keller F, Schvoerer E (2009) Hepatitis B virus mutations potentially conferring adefovir/tenofovir resistance in treatment-naïve patients. W J Gastroenterol 15(6):753-755.
Nagasaki F, Niitsuma H, Ueno Y, Imoue J, Kogure T, Fukushima K, Shimisegawa T (2007) The high incidence of the emergence of entecavir-resistant mutant among patients infected with Lamivudine-resistant hepatitis B virus. Tohoku J Exp Med 213:181–186
Angus P, Vaughan R, Yiong S, Yang H, Delaney W, Gibbs C, Brosgart C, Colledge D, Edwards R, Ayres A, Bartholomeusz A, Locarnini S (2003) Resistance to adefovir dipivoxil therapy associated with the selection of a novel mutations in the HBV polymerase. Gastroenterology 125:292–297
Sheldon J, Camino N, Rodes B (2005) Selection of hepatitis B virus polymerase mutations in HIV-coinfected patients treated with tenefovir. Antivir Ther 10:727–734
Yang H, Westland CE, Delaney W (2002) Resistance surveillance in chronic hepatitis B patients treated with adefovir dipivoxil for up to 60 weeks. Hepatotlogy 36:464–473
Baumert TF, Blum HE (2005) Hepatitis B virus mutations: molecular biology and clinical relevance. Vir Rev 6:177–192
Baumert TF, Thimme R, von Weizsacker F (2007) Pathogenesis of hepatitis B virus infection. W J Gastroenterol 13(1):82–90
Kazim SN, Sarin SK, Sharme BC, Khan LA, Hasnain SE (2006) Characterization of naturally occurring and lamivudine-induced surface gene mutations of hepatitis B virus in patients with chronic hepatitis B in India. Intervirol 49:152–160
Sheldon J, Ròdes B, Zoulim F, Bartholomeusz A, Soriano V (2006) Mutations affecting the replication capacity of the hepatitis B virus. J Virol Hep 13:427–434
Bock C, Tillmann H, Manns M, Trautwein C (1999) The pre-S region determines the intracellular localization and appearance of hepatitis B virus. Hepatology 30(2):517–525
Melegari M, Pier PS, Wands JR (1997) The small envelope protein is required for secretions of a naturally occurring Hepatitis B virus mutant with Pre-S1 deleted. J Virol 7(71):5449–5454
Bock C, Tillman H, Maschek H, Manns M, Trautwein C (1997) A pre-S mutation isolated from a patient with chronic hepatitis B infection leads to virus retention and misassembly. Gastroenterology 113:1976–1982
Lee S-Y, Choi MS, Lee D, Lee H, Koh KC, Paik SW, Yoo BC (2005) Overlapping gene mutations of hepatitis B virus in a chronic hepatitis B patient with hepatitis B surface antigen loss during lamivudine therapy. J Korean Med Sci 20:433–437
Sengupta S, Rehman S, Durgapal H, Acharya S, Panda S (2007) Role of surface promoter mutations in hepatitis B surface antigen production and secretion in occult hepatitis B virus infection. J Med Virol 79:220–228
Blackberg J, Kidd-Ljunggren K (2000) Occult hepatitis B virus after acute self-limited infection persisting for 30 years without sequence variation. J Hepatol 33:992–997
Squadrito G, Orlando M, Pollicino T, Raffa G, Restuccia T, Cacciola I, Di Marco V, Picciotto A, Colucci G, Craxi A, Raimondo G (2002) Virological profiles in patients with chronic hepatitis C and overt or occult HBV infection. Am J Gastroenterol 97(6):1518–1523
Otedo AE, McLigeyo SO, Okoth FA, Kayima JK (2003) Seroprevalence of hepatitis B and C in maintenance dialysis in a public hospital in a developing country. S Afr Med J 93(5):380–384
De-Maria N, Colantoni A, Friedlander L, Leandro G, Idilman R, Harig J, Van Thiel DH (2000) The impact of previous HBV infection on the course of chronic hepatitis C. Am J Gastroenterol 95(12):3529–3536
Fukuda R, Ishimura N, Niigaki M, Hamamoto S, Satoh S, Tanaka S, Kushiyama Y, Uchida Y, Ihihara S, Akagi S, Watanabe M, Kinoshita Y (1999) Serologically silent hepatitis B virus coinfection in patients with hepatitis C virus-associated chronic liver disease: clinical and virological significance. J Med Virol 58(3):201–207
Raimondo G, Pollicino T, Cacciola I, Squadrito G (2007) Occult hepatitis B virus infection. J Hepatol 46:160–170
Inigo R, Mariscal L, Bartolomé J, Castillo I, Navacerrada C, Movilla N, Pardo M, Carrero V (2003) Distribution of hepatitis B virus in the liver of chronic hepatitis C patients with occult hepatitis B virus infection. J Med Virol 70:571–580
Weber B, Melchior W, Gehrke R, Doerr WH, Berger A, Rabenau H (2001) Hepatitis B virus markers in anti-HBc only positive individuals. J Med Virol 64:312–319
Schuttler C, Fiedler N, Schmidt K, Repp R, Gerlich WH, Schaefer S (2002) Suppression of hepatitis B virus enhancer 1 e 2 by hepatitis C virus core protein. J Hepatol 37(6):855–862
Lusida MI, Sakugawa H, Motroko N-F, Muluanto S, Handajani R, Boediwarsono, Setiawan PB, Nidom CA, Ohgimoto S and Hotta H (2003) Genotype and Subtype Analyses of Hepatitis B Vírus (HBV) and Possible Co-Infection of HBV and Hepatitis C Virus (HCV) or Hepatitis D Vírus (HDV) in Blood Donors, Patients with Chronic Liver Disease and Patients on Hemodialysis is Surabaya, Indonesia. Microbiol Immunol 47(12):969-975
Maruyama T, McLachlan A, Iino S, Koike K, Kurokawa K, Milich DR (1993) The serology of chronic hepatitis B infection revisited. J Clin Invest 91:2586–2595
Joller-Jemelka HI, Wicki AN, Grob P (1994) Detection of HBs antigen in ‘anti-HBc alone’ positive sera. J Hepatol 21(2):269–272
Yotsuyanagi H, Yasuda K, Iino S, Moriya K, Shintani Y, Fujioe H, Tsutsumi T, Kimura S, Koike K (1998) Persistent viremia after recovery from self-limited acute hepatitis B. Hepatology 27(5):1377–1382
Greub G, Frei P (2001) Presence of low levels of anti-HBs antibody in so-called ‘anti-HBc alone’ subjects. Liver 21:380–383
Yamauchi K, Nakanishi T, Chiou S-S, Obata H (1998) Suppression of hepatitis B antibody synthesis by factor made by T cells from chronic hepatitis B carriers. Lancet 1:324–326
Bocher WO, Herzog-Hauff S, Schlaak J, Meyer zum Buschenfeld K, Lohr HF (1999) Kinetics of hepatitis B surface antigen-specific immune responses in acute and chronic hepatitis B or after HBs vaccination: stimulation of the in vitro antibody response by interferon gamma. Hepatology 29(1):238–244
Milich DR, Leroux-Roels GG (2003) Immunogenetics of the response to HBsAg vaccination. Autoimmun Rev 2(5):248–257
Desombere I, Willems A, Gijbels Y, Leroux-Roels G (2006) Partial delipidation improves the T-cell antigenicity of hepatitis B virus surface antigen. J Virol 80(7):3506–3514
Wang R-X, Boland G, Hattum J, de Gast GC (2004) Long term persistence of T cell memory to HBsAg after hepatitis B vaccination. World J Gastroenterol 10(2):260–263
Bocher B, Herzog-Hauff S, Herr W, Heermann K, Gerken G, Meyer ZUMB, Lohr HF (1996) Regulation of the neutralizing anti-hepatitis B surface (HBs) antibody response in vitro in HBs vaccine recipients and patients with acute or chronic hepatitis B virus (HBV) infection. Clin Exp Immunol 105(1):52–58
Bauer T, Jilg W (2006) Hepatitis B surface antigen-specific T and B cell memory in individuals who had lost protective antibodies after hepatitis B vaccination. Vaccine 24(5):572–577
Greub G, Zysset F, Genton B, Spertini F, Frei PC (2001) Absence of anti-hepatitis B surface antibody after vaccination does not necessarily mean absence of immune response. Med Microbiol Immunol (Berl) 189(3):165–168
Heijtink RA, Schneeberger PM, Postma B, Crombach W (2002) Anti-HBs levels after hepatitis B immunization depend on test reagents: routinely determined 10 and 100 IU/L seroprotection levels unreliable. Vaccine 20(23/24):2899–2905
Hou J, Lui Z, Gu F (2005) Epidemiology and prevention of hepatitis B virus infection. Int J Med Sci 2(1):50–57
Kao JH, Chen DS (2002) Global control of hepatitis B virus infection. Lancet 2:395–403
Allain J-P (2004) Occult hepatitis B virus infection: implications in transfusion. Vox Sang 86:83–91
Zervou EK, Dalekos GN, Boumba DS, Tsianos EV (2001) Value of anti-HBc screening of blood donors for prevention of HBV infection: results of a 3-years prospective study in Northwestern Greece. Transfusion 41:652–658
Liu C-J, Chen D-S, Chen P-J (2006) Epidemiology of HBV infection in Asian blood donors: emphasis on occult HBV infection ant the role of NAT. J Clin Virol 36:S33–S44
Wang JT, Wang TH, Lee C-Z, Chen P-J, Wang T-H, Chen D-S (2002) Transfusion-transmitted HBV infection in an endemic area: the necessity of more sensitive screening for HBV carriers. Transfusion 42:1592–1597
Arraes LC, Ximenez R, Andrieu J-M, Lu-W, Barreto S, Pereira LM, Castelo A (2003) The biological meaning of anti-HBc positive in blood donors: Relation to HBV-DNA and to other serological markers. Rev Inst Med Trop S Paulo 45(3):137–140
García-Montalvo B, Farfán-Ale J, Acosta-Viana K, Puerto-Manzano F (2005) Hepatitis B virus DNA in blood donors with anti-HBc as a possible indicator of active hepatitis B virus infection in Yucatan, México. Transfus Med 15(5):371–378
Ramia S, Ramlawi F, Kanaan M, Klayme S, Naman R (2005) Frequency and significance of antibodies against hepatitis B core (anti-HBc) antigen as the only serological marker for hepatitis B infection in Lebanese blood donors. Epidemiol Infect 133(4):695–699
Behzad-Behbahani A, Mafi-Nejad A, Tabei SZ, Lankarani KB, Torab A, Moaddeb A (2006) Anti-HBc & HBV-DNA detection in blood donors negative for hepatitis B virus surface antigen in reducing risk of transfusion associated HBV infection. Indian J Med Res 123(1):37–42
Banerjee A, Chandra P, Datta S, Biswas A, Bhattacharya P, Chakraborty S, Chakrabarti S, Bhattacharya S, Chakrabarty R (2007) Frequency and significance of hepatitis B virus surface gene variant circulating among ‘anti-HBc only’ individuals in Eastern India. J Clin Virol 40:312–317
Kleinman S, Kuhns M, Todd D, Glynn S, McManara A, DiMarco A, Busch M (2003) Frequency of HBV DNA detection in US blood donors testing positive for the presence of anti-HBc: implications for transfusion transmission and donor screening. Transfusion 43:696–704
Sciariada L, Grando D, Lochato A, Magni E (1991) Immune response to hepatitis B vaccine in persons with “anti-HBcAlone”. In: Hollinger FB, Lemon SM, Margolis HS (eds) Proceedings of the 1990 international symposium on viral hepatitis and liver disease: viral hepatitis and liver disease. Willians & Wilkins, pp 782–784
Sunbul M, Leblebicioglu H, Esen S, Eroglu C, Barut S (2000) Response to hepatitis B vaccine in HBsAg/Anti-HBs negative and anti-HBc positive subjects. Scan J Infect Dis 32:315–316
Acknowledgment
The authors thank the editors and reviewers for their helpful comments and suggestions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pondé, R.A.A., Cardoso, D.D.P. & Ferro, M.O. The underlying mechanisms for the ‘anti-HBc alone’ serological profile. Arch Virol 155, 149–158 (2010). https://doi.org/10.1007/s00705-009-0559-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-009-0559-6