Abstract
Purpose
Early diagnosis and treatment of scaphoid fractures is critical to achieve union and prevent wrist degenerative arthritis. Plain radiographic measurements can guide the early approach to suspected fractures. Specifically, the ability to predict fracture or fracture stability from plain radiographs may allow the traumatologist to expand initial referral to three-dimensional imaging. We evaluated the ability of four measured angles to predict presence of a scaphoid fracture and stability.
Methods
Fifty patients with a scaphoid fracture and 50 patients without fracture were evaluated for the cortical ring sign, scapho-lunate gapping, lateral scapholunate (SL), radio-scaphoid (RS), radio-lunate (RL), and radio-capitate (RC) angles by two-blinded observers.
Results
Measurement of an increased SL interval was associated with the presence of a scaphoid fracture as diagnosed on three-dimensional imaging [odds ratio (OR) 3.0, confidence interval (CI) 1.53–5.87, p = < 0.01]. The measured RL angle was associated with fracture displacement (OR 1.13, 95% CI 1.02–1.25, p = 0.02).
Conclusions
Scapholunate gapping on plain radiographs in the context of a clinically suspected scaphoid fracture should increase suspicion for a fracture and may prompt earlier 3-dimensional imaging, while the presence of an abnormal radiolunate angle should increase wariness for instability and can be used in preoperative planning.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Scaphoid fractures are the most common carpal bone fracture accounting for 2% of all fractures and 60–90% of all carpal fractures [1]. Despite their high incidence they are often a difficult fracture to both diagnose and treat. The scaphoid's tenuous blood supply and presence of vascular watershed area as well as instability of the fracture fragments create a poor fracture healing environment that can cause difficulties with union in both displaced and nondisplaced scaphoid fractures. Those fractures that go undiagnosed, entail significant associated instability, or have a delay in treatment, have an increased risk of nonunion which can result in eventual degenerative arthritis of the wrist. Early diagnosis and treatment of scaphoid fractures is therefore imperative to best achieve union and prevent resultant carpal instability, nonunion, and degenerative arthritis of the wrist [2]. Though three-dimensional imaging is often used for diagnosis, the initial evaluation includes a plain radiograph of the wrist. If certain measurements on a plain radiograph could predict the presence and/or displacement of a scaphoid fracture and associated instability, our ability to diagnose these fractures early and therefore treat expediently could be enhanced.
There are multiple described radiographic signs of carpal instability. These include increase in the scapholunate (SL), radio-lunate (RL), and capito-lunate angles on lateral radiographs of the wrist [3, 4]. The presence of a cortical ring sign has also been thought to signal carpal instability however, its presence has been found in up to 17–25% of normal wrist radiographs [5, 6]. As stated, scaphoid fractures with signs of associated carpal instability have been considered unstable fractures and carry an elevated risk of nonunion and other complications. Considering this data, it is uncertain how radiographic signs of carpal instability in scaphoid fractures should be interpreted. Furthermore, though some studies have evaluated the associations between radiographic measurements and scaphoid malunion or nonunion, it is unclear how helpful these measurements are in diagnosing a suspected and or displaced scaphoid fracture. We aimed to evaluate the effectiveness of four measured angles (lateral scapho-lunate, radio-scaphoid, radio-lunate, and radio-capitate angles) and the cortical ring sign, in predicting the presence of a scaphoid fracture and of fracture displacement/instability. We hypothesized that measurements used to evaluate wrist alignment will not predict the presence or absence of a fracture but will predict the presence of fracture displacement. Since early diagnosis and treatment of a scaphoid fracture is vital in preventing nonunion and subsequent wrist arthritis, an understanding of the ability for radiographic measurements to predict fracture and fracture instability would aid in the initial approach to suspected scaphoid fractures.
Methods
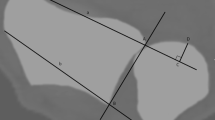
Six hundred radiographs performed for a suspected scaphoid fracture were reviewed. Of these, fifty cases were diagnosed as a scaphoid fracture by three-dimensional (3D) imaging and eligible for analysis (8%). Analysis of wrist radiographs performed as standard of care for 50 patients with the diagnosis of a scaphoid fracture and 50 patients with no 3D diagnosis of scaphoid fracture between 06/23/2014 and 08/16/2021 was performed. We included only cases with concurrent three-dimensional imaging, either magnetic resonance imaging (MRI) or computed tomography (CT) scan. Exclusion criteria for the scaphoid fracture cohort included radiographs of poor quality or scans with pathology other than a scaphoid fracture. Exclusion criteria for the normal radiographic cohort included radiographs of poor quality or scans with any wrist pathology. Both posteroanterior (PA and lateral plain radiographs of the wrist were used to assess for the presence of a cortical ring sign and to measure the lateral scapho-lunate (SL), radio-scaphoid (RS), radio-lunate (RL), and radio-capitate (RC) angles. Two-blinded observers performed the measurements. Five degrees of angle measurement was considered a significant difference. Figure 1 demonstrates measurements of the lateral view angles (Fig. 1).
Scaphoid fracture displacement was defined as 1 mm or more of displacement between the fragments on either MRI or CT scan. Demographic data were limited and only age and gender were collected.
Statistical analysis
Patient demographics and radiographic measurements were summarized under normal vs fracture patients or nondisplaced fracture vs. displaced fracture and were compared by two-sample t-test for continuous variables and chi-square test for categorical variables. Univariate logistic regression was used to assess the association between the measurements and the fracture type. Intraclass correlation coefficient (ICC) was obtained to assess the agreement between observers. All statistical tests were two-tailed and significant level was set at P < 0.05. All analysis was conducted in the R statistical software environment.
Results
One hundred radiographs were available for analysis. We included 50 that had been read as normal on three-dimensional imaging and 50 that had been read as a scaphoid fracture. Twenty-three fractures were displaced (46%). Thirty-eight were fractures of the scaphoid waist (76%), 8 were proximal pole fractures (16%), and 4 were distal pole or tuberosity fractures (8%). Of the fracture group 80% were male and the average age was 39.1(18.0) as opposed to 51.5 (19.2) in the non-fracture group (Table 1).
The comparison of the fracture and non-fracture groups is summarized in Table 1. (Table 1) Of the radiographic measurements, a widened posteroanterior SL interval was associated with the presence of a scaphoid fracture [odds ration (OR) 3.0, CI 1.53–5.87, p = < 0.01] (Fig. 2).
On the right: Posteroanterior view of a right wrist without a scaphoid fracture on 3-dimensional imaging and a normal (1.1 mm) scapholunate gap. On the left: Posteroanterior view of a left wrist that was read as no fracture and a wide (3.1 mm) scapholunate gap on the original radiograph and demonstrated a scaphoid fracture on 3-dimensional imaging
Table 2 describes the comparison between the displaced and nondisplaced fractures. An enlarged lateral radio-lunate angle (LA RL) was significantly associated with fracture displacement. With an Odds Ratio (OR) of 1.13, 95% confidence interval (CI) 1.02–1.25, p = 0.02, with a one-unit increase in LA RL angle, we expect to see about 13% increase in the odds of having a displaced scaphoid fracture (Fig. 3).
On the right: Lateral radiograph of a right wrist with minimally displaced scaphoid fracture on 3-dimensional imaging and a lateral radiolunate angle of 16.5 degrees. On the left: Lateral radiograph of a right wrist with a displaced scaphoid fracture on 3-dimensional imaging and a lateral radiolunate angle of 28.4 degrees
The intraclass correlation coefficient for each measurement showed an overall variability among observers. The LA RL angle was the most consistent at 0.74 and the LA RS angle having the most variability at 0.23 (Table 3).
Discussion
Our cohort was consistent with the literature in that the fracture population consisted of younger males [7]. Our fracture group was younger than the non-fracture group.
Scaphoid nonunion is a commonly encountered sequela that necessitates surgical treatment to obtain healing and prevent arthritic degeneration. The mode of displacement of scaphoid fractures has been shown to include extension and supination of the proximal fragment with no significant motion of the distal fragment. Resultant flexion of the scaphoid, and concomitant lunate extension can lead to abnormal forces and instability in the surrounding carpal joints and subsequently a predictable progression of degenerative changes [8]. Stability of the fracture fragments may be critical for healing and this has prompted the use of multiple techniques for management [9]. Late diagnosis and lack of stabilization may predispose a fracture to nonunion even in the presence of an uncompromised blood supply [10, 11]. Therefore, identifying markers of a scaphoid fracture and fracture instability on plain radiographs may allow for expedient diagnosis and treatment thus preventing nonunion and its challenges.
Several radiographic signs of carpal instability have been reported. A large SL gap in static injuries, or a changing gap under dynamic load can be seen on PA radiographs of the wrist [12]. We found an association between presence of scaphoid fracture and SL gapping on the PA view. A recent study suggested that fluoroscopic measurements in the middle of the scapholunate joint in neutral and 30° of ulnar deviation best capture all stages of scapholunate disruption. They found that measurements of less than 2.0 mm at the middle of the scapholunate interval may be considered within normal range [13]. Since scapholunate gapping on plain radiographs seems to be a reliable measurement, it may be a useful and easy to perform measurement on initial evaluation of a clinically suspected scaphoid fracture. A widened gap may prompt earlier 3-dimensional imaging to investigate for a fracture.
While the presence of acute scaphoid fracture and concomitant scapholunate ligament injury is thought to be rare it can be seen more commonly in scaphoid nonunion [14]. Cooney et. al associated scaphoid fracture instability with scapho-lunate angulation greater than 45 degrees or with luno-capitate angulation greater than 15 degrees [15]. Schädel-Höpfner et al. arthroscopically evaluated 34 wrists with acute scaphoid fractures and found 13 traumatic SLIL tears [16]. This could suggest a more common association between these injuries than previously thought and the presence of a scapholunate gap on plain radiographs in the context of a suspected scaphoid fracture should prompt further 3D imaging. In our cohort, we found that only 8% of the suspected scaphoid fractures sent for further evaluation had evidence of a fracture on 3D imaging. It is out of the scope of this study to evaluate the indications for 3D imaging or the cost-effectiveness of further imaging. However, it is possible that utilizing the associations found in this study on plain radiographs, may alter the practice of seeking 3D imaging when a scaphoid fracture is suspected.
When evaluating presence of the cortical ring sign between the fractured and normal cohort no significant difference was seen. As shown in previous studies the presence of cortical ring sign may indicate scaphoid flexion however can be seen in a high percentage of normal wrists [8].
The lateral radio-lunate angle had a significant association with the presence of a displaced scaphoid fracture. With lunate extension being described as a mode of displacement common to scaphoid fractures, the biomechanical shift may explain the increase in radio-lunate angle in the presence of displaced scaphoid fracture [8].
Evaluation of variability among observers through the intraclass correlation coefficient showed the LA RL angle to be most consistent at 0.74. The LA RS angle had the most variability at 0.23. This could be explained by the difficulty of locating the axis of the scaphoid with the overlapping profiles of the other carpal bones on lateral radiographs of varying quality. This difficulty has been previously reported by Garcia-Elias et al. showing overall error of goniometrically derived intracarpal angles to be a standard deviation of 5.2 degrees [17]. The components of the radio-lunate angle can more reliably be recreated possibly leading to the superior consistency of this measurement in our study.
A limitation of the study is that the radio-lunate angle is not an intercarpal angle. The difficulty of performing this measurement on each lateral wrist radiograph with identical wrist position likely portends high variability among this measurement and could affect its reliability.
We used three-dimensional imaging to define presence or absence of a fracture and displacement. There is some degree of inherent error in these exams [18]. Additionally, while we standardized the method of obtaining each wrist angle and measurement, the difficulty in accurately and reliably obtaining these measurements can affect the overall significance of our evaluations of these measurements. This was a radiographic study, and we did not evaluate any clinical associations such as physical exam. We did have significant differences between the patients that were found to have a fracture and those that were not however on analysis this discrepancy did not affect the results.
In summary, scapholunate gapping in the context of a suspected scaphoid fracture should increase the evaluator’s suspicion for a fracture and may prompt earlier 3D imaging. The presence of an abnormal radiolunate angle should increase suspicion of instability and can be used in preoperative planning. Further study can aid in a better understanding of the significance of these measurements and their clinical application.
References
Garala K, Taub NA, Dias JJ (2016) The epidemiology of fractures of the scaphoid: impact of age, gender, deprivation and seasonality. Bone Joint J 98-B(5):654–659. https://doi.org/10.1302/0301-620X.98B5.36938
Bain GI, Bennett JD, MacDermid JC, Slethaug GP, Richards RS, Roth JH (1998) Measurement of the scaphoid humpback deformity using longitudinal computed tomography: intra- and interobserver variability using various measurement techniques. J Hand Surg Am 23(1):76–81. https://doi.org/10.1016/S0363-5023(98)80093-2
Toms AP, Chojnowski A, Cahir JG (2011) Midcarpal instability: a radiological perspective. Skeletal Radiol 40(5):533–541. https://doi.org/10.1007/s00256-010-0941-1
Kani KK, Mulcahy H, Chew FS (2016) Understanding carpal instability: a radiographic perspective. Skeletal Radiol 45(8):1031–1043. https://doi.org/10.1007/s00256-016-2390-y
Pirela-Cruz MA, Hilton ME, Faillace J (2003) Frequency and characteristics of the scaphoid cortical ring sign. Surg Radiol Anat 25(5–6):451–454. https://doi.org/10.1007/s00276-003-0165-3
Abe Y, Doi K, Hattori Y (2008) The clinical significance of the scaphoid cortical ring sign: a study of normal wrist X-rays. J Hand Surg Eur 33(2):126–129. https://doi.org/10.1177/1753193407087572
MacDermid JC, McClure JA, Richard L, Faber KJ, Jaglal S (2021) Fracture profiles of a 4-year cohort of 266,324 first incident upper extremity fractures from population health data in Ontario. BMC Musculoskelet Disord 22(1):996. https://doi.org/10.1186/s12891-021-04849-7
Shah CM, Stern PJ (2013) Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. Curr Rev Musculoskelet Med 6(1):9–17. https://doi.org/10.1007/s12178-012-9149-4
Schormans PMJ, Brink PRG, Poeze M, Hannemann PFW (2018) Angular stable miniplate fixation of chronic unstable scaphoid nonunion. J Wrist Surg 7(1):24–30. https://doi.org/10.1055/s-0037-1603202
Sander AL, Sommer K, Schaf D, Braun C, Marzi I, Pohlemann T, Frank J (2018) Clinical outcome after alternative treatment of scaphoid fractures and nonunions. Eur J Trauma Emerg Surg 44(1):113–118. https://doi.org/10.1007/s00068-017-0773-y
Mandaleson A, Tham SK, Lewis C, Ackland DC, Ek ET (2018) Scaphoid fracture fixation in a nonunion model: a biomechanical study comparing 3 types of fixation. J Hand Surg Am 43(3):221–228. https://doi.org/10.1016/j.jhsa.2017.10.005
Megerle K, Pohlmann S, Kloeters O, Germann G, Sauerbier M (2011) The significance of conventional radiographic parameters in the diagnosis of scapholunate ligament lesions. Eur Radiol 21(1):176–181. https://doi.org/10.1007/s00330-010-1910-8
Said J, Baker K, Fernandez L, Komatsu DE, Gould E, Hurst LC (2018) The optimal location to measure scapholunate diastasis on screening radiographs. Hand (N Y) 13(6):671–677. https://doi.org/10.1177/1558944717729219
Black DM, Watson HK, Vender MI (1987) Scapholunate gap with scaphoid nonunion. Clin Orthop Relat Res 224:205–209
Cooney WP, Linscheid RL, Dobyns JH, Wood MB (1988) Scaphoid nonunion: role of anterior interpositional bone grafts. J Hand Surg Am 13(5):635–650. https://doi.org/10.1016/s0363-5023(88)80116-3
Schadel-Hopfner M, Junge A, Bohringer G (2005) Scapholunate ligament injury occurring with scaphoid fracture–A rare coincidence? J Hand Surg Br 30(2):137–142. https://doi.org/10.1016/j.jhsb.2004.09.017
Garcia-Elias M, An KN, Amadio PC, Cooney WP, Linscheid RL (1989) Reliability of carpal angle determinations. J Hand Surg Am 14(6):1017–1021. https://doi.org/10.1016/s0363-5023(89)80053-x
Sahu A, Kuek DK, MacCormick A, Gozzard C, Ninan T, Fullilove S, Suresh P (2021) Prospective comparison of magnetic resonance imaging and computed tomography in diagnosing occult scaphoid fractures. Acta Radiol. https://doi.org/10.1177/02841851211064595
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Human and animal rights
All human and animal studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Becker, J., Luria, S., Huang, S. et al. Wrist angle measurements in predicting the presence of a displaced scaphoid fracture. Eur J Orthop Surg Traumatol 33, 2271–2276 (2023). https://doi.org/10.1007/s00590-022-03418-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-022-03418-5