Abstract
Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) are the two most common patterns of posttraumatic wrist arthritis. This review discusses the etiology and clinical evaluation, as well as up-to-date treatment options, for both of these conditions. Classic as well as newer innovative techniques are discussed with clinical outcomes in order to provide an evidence-based review of the world’s literature on SLAC/SNAC wrist.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) patterns of wrist arthritis are two of the most common patterns of wrist arthritis seen by hand surgeons [1, 2]. Reports of 7,000-year-old prehistoric humans with SLAC wrists show that this pathological process has been ever-prevalent in our species [3]. Given the prevalence and disability associated with these conditions, it is imperative that practitioners can critically evaluate these patients both clinically and radiographically to provide treatment with reproducible results.
Etiology and natural history
SLAC wrist develops after attenuation, either traumatically or atraumatically, of the scapholunate ligament. Atraumatic causes of SLAC wrist include calcium pyrophosphate dehydrate deposition disease (CPPD), rheumatoid arthritis, neuropathic diseases, and β2-microglobulin associated amyloid deposition diseases [4, 5]. On the other hand, SNAC wrist develops following a scaphoid fracture that has progressed to a nonunion. Both of these processes lead to abnormal joint kinematics, since the lunate is unrestrained by the distal scaphoid and, therefore, assumes an extended posture. Over time, this may result in a dorsal intercalated segment instability (DISI) deformity, which invariably progresses to degenerative arthritis at the radioscaphoid articulation, followed by carpal collapse and midcarpal arthritis [6].
Whether secondary to long-standing scaphoid nonunion or scapholunate dissociation, a four-stage progressive pattern of arthrosis has been described by Watson and colleagues [1, 2]. Stage I is characterized by arthrosis at the radial styloid–distal scaphoid articulation, which progresses to stage II involvement of the proximal radioscaphoid joint in SLAC wrists and radiocapitate arthrosis in SNAC wrists. This is followed by stage III degenerative changes involving the midcarpal joint—specifically, the capitolunate joint (and scaphocapitate joint in SLAC wrists). Finally, stage IV wrists have pancarpal arthrosis with preservation of the radiolunate joint. Often, the only difference between SNAC and SLAC wrist arthritis involves the preservation of the articulation between the proximal pole of the scaphoid and the radius in SNAC wrists, since the proximal pole of the scaphoid appears to be unloaded and acts as an extension of the lunate through the intact scapholunate ligament [7].
Symptomatology in SLAC and SNAC wrists varies from that found incidentally in asymptomatic patients to debilitating wrist pain with limited motion and strength. Frequently, in elderly and low-demand patients, radiographic findings of SLAC or SNAC wrist may be found incidentally or with other pathology such as carpal tunnel syndrome, appropriately treated with carpal tunnel release not requiring surgical management of the wrist arthritis [8, 9]. In fact, contralateral wrist radiographs of the asymptomatic wrist often reveal radiographic findings of arthrosis, leading some authors to advise routinely obtaining bilateral radiographs [10]. Therefore, wrist pain is not a ubiquitous finding in SLAC and SNAC wrist arthrosis; however, it is still the predominant finding in a majority of presenting cases.
Clinical evaluation
The diagnosis of SLAC and SNAC wrist can be made on the basis of history, physical exam, and adequate radiographs. Patients will often present with wrist pain, dorsoradial swelling, and limited range of wrist motion. On exam, this pain can be elicited at the radiocarpal joint and midcarpal joint. There may or may not be associated swelling in a similar distribution. Care must be taken to differentiate scaphotrapeziotrapezoidal joint pain and thumb basal joint pain, as well as nonarthritic sources of pain, including carpal tunnel, trigger fingers, and DeQuervain’s or flexor carpi radialis tendonitis, as a radially based source of wrist pain.
Imaging
Bilateral biplanar wrist radiographs should be obtained to corroborate physical exam findings and help with treatment recommendations. Aside from differentiating SNAC and SLAC wrist, critical evaluation of the radiographs can help stage the arthritic process by determining isolated involvement of the radial styloid articulation with the distal pole of the scaphoid in stage I disease to pancarpal arthrosis in stage IV disease [11]. Along with this, other radiographic findings, such as chondrocalcinosis and concomitant basal joint arthritis, can be seen on these radiographs to help with clinical evaluation and treatment. Advance imaging in the form of computed tomography or magnetic resonance imaging is rarely indicated.
Nonoperative treatment options
Initially, nonsurgical treatment of symptomatic SLAC and SNAC wrist should be optimized. This can include wrist immobilization with splints, antiinflammatory medication, and corticosteroid injections. If symptoms worsen with disease progression, various operative treatment recommendations may be needed.
Operative treatment options
When symptoms have been refractory to conservative management, various surgical options exist for the treatment of SLAC and SNAC wrist. These vary from radial styloidectomy to distal pole scaphoid excision (for SNAC wrist), wrist denervation, partial wrist arthrodesis, proximal row carpectomy (PRC), and total wrist arthrodesis. The specific course of treatment will vary on the basis of personal preference as well as the stage of arthrosis. Often, intraoperative decisions must be made after determining the status of the capitate articular surface. In addition, multiple procedures are often combined—specifically, the addition of radial styloidectomy and wrist denervation to the other listed procedures.
Wrist denervation
Whether combined with other surgical procedures or done by itself, wrist denervation is an option in the operative treatment of chronic wrist pain. This is applicable in the setting of chronic wrist pain secondary to SLAC and SNAC wrists. The terminal branches of the anterior interosseous nerve (AIN) and the posterior interosseous nerve (PIN) have been shown to be responsible for painful stimuli at the wrist [12, 13]. Denervation can be either complete or incomplete, with the most common form of incomplete denervation involving a PIN neurectomy.
Multiple techniques have evolved for wrist denervation, and recent literature has looked at the anatomical considerations involved with AIN neurectomy. Lin et al. showed in a cadaveric study that denervation of the AIN via a 2-cm neurectomy as described by Berger, through a dorsal incision, poses risk to the motor branches to the pronator quadratus, and therefore, they recommended careful neurectomy at the distal border of the pronator quadratus [14, 15].
Schweizer et al. studied the long-term follow-up after complete wrist denervation at an average of 9.6 years for 70 patients. Two thirds of the patients had subjective long-term improvement in pain, and half had complete or marked pain relief. The best results were seen in patients with SLAC wrists. The authors concluded that this simple fast procedure does not decrease range of motion (ROM) and leaves all other surgical options open [16].
In a study looking specifically at long-term results of wrist denervation for stage II and stage III SLAC/SNAC wrist, 32 patients were evaluated at an average of 6.3 years after complete wrist denervation. Fifty-nine percent of patients reported subjective improvement after denervation, with average grip strength improvement of 51 % with minimal impact on wrist ROM [17].
Most recently, Radu et al. evaluated total and partial wrist denervation in 43 patients at an average follow-up of 4.3 years. They showed that a positive test denervation via local anesthetic did not guarantee postoperative pain reduction after surgical denervation. Thirty patients (70 %) had pain reduction after denervation, and 20 of those (66 %) were pain free at final follow-up. Pain was statistically significantly reduced at final follow-up only for the subgroup of patients without wrist arthrosis. Of those with complete denervation, 76 % reported pain reduction, with 57 % of those with partial denervation reporting pain reduction [18•].
Radial styloidectomy
Early symptomatic arthrosis in the SLAC and SNAC wrist presents between the radial styloid and the scaphoid. Although many patients are often beyond stage I disease when they require operative intervention, surgical options such as radial styloidectomy do exist for these early symptomatic patients. In addition, radial styloidectomy can be combined with other surgical treatments for more advanced disease if radiocarpal abutment continues to be a problem.
Previous research in the area of radial styloidectomy has shown the anatomic relationships of the radial styloid to the dorsal and palmer radiocarpal ligaments of the wrist. The most clinically significant radially based ligaments are the dorsal radiocarpal, radial collateral, palmar radioscaphocapitate (RSC), and palmar long and short radiolunate ligaments. Siegel and Gelberman showed the relationship of these ligaments to three specific types of radial styloidectomy: short oblique, vertical, and horizontal. Although all types of styloidectomy removed a certain degree of radiocarpal ligaments, the short oblique osteotomy preserved the most extrinsic ligamentous support to the wrist [19]. More recently, Nakamura et al. recommended against removing more than 3–4 mm with the oblique osteotomy to avoid increased carpal instability [20]. There have been reports of arthroscopic radial styloidectomy; however, true comparison of outcomes between this technique and open technique are not available [21].
Distal pole scaphoid excision
Radioscaphoid pain in the setting of early SNAC wrist can be managed differently than with SLAC wrist. If the capitolunate joint is well preserved, one can consider excision of the distal scaphoid fragment with or without radial styloidectomy. As has been reported by Downing [22] and, more recently, by Malerich [23], the distal pole of the scaphoid could be excised as long as more than half of the proximal fragment remained and there was no capitolunate arthrosis. This led to pain relief, with improved ROM and grip strength in 13 of 19 patients studied. However, of 4 patients with capitolunate arthrosis, 2 had persistent symptoms, and 3 had progressive degenerative changes. The authors concluded that distal pole excision is an alternative to partial wrist arthrodesis [23]. Soejima et al. reported that distal pole excision improved pain, strength, and ROM in patients with scaphoid nonunions. The authors stated that care must be taken with patients who have a type II lunate, since they have increased radioulnar translation of the lunate and, therefore, theoretically have increased cumulative traumatic wear at the scapholunate–capitate articulation [24]. Most recently, Ruch et al. reported on the benefits of distal pole scaphoid excision in patients who had failed previous surgical treatment for scaphoid nonunion without attenuation of the SL ligament [25].
Partial wrist arthrodesis
Partial wrist arthrodesis remains one of the most common procedures performed in the setting of SNAC/SLAC wrist arthrosis. There has been much debate as to the type of arthrodesis, as well as the comparison of partial arthrodesis with motion-preserving procedures such as PRC. In fact, the majority of recent literature in the surgical treatment of SLAC/SNAC wrist has compared the results of scaphoid excision and four-corner arthrodesis with PRC. Even with the vast amount of literature on the topic, there still appears to be no majority consensus on the matter.
Four-corner arthrodesis—K-wires and screws
Originally described by Watson and Ballet, this procedure involved excision of the scaphoid with K-wire fixation of the arthrodesis between the capitate and lunate. The authors used distal radius bone graft and replaced the scaphoid with a silicone implant, which later was no longer recommended because of implant dislocation [1]. Of note, the authors performed the surgery through two separate transverse incisions, one for the arthrodesis and a second to harvest distal radius bone graft. The wrist was immobilized, and the buried K-wires were removed after 6 weeks.
Using a similar technique, Dacho et al. reviewed 49 patients with average follow-up of 47 months. Postoperative AROM was 56 %, and grip strength was 76 % of the contralateral side. Forty-five patients (92 %) had bony fusion verified by x-ray, and 6 patients (12 %) required conversion to total arthrodesis because of pain or absence of bony fusion [26]. Since this description, there have been many modifications to the technique; however, the overall premise of the surgery remains unchanged.
Gracia-López et at. reported on 16 patients who underwent a modified four-corner arthrodesis using an autologous corticocancellous iliac crest “bone plate” and screw fixation. Wrists were immobilized for 3 weeks, and then progressive ROM was begun. At an average follow-up of 3 years, there were 13 excellent results and 3 good results. All 16 went on to have bony fusion and pain relief, with the ability to return to their previous occupation [27].
In a recent long-term follow-up study using staples for fixation, Bain and Watts followed 31 patients at a mean follow-up of 10 years. They noted that grip strength remained unchanged and wrist flexion decreased by 22 %. There was no significant change in pain, wrist function, satisfaction, or arc of motion between 1 and 10 years postoperatively. Two of the patients had gone on to total wrist arthrodesis for ongoing pain [28•].
Richards et al. reported their outcomes of four-corner arthrodesis using headless compression screws through an open technique for SLAC/SNAC wrist. They argued that the benefit of this fixation is the ability to allow early active ROM, which they allowed at 10–14 days postoperatively. A 95 % fusion rate was observed, and most fusions were seen within 6–8 weeks. Three patients developed screw loosening; however, only 1 of these went on to nonunion [29•].
Finally, in a recent study by Ozyurekoglu and Turker, 33 patients were followed for an average of 8 months after a modified scaphoid excision and four-corner arthrodesis using a percutaneous headless compression screw technique. After performing a limited arthrotomy for removal of cartilage and subchondral bone, capitolunate fixation was achieved with a percutaneous retrograde transmetacarpal headless compression screw, and a percutaneous antegrade screw was used for triquetrohamate fixation. Scaphoid bone graft was used in the procedure. The authors reported union in 31 of 33 (94 %) wrists, with only 1 patient going onto total arthrodesis. AROM was 71° versus 83° preoperatively, and grip strength improved from 41 % to 80 % of the contralateral side after surgery [30•].
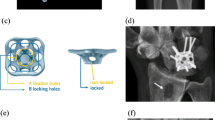
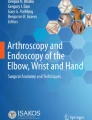
Four-corner arthrodesis—circular plates
After the original description of four-corner arthrodesis using K-wire fixation, circular plate constructs were developed as an alternative, with alleged more stable fixation leading to lower nonunion rates. Although a few studies have shown positive results with this construct, a majority have shown that the construct is fraught with complications and less successful outcomes.
Kendall et al. reported on 8 patients, with an average follow-up of 20 months. Radiographic union was achieved in only 3 of these patients (63 % nonunion rate), and ROM, 46 % of contralateral, as well as grip strength, 56 % of contralateral, were inferior to the results previously reported for K-wire fixation [31]. As reported by Vance et al., 58 patients undergoing four-corner arthrodesis either by plate fixation (n = 27) or by traditional fixation (n = 31) were compared. A 26 % nonunion rate was seen in the plate fixation group versus 3 % in the traditional group. Along with this, hardware impingement was seen in 22 % of the plate group versus 3 % of the traditional group [32]. Similarly, Chung et al. reported prospectively on 10 patients using the first-generation Spider Limited Wrist Fusion Plate (KMI, San Diego, CA) at mean follow-up of 1 year. They reported no noteworthy improvement in function, ADLs, work, pain, or patient satisfaction, with 3 patients having broken hardware [33]. Using the same plate, Shindle et al. retrospectively analyzed 16 patients, with average follow-up of 16 months. They reported a 56 % complication rate and a 25 % nonunion rate, both considerably higher than that obtained with previously published techniques for four-corner arthrodesis [34]. In more recent studies, Collins and Nolla, as well as De Smet et al., showed that comparing circular plates with traditional implants showed decreased wrist motion in the plate group, along with the previously noted higher nonunion rate [35, 36•].
Using second-generation implants, Merrell et al. showed improved results with circular plate constructs. At an average follow-up time of 46 months, 28 patients were analyzed. Grip strength averaged 82 % of the contralateral side, and ROM averaged 45 % of the contralateral side. Primary fusion was noted in all cases, with hardware complications in two cases. The author emphasized that an exacting technique with distal radius bone graft, adequate joint preparation, and two-screw fixation in each bone is needed for these results [37]. Similarly, Bedford and Yang reported positive results with this plate at a mean of 11 months follow-up. They had a 100 % union rate in 15 patients, with only one postoperative complication [38•].
Capitolunate arthrodesis
Central to the technique of four-corner arthrodesis is the need for a stable capitolunate fusion. As originally described, the hamate and triquetrum were part of the arthrodesis in order to decrease the likelihood of nonunion. Over the years, many authors have evaluated the role of an isolated capitolunate arthrodesis with or without scaphoid and/or triquetral excision to theoretically improve postoperative ROM. As was shown in biomechanical studies by Scobercea et al., scaphoid and triquetrum excision increased radial deviation at the cost of an increased radiolunate contact pressure of 44 % [39•].
Early reports by Kirschenbaum et al. showed increased nonunion rates with scaphoid excision and capitolunate arthrodesis using K-wire fixation. In their series, 6 of 18 patients (33 %) went onto pseudoarthrosis, which was considerably higher than conventional four-corner arthrodesis [40]. Kadji et al. also reported on isolated capitolunate fusion versus standard four-corner arthrodesis. They reported increased ROM of 10° volar flexion and 12° radial deviation; however, they continued to have a high nonunion rate of 18 % versus 0 % for standard four-corner arthrodesis in their cohort [41]. Calandruccio et al. reported on 14 patients undergoing capitolunate arthrodesis with scaphoid and triquetrum excision. They used compression screw fixation of the arthrodesis site and had improved results, with only 14 % nonunion rate. Grip strength and ROM were comparable to those for standard four-corner arthrodesis [42].
More recent studies have corroborated the benefits of capitolunate arthrodesis with modern techniques having outcomes similar to standard four-corner arthrodesis. Using the same technique as Calandruccio, Gaston et al. retrospectively compared 16 patients with capitolunate arthrodesis with 18 patients with four-corner arthrodesis. There was no statistically significant difference in ROM, strength, VAS, or DASH between the two groups. There were two nonunions in the four-corner group, as compared with none in the capitolunate group; however, 5 patients in the capitolunate group required screw removal secondary to migration. They stated that the benefits of capitolunate arthrodesis include easier reduction of the lunate after triquetrum excision, as well as avoiding symptomatic pisotriquetral arthritis at the expense of possible screw migration [43•].
Proximal row carpectomy
First described by T. T. Stamm, proximal row carpectomy (PRC) is an established surgical treatment for radiocarpal arthrosis [44]. The merits of PRC include the relative simplicity of the procedure and the lack of implanted fixation, since no bony healing is required. Given the inherent postoperative stability, Jacobs et al. have recently advocated for immediate postoperative mobilization, stating results similar to those for immobilized wrists [45]. As classically described, PRC can be considered in cases of stage I and II SLAC/SNAC wrist when the articular surfaces of the head of the capitate, as well as the lunate facet of the distal radius, are well preserved. In addition to this, preservation of the RSC ligament is needed to prevent postoperative ulnar translocation of the carpus. Outcomes of PRC in the treatment of SLAC/SNAC have shown favorable results.
Jebson et al. reported their long-term outcomes of PRC for wrist arthrosis. At an average follow-up of 13.1 years, wrist ROM was 63 % and grip strength was 83 % of the contralateral wrist. Radiocapitate arthrosis was absent/minimal in 76 % and moderate/severe in 24 %; however, this did not correlate with patient satisfaction or wrist pain. Two patients (10 %) had persistent pain and went on to have radiocapitate arthrodesis [46]. Similarly, DiDonna et al. reported on 21 patients, with an average follow-up of 14 years. Four failures (18 %) were noted, requiring fusion at an average of 7 years postoperatively, in patients younger than 35 years of age who underwent PRC. The remaining patients had an average flexion/extension arc of 72°, with an average grip strength of 91 %, as compared with the contralateral side. Although degeneration of the radiocapitate joint was seen radiographically in 14 cases, it had no association with subjective or objective function and did not preclude a successful clinical result. The authors cautioned against performing PRC in patients younger than 35 years [47].
The most recent long-term outcome of PRC was by Ali et al. In their group, 81 patients, with an average follow-up of 19.8 years, showed wrist motion and grip strength that were not significantly different from preoperative values. Seventy-four percent were dissatisfied with their results due to persistent pain or inability to return to their previous occupation. Sixty-four percent required daily pain medication for their wrist, and 15 % had gone onto total wrist arthrodesis. The authors concluded that long-term results of PRC can be poor and alternatives should be sought in younger patients and those with high-demand occupations. These results must be taken with caution, since much of the data were from survey follow-up and the patient population was heterogeneous, including neuromuscular patients undergoing PRC for improved wrist extension (15 %), a high proportion of active manual laborers (52 %), and only 46 % with a diagnosis of SLAC/SNAC wrist [48•].
PRC in stage III SLAC/SNAC wrist
As was stated previously, traditional teaching holds that capitate degeneration is a contraindication to PRC. However, as can be seen in the long-term reviews above, radiocapitate radiographic changes do not necessarily correlate with worse outcomes. That being said, much research has gone into treatment options for capitate arthrosis in the setting of PRC.
Kwon et al. retrospectively reviewed 8 patients with advanced capitolunate arthrosis treated with PRC and dorsal capsular interposition arthroplasty. After a mean follow-up of 41 months, ROM and grip strength were maintained at preoperative levels, and pain was significantly improved. Progression of arthritis was seen in 3 patients; however, this did not correlate with negative outcomes [49•].
Taking this one step further, Salomon and Eaton advocated for partial capitate recession in line with the hamate along with the capsular interposition. The belief was that this technique dispersed contact stresses over a wider area, since the resected proximal capitate and hamate created a more uniform presenting surface to the distal radius for the pseudarthrosis [50]. In a similar technique, Placzek et al. reviewed the results of 8 patients with stage II and III SLAC wrist treated with a capitate head resection and dorsal capsular interposition. ROM and grip strength were similar to preoperative values; however, pain was improved in 75 % of patients at 1-year follow-up [51].
Finally, in a recent study by Tang and Imbriglia, a surgical technique involving osteochondral resurfacing using grafts harvested from the resected carpal bones was combined with PRC in patients with substantial focal arthritis of the capitate measuring less than 10 mm in diameter. Eight patients were followed for an average of 18 months. Postoperative arc of motion was 75°, and grip strength was 71 % of the contralateral side. Pain improvement was seen in 88 % of patients, and follow-up radiographs showed that 75 % of patients had mild to no degeneration. Along with this, MR imaging at 21 months postoperatively showed graft incorporation [52].
PRC versus four-corner arthrodesis
The majority of recent literature concerning the treatment of SLAC/SNAC wrist has focused on four-corner arthrodesis versus PRC. Many studies have directly compared these two procedures, showing fairly comparable results. Those who criticize four-corner arthrodesis point to complications that are not seen with PRC, such as nonunion, hardware impingement, and decreased motion secondary to malposition of the lunate in the fusion mass. Those who criticize PRC state the decreased longevity in younger patients, as well as the nonanatomic articulation of the capitate with the lunate facet of the distal radius, leading to progressive arthrosis.
Wyrick et al. compared 17 patients treated with four-corner arthrodesis and 10 patients treated with PRC for SLAC wrist at mean follow-up of 31 months. The PRC group had increased postoperative ROM (115° vs. 95°) and grip strength (94 % vs. 74 % of the contralateral wrist), as compared with four-corner arthrodesis. Five patients (29 %) in the four-corner arthrodesis group failed treatment, and 3 of those went on to total wrist fusion. There were no failures in the PRC group [53]. Cohen and Kozin reported on a combined group of 38 patients from two cohorts at separate institutions. They noted no significant differences in ROM, grip strength, or physical health outcome scale scores [54]. Vanhove et al. looked at 30 patients with a mean follow-up of 3.5 years. They noted no significant difference in pain or functional outcome; however, there was a higher complication rate with four-corner arthrodesis, due to the need for internal fixation [55]. Dacho et al. looked at a group of 47 patients who showed increased arc of motion of 14° with PRC; however, there was increased grip strength with four-corner arthrodesis (72 % vs. 50 % of the contralateral side). They concluded that PRC was more favorable for those patients who required less grip strength for work [56].
In a systematic review of the previous literature, Mulford et al. reviewed 52 studies in order to compare the results of PRC with those of four-corner arthrodesis. They noted that grip strength, pain relief, and subjective outcome scores were similar between the two groups. PRC allowed increased postoperative ROM; however, they also had increased rates of progressive arthrosis, albeit asymptomatic. Complications were higher in the four-corner arthrodesis group, which were attributed to nonunion, hardware issues, and impingement.
Kiefhaber summarized these results and drew conclusions on the basis of these substantial data. Pain relief was similar with both procedures, with 85 % substantial pain relief. Arc of motion was comparable; however, four-corner arthrodesis usually had 10° less postoperative arc than PRC. Both procedures improved strength to 80 % of the contralateral side. The risk of conversion to total wrist arthrodesis was equal for both procedures at 5 %. PRC was shown to have increased rates of progressive arthrosis of the lunate fossa; however, this was not clinically correlated with pain or subsequent surgery. General complications were similar between the two procedures; however, those complications specific to four-corner arthrodesis included nonunion (5.5 %), dorsal impingement (2.6 %), and hardware issues (3.3 %). Kiefhaber’s preference was to favor four -corner arthrodesis for patients younger than 35 years and high-demand patients in their forties and early fifties, with PRC used for the less active patients in this same age group [57••].
Conversion to total wrist arthrodesis
The ultimate salvage for any motion-preserving procedure is total arthrodesis. As was noted previously, conversion rates of four-corner arthrodesis and PRC to total wrist arthrodesis are comparable at 5 %. Gohritz et al. reported on 20 patients who underwent conversion of four-corner arthrodesis to total wrist arthrodesis and noted that all but 2 of these patients (90 %) were satisfied with the secondary procedure and had considerable reduction in their pain level, albeit with some residual pain [58]. We are unaware of any literature looking specifically at outcomes after PRC conversion to total wrist arthrodesis.
Authors’ preferred treatment
In our practice, treatment of SLAC and SNAC wrist arthritis depends on several factors, including the magnitude of complaints, age of patient, level of physical activity, and radiographic stage.
Denervation is rarely done as an isolated procedure and is done in combination with traditional salvage procedures (PRC and four-corner arthrodesis). It is simple to perform and seemingly has no downside.
We rarely perform styloidectomy, since it has been found to be unnecessary in both PRC and four-corner arthrodesis. We reserve distal pole scaphoid excision for stage I SNAC wrist, and we prefer a palmar approach. It is simple to perform and burns no bridges should it fail to alleviate pain or if the degenerative process progresses.
PRC in general has stood the test of time, is simple to perform, and involves little rehabilitation. We will not normally perform a PRC in a wrist with capitolunate arthritis or advanced carpal collapse. In addition, we reserve PRC for patients who are at least 40 years of age who enjoy sedentary physical activities.
Four-corner arthrodesis is our preferred procedure for younger, active patients, especially if capitolunate arthritis is present. For fixation, we no longer use circular plates and prefer two cannulated, headless screws, one from the lunate into the capitate and one from the triquetrum, through the proximal hamate, and into the capitate (inserted through a separate ulnar incision). It is imperative that the lunate extension (DISI) be corrected, that bony preparation be meticulous, and that ample bone graft from the distal radius and or Gerty’s tubercle of the knee be harvested to supplement the arthrodesis.
Conclusion
SLAC/SNAC wrist arthritis are common diagnoses encountered by the practicing hand surgeon. A systematic evaluation and evidenced-based approach to treatment options, as described, provides the best potential for a successful outcome that is tailored to the patient’s physical requirements and lifespan. Careful determination of age, underlying etiology, presenting complaint, and stage of arthrosis, as well as postoperative activity expectations, can help the practitioner choose a treatment plan that will optimize not only outcomes, but also patient satisfaction.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg [Am]. 1984;9A:358–65.
Watson H, Ryu J. Evolution of arthritis of the wrist. Clin Orthop Relat Res. 1986;202:57–67.
Masmejean E, Dutour O, Touam C, et al. Bilateral SLAC (scapholunate advanced collapse) wrist: an unusual entity. Apropos of a 7000-year-old prehistoric case. Ann Chir Main Memb Super. 1997;16(3):207–14.
Stäbler A, Baumeister RG, Berger H. Carpal instability and secondary degenerative changes in lesions of the radio-carpal ligaments with various etiology. Handchir Mikrochir Plast Chir. 1990;22(6):289–95.
Saffar P. Chondrocalcinosis of the wrist. J Hand Surg (Br). 2004;29B:486–93.
Harrington RH, Lichtman DM, Brockmole DM. Common pathways of degenerative arthritis of the wrist. Hand Clin. 1987;3(4):507–27.
Weiss KE, Rodner CM. Osteoarthritis of the wrist. J Hand Surg. 2007;32A:725–46.
Fassler PR, Stern PJ, Kiefhaber TR. Asymptomatic SLAC wrist: does it exist? J Hand Surg. 1993;18A:682–6.
Vance RM, Gelberman R, Braun RM. Chronic bilateral scapholunate dissociation without symptoms. J Hand Surg. 1979;4A:178–80.
Vitello W, Gordon DA. Obvious radiographic scapholunate dissociation: x-ray the other wrist. Am J Orthop (Belle Mean NJ). 2005;34:347–51.
Stäbler A, Heuck A, Reiser M. Imaging of the hand: degeneration, impingement and overuse. Eur J Radiol. 1997;25(2):118–28.
Dellon AL, Mackinnon SE, Daneshvar A. Terminal branch of anterior interosseous nerve as source of wrist pain. J Hand Surg Br. 1984;9(3):316–22.
Dellon AL, Seif SS. Anatomic dissections relating the posterior interosseous nerve to the carpus, and the etiology of dorsal wrist ganglion pain. J Hand Surg. 1978;3(4):326–32.
Lin DL, Lenhart MK, Farber GL. Anatomy of the anterior interosseous innervation of the pronator quadratus: evaluation of structures at risk in the single dorsal incision wrist denervation technique. J Hand Surg. 2006;31(6):904–7.
Berger RA. Partial denervation of the wrist: a new approach. Tech Hand Up Extrem Surg. 1998;2(1):25–35.
Schweizer A, von Känel O, Kammer E, Meuli-Simmen C. Long-term follow-up evaluation of denervation of the wrist. J Hand Surg. 2006;31(4):559–64.
Rothe M, Rudolf KD, Partecke BD. Langzeitergebnisse nach Handgelenkdenervation bei fortgeschrittenem karpalem Kollaps (SLAC-/SNAC-Wrist Stadium II und III). Handchir Mikrochir Plast Chir. 2006;38(4):261–6.
• Radu CA, Schachner M, Tränkle M, et al. Functional results after wrist denervation. Handchir Mikrochi Plast Chir. 2010;42:279–86. Total and partial wrist denervation in 43 patients followed for 4.3 years. Test denervation did not guarantee postoperative pain reduction after surgical denervation. Thirty patients (70 %) had pain reduction after denervation and 20 of those (66 %) were pain free at final follow-up.
Siegel DB, Gelberman RH. Radial styloidectomy: an anatomical study with special reference to radiocarpal intracapsular ligamentous morphology. J Hand Surg. 1991;16(1):40–4.
Nakamura T, Cooney WP, Lui WH, Haugstvedt JR, Zhao KD, Berglund L, et al. Radial styloidectomy: a biomechanical study on stability of the wrist joint. J Hand Surg. 2001;26(1):85–93.
Yao J, Osterman AL. Arthroscopic techniques for wrist arthritis (radial styloidectomy and proximal pole hamate excisions). Hand Clin. 2005;21(4):519–26.
Downing FH. Excision of the distal fragment of the scaphoid and styloid process of the radius for nonunion of the carpal scaphoid. West J Surg Obstet Gynecol. 1951;59(3):217–8.
Malerich MM, Clifford J, Eaton B, Eaton R, Littler JW. istal scaphoid resection arthroplasty for the treatment of degenerative arthritis secondary to scaphoid nonunion. J Hand Surg. 1999;24(6):1196–205.
Soejima O, Iida H, Hanamura T, Naito M. Resection of the distal pole of the scaphoid for scaphoid nonunion with radioscaphoid and intercarpal arthritis. J Hand Surg. 2003;28(4):591–6.
Ruch DS, Papadonikolakis A. Resection of the scaphoid distal pole for symptomatic scaphoid nonunion after failed previous surgical treatment. J Hand Surg. 2006;31A(4):588–93.
Dacho A, Grundel J, Holle G, Germann G, et al. Long-term results of midcarpal arthrodesis in the treatment of scaphoid nonunion advanced collapse (SNAC-wrist) and scapholunate advanced collapse (SLAC-wrist). Ann Plast Surg. 2006;56(2):139–44.
Garcia-Löpez A, Perez-Ubeda MJ, et al. A modified technique of four-bone fusion for advanced carpal collapse (SLAC/SNAC wrist). J Hand Surg (Br). 2001;26B(4):352–4.
• Bain GI, Watts AC. The outcome of scaphoid excision and four-corner arthrodesis for advanced carpal collapse at a minimum of ten years. J Hand Surg (Am). 2010;35A:719–25. 31 patients at a mean follow-up of 10 years. They noted that grip strength remained unchanged, and wrist flexion decreased by 22 %. There was no significant change in pain, wrist function, satisfaction, or arc of motion between one and 10 years postoperatively.
• Richards AA, Afifi AM, Moneim MS. Four-corner fusion and scaphoid excision using headless compression screws for SLAC and SNAC wrist deformities. Tech Hand Up Extrem Surg. 2011;15(2):99–103. Outcomes of 4-corner arthrodesis using headless compression screws through an open technique for SLAC/SNAC wrist were evaluated. A 95 % fusion rate was observed and most fusions were seen within 6-8 weeks. 3 patients developed screw loosening however only 1 of these went on to nonunion.
• Ozyurekoglu T, Turker T. Results of a method of 4-corner arthrodesis using headless compression screws. J Hand Surg. 2012;37(3):486–92. 33 patients were followed for an average of 8 months after a modified scaphoid excision and 4-corner arthrodesis using a percutaneous headless compression screw technique. The authors reported union in 31 of 33 (94 %) wrists with only 1 patient going onto total arthrodesis. AROM was 71° vs. 83° preoperatively and grip strength improved from 41 % to 80 % of the contralateral side after surgery.
Kendall CB, Brown TR, Millon SJ, Rudisill LE, et al. Results of four-corner arthrodesis using dorsal circular plate fixation. J Hand Surg (Am). 2005;30A:903–7.
Vance MC, Hernandez JD, DiDonna ML, et al. Complications and outcome of four-corner arthrodesis: circular plate fixation versus traditional techniques. J Hand Surg (Am). 2005;30A:1122–7.
Chung KC, Watt AJ, Kotsis S. A prospective outcomes study of four-corner wrist arthrodesis using a circular limited wrist fusion plate for stage II scapholunate advanced collapse wrist deformity. Plast Reconstr Surg. 2006;118:433.
Shindle MK, Burton KJ, Weiland AJ, et al. Complications of circular plate fixation for four-corner arthrodesis. J Hand Surg (Br). 2007;32:50–3.
Collins ED, Nolla J. Spider plate fixation: no significant improvement in limited wrist arthrodesis. Tech Hand Upper Extrem. 2008;12(2):94–9.
• De Smet L, Deprez P, et al. Outcome of four-corner arthrodesis for advanced carpal collapse: circular plate versus traditional techniques. Acta Orthop Belg. 2009;75(3):323–7. Authors compared circular plates to traditional implants showing decreased wrist motion in the plate group along with higher nonunion rates.
Merrell GA, McDermott EM, Weiss A. Four-corner arthrodesis using a circular plate and distal radius bone grafting: a consecutive case series. J Hand Surg. 2008;33A:635–42.
• Bedford B, Yang SS. High fusion rates with circular plate fixation for four-corner arthrodesis of the wrist. Clin Orthop Relat Res. 2010;468:163–8. Authors reported positive results with second generation circular plate at a mean of 11 months follow-up. They had 100 % union rate in 15 patients with only one postoperative complication.
• Scobercea RG, Budoff JE, Hipp JA. Biomechanical effect of triquetral and scaphoid excision on simulated midcarpal arthrodesis in cadavers. J Hand Surg (Am). 2009;34A:381–6. Biomechanical study showing scaphoid and triquetrum excision increased radial deviation at the cost of an increased radiolunate contact pressure of 44 %.
Kirschenbaum D, Schneider LH, Kirkpatrick WH, et al. Scaphoid excision and capitolunate arthrodesis for radioscaphoid arthritis. J Hand Surg. 1993;18A:780–5.
Kadji O, Duteille F, Dautel G, Merle M. Arthrodèse carpienne des quatre os versus arthrodèse capitolunaire. À propos de 40 patients. Chir Main. 2002;21(1):5–12.
Calandruccio LH, Gelberman RH, Duncan SFM, Goldfarb CA, Pae R, Gramig W. Original communications: capitolunate arthrodesis with scaphoid and triquetrum excision. J Hand Surg. 2000;25(5):824–32.
• Gaston RG, Greenberg JA, Baltera RM, Mih A, et al. Clinical outcomes of scaphoid and triquetral excision with capitolunate arthrodesis versus scaphoid excision and four-corner arthrodesis. J Hand Surg. 2009;34A:1407–12. Retrospective review comparing 16 patients with capitolunate arthrodesis to 18 patients with 4-corner arthrodesis. There was no statistically significant difference in ROM, strength, VAS, or DASH between the two groups. There were 2 nonunions in the 4-corner group compared to none in the capitolunate group, however 5 patients in the capitolunate group required screw removal secondary to migration.
Stamm TT. Excision of the proximal row of the Carpus. Proc R Soc Med. 1944;38(2):74.
Jacobs R, Degreef I, De Smet L. Proximal row carpectomy with or without postoperative immobilization. J Hand Surg (Br). 2008;33:768.
Jebson PJL, Hayes EP, Engber WD. Proximal row carpectomy: a minimum 10-year follow-up study. J Hand Surg. 2003;28(4):561–9.
DiDonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomystudy with a minimum of ten years of follow-up. J Bone Joint Surg Br. 2004;86-A(11):2359–65.
• Ali MH, Rizzo M, Shin AY, Moran SL. Long-term outcomes of proximal row carpectomy: a minimum of 15-year follow-up. Hand Springer; 2012:1–7. 81 patients with average follow-up of 19.8 years showed that wrist motion and grip strength were not significantly different from preoperative values. Seventy-four percent were dissatisfied with their results due to persistent pain or inability to return to previous occupation. Sixty-four percent required daily pain medication for their wrist and 15% had gone onto total wrist arthrodesis. These results must be taken with caution as much of this data was from survey follow-up and the patient population was heterogeneous including neuromuscular patients undergoing PRC for improved wrist extension (15%), a high proportion of active manual laborers (52%), and only 46% with a diagnosis of SLAC/SNAC wrist.
• Kwon BC, Choi SJ, Shin J, et al. Proximal row carpectomy with capsular interposition arthroplasty for advanced arthritis of the wrist. J Bone Joint Surg Br. 2009;91-B(12):1601–6. Retrospective review of eight patients with advanced capitolunate arthrosis treated with PRC and dorsal capsular interposition arthroplasty with mean follow-up of 41 months. ROM and grip strength were maintained at preoperative levels and pain was improved. Progression of arthritis was seen in 3 patients, however this did not correlate with negative outcomes.
Salomon GD, Eaton RG. Proximal row carpectomy with partial capitate resection. J Hand Surg. 1996;21(1):2–8.
Placzek JD, Boyer M, Raaii F, Freeman DC, et al. Proximal row carpectomy with capitate resection and capsular interposition for treatment of scapholunate advanced collapse. Orthopedics 2008;31(1).
Tang P, Imbriglia JE. Osteochondral resurfacing (OCRPRC) for capitate chondrosis in proximal row carpectomy. J Hand Surg. 2007;32A:1334–42.
Wyrick J. Proximal row carpectomy and intercarpal arthrodesis for the management of wrist arthritis. J Am Acad Orthop Surg. 2003;11(4):277–81.
Cohen MS, Kozin S. Degenerative arthritis of the wrist: proximal row carpectomy versus scaphoid excision and four-corner arthrodesis. J Hand Surg (Am). 2001;26A:94–104.
Vanhove W, Vil JD, Van Seymortier P, et al. Proximal row carpectomy versus four-corner arthrodesis as a treatment for SLAC (scapholunate advanced collapse) wrist. J Hand Surg (Br). 2008;33E(2):118–25.
Dacho AK, Baumeister S, Germann G, et al. Comparison of proximal row carpectomy and midcarpal arthrodesis for the treatment of scaphoid nonunion advanced collapse (SNAC-wrist) and scapholunate advanced collapse (SLAC-wrist) in stage II. J Plast Reconstr Aesthet Surg. 2008;61:1210-12-18.
•• Kiefhaber TR. Management of scapholunate advanced collapse pattern of degenerative arthritis of the wrist. J Hand Surg. 2009;34(8):1527–30. Summary article discussing treatment options for SLAC wrist. Kiefhaber’s preference was to favor 4-corner arthrodesis for patients younger than 35 years and high-demand patients in their forties and early fifties with PRC used for the less active patients in this same age group.
Gohritz A, Gohla T, Stutz N, Moser V, et al. Special aspects of wrist arthritis management for SLAC and SNAC wrists using midcarpal arthrodesis: results of bilateral operations and conversion to total arthrodesis. Bull Hosp Jt Dis. 2005;63(1–2):41–8.
Disclosure
C. M. Shah: none; P.J. Stern: member of the JBJS Board of Trustees.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, C.M., Stern, P.J. Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. Curr Rev Musculoskelet Med 6, 9–17 (2013). https://doi.org/10.1007/s12178-012-9149-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12178-012-9149-4