Abstract
We present a case of a secondary injury to the femoral artery in a geriatric male patient who sustained a pertrochanteric femoral fracture. Six days after closed fracture reduction and intramedullary femoral nailing, the patient presented with persistent hematocrit level drops, femoral swelling and pain. A computed tomography angiography of the femur revealed a perforation of the profunda femoris artery through the dislocated lesser trochanter fragment, and immediate surgical revision was induced. The patient returned to his pre-injury mobilization level without any peripheral vascular or neurological deficiencies. A literature review suggests that the occurrence of vascular damage in proximal femoral fractures is rare but mainly presents in geriatric patients due to atherosclerosis and brittle bone mass.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arterial injury is a rare complication of internal fixation of proximal femoral fractures. Injuries to the profunda femoris artery (PFA) are usually iatrogenic and mainly due to a direct trauma caused by a screw, drill or a retractor. Less commonly is the injury attributed to displaced fracture fragments [1,2,3], which constitutes 0.2% of all PFA injury cases [1].
We present a case in a geriatric male patient in whom an injury to the PFA occurred 6 days after closed reduction and intramedullary femoral nailing. The postoperatively reduced lesser trochanter dislocated ventro-cranially and caused a hemorrhage into the vastus medialis muscle.
In general, complications in pertrochanteric fractures increase in geriatric patients due to the observed demographic changes with an increase in the geriatric population, atherosclerosis [4] and the brittle bone structure accompanying the advanced stages of osteoporosis [5].
Case report
An eighty-five-year-old Caucasian male arrived at the emergency department of a level-I tertiary-care center with the ambulance after a fall from standing height while attempting to go to bed in a home setting. He presented with left hip pain and an inability to walk. The left lower extremity was shorter and externally rotated with normal peripheral pulses, no thigh swelling and a normal capillary refill time. Before the accident, the patient was able to mobilize himself with the aid of a walking stick, lived independently and had the following known medical conditions: arterial hypertension, atrial fibrillation (Marcoumar intake) and prostatahyperplasia with a permanent catheter.
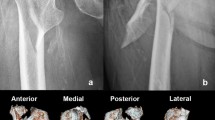
The obtained radiographs (Fig. 1) displayed a comminuted left pertrochanteric femoral fracture with avulsion of the lesser trochanter and part of the greater trochanter (31-A2.1 pertrochanteric femoral instable fracture, AO classification).
The admission blood results showed a hematocrit of 0.40, PZ 22% and an INR of 3.9. Marcoumar was paused, 5000 units of subcutaneous Fragmin were administered for thrombosis prophylaxis, and furthermore the supplementation with Konakion 10 mg was initiated. The patient’s left lower extremity was managed with a foam rail overnight, and he was taken to the operating theater with a PZ of 70%, INR of 1.21 and the same stable hematocrit the following day. Under antibiotic coverage with cefuroxim 1.5 g single shot, a closed reduction and an osteosynthesis with an intramedullary nail (Gamma Nail, Stryker TN, USA) was carried out. There were no complications during the procedure, the patient’s mean arterial blood pressure was stable, and he did not require transfusions (Fig. 2).
The patient recovered well with a hematocrit of 0.28 on the first postoperative day, and full-body weight-bearing mobilization with a wheeled walker was initiated on the second postoperative day.
On the fourth postsurgical day, the blood count showed a hematocrit of 0.26 and the patient received two units of packaged red blood cells with a raising hematocrit of 0.32 the next day.
On postoperative day six, the mobilization of the patient under physiotherapy could not be carried out due to increasing pain in the left hip. The thigh was swollen and tight. The peripheral pulses were palpable and symmetrical. The blood count check showed a hematocrit of 0.22, and a sonography of the thigh was carried out. The results were inconclusive, and a CT angiogram was performed. It showed a dislocation of the lesser trochanter in a ventral and cranial direction, whereas the most ventral and caudal part of the displaced fragment was seen close to the profunda femoris artery with radiocontrast agent extravasation (Fig. 3). In addition, a large hemorrhage was depicted in the left vastus medialis muscle.
The patient was taken immediately to the operating room where the hematoma was opened and the profunda femoris artery was identified as the source of bleeding. The lesser trochanter had punctuated the arterial wall and caused a longitudinal tear and a half the arterial circumference extending laceration. Intraoperatively, the patient received 5000 units of intravascular heparin and the lesser trochanter fragment was partially resected. The direct repair of the artery was not successful due to pronounced laceration, and the affected arterial segment had to be resected. Due to the age of the patient and the distal arterial afflux of blood, no profunda arterial graft was carried out and the arterial ends were ligated (Fig. 4).
Perioperatively, the patient received four units of packed red blood cells, and on the medical floor, the patient demonstrated a stable hematocrit and normal vital signs. Remobilization was initiated with a wheeled walker and the course of the remaining hospital stay remained uneventful. He was discharged independently standing and full weight bearing with a hematocrit of 0.41, and symmetrical periphereal pulses.
Discussion
The prevalence of injury to the PFA following the treatment of an intertrochanteric femur fracture with dynamic hip screw or cephalomedullary fixation is 0.21% [1, 6].
PFA injury (0.2%) [1] may be caused by different mechanisms, but is most commonly affiliated with the tip of protruding drills or cortical screws, wound retractors and sharp bone fragments [7,8,9]. In the presented case, it was due to the medial and proximal displacement of the lesser trochanter fragment as a result of the pull of the iliopsoas muscle during postoperative mobilization [3, 10,11,12,13].
The signs of acute bleeding in the clinical setting include hypotension, tachycardia, a decrease in the hematocrit, swelling of the thigh with possibly palpable pulsation and pain. However, this depicted scenario is more frequent when the arterial injury is caused by direct and rapid trauma [8, 14]. As presented in our case, the fall in hematocrit as well as the gradually growing swelling and pain in the left thigh was observed progressively over a period of 12 h. In addition, our patient did not present with any tachycardia or decrease in blood pressure. For surgeons, it is important to recognize early enough the clinical signs of early bleeding [15]. Additionally duplex ultrasonography, computer tomography (CT), CT angiography and magnetic resonance imaging (MRI) may be necessary for diagnosis.
In general, the geriatric population is more prone to those injuries due to the atherosclerotic, fragile and more rigid low-flow arteries [6]. Further risk factors are osteoporosis [16,17,18], unstable fracture patterns [18,19,20], unsatisfactory reduction [17, 18, 21] and inaccurate internal fixation procedures [10, 16,17,18,19,20,21]. Several authors consider that the incidence of a trochanter lesser fragment injuring the PFA has risen in recent years and will continue to rise because of the increasing frequency of these fractures [6, 10].
Lee et al. [22] report that carrying out a candy package wiring technique of the lesser trochanter fragment promotes rehabilitation and prevents fragment dislocation in elderly patients.
In summary, injury to the PFA is rare; however, the geriatric population is more prone to these lesions. Clinical suspicion is the primary key for diagnosis. Gentle and atraumatic intraoperative technique and instrument handling are mandatory to prevent this injury. Furthermore, additional fixation of large fragments of the lesser trochanter may be an option [2, 3].
References
Lazarides MK, Arvanitis DP, Dayantas JN (1991) Iatrogenic arterial trauma associated with hip surgery: an overview. Eur J Vasc Surg 5:549–556
Ryzewicz M, Robinson M, McConnell J, Lindeque B (2006) Vascular injury during fixation of an intertrochanteric hip fracture in a patient with severe atherosclerosis. JBJS 88:2483–2486
Osagie L, Gallivan S, Pearse Y (2015) Profunda femoris injury following lesser trochanter displacement: complications following intramedullary femoral nailing. Injury 46:411–413
Hyde Z, Mylankal KJ, Hankez GJ et al (2013) Peripheral arterial disease increases the risk of subsequent hip fracture in older men: the health in men study. Osteoporos Int 24(5):1683–1688
Lim SJ, Yeo I, Yoon PW et al (2018) Incidence, risk factors, and fracture healing of atypical femoral fractures: a multicenter case-control study. Osteoporos Int 29(11):2427–2435
Karanikas I, Lazarides M, Arvanitis D et al (1993) Iatrogenic arterial trauma associated with hip fracture surgery. Acta Chir Belg 93:284–286
Nasr AY, Badawoud MH, Al-Hayani AA et al (2014) Origin of profunda femoris artery and its circumflex femoral branches: anatomical variations and clinical significance. Folia Morphol 73(1):58–67
Patelis N, Koutsoumpelis A, Papoutsis K, et al (2014) Iatrogenic injury of profunda femoris artery branches after intertrochanteric hip screw fixation for intertrochanteric femoral fracture: a case report and literature review. Case reports in vascular medicine
Laohapoonrungsee A, Sirirungruangsarn Y, Arpornchayanon O (2005) Pseudoaneurysm of profunda femoris artery following internal fixation of intertrochanteric fracture: two cases report. J Med Assoc Thail 88(11):1703–1706
Barquet A, Gelink An Giannoudis PV (2015) Proximal femoral fractures and vascular injuries in adults: incidence, aetiology and outcomes. Injury 46:2297–2313
Whitehell R, Wang GJ, Edwards JR et al (1978) Late injuries to the femoral vessels after fracture of the hip. Case report. JBJS Am 60(4):541–542
Keel JD, Eyres KS (1993) Vascular injury by an intertrochanteric fracture fragment. Injury 24(5):350–352
Klanke J, Stepanek E, Wetermann K (2002) Injury of a branch of the arteria profunda femoris after a pertrochanteric femur fracture. Osteosynth Trauma Care 10(2):76–80
Moreyra CE, Lavernia CJ, Cooke CC (2004) Late vascular injury following intertrochanteric fracture reduction with sliding hip screw. J Surg Orthop Adv 13(3):170–173
McQueen MM, Gaston P, Court-Brown C (2000) Acute compartment syndrome. Who is at risk? JBJS 82(2):200–203
Brunner A, Joeckel JA, Babst R (2008) The PFNA proximal femur nail in treatment of unstable proximal femur fractures: 3cases of postoperative perforation of the helical blade into the hip joint. J Orthop Trauma 22(10):731–736
Bonnaire F, Weber A, Boesl O et al (2007) ‘Cutting out’ bei pertrochantaeren frakturen-ein problem der osteoporose? Unfallchirurg 110(5):425–432
Lucke M, Burghardt RD, Siebenlist S et al (2010) Medial migration of lag screw with intrapelvic dislocation in gamma nailing-a unique problem? A report of 2 cases. J Orthop Trauma 24:e6–11
Weil YA, Gardner MJ, Mikhail G et al (2008) Medial migration of intramedullary hip fixation devises: a biomechanical analysis. Arch Orthop Trauma Surg 128(2):227–234
Flint JH, Sanchez-Navarro CF, Buckwalter JA et al (2010) Intrapelvic migration of a gamma nail lag screw: review of the possible mechanisms. Orthopedics. https://doi.org/10.3928/01477447-20100225-19
Brodell JD, Leve AR (1983) Disengagement and intrapelvic protrusion of the screw from a sliding screw-plate device. JBJS Am 65(5):697–701
Lee JM, Cho Y, Kim J et al (2017) Wiring techniques for the fixation of trochanteric fragments during bipolar hemiarthroplasty for femoral intertrochanteric fracture: clinical study and technical note. Hip Pelvis 29(1):44–53
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kanovsky, A., Mueller, E.J. & Miller, E. Secondary profunda femoris artery injury after intramedullary femoral nailing in a geriatric pertrochanteric femur fracture: case report. Eur J Orthop Surg Traumatol 29, 1811–1814 (2019). https://doi.org/10.1007/s00590-019-02500-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02500-9