Abstract
Purpose
Spinopelvic parameters can be useful in identifying risk factors for lumbar degenerative disc disease, but few studies assess patients with single-level disc herniation and most do not evaluate symptoms. This comparative retrospective study was aimed to analyse spinopelvic parameters, symptoms and MRI changes in patients with single-level lumbar disc herniation undergoing conservative or surgical treatment.
Methods
Patients with clinical and radiological assessment (Japanese Orthopaedic Association Score) and an MRI evaluation of the lumbar spine were identified and divided into two groups: surgically treated (group A) and not requiring surgery (group B). Spinopelvic parameters were determined on standing profile radiographs of the lumbar spine and pelvis, and mean values were compared to those reported in the literature for normal subjects. MRI findings were graded according to the system described by Pfirrmann et al.
Results
The study included 71 patients with single-level lumbar disc herniation: 26 in group A (39.4 ± 12.1 years) and 45 in group B (51.4 ± 17.2 years). The notable differences in spinopelvic parameter means between the two groups did not reach statistical significance. A positive correlations of age with pelvic tilt and Pfirrmann changes with pelvic incidence was only found in group A, while both groups showed highly significant positive correlations of pelvic incidence with the spine’s conformational type (p = 0.001).
Conclusions
Characteristic changes in spinopelvic parameters identified in patients with lumbar degenerative disc disease were a reduction in pelvic incidence, sacral slope and lumbar lordosis, with an increased pelvic tilt. These were found to correlate with MRI changes in surgically treated patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Low back pain (LBP) is one of the most common medical problems that can lead to temporary or permanent disabilities, associated with an important socioeconomic and healthcare burden [1]. With an estimated point prevalence of 11.9 ± 2.0 %, as much as 50–70 % of the general population suffers from at least one episode of LBP in their lifetime [2, 3]. Although LBP is not a disease in itself, rather a series of symptoms, one of its major causes is lumbar degenerative disc disease [4]. In spite of progresses made in clinical and basic research, there is still no general consensus regarding risk factors and physiopathological mechanisms involved [1, 5, 6].
Introduced around 1985, the concept of sagittal balance has been widely used in the assessment and management of spinal disorders, with growing interest in the study of spinopelvic parameters in the last three decades [7–9]. Continuing the work of During and Duval-Beaupère [10, 11], a series of authors have highlighted the importance of sagittal balance in spinal pathology [12–16]. Among them Roussouly played a key role in promoting the concept by creating a classification in the asymptomatic population [17]. Other studies conducted in asymptomatic patients revealed correlations between spinopelvic parameters and the sagittal curvatures of the spine, especially the lower arch of the lumbar lordosis (LL), corresponding to L4–S1 vertebrae [12].
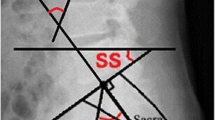
It is generally believed that the form and spatial orientation of the pelvis determine the organization of the spine and its curvatures. Lateral view radiographs can be used to identify the shape of the pelvis through assessment of the pelvic incidence (PI), a fix anatomical angle that is specific for each individual and does not suffer any changes after adolescence. This parameter is linked with two other pelvic measurements: pelvic tilt (PT) and sacral slope (SS); their interdependency can be expressed using the mathematical formula PI = PT + SS. While PI has a fixed value, uninfluenced by external factors, both PT and SS depend upon a series of factors. Firstly, PT characterises the rotation of the pelvis around the femoral heads–backwards rotation (retroversion) of the pelvis increases PT, while forward rotation (anteversion) decreases the value of PT. Secondly, SS can be defined as a compensatory angle of PT characterised by the position of the sacral S1 endplate (Fig. 1).
Patients with degenerative disc disease often show a loss of LL, which has to be compensated in the spinal alignment in order to re-establish pelvic sagittal balance; any imbalance can be a source of pain manifested as LBP. As a morphological parameter, PI is unmodified by degenerative changes so its correlation with LL might offer information about sagittal balance in patients with lumbar degenerative disc disease. Several studies have shown that degenerative disc disease, degenerative or isthmic spondylolisthesis and degenerative scoliosis may be related to specific changes in the sagittal balance of the spine [13, 15, 18]. However, few studies were made on patients with single-level disc herniation and most did not assess patient symptoms, in spite of their importance in treatment decisions. This retrospective study comparatively analysed spinopelvic parameters, symptoms and MRI changes in patients with single-level lumbar disc herniation undergoing conservative or surgical treatment.
Materials and methods
The study was based on the premise that degenerative spinal disorders associate specific changes of sagittal balance of the spine. We hypothesised that in the case of single-level lumbar disc herniation, sagittal balance parameters will show different correlations with symptomatology and MRI changes in patients with an indication for conservative versus surgical treatment.
This retrospective observational study included patients diagnosed with lumbar degenerative disc disease between October 2012 and January 2015 in the Clinic of Orthopaedics and Traumatology II of the Timișoara Emergency County Hospital. The study protocol was approved by the local ethics committee, and the study was prepared according to the STROBE statement for observational studies (STROBE checklist version 4).
Inclusion criteria were the concomitant presence of a single-level lumbar disc herniation, a thorough clinical and radiological assessment (including the Japanese Orthopaedic Association—JOA score for low back pain), and an MRI evaluation of the lumbar spine (data from machines with a minimum of 1.5 T, sagittal T1-weighted spin-echo and T2-weighted fast spin-echo sequences). Patients with missing clinical, radiological or MRI data, as well as prior surgical interventions on the lumbar spine were excluded from the study. Further exclusion criteria were the presence of multilevel disc herniation, presence of spinal deformities (scoliosis/spondylolisthesis), spinal tumours, or disorders of the hip and pelvic girdle that could influence spinal sagittal balance measurements.
All patients underwent an initial 6 weeks of conservative treatment. Clinical, demographic and imagistic data were retrieved from patient records. Patients were divided into two groups according to the JOA score at the end of the initial 6 weeks of conservative treatment. The score’s value (ranging from −6 to 29) was used to determine the indication for surgical treatment—a value <14 was regarded as a sign of the necessity of an operative intervention. Group A included patients who received surgical treatment by microdiscectomy. Group B consisted of patients that had a positive response to conservative treatment in the first 6 weeks and did not require surgery. All patients were treated by the same team of surgeons, regardless of the treatment type (conservative or surgical).
Standing profile radiographs of the lumbar spine and pelvis were used to determine spinopelvic parameters according to the protocol described by Roussouly et al. [17] and to determine spinal conformational type (Fig. 2). Radiographic images in DICOM format were processed using Surgimap Spine 2.1.2 software (Nemaris Inc., New York, USA) for pelvic sagittal balance measurements. Target spinopelvic parameters were PI, PT, SS, LL and upper and lower arch of LL (Fig. 3). Of these, PI was measured as the angle between the perpendicular drawn from the middle of the S1 endplate and the line connecting the bi-coxo-femoral axis to the middle of the S1 endplate; PT was determined as the angle between the line connecting the middle of the S1 endplate to the bi-coxo-femoral axis and the vertical axis, while SS corresponded to the angle between the sacral endplate and the horizontal axis. Thus, both PT and SS vary depending on the orientation of the pelvis. The Cobb method was used to determine LL between the upper endplates of S1 and L1; the upper and lower arches of LL were measured between L1 and L4, and L4 and S1, respectively.
In order to analogize the values of these spinopelvic parameters with the ones found in the asymptomatic population, the mean values obtained were statistically compared to the means published by Chaléat-Valayer et al. [19] for a cohort of 709 normal subjects.
MRI data were analysed and classified by two of the authors, using the grading system described by Pfirrmann et al. [20] for lumbar intervertebral disc degeneration. This recognises 5 grades, based on the height and structure of the intervertebral disc, distinction of nucleus pulposus and annulus fibrosus, and signal intensity on T2-weighted images.
Statistical analysis of data was performed using SPSS 20.0 Statistical Software (IBM Corporation, Armonk, NY, USA), and data were expressed as mean ± SD. The Pearson r coefficient was used to evaluate correlations between demographic, clinical and imagistic data, and the studied spinopelvic parameters. Student’s t test was used for comparing mean spinopelvic parameters in the included patients with the published values for the asymptomatic population. For all tests, a p value ≤0.05 was considered statistically significant and a p value ≤0.001 was considered highly significant.
Results
The study involved a series of 71 patients that presented adequate clinical and imagistic assessment: 26 were included in group A (14 males, 12 females) and 45 in group B (23 males, 22 females). Mean age was 39.4 ± 12.1 years in group A and 51.4 ± 17.2 years in group B. Based on sagittal balance type according to the classification of Roussouly, patients from group A showed a predominance of conformational types II and I (50.0 and 23.07 % of cases), while in group B types III and I were predominant (40.0 and 33.33 %, respectively)—Fig. 4 shows a representative case from each group. There were notable differences in spinopelvic parameter means between the two groups, especially in PI and LL, but without reaching statistical significance (Tables 1, 3).
Patient age was significantly positively correlated with PT in group A, without a similar correlation in group B; there was also a positive correlation of age with Pfirrmann changes in both groups (Table 2). Age was positively correlated with the upper arch of LL and LL in group A (p = 0.004 and p = 0.028, respectively). The latter correlation was not observed in group B.
The JOA score values were positively correlated with MRI changes in both groups, but a correlation with the spine’s conformational type was only found in group B. Pfirrmann changes found in both groups were positively correlated with PT, LL and the upper arch of LL (L1–L4), while a correlation of MRI changes with PI was only identified in patients from group A (p = 0.001).
A highly significant positive correlation of PI was found with conformational type in both patient groups (p = 0.001), with significant negative correlations of PI with LL and the lower arch of LL (L4–S1)—these negative correlations were stronger for group A.
Although there was a highly significant negative correlation of SS with LL and the lower arch of LL in both groups, patients from group A showed a stronger correlation.
There were no statistically significant differences in the mean values of PI, PT, SS and LL between the two patient groups (Table 3). When compared to the mean values observed in the asymptomatic population, there were statistically significant differences between the means of both SS and LL for both patient groups. However, mean PI values were significantly different only between patients from group A and normal subjects, while the same was found for mean PT values for patients in group B as compared to asymptomatic subjects.
Discussion
The pelvis’ relative position to the spine is a decisive factor influencing spinal curvatures. As there are no standard pelvis sagittal balance values available for the general population, normal physiological curvatures of the spine are hard to define [21, 22]. It seems that the most important factor is the congruence between spine curvatures, yielding an optimal position that is maintainable with minimal muscular effort, with the body’s weight axis in a physiological position [22, 23]. Thus, determining the spatial position of the pelvis is of paramount importance, and measuring spinopelvic parameters can offer valuable information about this factor.
Loses of LL have important consequences on spinal alignment and must be compensated to maintain pelvic sagittal balance. In patients with degenerative disc disease, the loss of LL is a frequent find that has the potential to influence sagittal balance; LBP in these patients suggests that the imbalance can be a source of pain.
In the asymptomatic general population, authors found a major correlation between LL and SS, leading Roussouly et al. [17] to define their classification of sagittal balance. As a morphological parameter, PI is not influenced by degenerative changes, so its correlations might offer important clues about sagittal balance in a population with lumbar degenerative disc disease.
Our results show that patients with degenerative disc disease have a sagittal balance profile with an average small PI, a large PT and reduced SS. These changes were associated with a decrease in LL, indicating a “flat-back”-type posture, more pronounced in patients that needed surgical treatment (group A). It is important to note that the reduction in LL may result not only from loss of vertebral body height, but also from adopting an antalgic posture to reduce pressure on the rear portion of the intervertebral disc. The decrease in LL occurs prior to moving to the C7 plumb line, leading to postural imbalance. This imbalance can be compensated to a certain degree by retroversion of the pelvis, but the compensatory ability is limited. Because PI is the most reliable indicator of this ability to compensate for LL loss, it is interesting to note that in patients with degenerative disc disease the value of this parameter is often low [13, 22, 24, 25]. These observations are consistent with the results of our study—patients in both groups showed higher mean values of PT (reaching statistical significance when comparing group B with normal subjects) and significantly lower mean values of SS and LL compared to the values reported in the literature for asymptomatic individuals [19].
Barrey et al. [22] have reported a tendency of increased LL in patients over the age of 45, implying the presence of a higher LL in the elderly; our results were different, with a correlation found between age and LL only in patients from group A, whose mean age was lower compared to group B.
Although the clinical score values correlated with MRI changes in both groups, only group B showed JOA score correlations with sagittal balance conformational type—this may be due to the small number of patients in group A. The fact that Pfirrmann MRI changes were significantly correlated with PT suggests that degenerative lesions precede the specific pelvic balance redress mechanisms, such as pelvic retroversion.
Given the higher average age of patients from group B, degenerative disc disease changes might be overlapped with the normal changes of ageing; however, this is not the case for patients in group A, where the low average age suggests only the presence of degenerative disease. In addition, 73.07 % of patients in group A showed a type II or type I sagittal balance, corresponding to the “flat-back”-type posture often associated with disc pathology, whereas in group B 40 % of patients were classified into type III, considered to have the most harmonious curves of the spine. This suggests that in group B a fairly large proportion of disc degenerative changes might be due to the normal ageing process. However, almost the same numbers of patients (33.33 %) were classified as conformational type I, so group B showed a notable heterogeneity.
The study’s main limitations are due to the small number of patients included, which hindered appropriate stratification, and as such resulting subgroups did not allow us to draw definite conclusions. A second important limitation is the absence of a control group of healthy subjects—this was partially corrected by comparing the found spinopelvic parameters to the values reported in the literature, but unfortunately these data vary from one study to another. However, the present study has the benefit of assessing and correlating patient symptoms with a series of spinopelvic parameters important for sagittal balance and will serve as a starting point for prospective investigations.
Conclusions
Patients with single-level lumbar degenerative disc disease that underwent surgical treatment presented fundamental changes of spinopelvic parameters: reduced PI, SS and LL compared to patients treated by conservative means. Also, patients in need of surgical treatment tend to have Roussouly conformational types II and I, with a significantly lower PI compared to normal subject, which correlates with Pfirrmann MRI changes.
References
Katz JN (2006) Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am 88(Suppl 2):21–24. doi:10.2106/JBJS.E.01273
Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, Woolf A, Vos T, Buchbinder R (2012) A systematic review of the global prevalence of low back pain. Arthritis Rheum 64(6):2028–2037. doi:10.1002/art.34347
Hoy D, Brooks P, Blyth F, Buchbinder R (2010) The Epidemiology of low back pain. Best Pract Res Clin Rheumatol 24(6):769–781. doi:10.1016/j.berh.2010.10.002
Schmidt CO, Raspe H, Pfingsten M, Hasenbring M, Basler HD, Eich W, Kohlmann T (2007) Back pain in the German adult population: prevalence, severity, and sociodemographic correlates in a multiregional survey. Spine (Phila Pa 1976) 32(18):2005–2011. doi:10.1097/BRS.0b013e318133fad8
Taher F, Essig D, Lebl DR, Hughes AP, Sama AA, Cammisa FP, Girardi FP (2012) Lumbar degenerative disc disease: current and future concepts of diagnosis and management. Adv Orthop 2012:970752. doi:10.1155/2012/970752
Oprea M, Popa I, Cimpean AM, Raica M, Poenaru DV (2015) Microscopic assessment of degenerated intervertebral disc: clinical implications and possible therapeutic challenge. Vivo 29(1):95–102
Vaz G, Roussouly P, Berthonnaud E, Dimnet J (2002) Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J 11(1):80–87
Barrey C, Roussouly P, Le Huec JC, D’Acunzi G, Perrin G (2013) Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J 22(Suppl 6):S834–S841. doi:10.1007/s00586-013-3030-z
Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW (1995) An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine (Phila Pa 1976) 20(12):1351–1358
During J, Goudfrooij H, Keessen W, Beeker TW, Crowe A (1985) Toward standards for posture. Postural characteristics of the lower back system in normal and pathologic conditions. Spine (Phila Pa 1976) 10(1):83–87
Duval-Beaupère G, Legaye J (2004) Composante sagittale de la statique rachidienne (in French). Rev Rhum 71:105–119. doi:10.1016/j.rhum.2003.09.018
Le Huec JC, Faundez A, Dominguez D, Hoffmeyer P, Aunoble S (2015) Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop 39(1):87–95. doi:10.1007/s00264-014-2516-6
Mehta VA, Amin A, Omeis I, Gokaslan ZL, Gottfried ON (2015) Implications of spinopelvic alignment for the spine surgeon. Neurosurgery 76(Suppl 1):S42–S56; discussion S56. doi:10.1227/01.neu.0000462077.50830.1a
Lazennec JY, Ramare S, Arafati N, Laudet CG, Gorin M, Roger B, Hansen S, Saillant G, Maurs L, Trabelsi R (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9(1):47–55
Ferrero E, Ould-Slimane M, Gille O, Guigui P, French Spine S (2015) Sagittal spinopelvic alignment in 654 degenerative spondylolisthesis. Eur Spine J 24(6):1219–1227. doi:10.1007/s00586-015-3778-4
Dai J, Yu X, Huang S, Fan L, Zhu G, Sun H, Tang X (2015) Relationship between sagittal spinal alignment and the incidence of vertebral fracture in menopausal women with osteoporosis: a multicenter longitudinal follow-up study. Eur Spine J 24(4):737–743. doi:10.1007/s00586-014-3637-8
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30(3):346–353
Aykac B, Ayhan S, Yuksel S, Guler UO, Pellise F, Alanay A, Perez-Grueso FJ, Acaroglu E, Group EESS (2015) Sagittal alignment of cervical spine in adult idiopathic scoliosis. Eur Spine J 24(6):1175–1182. doi:10.1007/s00586-015-3868-3
Chaleat-Valayer E, Mac-Thiong JM, Paquet J, Berthonnaud E, Siani F, Roussouly P (2011) Sagittal spino-pelvic alignment in chronic low back pain. Eur Spine J 20(Suppl 5):634–640. doi:10.1007/s00586-011-1931-2
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26(17):1873–1878
Vrtovec T, Pernus F, Likar B (2009) A review of methods for quantitative evaluation of spinal curvature. Eur Spine J 18(5):593–607. doi:10.1007/s00586-009-0913-0
Barrey C, Jund J, Noseda O, Roussouly P (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 16(9):1459–1467. doi:10.1007/s00586-006-0294-6
Legaye J, Duval-Beaupere G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7(2):99–103
Johnson RD, Valore A, Villaminar A, Comisso M, Balsano M (2013) Sagittal balance and pelvic parameters–a paradigm shift in spinal surgery. J Clin Neurosci 20(2):191–196. doi:10.1016/j.jocn.2012.05.023
Le Huec JC, Charosky S, Barrey C, Rigal J, Aunoble S (2011) Sagittal imbalance cascade for simple degenerative spine and consequences: algorithm of decision for appropriate treatment. Eur Spine J 20(Suppl 5):699–703. doi:10.1007/s00586-011-1938-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Mardare, M., Oprea, M., Popa, I. et al. Sagittal balance parameters correlate with spinal conformational type and MRI changes in lumbar degenerative disc disease: results of a retrospective study. Eur J Orthop Surg Traumatol 26, 735–743 (2016). https://doi.org/10.1007/s00590-016-1842-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-016-1842-3