Abstract
Purpose
A retrospective cross-sectional study was designed to explore the role of spinopelvic sagittal alignment in upper lumbar disc herniation (ULD) development.
Methods
A total of 207 consecutive patients who underwent surgery for single-level lumbar disc herniation [24 with ULD and 183 with lower lumbar disc herniation (LLD)] and 40 asymptomatic volunteers were enrolled. Full-length radiographs of the spine were taken to evaluate pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), thoracic kyphosis (TK), lumbar lordosis (LL), and sagittal vertical axis (SVA). The Roussouly classification was utilized to categorize all subjects according to their sagittal alignment. Spinopelvic parameters and Roussouly classification results were compared between groups.
Results
There were significant differences in PI, SS, PT, LL, and SVA between the ULD, LLD, and control groups. PI in the ULD (40.9°) was significantly lower than in the LLD and control groups (48.8° and 47.6°, respectively). LL was significantly lower in the ULD than in the LLD (−32.4° and −40°, respectively). There were significant differences between the three groups in Roussouly types. The LLD had a significantly higher proportion (62.6 %) of type 2 lordosis (flat back), and the ULD had a higher proportion (33.3 %) of type 1 lordosis than the other groups.
Conclusions
This study demonstrated the importance of PI and lumbar curvature in the pathogenesis of ULD. The higher prevalence of short LL and long TK with low PI in the ULD group implies that an increased mechanical stress at this level may be one of the risk factors of ULD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic incidence (PI), which was first described by Duval-Beaupère et al. is an individualized morphological parameter not affected by posture and considered to be a permanently invariable parameter involved in the regulation of the sagittal alignment of the spine and pelvis [1, 2]. Additionally, being unaffected by lumbar degenerative changes, PI represents a constant guide value facilitating the understanding of variations in the patient population [1, 3–6].
In light of the beginning of the era of sagittal balance, many studies have been published about the influence of spinopelvic parameters on sagittal imbalance and degenerative disease, including spondylolisthesis [3, 7–12]. In degenerative spondylolisthesis, high PI was proved to be a predisposing factor since a greater sacral slope (SS) and lumbar lordosis (LL) resulted in a greater shear force at the lumbosacral junction [13–17].
Upper lumbar disc (ULD) herniation is relatively uncommon. Thus, approximately 5 % of lumbar disc herniation cases are reported to occur at the upper lumbar spine [18, 19]. The definition of ULD is somewhat debatable. Although in the present study, ULDs are defined as the L1–2 and L2–3 levels, some authors included the T12–L1 and L3–4 levels in this definition. Sanderson et al. reported that the characteristics and clinical outcomes of L3–4 disc herniation patients matched much more closely those of L4–5 and L5–S1 disc herniation patients, and therefore they proposed that future studies of upper versus lower disc herniation should include L3–L4 herniation in the lower category [20].
Because of the rarity of ULD, its pathogenesis has not been thoroughly studied. Most studies dedicated to lumbar disc degeneration or herniation included only the lower lumbar spine. We assumed that, similar to other lumbar degenerative diseases, spinopelvic parameters and lumbar curvature might influence the pathogenesis of ULD. However, there is little information on the changes of spinopelvic parameters in patients with ULD, especially in terms of PI. The purpose of this study was to evaluate the influence of spinopelvic parameters in patients with ULD and to compare them with spinopelvic parameters in a normal population as well as in patients with lower lumbar disc herniation (LLD).
Materials and methods
Patient population
After approval of Institutional Review Board of our institute, we retrospectively evaluated a total of 207 patients less than 60 years old who underwent open lumbar discectomy or percutaneous endoscopic discectomy for single-level symptomatic lumbar disc herniation between January 2010 and January 2012. Patients with spondylolysis, tumor, trauma, congenital or acquired deformity, infection, and history of spine surgery were excluded. The study group comprised 139 men and 67 women with the mean age of 43.7 years (range 19–59). There were eight patients with herniation of the nucleus pulposus at L1–2, 16 at L2–3, 19 at L3–4, 96 at L4–5, and 67 at L5–S1. The L1–2 and L2–3 discs were defined as ULDs, and the L3–4, L4–5, and L5–S1 discs were defined as LLDs [20]. Table 1 shows the results of comparison of demographic data between the groups.
As a control group, 40 healthy volunteers (15 women and 25 men; mean age 33.6 years; age range 19–53) without spinal pathology were recruited.
Radiographic evaluation
Full-length radiographs of the spine extending from the base of the skull to the proximal femur in the anteroposterior and lateral planes were obtained. The radiographs were digitized and analyzed by a team of researchers. An independent observer measured all radiographic parameters using a dedicated software package with a built-in picture-archiving communication system (PiView; INFINITT Co Ltd, Seoul, South Korea). For radiography of the spine, each patient was asked to stand comfortably erect. The arms were flexed, the hands were placed on the clavicles, and the knees were extended. Two 30 cm × 90 cm exposures from the base of the skull to the proximal femur in the posterior to anterior plane and in the left to right lateral plane were obtained. The distance from the radiographic source to the film was maintained at 230 cm for all exposures. Full-length standing anteroposterior and lateral radiographs were taken preoperatively.
Sagittal balance was determined by measuring the sagittal vertical axis (SVA) with a plumb line from the center of the C7 vertebral body to the posterior sacral prominence on the lateral radiograph. A regional sagittal modifier was included to describe each of the two regions of the spine: main thoracic kyphosis (TK), and lumbar lordosis (LL). Main TK was measured from the T5 superior endplate to the T12 inferior endplate. LL was measured from the T12 inferior endplate to the S1 superior endplate by the Cobb method. The pelvic parameters, PI, sacral slope (SS), and pelvic tilt (PT), were measured in each whole spine lateral view. SS is the angle between the S1 superior endplate and a horizontal line. PT is defined as the angle between a vertical line originating at the center of the bicoxofemoral axis and a line drawn between the same point and the middle of the superior endplate of S1. PI is defined as the angle between the line perpendicular to the sacral plate and the line connecting the midpoint of the sacral plate to the bicoxofemoral axis (Fig. 1).
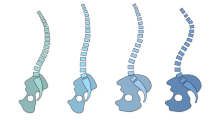
The Roussouly classification was utilized for describing variations in the sagittal morphology of the spine as shown in Fig. 2.
The four types of the Roussouly sagittal classification. The shape of lumbar lordosis depends on sacral slope (SS) orientation. Types 1 and 2 have SS < 35°, type 3 has 35° < SS < 45°, and type 4 has SS > 45°. Generally, the PI is low in types 1 and 2 and high in type 3. Note the location of the apex of the lumbar lordosis. In type 1, it is in the center of the L5 vertebral body; in type 2, it is at the base of the L4 vertebral body; in type 3, it is in the center of the L4 vertebral body; and in type 4 it is in the center of the L4 vertebral body or higher
The presence of retrolisthesis and spondylolisthesis at or adjacent to the level of herniation was assessed to evaluate instability.
Statistical analysis
Statistical analysis was performed using SPSS 14.0K (SPSS Inc., Chicago, IL). A probability value <0.05 was considered to indicate a statistically significant difference. The Mann–Whitney U test, Kruskal–Wallis test for non-parametric data and student t test, one-way analysis of variance (ANOVA) for parametric data were used to compare the variables. Bonferroni post hoc test was utilized for subgroup comparison after ANOVA test.
Results
Table 2 shows spine and pelvic parameters in the ULD, LLD, and control groups. There were significant differences in PI, SS, PT, LL, and SVA between the three groups. A post hoc test (Table 3) revealed that PI was significantly lower in the ULD group than in the LLD and control groups. Both the ULD and LLD groups had significant lower SS than the control group (p = 0.000 and 0.002, respectively). LL was significantly lower in the ULD group than in the LLD group (p = 0.006), while there was no difference with the control group (p = 0.182). In terms of SVA, both the ULD and LLD groups showed significantly higher values than the control group (p = 0.000 in both cases).
Nine (37.5 %) cases of retrolisthesis at or adjacent to the level of herniation were identified in the ULD group, whereas no such cases were present in the LLD group. No cases of spondylolisthesis were observed.
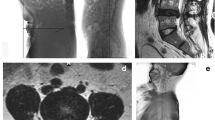
Table 4 compares the results of the Roussouly classification in the ULD, LLD, and control groups. The Kruskal–Wallis test showed significant differences between the groups (p = 0.001). The proportion of type 2 lordosis (flat back) was significantly higher in the LLD group (62.6 %), while the ULD group had a higher proportion (33.3 %) of type 1 lordosis than the control group (Figs. 3, 4).
An illustration of upper lumbar disc herniation. T2 sagittal magnetic resonance imaging (MRI) a shows disc herniation at the L2–3 level. Note the lumbarization of the S1 vertebra. A whole spine lateral radiograph b shows Roussouly type 1 lordosis and low PI and SS. (PI = 37°, SS = 12°, LL = −27°, and TK = 36°)
Discussion
The present study shows a significant correlation between the location of disc herniation and spinopelvic alignment. Thus, the ULD group had significantly lower PI and LL than then the LLD and control groups. Furthermore, both the ULD and LLD groups had decreased SS and anterior shifting of sagittal balance in comparison with the control group. Decreased LL and SS in disc herniation have been previously reported by many authors [7, 12, 21]. Flat lumbar spine is caused by segmental discopathy or loss of disc height, a postural change secondary to an analgesic response to avoid posterior disc hyperpression, or foraminal stenosis due to a herniated disc and tonic contraction of the surrounding lumbopelvic muscles [12, 22]. Decreased SS indicates pelvic retroversion as a mechanism of compensating for the loss of LL and preserving sagittal balance. Sagittal imbalance due to loss of lordosis is also partially corrected by the pelvic retroversion [12]. In the present study, PT in the LLD group was greater than in the ULD and control groups because the high PI in the LLD group permitted a greater range of pelvic retroversion, which led to a more efficient alleviation of the loss of lordosis than in the ULD group. Our spinopelvic parameters in disc herniation are concordant with the results of previous studies of spinopelvic parameters and lumbar disc degeneration [7, 12, 22].
The ULD groups had significantly lower PI (40.9°) than the LLD and control groups (48.8° and 47.6°, respectively, p = 0.000). The interpretation of this finding is more straightforward if the results of the Roussouly classification are taken into account. The ULD and LLD groups had significantly higher rates of Roussouly type 1 (39.5 %) and type 2 (66.3 %), respectively. According to the Roussouly classification of sagittal alignment of the lumbar spine, type 1 is a combination of kyphosis and short lordosis at the lower arc of the spine, and type 2 represents flat back [6]. In type 1 lordosis, SS is less than 35°, and this is associated with a low PI. In the upper spine, the kyphosis of the thoracolumbar junction is significant, and the kyphosis and lower arc of lordosis are minimal. In type 2 lordosis, the entire spine is relatively hypolordotic and hypokyphotic, and the lower arc of lordosis is relatively flat. In light of this difference in sagittal alignment, Roussouly proposed the concept of degenerative evolution and pathological balance [10]. In type 1 lordosis, junctional discs between the thoracolumbar kyphosis and the lumbar lordosis are tilted with a risk of retrolisthesis, while lower lumbar discs (L4–5 and L5–S1) are generally preserved from degeneration. In type 2 lordosis, the risk of early disc degeneration with central disc herniation is increased because the orientation of the disc is horizontal and the disc pressure is maximal.
Many authors reported that mechanical stress influences the pathogenesis of ULD. Hu et al. found that isolated high lumbar disc degeneration is often associated with pre-existing abnormalities such as end-plate defects, Scheuermann’s disease, limbus vertebra, and others, as well as repeating work activities that put high stress on the spine, such as in construction workers, airplane mechanics, etc. [23]. They concluded that altered mechanics are associated with frequent lumbar disc pathologies. Xu et al. showed that ULD was significantly related to presence of adjacent wedge-shaped vertebrae and larger kyphotic angle at the adjacent segment [24]. They postulated that shear stress and compression forces secondary to the presence of wedge-shaped vertebrae may induce biomechanical changes that accelerate the degeneration of adjacent discs at upper lumbar levels. In the present study, ULD was also associated with increased stress at the thoracolumbar junction in Roussouly type 1 lordosis with lower PI. In the pathogenesis of lumbar disc herniation, disruption of disc structure due to excessive mechanical loading is important [25]. Kyphosis of the upper lumbar spine concentrates transitional stress between the rigid thoracic spine with the rib cage and short lordosis of the lower lumbar spine. In this regard, we observed a high prevalence of retrolisthesis in the L1–2 and L2–3 cases (nine out of 24 cases).
The present study determined that retrolisthesis is highly prevalent in ULD. This is concordant with the results of previous studies, which reported that backward slip was common in upper lumbar vertebrae with low PI and considered it a compensatory mechanism for sagittal imbalance in lumbar degenerative diseases [8, 26]. Although Shen et al. showed that there is no relationship between retrolisthesis and disc degeneration at the L5–S1 level [27], the pathogenesis of ULD is different from that of LLD [20]. It seems that mechanical stress that concentrates at the junction of thoracic kyphosis and lumbar lordosis in patients with low PI plays a key role in the development of ULD.
To the best of our knowledge, this is the first study of the role of global sagittal balance in the pathogenesis of ULD. ULD groups had significantly lower PI and Roussouly type 1 lordosis, whereas LLD group had higher PI with Roussouly type 2 lordosis.
There are some limitations to this study. The number of ULD in this study is relatively low because of rarity of its incidence. Multicenter study with larger cohort would strength this result. In addition, many other factors leading to disc herniation need to be investigated in future longitudinal studies for more accurate evaluation.
Conclusions
Because of the rarity of ULD, its etiology has not been understood as well as that of LLD. This study demonstrated the importance of PI and lumbar curvature in the pathogenesis of ULD. The higher prevalence of short LL and long TK with low PI in ULD patients indicates the presence of increased mechanical stress at this level. A further longitudinal study is necessary to clarify how the mechanical stress impacts ULD development among multiple other factors.
References
Legaye J, Duval-Beaupere G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20:451–462
Schwab F, Lafage V, Patel A, Farcy JP (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 34:1828–1833. doi:10.1097/BRS.0b013e3181a13c08
Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, Kim YJ (2009) Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976) 34:785–791. doi:10.1097/BRS.0b013e31819d0c86
Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, Prat-Pradal D, Legaye J, Duval-Beaupere G, Pelissier J (2006) Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 15:415–422. doi:10.1007/s00586-005-0984-5
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30:346–353 (00007632-200502010-00016)
Yang X, Kong Q, Song Y, Liu L, Zeng J, Xing R (2014) The characteristics of spinopelvic sagittal alignment in patients with lumbar disc degenerative diseases. Eur Spine J 23:569–575. doi:10.1007/s00586-013-3067-z
Jeon CH, Park JU, Chung NS, Son KH, Lee YS, Kim JJ (2013) Degenerative retrolisthesis: is it a compensatory mechanism for sagittal imbalance? Bone Joint J 95-B:1244–1249. doi:10.1302/0301-620X.95B9.31237
Bae JS, Jang JS, Lee SH, Kim JU (2012) Radiological analysis of lumbar degenerative kyphosis in relation to pelvic incidence. Spine J 12:1045–1051. doi:10.1016/j.spinee.2012.10.011
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20(Suppl 5):609–618. doi:10.1007/s00586-011-1928-x
Schwab F, Patel A, Ungar B, Farcy JP, Lafage V (2010) Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 35:2224–2231. doi:10.1097/BRS.0b013e3181ee6bd4
Barrey C, Jund J, Noseda O, Roussouly P (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 16:1459–1467. doi:10.1007/s00586-006-0294-6
Liu H, Li S, Zheng Z, Wang J, Wang H, Li X (2014) Pelvic retroversion is the key protective mechanism of L4–5 degenerative spondylolisthesis. Eur Spine J 24:1204–1211. doi:10.1007/s00586-014-3395-7
Funao H, Tsuji T, Hosogane N, Watanabe K, Ishii K, Nakamura M, Chiba K, Toyama Y, Matsumoto M (2012) Comparative study of spinopelvic sagittal alignment between patients with and without degenerative spondylolisthesis. Eur Spine J 21:2181–2187. doi:10.1007/s00586-012-2374-0
Schuller S, Charles YP, Steib JP (2011) Sagittal spinopelvic alignment and body mass index in patients with degenerative spondylolisthesis. Eur Spine J 20:713–719. doi:10.1007/s00586-010-1640-2
Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O’Brien M (2005) The importance of spino-pelvic balance in L5–S1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine (Phila Pa 1976) 30:S27–S34 (00007632-200503151-00007 [pii])
Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O’Brien M, Chopin D, Hresko T, Dimnet J (2004) Spondylolisthesis, pelvic incidence, and spinopelvic balance: a correlation study. Spine 29:2049–2054. doi:10.1097/01.brs.0000138279.53439.cc
Sanderson SP, Houten J, Errico T, Forshaw D, Bauman J, Cooper PR (2004) The unique characteristics of “upper” lumbar disc herniations. Neurosurgery 55:385–389. doi:10.1227/01.neu.0000129548.14898.9b
Albert TJ, Balderston RA, Heller JG, Herkowitz HN, Garfin SR, Tomany K, An HS, Simeone FA (1993) Upper lumbar disc herniations. J Spinal Disord 6:351–359
Sanderson SP, Houten J, Errico T, Forshaw D, Bauman J, Cooper PR (2004) The unique characteristics of “upper” lumbar disc herniations. Neurosurgery 55:385–389 (discussion 389)
Rajnics P, Templier A, Skalli W, Lavaste F, Illes T (2002) The importance of spinopelvic parameters in patients with lumbar disc lesions. Int Orthop 26:104–108
Endo K, Suzuki H, Tanaka H, Kang Y, Yamamoto K (2010) Sagittal spinal alignment in patients with lumbar disc herniation. Eur Spine J 19:435–438. doi:10.1007/s00586-009-1240-1
Hsu K, Zucherman J, Shea W, Kaiser J, White A, Schofferman J, Amelon C (1990) High lumbar disc degeneration. Incidence and etiology. Spine 15:679–682
Xu JX, Yang SD, Wang BL, Yang DL, Ding WY, Shen Y (2015) Correlative analyses of isolated upper lumbar disc herniation and adjacent wedge-shaped vertebrae. Int J Clin Exp Med 8:1150–1155
Adams MA, Roughley PJ (2006) What is intervertebral disc degeneration, and what causes it? Spine (Phila Pa 1976) 31:2151–2161. doi:10.1097/01.brs.0000231761.73859.2c
Jeon I, Kim SW (2015) Retrolisthesis as a compensatory mechanism in degenerative lumbar spine. J Korean Neurosurg Soc 57:178–184. doi:10.3340/jkns.2015.57.3.178
Shen M, Razi A, Lurie JD, Hanscom B, Weinstein J (2007) Retrolisthesis and lumbar disc herniation: a preoperative assessment of patient function. Spine J 7:406–413. doi:10.1016/j.spinee.2006.08.011
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Bae, J., Lee, SH., Shin, SH. et al. Radiological analysis of upper lumbar disc herniation and spinopelvic sagittal alignment. Eur Spine J 25, 1382–1388 (2016). https://doi.org/10.1007/s00586-016-4382-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4382-y