Abstract
Purpose
To investigate the relationship between sagittal spinal alignment and the incidence of vertebral fracture in patients with osteoporosis.
Methods
A cohort of 1,044 postmenopausal women with osteoporosis were prospectively observed for the incidence of lumbar vertebral fracture. Baseline characteristics of the subjects were recorded, including age, year post-menopause, body height and weight, lumbar spine BMD (LSBMD) and femoral neck BMD (FNBMD). Patients with radiologically diagnosed lumbar vertebral fractures were assigned to the fracture group, and 150 randomly selected participants were assigned to the non-fracture group. Parameters depicting sagittal spinal alignment, including sacral slope (SS), pelvic tilt, pelvic incidence (PI), thoracic kyphpsis, lumbar lordosis (LL), lumbar lordosis index (LLI) and sagittal vertical axis, were measured for both groups. Comparison between the two groups was carried out by Student’s t test. Variables showing significant differences were entered into a logistic regression analysis to determine the independent risk factors.
Results
Patients with fracture events had significantly lower LSBMD as well as a significantly longer year post-menopause. Besides, patients with vertebral fracture were found to have significantly lower LL, LLI, SS and PI. Regression analysis showed that LSBMD (OR = 0.27), LL (OR = 0.3), LLI (OR = 0.43) and PI (OR = 0.67) had significant associations with the risk of vertebral fracture.
Conclusions
Osteoporosis patients with low LL, LLI, and PI could be at high risk of lumbar vertebral fracture. In addition to BMD, the abnormal sagittal spinal profile should also be taken into consideration when predicting the incidence of vertebral fracture in such patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a major public health problem characterized by low bone mass, diminished bone strength and increased skeletal fragility leading to the risk for future fractures of the hip, spine or wrist [1]. As a common clinical manifestation of osteoporosis, vertebral fractures could have a strong impact on patients’ morbidity and mortality [2–4]. Following osteoporotic vertebral fracture, there might be permanent spinal deformity and other physical consequences including acute and chronic back pain, immobility, hyperkyphosis and height loss. Population studies demonstrated that vertebral fractures are associated with diminished physical and functional status and overall decline in a patient’s health-related quality of life [5–7].
Since the physical, psychosocial and public health sequelae of vertebral fractures are pronounced, identification of osteoporosis patients at potential risk of vertebral fractures is of great value for clinicians [8, 9]. In contrast to the numerous studies on risk factors for hip fracture, however, there are relatively few data concerning risk factors for vertebral fracture related to osteoporosis. Osteoporotic vertebral fracture risk was previously estimated on the basis of bone mineral density (BMD), which is known to be lower in patients with fractures than controls [10, 11]. However, earlier studies found that women with low BMD could experience no fractures, and there exists substantial overlap in BMD between women with and without radiologically evidenced vertebral compression [12, 13]. Herein it seems that BMD alone may be insufficient for the evaluation of risk for vertebral fracture. In an attempt to understand why some women with low-bone density do not have fractures, other properties of bone that contribute to its strength and three-dimensional bone size have also been investigated, which however, can only explain a small part of the development of vertebral fracture in osteoporosis patients [14, 15]. Therefore, more biomechanical researches that take into account spinal kinetics should be helpful to predict fracture risk of vertebral body.
Sagittal spinal alignment has been reported to play an important role in the biomechanical adaptation of the spine in pathology [16, 17]. In cases with abnormal sagittal spinal profile, gradual failure occurs on the dynamic and static stabilizer along with progressive deformity and limitation of function. Recently, Lee et al. [18] described abnormal sagittal alignment in osteoporosis population as compared with normal controls, and they reported the significant association between high pelvic incidence (PI) and sagittal imbalance in osteoporotic patients. To our knowledge, however, no studies have specifically examined the role of sagittal spinal alignment as a possible determinant of vertebral fractures in osteoporosis patients. We believe that the investigation into sagittal spinal profile of osteoporosis patients can provide clues of the development of vertebral fracture. In the current study, a cohort of osteoporosis patients were prospectively followed up with a mean period of more than 5 years. The aim of this prospective study was to investigate the relationship between sagittal spinal alignment and the incidence of vertebral fracture in patients with osteoporosis.
Methods
Subjects
Under the approval of the local institutional review board, a cohort of 1,321 postmenopausal women who received osteoporosis treatments between April 2004 and March 2011 at three different institutes were prospectively assessed for eligibility of recruitment in the current study. All osteoporotic patients met the diagnostic criterion for osteoporosis (T score <−2.5), and were considered eligible to participate if they had been medically treated for at least 1 year. The exclusion criteria for the current analysis are secondary osteoporosis (e.g., osteopenia with hyperparathyroidism, hyperthyroidism, chronic kidney disease, or osteomalacia), history of previous vertebral fracture and follow-up of less than 2 years.
The endpoint for follow-up was the incidence of vertebral fracture. Radiographs were taken at baseline and during the follow-up period annually, or when a patient complained of fracture-related symptoms. Overall, a total of 1,044 subjects were finally included in this study after the exclusion of 123 cases with secondary osteoporosis, 87 cases with a history of vertebral fracture and 67 cases with insufficient follow-up duration. During the follow-up, all the recruited subjects were prescribed with drugs licensed for the treatment of osteoporosis, including bisphosphonates, selective estrogen receptor modulators, calcitonin, parathyroid hormone and strontium ranelate.
Demographic data collection
Baseline characteristics of the subjects were recorded as they were initially included in the study, including age, year post-menopause, body height and weight, lumbar spine BMD (LSBMD) and femoral neck BMD (FNBMD). Body mass index (BMI) was determined by dividing weight by height square. LSBMD and FNBMD of the non-dominant proximal femur were measured by dual-energy X-ray absorptiometry (DEXA) (XR-36; Norland Corp., Fort Atkinson, WI, USA).
Radiographic examination
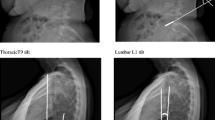
A standardized radiological examination was performed for all participants. Standing left lateral radiograph covering the spine and pelvis was obtained for each participant, who was instructed to stand with the hips and knees fully extended and with the hands rested on supports at the level of their shoulders [19]. Vertebral fractures were defined by an experienced spine surgeon if there was a height reduction of 20 % or more (of at least 4 mm) in any of three vertebral heights (anterior, middle or posterior) between the baseline and the final follow-up x-ray film, or if the vertebrae fulfill the McCloskey-Kanis criteria for a prevalent deformity in the final follow-up film [20]. Patients with radiologically diagnosed lumbar vertebral fractures were assigned to the fracture group, and 150 randomly selected participants were assigned to the non-fracture group.
Parameters depicting sagittal alignments, including sacral slope (SS), pelvic tilt (PT), PI, thoracic kyphpsis (TK), lumbar lordosis (LL) and sagittal vertical axis (SVA), were measured in digital format of the baseline radiograph of the two groups with Surgimap (Spine Software, version 1.1.2, New York, NY, USA) by two residents (D.J. and Y.X.) [19]. Briefly, SS was measured as the angle formed between the superior endplate of S1 and the horizontal plane. PT was measured as angle between the vertical plane and a straight line joining the centers of the femoral heads and the center of the superior endplate of S1. PI was termed as the angle between a line drawn from center of the hip axis to the center of the superior endplate of S1 and perpendicular to the endplate. TK was measured as the angle between the upper endplate of T5 and the lower endplate of T12. LL was measured as the angle between the two lines through the superior endplate of L1 and S1, respectively. Lumbar lordosis index (LLI) was calculated as the ratio of LL to PI [21, 22]. Sagittal balance was defined using the SVA, which was defined as the horizontal distance between a plumb line dropped from the center of the C7 body and the posterior-superior corner of the S1 body. The normal neutral range for sagittal spinal balance was defined as being within 3 cm from the posterior-superior corner of the S1 body.
Radiographs of 100 subjects were randomly selected to determine the inter- and intra-observer reliability using inter- and intra-class correlation coefficients. The inter-observer reliability was high for all the six radiological parameters: 0.912 for SS, 0.887 for PT, 0.921 for PI, 0.932 for PT, 0.945 for LL and 0.913 for SVA. The intra-observer reliability was also high for above radiological parameters: 0.926 for SS, 0.917 for PT, 0.884 for PI, 0.913 for PT, 0.921 for LL and 0.943 for SVA. Therefore, the method of digitally measuring these parameters was confirmed to be acceptable, and the measured data were highly reliable.
Statistical analysis
The data were analyzed using the SPSS 13.0 software (SPSS Inc., Chicago, IL, USA). Descriptive statistics of the baseline characteristics were calculated for all subjects in form of mean value and standard deviation. The incidence of vertebral fracture was calculated as the ratio of the number of fracture patients to the total number of the cohort. With a 5-year value used as age-span, participants were stratified into four age-groups that were composed of patients aged 50–54, 55–59, 60–64, and 65–69 years old, respectively. The incidence of vertebral fracture in each group was calculated, respectively, and the difference of incidence was analyzed using Chi square test. Comparison between the fracture and the non-fracture group regarding baseline characteristics and radiographic parameters was carried out by Student’s t test. Variables showing significant differences were entered into a logistic regression analysis to determine the independent variables associated with the incidence of vertebral fracture. The receiver operating characteristics (ROC) curve was created to identify the best cut-off point for statistically significant variables. Statistical significance was set at a level of p value less than 0.05.
Results
Over a mean follow-up period of 6.7 years, 127 participants (12.2 %) of the cohort were confirmed to have at least one incident lumbar vertebral fracture. The average baseline age of the fracture patients was 56.9 ± 6.8 years (range 50–67 years). The mean year post-menopause was 8.2 ± 4.3 years. The mean weight and BMI of the patients were 57.2 ± 3.9 kg and 23.2 ± 1.5 kg/m2, respectively. The mean LSBMD and the mean FNBMD were 0.723 ± 0.112 and 0.684 ± 0.089 g/cm2, respectively. The incidence of vertebral fracture of the four age-groups was 10.2 % for group 1, 12.1 % for group 2, 12.4 % for group 3 and 13.1 % for group 4, which increased with the age but with no statistical significance. Regarding the localization of the fractures, we found 47 located in L1, 32 in L2, 39 in L3, 29 in L4 and 15 in L5, respectively.
Results of the comparison between the fracture and non-fracture group were shown in Table 1. The average baseline age of the non-fracture group was 54.8 ± 7.4 years (range 53–66 years). There were statistically significant differences in year post-menopause, LSBMD and sagittal spinal alignment including LL, LLI, SS, and PI. Participants with fracture events had significantly lower LSBMD (0.723 ± 0.112 vs. 0.815 ± 0.094 g/cm2, p < 0.001) as well as a significantly longer year post-menopause (8.2 ± 4.3 vs. 5.1 ± 3.5 years, p = 0.003). Besides, patients with vertebral fracture were found to have significantly lower LL, LLI, SS and PI (41.3 ° ± 6.2 ° vs. 47.5 ° ± 7.3 °, p = 0.001 for LL; 24.5 ° ± 4.2 ° vs. 31.3 ° ± 5.1 °, p < 0.001 for SS; 0.97 ± 0.21 vs. 1.03 ± 0.37, p < 0.001 for LLI; 42.3 ° ± 8.7 ° vs. 46.2 ° ± 9.4 °, p = 0.01 for PI). As for baseline age, BMI, LNBMD, TK, PT and SVA, there was no significant difference between the two groups.
A logistic regression model was used to analyze the covariate effects that had been shown to have a significant relationship with the development of vertebral fracture in the crude analysis. Year post-menopause, LSBMD, LL, SS and PI were entered into the model as the candidate predictive variables. As shown in Table 2, LSBMD (OR = 0.27, 95 % CI = 0.18–0.34), LL (OR = 0.32, 95 % CI = 0.14–0.47), LLI (OR = 0.43, 95 % CI = 0.33–0.51) and PI (OR = 0.67, 95 % CI = 0.53–0.79) were found to have significant associations with the presence of vertebral fracture.
ROC analyses of quantitative indices were performed to determine the optimal cut-off values of above variables to predict the risk of vertebral fracture. The optimal cut-off point of year post-menopause was 7.2 years, with a sensitivity and specificity of 81.5 and 59.3 %, respectively. The optimal cut-off point of LSBMD was 0.730 g/cm2, with a sensitivity and specificity of 83.2 and 64.3 %, respectively. The optimal cut-off point of LL was 41° with a sensitivity and specificity of 80.5 and 61.2 %, respectively. The optimal cut-off point of PI was 42°, with a sensitivity and specificity of 79.5 and 62.3 %, respectively.
Discussion
The treatment and prevention of vertebral fracture has gained increasing concern in recent years for its potential impact on healthcare and quality of life amongst the elderly [7, 9]. By far the most widespread cause is regarded to be osteoporosis, with vertebral fractures accounting for more than 45 % of all osteoporotic fractures [23]. For patients with osteoporosis, the risk of vertebral fracture could be increased due to a reduction in compressive strength of bone, usually in form of either burst fracture or wedge compression fracture [24]. Despite its prevalence, the etiology of vertebral fracture remains relatively poorly understood. Previous studies have confirmed that age, BMD and history of fracture could be associated with incidence of vertebral fracture [25–27]. In addition, biomechanical models that aim to predict fracture of the vertebral body showed that local and global spinal properties and structural changes could also be significant risk factors [15, 28, 29]. Various geometric parameters of the vertebral body have thus been investigated, such as anterior vertebral height, vertebral cross-sectional area, and spinal deformity index [30, 31]. With the development of concepts on spinal biomechanics, there has been an increasing emphasis on the understanding of sagittal spinal alignment. Considering that sagittal spinal profile serves as an important part of the individual spinal properties, we therefore prospectively investigated the relationship of sagittal spinal alignment and risk of vertebral fracture in menopausal female with osteoporosis. In the current study, we found significantly different baseline sagittal profiles between osteoporosis patients with and without vertebral fracture. For patients developed incidental vertebral fracture in the follow-up, they had significantly lower LL, LLI and PI at the baseline examination as compared with those having no vertebral fracture detected. As evidenced by the regression analysis, all these three parameters were independent risk factors for the occurrence of vertebral fracture in patients with osteoporosis.
As a constant anatomic signature describing the shape of pelvis, PI serves as a strong determinant of the sagittal spinal alignment in the erect position, which can hardly be influenced by pathologic spinal disorders except for sacro-iliac (SI) joint diseases [16, 19]. As pelvic incidence is the algebraic sum of SS and PT, a lower value of PI indicates that either or both of these values are decreased. Namely, patients with a low PI value usually have low SS and LL values. Furthermore, a low value of LLI was commonly indicative of a low value of LL, which was a well-known factor of excessive mechanical stress on the vertebral body [21]. In many biomechanical models, compressive forces were proved to be associated with the presence of vertebral fracture, which can occur when the force applied to bone exceeds its load-bearing capacity. Therefore, low PI, LL and LLI of osteoporosis patients are therefore quite indicative of accelerated degenerative changes and predisposition to vertebral fracture. In the present study, the ROC analysis showed that the optimal cut-off values of PI and LL were 42 °and 41 °, respectively. As reported by Zhu et al. [19], the normal values of LL and PI in asymptomatic adults of the Chinese population were 48.2 ° and 44.6 °, respectively. Herein, it appears that osteoporosis patients at potential risk of vertebral fracture tend to have significantly lower PI and LL. As for other sagittal parameters including TK and SS, no significant relationship with the incidence of vertebral fracture was found in the present study. To note, TK of patients with vertebral fracture seemed relatively small as compared with the normal value of Chinese female adults (28.1 °) as reported by Zhu et al. We speculated that this difference might be attributed to the inherently different PI and LL of these two cohorts (42.3 ° vs. 44.9 ° for PI; 41.3 ° vs. 48.8 ° for LL), since the reciprocal relationship among the sagittal components of the spine have been well documented in previous studies. Comparison of SVA between the two groups showed that most of the osteoporosis patients could have a normal sagittal balance before the presence of fracture. Lee et al. [18] observed obvious sagittal imbalance in osteoporosis patients with a history of vertebral fracture, and they concluded that PI was a remarkable predictor for the sagittal imbalance. Collectively, it can be concluded that PI is of great value in the prediction of incidental vertebral fracture in osteoporosis patients which can subsequently lead to the sagittal imbalance.
In addition to sagittal spinal alignments, we found that advancing lower BMD measured at the vertebral body was remarkably associated with the risk of vertebral fractures. As indicated by the odds ratio shown in the regression analysis, LSBMD could contribute most highly to the risk of vertebral fracture as compared with other risk factors. Similarly, Jergas et al. [32] observed obvious difference in BMD of subregion of vertebral body between 331 postmenopausal women with and without vertebral fractures. Sandor et al. [33] reported that subregional analysis of lumbar BMD using QCT could discriminate between fracture and non-fracture cases with 90 % accuracy. Collectively, these studies suggest that osteoporosis patients with and without vertebral fractures are likely to be discriminated by the BMD of vertebral body.
In previous literatures age was reported to be a predictor for the development vertebral fracture [11]. In the current study, we observed that the age of fracture patients was older than that of non-fracture patients, while the difference was not significant. In this study the incidence of vertebral fracture was specifically investigated in menopausal women with osteoporosis. Herein, as compared with prior studies, the relatively smaller age span of our subjects could make the difference of age between the fracture and the non-fracture group unremarkable. Instead of age, we noted that patients with vertebral fracture had significantly longer year post-menopause. In the studies of Pouilles et al. [34], early age at menopause was confirmed to be significantly associated with the risk of vertebral fracture. Although it was later excluded from the logistic regression model as the independent risk factor for the vertebral fracture, we speculated that a longer year post-menopause could possibly indicate potentially lower BMD, which substantially act as a strong predictor for vertebral fracture. Therefore, compared with chronological age, year post-menopause seems more representative for the risk of vertebral fracture in elderly women.
The present longitudinal study focuses on sagittal spinal profile of the patients with osteoporosis to predict the risk of vertebral fracture. Our findings suggest that an assessment of sagittal spinal profile would be useful for the prediction of future vertebral fractures over a long period of time. Overall, predictive models for vertebral fracture should encompass a range of important parameters including BMD and patient-specific factors such as LL, LLI and PI. It is noteworthy that the present findings should be interpreted within the context of the following limitation. In the current study, only postmenopausal women were included. It has been proved that there exists remarkable gender difference regarding the risk factors of osteoporotic vertebral fracture [35]. Hence, further studies are warranted to verify whether the current findings can be applied to predict the risk of vertebral fracture in male osteoporosis patients. Besides, the incidence for new fractures in current study (12 % over 5 years) seemed lower than those reported by prior studies in this field. We believed the variation concerning the incidence for new fractures between different studies could be largely resulted from the inconsistent inclusion criteria of the subjects, divergent social structure and lifestyle of the investigated population, different sample size or even the ethnic differences. Herein, a consistently-designed study should be more informative to reveal the incidence of vertebral fracture and the related influential factors. Third, in our study we primarily focused on potentially risky factors including age, year post-menopause, BMD, and BMI, and did not take into account other factors including smoking status or physical activity. Future studies including these factors should be helpful for a more sound conclusion.
In conclusion, we have performed a large-scale prospective study and demonstrated that osteoporosis patients with low LL, LLI and PI could be at high risk of lumbar vertebral fracture. In addition to BMD, the abnormal sagittal spinal profile should also be taken into consideration when predicting the incidence of vertebral fracture in such patients.
References
Jackson SA, Tenenhouse A, Robertson L (2000) Vertebral fracture definition from population-based data: preliminary results from the Canadian Multicenter Osteoporosis Study (CaMos). Osteoporos Int 11:680–687
Ferrar L, Roux C, Felsenberg D, Gluer CC, Eastell R (2012) Association between incident and baseline vertebral fractures in European women: vertebral fracture assessment in the Osteoporosis and Ultrasound Study (OPUS). Osteoporos Int 23:59–65
Imai K (2011) Vertebral fracture risk and alendronate effects on osteoporosis assessed by a computed tomography-based nonlinear finite element method. J Bone Miner Metab 29:645–651
Roux C, Baron G, Audran M, Breuil V, Chapurlat R, Cortet B, Fardellone P, Tremollieres F, Ravaud P (2011) Influence of vertebral fracture assessment by dual-energy X-ray absorptiometry on decision-making in osteoporosis: a structured vignette survey. Rheumatology (Oxford) 50:2264–2269
Begerow B, Pfeifer M, Pospeschill M, Scholz M, Schlotthauer T, Lazarescu A, Pollaehne W, Minne HW (1999) Time since vertebral fracture: an important variable concerning quality of life in patients with postmenopausal osteoporosis. Osteoporos Int 10:26–33
Kushida K, Fukunaga M, Kishimoto H, Shiraki M, Itabashi A, Inoue T, Kaneda K, Morii H, Nawata H, Yamamoto K, Ohashi Y, Orimo H (2004) A comparison of incidences of vertebral fracture in Japanese patients with involutional osteoporosis treated with risedronate and etidronate: a randomized, double-masked trial. J Bone Miner Metab 22:469–478
Wilson S, Sharp CA, Davie MW (2012) Health-related quality of life in patients with osteoporosis in the absence of vertebral fracture: a systematic review. Osteoporos Int 23:2749–2768
Gabriel SE, Tosteson AN, Leibson CL, Crowson CS, Pond GR, Hammond CS, Melton LR (2002) Direct medical costs attributable to osteoporotic fractures. Osteoporos Int 13:323–330
Pluijm SM, Tromp AM, Smit JH, Deeg DJ, Lips P (2000) Consequences of vertebral deformities in older men and women. J Bone Miner Res 15:1564–1572
Shin CS, Kim MJ, Shim SM, Kim JT, Yu SH, Koo BK, Cho HY, Choi HJ, Cho SW, Kim SW, Kim SY, Yang SO, Cho NH (2012) The prevalence and risk factors of vertebral fractures in Korea. J Bone Miner Metab 30:183–192
Waterloo S, Nguyen T, Ahmed LA, Center JR, Morseth B, Nguyen ND, Eisman JA, Sogaard AJ, Emaus N (2012) Important risk factors and attributable risk of vertebral fractures in the population-based Tromso study. BMC Musculoskelet Disord 13:163
Norimatsu H, Mori S, Uesato T, Yoshikawa T, Katsuyama N (1989) Bone mineral density of the spine and proximal femur in normal and osteoporotic subjects in Japan. Bone Miner 5:213–222
Vokes TJ, Giger ML, Chinander MR, Karrison TG, Favus MJ, Dixon LB (2006) Radiographic texture analysis of densitometer-generated calcaneus images differentiates postmenopausal women with and without fractures. Osteoporos Int 17:1472–1482
Snyder BD, Piazza S, Edwards WT, Hayes WC (1993) Role of trabecular morphology in the etiology of age-related vertebral fractures. Calcif Tissue Int 53(Suppl 1):S14–S22
Gilsanz V, Loro ML, Roe TF, Sayre J, Gilsanz R, Schulz EE (1995) Vertebral size in elderly women with osteoporosis. Mechanical implications and relationship to fractures. J Clin Invest 95:2332–2337
Winter RB, Lonstein JE, Denis F (2009) Sagittal spinal alignment: the true measurement, norms, and description of correction for thoracic kyphosis. J Spinal Disord Tech 22:311–314
Lafage V, Smith JS, Bess S, Schwab FJ, Ames CP, Klineberg E, Arlet V, Hostin R, Burton DC, Shaffrey CI (2012) Sagittal spino-pelvic alignment failures following three column thoracic osteotomy for adult spinal deformity. Eur Spine J 21:698–704
Lee JS, Lee HS, Shin JK, Goh TS, Son SM (2013) Prediction of sagittal balance in patients with osteoporosis using spinopelvic parameters. Eur Spine J 22:1053–1058
Zhu Z, Xu L, Zhu F, Jiang L, Wang Z, Liu Z, Qian BP, Qiu Y (2014) Sagittal alignment of spine and pelvis in asymptomatic adults: norms in Chinese populations. Spine (Phila Pa 1976) 39:E1–E6
Grigoryan M, Guermazi A, Roemer FW, Delmas PD, Genant HK (2003) Recognizing and reporting osteoporotic vertebral fractures. Eur Spine J 12(Suppl 2):S104–S112
Boissiere L, Vital JM, Aunoble S, Fabre T, Gille O, Obeid I (2014) Lumbo-pelvic related indexes: impact on adult spinal deformity surgery. Eur Spine J. doi:10.1007/s00586-014-3402-z
Boissiere L, Bourghli A, Vital JM, Gille O, Obeid I (2013) The lumbar lordosis index: a new ratio to detect spinal malalignment with a therapeutic impact for sagittal balance correction decisions in adult scoliosis surgery. Eur Spine J 22:1339–1345
Sisodia GB (2013) Methods of predicting vertebral body fractures of the lumbar spine. World J Orthop 4:241–247
Bouxsein ML, Melton LR, Riggs BL, Muller J, Atkinson EJ, Oberg AL, Robb RA, Camp JJ, Rouleau PA, McCollough CH, Khosla S (2006) Age- and sex-specific differences in the factor of risk for vertebral fracture: a population-based study using QCT. J Bone Miner Res 21:1475–1482
Sanfelix-Gimeno G, Sanfelix-Genoves J, Hurtado I, Reig-Molla B, Peiro S (2013) Vertebral fracture risk factors in postmenopausal women over 50 in Valencia Spain. A population-based cross-sectional study. Bone 52:393–399
Lopes JB, Danilevicius CF, Takayama L, Caparbo VF, Menezes PR, Scazufca M, Kuroishi ME, Pereira RM (2011) Prevalence and risk factors of radiographic vertebral fracture in Brazilian community-dwelling elderly. Osteoporos Int 22:711–719
Fujiwara S, Hamaya E, Goto W, Masunari N, Furukawa K, Fukunaga M, Nakamura T, Miyauchi A, Chen P (2011) Vertebral fracture status and the World Health Organization risk factors for predicting osteoporotic fracture risk in Japan. Bone 49:520–525
Duan Y, Parfitt A, Seeman E (1999) Vertebral bone mass, size, and volumetric density in women with spinal fractures. J Bone Miner Res 14:1796–1802
Huang MH, Barrett-Connor E, Greendale GA, Kado DM (2006) Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res 21:419–423
Briggs AM, Wrigley TV, van Dieen JH, Phillips B, Lo SK, Greig AM, Bennell KL (2006) The effect of osteoporotic vertebral fracture on predicted spinal loads in vivo. Eur Spine J 15:1785–1795
Cairoli E, Eller-Vainicher C, Ulivieri FM, Zhukouskaya VV, Palmieri S, Morelli V, Beck-Peccoz P, Chiodini I (2014) Factors associated with bisphosphonate treatment failure in postmenopausal women with primary osteoporosis. Osteoporos Int 25:1401–1410
Jergas M, Breitenseher M, Gluer CC, Black D, Lang P, Grampp S, Engelke K, Genant HK (1995) Which vertebrae should be assessed using lateral dual-energy X-ray absorptiometry of the lumbar spine. Osteoporos Int 5:196–204
Sandor T, Felsenberg D, Brown E (1997) Discriminability of fracture and nonfracture cases based on the spatial distribution of spinal bone mineral. J Comput Assist Tomogr 21:498–505
Pouilles JM, Tremollieres F, Bonneu M, Ribot C (1994) Influence of early age at menopause on vertebral bone mass. J Bone Miner Res 9:311–315
Roy DK, O’Neill TW, Finn JD, Lunt M, Silman AJ, Felsenberg D, Armbrecht G, Banzer D, Benevolenskaya LI, Bhalla A, Bruges AJ, Cannata JB, Cooper C, Dequeker J, Diaz MN, Eastell R, Yershova OB, Felsch B, Gowin W, Havelka S, Hoszowski K, Ismail AA, Jajic I, Janott I, Johnell O, Kanis JA, Kragl G, Lopez VA, Lorenc R, Lyritis G, Masaryk P, Matthis C, Miazgowski T, Gennari C, Pols HA, Poor G, Raspe HH, Reid DM, Reisinger W, Scheidt-Nave C, Stepan JJ, Todd CJ, Weber K, Woolf AD, Reeve J (2003) Determinants of incident vertebral fracture in men and women: results from the European Prospective Osteoporosis Study (EPOS). Osteoporos Int 14:19–26
Acknowledgments
We sincerely thank Dr. Bingjian Wang from the Huai'an First People's Hospital for his assistance with the proof-reading of our manuscript.
Conflict of interest
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Dai, X. Yu and S. Huang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Dai, J., Yu, X., Huang, S. et al. Relationship between sagittal spinal alignment and the incidence of vertebral fracture in menopausal women with osteoporosis: a multicenter longitudinal follow-up study. Eur Spine J 24, 737–743 (2015). https://doi.org/10.1007/s00586-014-3637-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3637-8