Abstract
Purpose
To evaluate postoperative recurrence, survival and metastasis results and related factors of sacral chordoma.
Methods
Between 1978 and 2013, a total of 171 patients with sacral chordoma were diagnosed at our institution and 162 cases underwent operation. The clinical characteristics, treatment and outcomes of all these patients were reviewed.
Results
The 3-year recurrence free survival rate was 83.1%. The median recurrence free survival time was 73 ± 7.8 months. Tumor level in sacrum and surgical margin were significant factors influencing recurrence. Recurrence was significant factor influencing metastasis. One hundred and fifty-seven cases were followed up for an average of 55.6 months. 135 cases (86%) survived, 37 cases (23.6%) developed recurrence, and 17 cases (10.8%) developed metastasis. The overall 5- and 10-year survival rate was 88.3% and 59.6%, respectively. Age (p = 0.037) and metastasis (p = 0.001) were significant factors influencing survival. The 3-year recurrence free survival rate was 80.1%. The median recurrence free survival time was 69 ± 12.7 months. Tumor level in sacrum (p = 0.035) and surgical margin (p = 0.009) were significant factors influencing recurrence. Seventeen cases (10.8%) had metastasis. Recurrence (p = 0.016) was significant factors influencing metastasis.
Conclusions
Sacral chordoma tended to occur in elderly male patients and locate below sacral 3 level. The recurrence rate was high, especially for tumor above sacral 3 level. Wide surgical margin is very important for good local control. The patients with metastasis had poor prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chordoma is a rare malignant tumor originated from the embryonic notochordal remnants [1]. The incidence rate was only 0.5–0.8/million, accounting for about 17.5% of axial primary malignant bone tumor [1, 2]. Most sacral chordoma patients are in the fifth to seventh decades. The male and female incidence rate is about 2–3:1. The patients with sacral chordomas often complain chronic sacral or flank pain with a quite long history. When tumors grow larger and invade pelvic organs or nerve roots, rectum and bladder dysfunction will present. Therefore, many patients undergo delayed diagnosis and treatment.
The most effective treatment is surgical excision. But the complex anatomy induces operative difficulty. Postoperative complications and recurrences are common. Because of its low incidence, bulks of cases were rarely reported [3–5]. Postoperative local recurrence rates were as high as 43–85% [3–11]. Most recurrences were found in three years postoperative. The inappropriate surgical margin was related to recurrence. Huge tumor and extensive involvement increased difficulty for safe surgical resection. Literature reports showed 5 and 10 years survival rates which were 45–97 and 28–71%, respectively [3–11]. The data showed great differences in survival. Therefore, we reviewed bulk of sacral chordoma cases at our institution in China. The postoperative recurrence, survival and metastasis results were analyzed, and related influence factors were also evaluated.
Materials and methods
General clinical characteristic
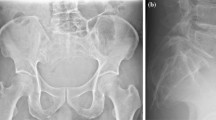
The entire cohort of 171 consecutive patients with sacral chordoma was retrospectively analyzed in the study at our institution between 1978 and 2013 (Table 1). Inclusion criteria: diagnosis of sacral chordoma was pathological confirmed; complete data as clinical, radiological and pathological results were collected; follow-up was more than 12 months. The primary manifestations were lumbosacral pain which may radiate to the buttocks, perineal or lower extremity. The average time interval from onset of symptoms to diagnosis was 23.6 (2–132) months. All patients received sacral radiograph examinations. CT was used in 156 cases since 1985 and MRI was used in 145 cases since 1990. The maximal tumor diameter and maximum transverse diameter in axial were measured in MRI (if available) or CT. Needle biopsy was performed in primary cases before operation. The pathological diagnosis was confirmed by postoperative pathology.
Operation method
162 patients received operation. Preoperative high selective tumor supplying artery embolization was performed in 77 cases since 2005. Surgical methods contained single posterior approach and combined approach. Anterior retroperitoneal approach could reveal the iliac vascular and lumbosacral nerve root clearly. The main purpose of anterior approach is ligating internal iliac artery to reduce bleeding. Therefore, with the application of the preoperative high selective embolization of vessels which supplied the tumor, the combined approach was seldom used and almost all cases were treated with posterior approach in the latter of our study. Posterior approach could expose dorsal sacrum and iliac wing and surrounding soft tissue, so as to resect tumor completely. The intraoperative osteotomy level was generally confirmed through fluoroscopy and measurement. The average operation time was 256.7 (70–495) minutes; the average intraoperative blood loss was 3023 (400–8500) ml. The wound was examined on postoperative day 3. Drains were removed if drainage fluid was less than 30 ml per day. The postoperative specimens were soaked in formalin and then cut in the maximum diameter of the tumor for cross and sagittal sections, to confirm the surgical margin. 157 cases with completed data were evaluated. According to the musculoskeletal tumor surgical staging (Enneking staging) [5], the results included intracapsular resection in 64 cases, marginal resection in 62 cases and wide resection in 31 cases. The patients with positive margin received radiotherapy postoperative. Therefore, sixty-four cases with intralesional margin received radiotherapy postoperative. The surgical margin was based on the evaluation of the postoperative specimen. The specimen was soaked in formalin and then cut for evaluation. We considered 1.5 cm margin of normal bone or soft tissue resection as wide margin. But this 1.5 cm wide margin was not applied to anterior margin of the tumors, which are often adjacent to visceral organs but rarely involve the viscera.
Follow-up
The patients were followed every three months during the first 2 years postoperatively. Physical examination, plain radiography of the chest, sacrum, and lower lumbar spine and ultrasonography was also performed. If ultrasonography showed any abnormal sign, CT and MRI would be performed. Ultrasonography, chest CT, lumbosacral CT and MRI and whole-body bone scanning were performed every 6 months. After the third postoperative year, patients were followed once a year. It contained plain radiography of the chest, sacrum, and lower lumbar spine, ultrasonography of the surgical site, chest CT, lumbosacral CT and whole-body bone scanning.
Statistical analysis
Kaplan–Meier method was used for overall survival (OS) and recurrence free survival (RFS). Multiple Cox regression analysis was used for the factors on recurrence, survival and metastasis. Log-rank test was used to compare overall survival and recurrence free survival in different group. Continuous variables were compared with the t test and categorical variables were compared by Chi-square test or Fisher exact probability method. Correlation analysis of influence factor on recurrence time was done: Pearson correlation test was used for parametric factors and Spearman correlation test for nonparametric factors. The data were analyzed by SPSS software (version 16.0; SPSS, Chicago, IL, USA). All statistical values were considered significant at p < 0.05.
Result
Recurrence
After removing nine nonoperative cases and five cases with incomplete data, 157 cases were evaluated. The average follow-up time was 55.6 months (median 49.5, range 12–279 months). Thirty-seven cases (23.6%) developed recurrence after an average of 33.9 months (median 30, range 3–97 months). Twenty cases (54.1%) developed recurrence in 3 years and thirty-two cases (86.4%) developed recurrence in 5 years postoperative. Kaplan–Meier analysis shows that the 3-year RFS was 80.1% and the 5-year RFS was 48.1%. The median RFS time was 69 ± 12.7 months (95% Confidence interval 49.0–89.0 months) (Fig. 1a).
Multivariate analysis showed the tumor level in sacrum and surgical margin were significant factors (Table 2). So the tumor level in sacrum and surgical margin needed further analysis. The 5-years RFS in group above S3 and group below S3 were 27.9 and 62.5%, respectively; the median RFS time was 53 and 84 months, respectively (Fig. 1b). The recurrence rate in group above S3 was significantly higher than that in group below S3 (p = 0.010). The 5 years RFS of intracapsular, marginal and wide resection were 34.6, 56.9 and 83.3%, respectively; the median recurrence free survival time was 47, 65 and 124 months, respectively (Fig. 1c). The recurrence rate in non-wide margin group was significantly higher than that in wide margin group (p = 0.012). Before 2005, we usually performed intracapsular resection in tumor above S3 to protect sacral 1-3 nerve root, so for further analysis, we compare cases before and after 2005. Before 2005, intracapsular margin rate was 68.0% and recurrence rate was 52.0%; after 2005, intracapsular margin rate was 38.4% and recurrence rate was 19.2%. The recurrence rate was significant different in two groups (p = 0.014), this result confirm the effect of margin on recurrence. The tumor size showed no significant difference effect on recurrence (p = 0.817). The average maximum diameter of tumor in recurrence group and non-recurrence group were 9.2 and 8.8 cm, respectively.
Age (p = 0.316, r = 0.163), gender (p = 0.502, r = 0.109), tumor size (p = 0.076, r = 0.347), tumor level in the sacrum (p = 0.354, r = 0.150), operation time (p = 0.591, r = 0.136), blood loss (p = 0.865, r = 0.043) and surgical margin (p = 0.229, r = 0.195) had no significant correlation with the recurrence time.
Survival
One hundred and thirty-five cases (86%) survived and 22 cases (14%) died. Seven patients died of lung metastasis and three of them were recurrent cases. Seven patients died in perioperative period and six of them were recurrent cases. Three cases died of repeated tumor relapse and they finally could not tolerate operation, cachexia and consumption. There were five patients who died of other diseases, but not chordoma. So 54.5% (12 cases) of died patients were recurrent cases and 18.5% (25 cases) of survival patients were recurrent cases (p = 0.000). Average postoperative survival time of death was 51.2 months (median 45.5, range 4-120 months). Kaplan–Meier survival analysis showed the 5-year OS was 88.3%, 10-year OS was 59.6% (Fig. 2a). The 5-year and 10-year disease-specific survival was 89.6 and 64.1%, respectively.
Multivariate analysis showed age (p = 0.037), tumor size (p = 0.034) and metastasis (p = 0.001) are significant factors for survival, while gender (p = 0.157), tumor level (p = 0.285) and recurrence (p = 0.087) were not. So those significant factors needed further analysis. The mean age in survival group and death group were 52.6 ± 12.2 and 65 ± 10.2 years, respectively (p = 0.000). The average maximal tumor diameter in survival group and death group were 8.7 ± 2.9 and 10 ± 3.1 cm, respectively. But no significant difference were shown between these two groups (p = 0.136). The 5-year OS in metastasis group was significantly lower than that in non-metastasis group (p = 0.001) (Fig. 2b). Local recurrence showed no significant effect on survival (p = 0.072).
Metastasis
Seventeen cases (10.8%) developed metastasis, which included five cases of primary lung metastasis, three cases of bone metastasis (ribs and vertebral body) and nine cases of lung metastasis postoperative. In all 14 cases with lung metastasis, nine patients died. Two patients with rib metastasis received rib resection and no new lesion was found. One patient with spinal metastasis received tumor resection and decompression operation. But the lesion relapsed in spine and the patient received operation again. Multivariate analysis showed that local recurrence was the only significant factor for metastasis (Table 2).
Discussion
Sacral chordoma grows slowly with no significant early symptom in many patients. The average time interval from onset of symptoms to diagnosis at our institute was nearly 2 years, and the longest was 11 years. The maximal tumor diameter was up to 16.7 cm. There was usually delayed diagnosis and treatment [2, 5].
Sacral chordoma is a low-grade malignant tumor with recurrence and metastasis tendency. A recent large series of 99 sacral chordomas with long follow-up showed OS at 5, 10, and 15 year were 92, 45 and 36%, respectively [12]. The incidence of local recurrence and distant metastases were 30 and 9% at 5 years, 46 and 18% at 10 years. The authors suggested the tumor size and surgical margin were significant predictors of long-term outcome. The previous reports showed quite different survival rate and the long-term results were poor. We followed 157 cases and found that 135 cases survived (86%). The 5-year OS was 88.3% and 10-year OS was 59.6%, which showed a high survival rate compared with literatures. Through the analysis of influencing factors on survival, we found elderly and metastasis were poor factors for survival, which was similar with the literature [2, 4].
The health condition of the elder is weaker than that of young people. So the elders have poor tolerance of sacral tumor resection and perioperative risk is higher. If the tumor has recurrence or metastasis, some elderly patients cannot receive second operation due to the poor physical condition. So the survival rate is low. The results also suggested us to consider the potential relationship between recurrence and survival. But the multivariate analysis did not show significant effect on survival (p = 0.087). There may be some reasons although the overall sample size was large, but the number of deaths was relatively small; some other parallel factors may mix with recurrence. Some patients could not bear repeated surgery and complications, so the quality of life was poor. In recent years, with the improvement of oncology concept and surgical techniques, peri-operation death was rare.
Some recent studies [13, 14] on possible biomarkers of sacral chordoma showed positive results. Hobusch [13] analyzed 24 chordomas and found C-reactive protein (CRP) was an independent survival factor. The survival rate of patients with high preoperative CRP level (>1.0 mg/dl) was significant lower than that with low CRP level (<1.0 mg/dl). CRP is an acute-phase protein in chronic inflammatory microenvironment caused by many types of tumors. Therefore, the inflammation may be related with the processes of tumor growth, recurrence and metastasis. Another study [14] with 37 chordoma samples showed that the expression of PHLPP1 was down-regulated in chordoma and this was correlated with tumor relapse. It suggested that PHLPP1 may be a prognostic indicator for sacral chordoma,
The metastasis rate in our study was 10.8%; the survival rate of patient with metastasis was lower. Previous reports showed metastasis rate was 5–40% with poor prognosis [2, 4, 11]. We found that gender, tumor level, tumor size were not significant factors affecting survival. While the literature report showed male, small tumor size and located in the distal sacrum, wide margin and early treatment was good factors [2, 12, 15].
As many patients can have long-term survival, local control is very important. The preferred treatment of sacral chordoma is surgical resection and it is not sensitive to chemotherapy. Radiotherapy may decrease the local recurrence rate [3], but did not improve survival [16, 17]. We found the tumor level in sacrum and surgical margin were significant factors influencing recurrence.
Tumor level in sacrum was significant factor which affected local recurrence. Our study showed the recurrence rate in group above S3 was 38.1%, while the recurrence rate in group below S3 was 18.3%. As S3 was a dividing line, high level tumor tended to recurrent. The reasons may be as following: sacral nerves above S3 have more important function for recovery, it’s more difficult to achieve safe margin for nerve protection; there are less important anatomical structures below S3, so wide excision can be achieved; tumor above S3 is closed to major vascular, more bleeding during operation increased difficulty and risk. Previous reports [18, 19] with small samples also suggested the high recurrence rate of high level tumor.
Our data showed that different surgical margin led to different recurrence rate. The recurrence rate after intracapsular resection, marginal resection and wide resection were 31.3, 24.2 and 6.5%, respectively. But because of the special position and anatomical structure, wide surgical margin is often difficult to achieve. According to literatures, recurrence rate after wide resection was 0–60%, while the recurrence rate after non-wide resection was 43–85% [3–7, 9, 11, 20]. Yonemoto [11] reported intracapsular resection led to high recurrence rate as 60%, and cases with wide excision showed no recurrence. Fuchs [7] reported only one case of recurrence in 31 cases with wide resection, but 22 cases of recurrence in 31 cases with unsafe margin. The recent reports and review also confirmed that wide resection margin could lead to good long-term prognosis [15, 21]. Ruosi [22] reported 14 patients treated with sacral chordoma resection and the local recurrence was 42.86%. The authors suggested that the resection should result in margin as wide as possible to decrease the risk of recurrence. Another recent study [23] on 29 sacral chordomas received “en bloc” resection showed low recurrence rate (24.1%) with wide margins.
Some authors [3, 5] suggested tumor size was related to recurrence. Our cases showed the maximum tumor diameter in recurrent group was greater than that in non-recurrence group, but there was no significant difference. Thieblemont [24] reported that age was related to recurrence. Our study showed recurrence group had higher age, but there was no significant difference. In addition, operation time and blood loss during operation did not affect recurrence rate. The average recurrent time was 33.9 months and more than half of cases were in first 3 years. Postoperative radiotherapy was associated with local control following intralesional excision [25, 26]. Some recent reports [27, 28] showed that high-dose photon/proton treatment with sacral chordoma resulted good local control. Carbon ion treatment also resulted in preservation of urinary-anorectal function [29]. Some recent studies [30, 31] suggested that miR-1 and STAT-3 (signal transducer and activator of transcription) may be potential therapeutic target for chordoma,
There are some limitations in this paper. First, it was a retrospective study. Second, this consecutive series spans a quite long period. Heterogeneity of materials and methods is a week point. The imaging examination methods, apply of artery embolism and surgical technology had changed with time. For surgical method, we usually performed intralesional resection in tumor above S3 to protect nerve root before 2005. Therefore, as we analyzed in results, late cases showed the tendency of safer margins and lower recurrence rates in contrast with early cases. Especially for tumors above S3, lower intracapsular margin rates and recurrence rates were achieved after 2005. In recent years, the preoperative embolization greatly reduced intraoperative bleeding and perioperative mortality in our clinical practice. Many reports [32–36] suggested the preoperative selective arterial embolization is an effective method to control bleeding during the resection of sacrum tumor. The high selective embolization of tumor supplying artery can also reduce the incidence of complications, such as delayed wound healing and local muscle or skin necrosis.
In recent years, the development of surgical techniques has improved the safety of operation, but how to achieve good local control is still difficult. We reviewed the large sample of patients and found tumor level in sacrum and surgical margin were significant factors influencing recurrence. Patients with metastasis had poor survival prognosis, while recurrence was related to metastasis. The tumor location, size, and surrounding important anatomic structures often restrict the access to safe margin. Through rigorous preoperative design, grasp of complex anatomy and postoperative assessment, we may bring benefit to more patients.
References
McMaster ML, Goldstein AM, Bromley CM et al (2001) Chordoma: incidence and survival patterns in the United States, 1973–1995. Cancer Causes Control 12:1–11
Eriksson B, Gunterberg B, Kindblom LG (1981) Chordoma: a clinicopathologic and prognostic study of a Swedish national series. Acta Orthop Scand 52:49–58
York JE, Kaczaraj A, Abi-Said D et al (1999) Sacral chordoma: 40-year experience at a major cancer center. Neurosurgery 44(1):74–79
Samson IR, Springfield DS, Suit HD (1993) Operative treatment of sacrococcygeal chordoma. J Bone Joint Surg (Am) 75(10):1476–1484
Baratti D, Gronchi A, Pennacchioli E et al (2003) Chordoma: natural history and results in 28 patients treated at a single institution. Ann Surg Oncol 10:291–296
Bergh P, Kindblom LG, Gunterberg B et al (2000) Prognostic factors in chordoma of the sacrum and mobile spine: a study of 39 patients. Cancer 88:2122–2134
Fuchs B, Dickey ID, Yaszemski MJ et al (2005) Operative management of sacral chordoma. J Bone Joint Surg Am 87:2211–2216
Gunterberg B, Romanus B, Sterner B (1976) Pelvic strength after major amputation of the sacrum: an experimental study. Acta Orthop Scand 47:635–642
Hulen CA, Temple HT, Fox WP et al (2006) Oncologic and functional outcome following sacrectomy for sacral chordoma. J Bone Joint Surg Am 88:1532–1539
Osaka S, Kodoh O, Sugita H et al (2006) Clinical significance of a wide excision policy for sacrococcygeal chordoma. J Cancer Res Clin Oncol 132:213–218
Yonemoto T, Tatezaki S, Takenouchi T et al (1999) The surgical management of sacrococcygeal chordoma. Cancer 85:878–883
Radaelli S, Stacchiotti S, Ruggieri P et al (2016) Sacral chordoma: long-term outcome of a large series of patients surgically treated at two reference centers. Spine 41(12):1049–1057 (Phila Pa 1976)
Hobusch GM, Bodner F, Walzer S et al (2016) C-reactive protein as a prognostic factor in patients with chordoma of lumbar spine and sacrum-a single center pilot study. World J Surg Oncol 14(1):111–116
Chen H, Zhang K, Wu G et al (2015) Low expression of PHLPP1 in sacral chordoma and its association with poor prognosis. Int J Clin Exp Pathol 8(11):14741–14748
Varga PP, Szövérfi Z, Fisher CG et al (2015) Surgical treatment of sacral chordoma: prognostic variables for local recurrence and overall survival. Eur Spine J 24(5):1092–1101
Catton C, O’Sullivan B, Bell R et al (1996) Chordoma: long-term follow-up after radical photon irradiation. Radiother Oncol 41:67–72
Ozerdemoglu RA, Transfeldt EE, Thompson RC (1999) Lumbosacral chordoma: prognostic factors and treatment. Spine 24:1639–1645
Chen KW, Yang HL, Lu J et al (2010) Prognostic factors of sacral chordoma after surgical therapy: a study of 36 patients. Spinal Cord 48:166–171
Hanna A, Aston S, Briggs R et al (2008) Sacral chordoma can local recurrence after sacrectomy be predicted? Clin Orthop Relat Res 466:2217–2223
Puri A, Agarwal MG, Shah M et al (2009) Decision making in primary sacral tumors. Spine J 9:396–403
Kayani B, Hanna SA, Sewell MD et al (2014) A review of the surgical management of sacral chordoma. Eur J Surg Oncol 40(11):1412–1420
Ruosi C, Colella G, Di Donato SL et al (2015) Surgical treatment of sacral chordoma: survival and prognostic factors. Eur Spine J 24(Suppl 7):912–917
Dubory A, Missenard G, Lambert B et al (2014) “En bloc” resection of sacral chordomas by combined anterior and posterior surgical approach: a monocentric retrospective review about 29 cases. Eur Spine J 23(9):1940–1948
Thieblemont C, Biron P, Rocher F et al (1995) Prognostic factors in chordoma: role of postoperative radiotherapy. Eur J Cancer 31A:2255–2259
Jian BJ, Bloch OG, Yang I et al (2010) Adjuvant radiation therapy and chondroid chordoma subtype are associated with a lower tumor recurrence rate of cranial chordoma. J Neurooncol 98(1):101–108
Boriani S, Saravanja D, Yamada Y et al (2009) Challenges of local recurrence and cure in low grade malignant tumors of the spine. Spine 34(22 Suppl):S48–S857 (Phila Pa 1976)
DeLaney TF, Liebsch NJ, Pedlow FX et al (2014) Long-term results of Phase II study of high dose photon/proton radiotherapy in the management of spine chordomas, chondrosarcomas, and othersarcomas. J Surg Oncol 110:115–122
Imai R, Kamada T, Sugahara S et al (2011) Carbon ion radiotherapy for sacral chordoma. Br J Radiol 84(3):48–54
Nishida Y, Kamada T, Imai R et al (2011) Clinical outcome of sacral chordoma with carbon ion radiotherapy compared with surgery. Int J Radiat Oncol Biol Phys 79:110–116
Osaka E, Yang X, Shen JK et al (2014) MicroRNA-1 (miR-1) inhibits chordoma cell migration and invasion by targeting slug. J Orthop Res 32(8):1075–1082
Yang C, Hornicek FJ, Wood KB et al (2010) Blockage of Stat3 with CDDO-Me inhibits tumor cell growth in chordoma. Spine 35:1668–1675
Yang HL, Chen KW, Wang GL et al (2010) Pre-operative transarterial embolization for treatment of primary sacral tumors. J Clin Neurosci 17(10):1280–1285
Xiaodong T, Wei G, Rongli Y et al (2009) Risk factors for blood loss during sacral tumor resection. Clin Orthop Relat Res 467:1599–1604
Yang H, Zhu L, Ebraheim NA et al (2010) Surgical treatment of sacral chordomas combined with transcatheter arterial embolization. J Spinal Disord Tech 23(1):47–52
Yin CH, Benjamin N, Randall WP et al (2011) Transarterial Onyx embolization of sacral chordoma: case report and review of the literature. Albuquerque J NeuroIntervent Surg 3:85–87
Xiaodong T, Wei G, Rongli Y et al (2010) Use of aortic balloon occlusion to decrease blood loss during sacral tumor resection. J Bone Joint Surg Am 92(8):1747–1753
Acknowledgments
The work is supported by Beijing Talents Fund (NO. 2015000021469G181).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest regarding this study.
Additional information
Level of evidence: Case series. IV.
Rights and permissions
About this article
Cite this article
Yang, Y., Niu, X., Li, Y. et al. Recurrence and survival factors analysis of 171 cases of sacral chordoma in a single institute. Eur Spine J 26, 1910–1916 (2017). https://doi.org/10.1007/s00586-016-4906-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4906-5